ABSTRACT
BACKGROUND
Nonmedical use of prescription psychostimulants such as methylphenidate and amphetamine salts for the purpose of cognitive enhancement is a growing trend, particularly in educational environments. To our knowledge, no recent studies have evaluated the use of these psychostimulants in a medical academic setting.
OBJECTIVE
To conduct an online census of psychostimulant use among medical students.
DESIGN
In 2011, we conducted a multi-institutional census using a 31–48 item online survey regarding use of prescription psychostimulants.
PARTICIPANTS
2,732 actively enrolled medical students at four private and public medical schools in the greater Chicago area.
MAIN MEASURES
Prevalence and correlates of psychostimulant use
KEY RESULTS
1,115 (41 %) of students responded to the web-based questionnaire (range 26–47 % among schools). On average, students were 25.1 years of age (SD = 2.7, range 20–49), and single (70 %). Overall, 18 % (198/1,115) of this medical student sample had used prescription psychostimulants at least once in their lifetime, with first use most often in college. Of these, 11 % (117/1,115) of students reported use during medical school (range 7–16 % among schools). Psychostimulant use was significantly correlated with use of barbiturates, ecstasy, and tranquilizers (Pearson’s correlation r > 0.5, Student’s t-test p < 0.01); male gender (21 % male versus 15 % female, Chi squared p = 0.007); and training at a medical school which by student self-report determined class rank (68 % versus 51 %, Chi-squared p = 0.018). Non-users were more likely to be first year students (Chi-squared p = 0.048) or to have grown up outside of the United States (Chi-squared p = 0.013).
CONCLUSIONS
Use of psychostimulants, including use without a prescription, is common among medical students. Further study of the side effects, medical implications, and use during post-graduate medical training and medical practice is needed to inform evidence-based policy.
KEY WORDS: cognitive enhancement, nootropics, amphetamine salts, methylphenidate, medical students, drug use
INTRODUCTION
Non-medical use of prescription-grade stimulants to enhance cognitive function in healthy adults has attracted national attention from policy makers, educators, researchers, and the general public, and has stimulated much ethical debate surrounding the use cognitive-enhancing substances, also called nootropics, among the healthy.1 These factors along with evidence supporting memory-boosting and attention-boosting properties of prescription-grade stimulants has led to expanding popularity2 of these drugs among educated young adult populations. Recent reviews have identified prescription psychostimulant use as a growing problem in modern prescription drug abuse, with a 5–35 % of college students using psychostimulants for non-medically prescribed purposes,3 with a high proportion of children and young adults obtaining these drugs from off-market sources.4
Prescription-grade psychostimulants are frequently prescribed to treat attention deficit hyperactivity disorder (ADHD) among children, attention deficit disorder (ADD) among adults, narcolepsy, obesity, fatigue, dementia, and hyperactivity.5,6 For individuals with reduced self-regulation and motivation, and difficulties with distraction, task initiation, multitasking and organization, the symptoms seen in ADD, prescription psychostimulants have been shown to improve functioning in daily roles. Within healthy populations, psychostimulants such as amphetamines have also been shown to improve short-term memory,7,8 verbal recall,9 and memory consolidation.10 However, not all effects of psychostimulants are beneficial. Continued use of psychostimulants can lead to increased tolerance for the drugs and psychological dependence,11 although the time period required for such dependence has not been adequately characterized.
Because of the high potential for abuse and dependence,12 psychostimulants are considered controlled substances under the U.S. Controlled Substances Act.13 Widespread use of cognitive-enhancing drugs for non-medically prescribed purposes is a relatively “new” diversion in the United States (U.S.). From 1990 to 1999, a two to five-fold increase in the prevalence of methylphenidate prescriptions was observed in the U.S.3 College students using non-physician directed psychostimulants most often cited non-medical reasons for use, such as to increase concentration (65.2 %), assist with studying (59.8 %), and increase alertness (29.9 %).14 Given this high rate of illicit use, it is not surprising that access to psychostimulants among healthy populations is frequently through off-market sources. A recent survey indicated that 26 % of college students with a prescription for methylphenidate had at least once given or sold some of their medication to others.14 Thus, psychostimulants represent an easily accessible medication that is perceived to improve cognitive performance.
There is much evidence to suggest that medical students in the U.S.15–17 and beyond18–20 may be susceptible to alcohol and drug use. Baldwin et al. in a 1991 study found that 87.5 % of medical students used alcohol and 10 % of medical students smoked marijuana at least once within the previous month.15 This trend appears to continue into residency, with increasing likelihood of both alcohol and illicit drug use after medical school (50 % second year of medical school vs. 65 % during first year residency).21 Recent increases in methylphenidate and amphetamine use among U.S. college students14 and data suggesting that competitive college environments predict increased stimulant use3 lead us to suspect continued stimulant use into medical school and beyond. The June 2009 edition of the Association of American Medical College’s Reporter also highlighted this issue, suggesting that students who used psychostimulants in college are now entering medical schools across the U.S.22
Given these trends, non-prescription psychostimulant abuse potentially represents a prevalent, uncharacterized issue, with major implications for physician competence and conduct.
