ABSTRACT
BACKGROUND
The 2003 and 2011 Accreditation Council for Graduate Medical Education (ACGME) common program requirements compress busy inpatient schedules and increase intern supervision. At the same time, interns wrestle with the effects of electronic medical record systems, including documentation needs and availability of an ever-increasing amount of stored patient data.
OBJECTIVE
In light of these changes, we conducted a time motion study to determine how internal medicine interns spend their time in the hospital.
DESIGN
Descriptive, observational study on inpatient ward rotations at two internal medicine residency programs at large academic medical centers in Baltimore, MD during January, 2012.
PARTICIPANTS
Twenty-nine interns at the two residency programs.
MAIN MEASURES
The primary outcome was percent of time spent in direct patient care (talking with and examining patients). Secondary outcomes included percent of time spent in indirect patient care, education, and miscellaneous activities (eating, sleeping, and walking). Results were analyzed using multilevel regression analysis adjusted for clustering at the observer and intern levels.
KEY RESULTS
Interns were observed for a total of 873 hours. Interns spent 12 % of their time in direct patient care, 64 % in indirect patient care, 15 % in educational activities, and 9 % in miscellaneous activities. Computer use occupied 40 % of interns’ time. There was no significant difference in time spent in these activities between the two sites.
CONCLUSIONS
Interns today spend a minority of their time directly caring for patients. Compared with interns in time motion studies prior to 2003, interns in our study spent less time in direct patient care and sleeping, and more time talking with other providers and documenting. Reduced work hours in the setting of increasing complexity of medical inpatients, growing volume of patient data, and increased supervision may limit the amount of time interns spend with patients.
KEY WORDS: residency work hours, graduate medical education, time motion
The Accreditation Council for Graduate Medical Education (ACGME) Common Program Requirements, launched in July of 2003 and revised in 2011, limit continuous and total work hours for interns and increase supervision requirements.1 Many question whether limiting the length of shifts and total time in the hospital, particularly for interns, will reduce the time spent at the patient’s bedside and alter the balance between service and learning.2,3 Changes to the healthcare landscape, including adoption of electronic medical record and provider order entry systems, shortened hospitalizations, increased supervision, and team-based care, may also impact intern time allocation.
Concerns about how residency program structure affects inpatient care and the patient–doctor relationship4 prompted the first time motion studies of residents. These revealed that residents spent little time delivering direct patient care and devoted the majority of time to administrative tasks.5,6 In the wake of the New York State Bell Commission recommendations of 1989, a set of formal time-motion studies by Lurie7,8 found that interns spent more time documenting, 42–45 %, than they did with patients, 18–22 %, and up to 40 % of time engaged in “miscellaneous” activities like sleeping and eating. Follow-up studies9,10 and a meta-analysis during pre-2003 conditions found similar results.11–13 A recent time motion study by Fletcher using data collected in 2010, following the 2003 ACGME work hours reform, found that interns on call spent considerably less time with patients and more time documenting and communicating with the medical team than the prior studies.14
To understand the impact of the 2003 and 2011 work hours limits on the inpatient work of internal medicine interns throughout the work week, we conducted a time-motion study at two large academic medical centers in Baltimore. We hypothesized that interns today spend a minority of their time in direct patient care, in educational activities, and sleeping, and a majority of their time engaged in indirect patient care activities, including utilizing the electronic medical record (EMR) and writing notes.
METHODS
Study Design and Setting. This was a descriptive observational study modeled on previous investigations.7–9 Internal medicine interns at two large (1,051 and 757 beds, respectively), tertiary care academic medical centers in Baltimore, Maryland were observed for 3 weeks of inpatient work during January, 2012. Resident teams at both hospitals care for a predominantly urban population, as well as patients referred from community hospitals. Neither site employs mid-level providers on the resident inpatient medical services. Interns were shadowed throughout the call cycle to allow for a global assessment of time spent with patients.