To our knowledge, no recent studies have evaluated the use of amphetamines, methylphenidate, or other cognitive-enhancing drugs on U.S. medical school campuses. With this in mind, we conducted an online survey of medical students about their use of and attitudes towards stimulant medications.
METHODS
We administered an online, anonymous, cross-sectional survey about cognitive enhancement drug use and associated factors to all enrolled students at four Chicago-area medical schools, one public and three private institutions, henceforth labeled as Schools A through D for institutional privacy. A team of collaborators designed survey items, similar in style to those used in the Monitoring the Future Study (University of Michigan, Ann Arbor, MI23), and piloted them with ten podiatry students.
Sections included demographic profile, substance use, and psychostimulant use. Demographic questions included age, gender, region where the student grew up, marital status, current year in medical school, and type of medical school (i.e., private or public). Substance use questions included frequency of use of coffee, caffeinated soda, caffeine pills, energy bars, energy-boosting pills, energy drinks, and weight loss pills, alcohol (one can or bottle of beer, glass of wine or shot of hard liquor), tobacco (one cigarette or equivalent), barbiturates, cocaine, ecstasy (MDMA), heroin or other opiate, marijuana, LSD or other psychedelic, or tranquilizers. Questions regarding psychostimulant use included “have you ever taken amphetamines or other psychostimulants,” “has a doctor ever prescribed a psychostimulant for you,” timing of first psychostimulant use (elementary school, middle school or junior high, high school, college, medical school or other advanced degree/graduate education), frequency of use in last 30 days, 12 months, and lifetime, preferred type of psychostimulant, whether they had ever given away or sold a psychostimulant that was prescribed to them (if applicable), whether they felt they would be using psychostimulants 5 years from now, and whether they felt their experience would make them more or less likely to prescribe psychostimulants in the future. At the end of the survey, all students were asked, “do you feel that medical students’ psychostimulant use is a problem?” (answers included yes, no or unsure) and “do you think that it is okay for medical students to take psychostimulants to enhance academic performance?” (answers yes, no, or unsure). Additionally, students were given the chance to respond to the open-ended question “please provide additional comments (optional).” Respondents were only required to answer branching questions in the survey; all other questions could remain unanswered.
On average, the survey took between 3 and 7 min to complete among our pilot population. It comprised 48 questions for individuals who had previously used amphetamines and 31 questions for non-users. For protection of student anonymity, the survey did not contain any identifiable data, and a Certificate of Confidentiality was obtained from the National Institute(s) of Health. No questions were worded in a way that might allow investigators to identify a particular student’s responses.
All enrolled students at the participating schools were invited to complete the web-based survey, and all responses were self-reported. Between mid-October and December 2011, each of the designated study site directors sent an e-mail invitation and three follow-up e-mail reminders to medical students at their school. E-mail invitations included a brief explanation of the study; a statement regarding the anonymous nature of survey, which included a summary of the certificate of confidentiality; and a hyperlink to the online survey website. Students were requested not to complete the survey a second time if they had already completed it once. Students were required to complete a modified consent prior to initiating the online survey. The consent form was not linked to the survey itself.
Funding was provided by an educational development fund at School A. Institutional Review Boards at all participating schools approved the study prior to implementation. The Office of Measurement Services (OMS) associated with the University of Minnesota contracted for online hosting of the survey and data analysis. Statistical analyses, including frequencies, Chi squared, Pearson’s correlation coefficients, and Student’s t-tests, were performed using SPSS.
RESULTS
Participants
Total medical student enrollment was 750 for School A, 695 for School B, 530 for School C, and 740 for School D. Of the 2,732 eligible students, 41 % (1,115) responded to the online questionnaire (range 26–47 % among schools). The mean age of respondents was 25.1 years of age (SD = 2.7, range 20–49) and 70 % were single. Overall, approximately half of all respondents were female (52 %). Respondents represented an equal mix of all class years (25 % first year, 56 % female; 28 % second year, 55 % female; 24 % third year, 47 % female; 22 % fourth year, 51 % female; 0.9 % fifth year or beyond, 40 % female). The demographics of the respondents were not significantly different than the overall student enrollment at each school.
Psychostimulant Use
On average, 18 % (198/1,115) of respondents had used psychostimulants, such as amphetamines or methylphenidate, at least once in their lifetime (range 13–26 % among schools). Most often students reported their first experience with psychostimulants in college (57 %, 108/190, eight no response), with the next largest proportion of students reporting first use in medical school (22 %, 42/190), high school (12 %, 23/190), or other professional or graduate school (3 %, 6/190). Of the 198 students who reported ever using psychostimulants, 60 % reported use during medical school, indicating that the overall prevalence of psychostimulant use while in medical school is 11 % (117/1,115; range among schools of 4–17 %, nonsignificant). Frequency of psychostimulant use ranged widely, with 23 % of students (18/78, 39 no response) reporting only one use in the previous 30 days, 54 % of students (42/78) between two and 25 uses in the previous 30 days, 19 % of students (15/78) daily use, and 4 % of students (3/78) reporting 60 to 90 uses in the previous 30 days. Of stimulant users, the median frequency was 10 to 12 separate occasions in the previous 30 days. Preferred psychostimulants were most often amphetamine salts (Adderall©, 75 %) or methylphenidate (Ritalin©, Concerta©, Metadate©, and Methylin©; 41 %), taken by oral ingestion (92 %) and/or inhalation (18 %).