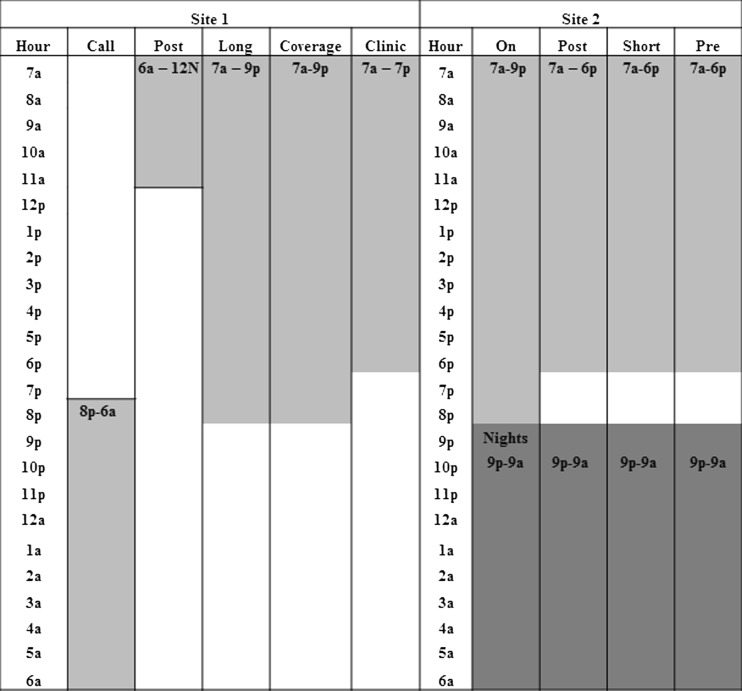
We recruited interns so as to observe them over an equal number of hours at both sites and to sample shifts in proportion to the amount of workweek time interns spend on each of these shifts. Site 1 uses a modified overnight call system, wherein interns take “overnight” call from 8 pm until noon once every five nights, and rotate through daytime admitting and coverage roles in the intervening days (Fig. 1). Two general medicine teams from site 1 were selected at random for participation. All ten interns rotating on these two teams at the time of the study, representing 21 % of the medicine interns at site 1, were approached for participation. Interns at site 1 were observed for three shifts, each representing different positions in the call cycle.
Figure 1.
Weekday call schedule, site 1 and 2. At Site 1, call/post is an overnight admitting shift, beginning at 8 pm and ending at 12 pm the following day. Long is a daytime admitting shift beginning at 7 am and ending at 9 pm. Coverage is a daytime shift beginning at 7 am and ending at 9 pm. Clinic is a daytime shift split between the hospital and outpatient clinic that was not observed during this study. Weekend schedules are similar, but vary somewhat to allow interns days off. At Site 2, on-call is a daytime admitting shift beginning at 7 am and ending at 9 pm. Pre-call, short-call, and post-call are daytime shifts beginning at 7 am and ending at 6 pm. Nights is an overnight admitting rotation beginning at 9 pm and ending at 9 am the following day. Weekend schedules are similar, but vary somewhat to allow interns days off.
Interns at site 2 rotate through four general medicine teams and one night float team. A total of 19 interns were approached for participation at site 2, representing 27 % of medicine interns. A convenience sample of intern shifts was chosen based on position in the call cycle on general medicine wards services and night float during the study period. Interns at site 2 were observed for one to four shifts each.
All observed interns were in good standing with their residency program and provided informed consent to participate in the study. The institutional review board (IRB) at Site 1 approved the study; Site 2 deemed it not to be human subjects research.
Observers
Twenty-two trained undergraduate university students served as the observers. All observers collected data at both institutions. We trained observers to collect data without interrupting patient care. Observers learned how to categorize and record the various activities on the observation tool. Observers were tested using the tool while viewing a video of interns engaging in various non-patient care activities, and were only certified to participate in the study once achieving ≥ 85 % concordance rate with the researchers in the mock observation.
Four hours of quality assurance was completed at both institutions during the study. Congruence between observer and research team member was > 85 % for each hour of observation. Observers were assigned to shifts beginning just prior to the intern’s arrival, and observations lasted until the intern left the hospital.
Observation Tool
Observers recorded intern activities using the iPod Touch™ “TimeTracker” application. The application allows observers to track intern time utilization in a variety of activities in real-time, including multitasking. Data collection was anonymous. We categorized activities based on previous studies,7–9 as well as pilot data.
Outcomes
Our primary outcome was time spent in direct patient care. Direct patient care included all activities conducted face-to-face with patients or their families, including bedside rounds, procedures, and family meetings. Secondary outcomes were time spent in indirect patient care, educational activities, and miscellaneous activities. Indirect patient care included viewing patient charts, entering orders, writing notes, speaking with other members of the medical team, engaging in handoffs in care, and transporting patients. Educational activities included non-bedside rounds, conferences, and teaching students. Basic activities included eating, sleeping, walking, and recreational activities. Independent variables included hospital site, gender of intern, shift type, shift length, number of patients admitted during the shift, and number of patients on service.
Data Analysis
Based on the historical studies, we powered our study to enable us to detect a difference of 8 % in our primary outcome between sites (α = 0.05, β = 0.2), by collecting 500 hours of data at each site. We pooled all data to determine the percent of overall time spent in each category and activity. The average amount of time spent with each patient during a particular shift was calculated by aggregating observed time spent in direct patient care divided by number of patients cared for by the intern during the shift. We calculated average time per newly admitted patient for the admitting shifts as the time spent in direct patient care during the initial patient evaluation divided by the number of patients admitted during the shift. Total computer time was calculated as the sum of time spent writing electronic notes, writing orders, reviewing patient charts, and reading.
Raw data were adjusted for intern multitasking. When multitasking occurred, the overlapping time was assigned to the activity more closely related to direct patient care. For example, time spent writing a note while speaking to a patient was recorded by observers as both direct and indirect patient care, and then later recoded as direct patient care, to bias towards our primary outcome.
We used simple (unadjusted linear) regression analysis as well as multilevel regression analysis to test for differences between hospital sites, teams, shifts, and intern gender, after adjusting for clustering at the observer and intern levels. All analyses were performed in Excel 2010 and Stata 11 IC (College Station, TX).
RESULTS
All interns approached agreed to participate. We observed ten interns at Site 1 and 19 interns at Site 2, for a total of 1072 hours at the two institutions. After adjustment for time spent multitasking, a total of 873 hours (439 at Site 1 and 434 at Site 2) of non-overlapping data were analyzed. Twenty-nine percent of this time was during night shifts and 62 % was during admitting shifts. Each intern was observed for an average of 37 hours (range 8–69 hours).
Time Spent by Activity Category
Interns spent a mean of 12 % of their time engaged in direct patient care (Table 1). Admission and follow-up patient evaluations consumed the majority of direct patient care time. Family meetings, patient education, and procedures each took less than 1 % of intern time. Indirect patient care accounted for over 60 % of intern time at both institutions. Talking to other providers, including residents, attending physicians, consultants, and allied health professionals consumed 20 % of total time. Writing admission and progress notes and reviewing the patient’s chart comprised the second and third most time-intensive activities in this category, respectively.
Table 1.
Percent of Time Spent in Each Activity by Site.
| Total | Site 1 | Site 2 | |
|---|---|---|---|
| Total time (hours) | 873 | 439 (50.3 %) | 434 (49.7 %) |
| Activity | |||
| Direct patient care | 12.3 % | 11.4 % | 13.3 %* |
| Initial patient evaluation | 3.8 % | 3.6 % | 4.1 % |
| Follow-up patient visit | 7.2 % | 6.5 % | 7.8 %*† |
| Patient education | 0.1 % | 0.1 % | 0.1 % |
| Family meeting | 0.5 % | 0.4 % | 0.6 % |
| Procedures | 0.7 % | 0.8 % | 0.6 % |
| Education | 14.7 % | 18.8 % | 10.6 %* |
| Educational conferences | 2.3 % | 2.8 % | 1.8 % |
| Reading about medicine | 2.1 % | 2.8 % | 1.3 %*† |
| Rounds | 9.7 % | 12.2 % | 7.3 %*† |
| Teaching students | 0.6 % | 1 % | 0.3 % |
| Indirect patient care | 63.6 % | 61.2 % | 66.1 %* |
| Reviewing patient chart | 14.5 % | 14.7 % | 14.3 % |
| Writing notes | 16.1 % | 13.1 % | 19.1 % |
| Talking with providers | 20 % | 20.5 % | 19.5 % |
| Paperwork | 3.8 % | 1.5 % | 6.1 %*† |
| Writing orders | 6.4 % | 7.3 % | 5.4 % |
| Handoffs | 2.9 % | 4 % | 1.7 %*† |
| Miscellaneous activities | 9.3 % | 8.6 % | 10 % |
| Eating | 1 % | 0.8 % | 1.3 % |
| Social/recreation | 1 % | 2.4 % | 1.7 % |
| Walking | 5.9 % | 5 % | 6.8 %* |
| Sleeping | 0.3 % | 0.3 % | 0.2 % |
* p < 0.05 in unadjusted analysis between Site 1 and Site 2
† p < 0.05 in analysis adjusted for clustering at the intern and observer levels
Patient transport and procedure consent each accounted for less than 0.1 % of time
After indirect patient care activities, education accounted for the second largest amount of intern time. Rounds conducted outside of the patient’s room comprised the largest activity within the education category.
Total computer time represented about 40 % of the intern’s time at both institutions. Overall, 3 % of time was spent in face-to-face handoffs. Interns spent up to 7 % of their time walking, and less than 1 % percent of their time eating, sleeping, and socializing.
Bivariate Analyses
At Site 2, interns spent a significantly larger percent of time in direct patient care, 13.3 % vs. 11.4 %, and indirect patient care, 66.1 % vs. 61.2 %, as well as in follow-up patient visits, completing paperwork, and walking than at Site 1 (Table 2). At Site 1, interns spent a larger proportion of time in educational activities, 18.8 % vs. 10.6 %. A larger proportion of time spent in attending rounds outside the patient’s room at site 1 accounted for the majority of this difference.
Table 2.
Time Spent Per Patient by Shift
| Overall | Site One | Site Two | |
|---|---|---|---|
| Minutes (SD) | Minutes (SD) | Minutes (SD) | |
| Per patient, overall | 7.7 (5.8) | 7.3 (7.0) | 8.0 (4.4) |
| Day admitting shift | 9.9 (7.1) | 11.2 (9.1) | 8.7 (4.5) |
| Night admitting shift | 6.6 (5.6) | 6.8 (6.3) | 6.1 (4.3) |
| Non admitting Shift | 6.7 (4.2) | 4.3 (3.0) | 8.5 (4.1) |
| Per new admission | 16.6 (11.7) | 20.6 (14.4) | 13.6 (8.3) |
| Day admitting shift | 14.6 (9.9) | 24.5 (11.5) | 10.6 (5.6) |
| Night admitting shift | 18.6 (13.3) | 18.5 (15.8) | 18.6 (10.0) |
Adjusted/Multivariable Analyses
Multilevel regression analysis revealed no significant differences between sites in time spent in each activity category after adjusting for clustering at the intern and observer level. Time spent in direct patient care did not differ significantly between interns on day and night shifts, 12.6 % vs. 11.9 %, or between male and female interns, 12.2 % vs. 12.5 %. Interns spent more time in direct patient care on admitting shifts than non-admitting shifts, 12.7 % vs. 11.9 %, (p < 0.01).
Time Per Patient
Interns spent a mean of 7.7 (range 0–39.6) minutes with each patient on their service per day (Table 2). This varied by shift, with more time spent with patients during daytime admitting shifts, such as the long-call and on-call shifts, and less time spent with patients during the coverage shift. Interns spent a mean of 16.6 (range 4.4–54.5) minutes admitting each patient. There was not a significant difference in average time spent with each patient or with each admission between site 1 and site 2.
DISCUSSION
In January of 2012, interns in this study spent a minority of their time, approximately 12 %, in direct contact with patients. Two-thirds of intern time was spent in indirect patient care, including entering orders, consulting with other physicians, writing notes, and reading the patient chart. Interns spent 40 % of their time in front of computer screens, and more time reviewing patient charts than directly engaging patients.
Our study provides a timely multi-center look at how interns spend their time in the hospital. Our methodology mirrored that of previous studies, allowing for comparison between the studies. We included ten times as much observation time as the Lurie and Moore studies7–9 combined, and nearly sixty times as much observation time as the Fletcher study,14 allowing for more precise estimates. We also collected data throughout the call cycle rather than just call nights. We incorporated rigorous observer training and quality control. Our data collection methodology allowed measurement of rapidly changing and simultaneous performance of intern activities. This was necessary for accurate measurements, as discrete intern tasks lasted four minutes on average and 18 % of time was spent multitasking. Direct patient care time was very similar at the two programs, despite very different call schedules and team structure.
Today’s interns spend fewer total hours in the hospital than interns in the pre-2003 ACGME-mandated 80-hour work week.15 They also eat and sleep less in the hospital than in historical studies,7–10 leaving a larger proportion of their time to engage in work and learning activities. Despite this, the percent of time spent directly with patients in this study was less than described in the published literature prior to 2003, and very similar to Fletcher’s results.14 Our findings mirror those from a 2006 national survey of medicine residents, in which the majority of residents reported spending at least 4 hours per day in documentation, and less time in direct patient care.16
Compared with the pre-2003 historical studies, interns in this study spent more time in indirect patient care. The growing volume of data stored on patients likely contributes to the 40 % of time spent in front of computers. This is not inherently undesirable, as the EMR may contain reliable and organized historical information. Likewise, a team approach to caring for patients necessitates more communication, which encompassed 20 % of intern time outside of rounds in this study. While decreasing direct patient care time, it is possible that focusing on these activities improves education and care quality.
We found that interns spent considerable time in education, likely because we followed interns throughout the work week rather than only call nights, when organized educational activities may be missed. Time spent in educational activities varied between the sites as did their rounding routines. The impact of longer non-bedside rounds at Site 1 is not known, as this may contribute to education but may also reduce direct patient care. Interns surveyed by Dresselhaus and colleagues described certain educational activities, such as work rounds, as of lower educational value than time with patients.10
Time spent with each patient varied substantially between interns, and may speak to differences in practice style, patient volume and complexity, the amount of past data in the EMR for a particular patient, or demands of various positions in the call cycle.
Our study was limited to internal medicine interns on inpatient rotations at two academic medical centers in Baltimore. Time allocation may vary by residency programs, by specialty, and during outpatient rotations. Second, using non-medical observers may have decreased precision in our estimates, although we employed rigorous training and quality control. We also accounted for bias by adjusting for clustering at the observer and intern levels in our analysis. Third, we only observed hospital work, and may have missed work performed at home before or after the shift.17 However, this bias is likely conservative, in the direction of increasing estimates of time spent in direct patient care. Fourth, we attempted to limit the Hawthorne effect by training observers to be as unobtrusive as possible and by averaging time allocation across the group of interns. In addition, observed subjects tend to habituate rapidly to being observed.18 Fifth, since we did not collect identifying data on interns, we were not able to identify associations between intern characteristics and time spent in direct patient care. Sixth, we observed interns during a single month, although time spent with patients may vary throughout the year. Seventh, we observed a convenience sample of interns based on rotation and call schedule and a small number of interns at each site. However, all interns approached agreed to participate, and we were able to observe interns throughout the call cycle, enabling a more comprehensive assessment of our outcomes. Eighth, we do not have data from the two institutions observed prior to 2011 to which we can compare our results. Finally, this study did not include data on the quality of doctor–patient interactions.
The goal of residency training is to produce competent physicians capable of practicing independently. To reach the educational milestones needed to demonstrate independence, residents must hone their skills in patient care and communication. As the ACGME common program requirements highlight, “For the resident, the essential learning activity is interaction with patients under the guidance and supervision of faculty members.”1 Prior studies have found that more time spent with patients may improve patient satisfaction, patient education, and clinical outcomes, and reduce inappropriate prescribing.19–22
In the wake of the 2003 and 2011 work hours limitations, the proportion and absolute amount of time spent in direct patient care has dropped in both Fletcher’s study14 and this study. As a result, the total time residents can expect to spend learning from patients appears to have decreased, which may affect the quality of the patient–physician relationship and the quality of care delivered. As programs continue to evolve and adapt to the 2011 work hours regulations, it remains unclear if further decreases in direct care time will occur.
While obtaining patient data from the EMR may be efficient and reliable, computer-based care likely results in less time for patient education and may detract from the doctor–patient relationship. Residency program directors report that documentation requirements may limit educational opportunities.16 Prioritizing direct patient care is necessary to perform Entrustable Professional Activities, a core outcome of achieving independent practice.23,24 Reorganization of resident teams to decrease patient volume and increase focus on teaching and patient-centered care has been shown to increase educational time and decrease indirect patient care time, and improve patient outcomes.25,26 Educators might optimize the efficiency of conferences and rounds to ensure residents are deriving maximal benefit from these sessions.
Several hospital-level strategies might increase time available for direct patient care. Integration of EMR systems to produce automatic summaries of patient histories, and automatic populating of some data fields might improve intern efficiency. Geographic cohorting of patients within the hospital could result in less time spent walking and more time spent with patients. Task shifting could assign some activities to non-physician health care staff.
In conclusion, interns in our study spent a minority of time directly caring for patients, and devoted nearly two thirds of their time to indirect patient care. While interns have reduced hospital shift lengths and total work hours under the 2003/2011 ACGME requirements, intern time is being spent more “productively,” as they sleep and eat less in the hospital. Despite this, interns appear to be spending proportionally less time in direct patient care today than in previous decades. Educators and policymakers should place attention on ways to maximize the amount of time interns are able to spend with patients. Residency programs and the ACGME must determine if the current allocation of intern work time is optimal and allows us to produce internists that are competent and practice patient-centered care.
Acknowledgements
Funding
We would like to acknowledge the Osler Center for Clinical Excellence at Johns Hopkins, as well as the Johns Hopkins Hospitalist Scholars Fund, which funded stipends for our observers as well as transportation and logistical costs of the study.
Prior Presentations
This work was presented as a poster at the Johns Hopkins Institute for Excellence in Education Conference on March 23, 2012.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Common Program Requirements Effective July 1, 2011. Chicago, IL: Accreditation Council for Graduate Medical Education. Available at http://www.acgme.org/acgmeweb/Portals/0/dh_dutyhoursCommonPR07012007.pdf. Accessed January 25, 2013.
- 2.Drolet BC, Spalluto LB, Fischer SA. Residents’ perspectives on ACGME regulation of supervision and duty hours—a national survey. New Engl J Med. 2010;e34:1–4. doi: 10.1056/NEJMp1011413. [DOI] [PubMed] [Google Scholar]
- 3.Drolet BC, Christopher DA, Fischer SA. Residents’ response to duty-hour regulations—a follow-up national survey. N Engl J Med. 2012;366:e35. doi: 10.1056/NEJMp1202848. [DOI] [PubMed] [Google Scholar]
- 4.Mizrahi T. Getting rid of patients: contradictions in the socialization of physicians. New Brunswick, NJ: Rutgers University Press; 1986. pp. 14–30. [Google Scholar]
- 5.Payson HE, Gaenslen EC, Jr, Stargardter FL. Time study of an internship on a university medical service. New Engl J Med. 1961;264:439–43. doi: 10.1056/NEJM196103022640906. [DOI] [PubMed] [Google Scholar]
- 6.Gillanders W, Heiman M. Time study comparison of three intern programs. J Med Educ. 1971;46:142–9. doi: 10.1097/00001888-197102000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Lurie N, Rank B, Parenti C, Woolley T, Snoke W. How do house officers spend their nights? A time study of internal medicine house staff on call. New Engl J Med. 1989;320(25):1673–7. doi: 10.1056/NEJM198906223202507. [DOI] [PubMed] [Google Scholar]
- 8.Parenti C, Lurie N. Are things different in the light of day? A time study of internal medicine house staff days. Am J Med. 1993;94:654–8. doi: 10.1016/0002-9343(93)90220-J. [DOI] [PubMed] [Google Scholar]
- 9.Moore SS, Nettleman MD, Beyer S, Chalasani K, Fairbanks RJ, Goyal M, Carter M. How residents spend their nights on call. Acad Med. 2000;75:1021–4. doi: 10.1097/00001888-200010000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Dresselhaus TR, Luck J, Wright BC, Spragg RG, Lee ML, Bozzette SA. Analyzing the time and value of housestaff inpatient work. J Gen Intern Med. 1998;13(8):534–40. doi: 10.1046/j.1525-1497.1998.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boex JR, Leahy PJ. Understanding residents’ work: moving beyond counting hours to assessing educational value. Acad Med. 2003;78:939–44. doi: 10.1097/00001888-200309000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Chung RS, Ahmed N. How surgical residents spend their training time: the effect of a goal-oriented work style on efficiency and work satisfaction. Arch Surg. 2007;142:249–52. doi: 10.1001/archsurg.142.3.249. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell J, Hayhurst C, Robinson SM. Can a senior house officer’s time be used more effectively? Emerg Med J. 2004;21:545–7. doi: 10.1136/emj.2003.007088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fletcher KE, Visotcky AM, Stagle JM, Tarima S, Weinger MB, Schapira MM. The composition of intern work while on call. J Gen Intern Med. 2012 doi: 10.1007/s11606-012-2120-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jagsi R, Weinstein DF, Shapiro J, Kitch BT, Dorer DJ, Weissman JS. The Accreditation Council for Graduate Medical Education’s limits on residents’ work hours an patient safety: a study of resident experiences and perceptions before and after hours reductions. Arch Intern Med. 2008;168(5):493–500. doi: 10.1001/archinternmed.2007.129. [DOI] [PubMed] [Google Scholar]
- 16.Oxentenko AS, West CP, Popkave C, Weinberger SE, Kolars JC. Time spent on clinical documentation: a survey of internal medicine residents and program directors. Arch Intern Med. 2010;170(4):377–80. doi: 10.1001/archinternmed.2009.534. [DOI] [PubMed] [Google Scholar]
- 17.Mourad M, Vidyarthi A, Hollander H, Ranji S. Shifting indirect patient care duties to after hours in the era of work hours restrictions. Acad Med. 2011;86(5):586–90. doi: 10.1097/ACM.0b013e318212e1cb. [DOI] [PubMed] [Google Scholar]
- 18.Ampt A, Westbrook J, Creswick N, Mallock N. A comparison of self-reported and observational work sampling techniques for measuring time in nursing tasks. J Health Serv Res Pol. 2007;12(1):18–24. doi: 10.1258/135581907779497576. [DOI] [PubMed] [Google Scholar]
- 19.Morell DC, Evans ME, Morris RW, et al. The “five minute” consultation: effect of time constraint on clinical content and patient satisfaction. Br Med J. 1986;292:870–3. doi: 10.1136/bmj.292.6524.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson A, McDonald P, Hayes L, Cooney J. Health promotion in the general practice consultation: a minute makes a difference. Br Med J. 1992;304:227–30. doi: 10.1136/bmj.304.6821.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dugdale DC, Epstein R, Pantilat SZ. Time and the patient–physician relationship. J Gen Intern Med. 2001;14(S1):S34–40. doi: 10.1046/j.1525-1497.1999.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tamblyn R, Berkson L, Dauphinee WD, et al. Unnecessary prescribing of NSAIDs and the management of NSAID-related gastropathy in medical practice. Ann Intern Med. 1997;129:429–38. doi: 10.7326/0003-4819-127-6-199709150-00003. [DOI] [PubMed] [Google Scholar]
- 23.Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system—rationale and benefits. N Engl J Med. 2012;366:1051–56. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 24.Association of Program Directors in Internal Medicine. End of Training EPAs. Available at http://www.im.org/AcademicAffairs/milestones/Pages/EndofTrainingEPAs.aspx. Accessed January 25, 2013.
- 25.McMahon GT, Katz JT, Thondike ME, Levy BD, Loscalzo J. Evaluation of a redesign initiative in an internal-medicine residency. N Engl J Med. 2010;362(14):1304–1311. doi: 10.1056/NEJMsa0908136. [DOI] [PubMed] [Google Scholar]
- 26.Record JD, Rand C, Christmas C, et al. Reducing heart failure readmissions by teaching patient-centered care to internal medicine residents. Arch Intern Med. 2011;171(9):858–9. doi: 10.1001/archinternmed.2011.156. [DOI] [PubMed] [Google Scholar]