Psychostimulant Acquisition and Reasons for Use
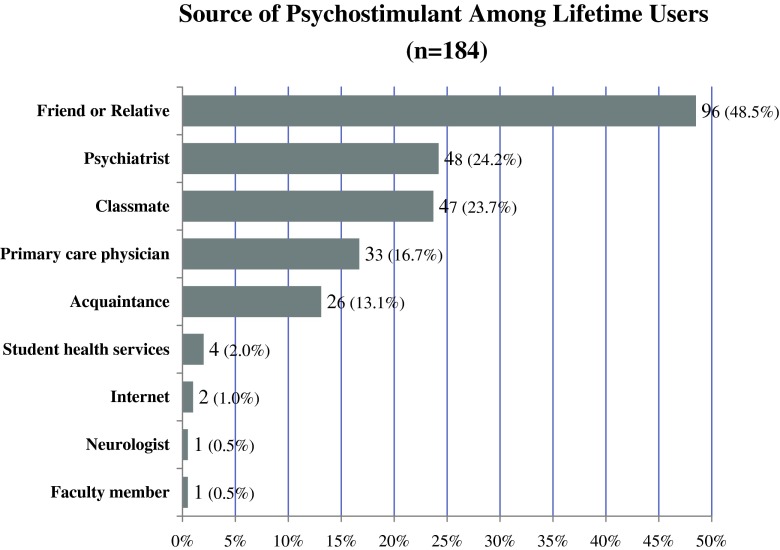
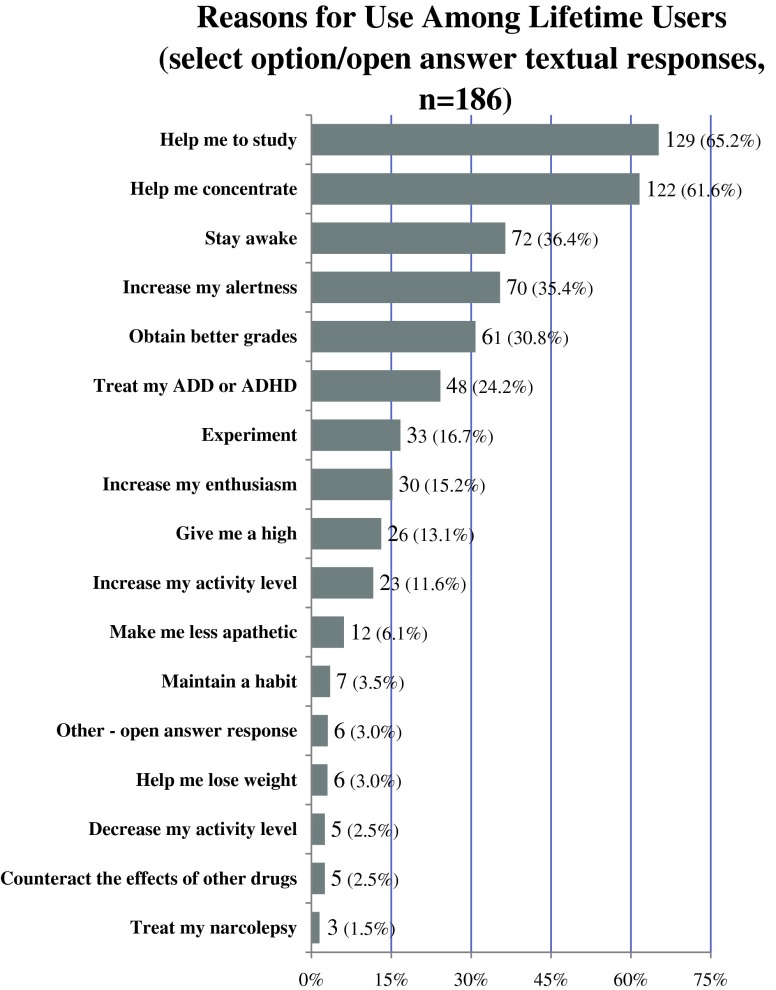
Non-medically prescribed use of psychostimulants was common, with 63 % (123/197, one no response) of students with at least one lifetime use stating that they received their psychostimulant from a friend, relative, classmate or acquaintance (Fig. 1). Of the students who had received a prescription for psychostimulants and responded to the question “have you ever given away or sold a psychostimulant that had been prescribed for you” 23 % (18/77, zero no response) of students reported that they had—at least once—done so. When queried on reasons they used psychostimulants, students most often endorsed using psychostimulants to help them study (69 %) and to aid with concentration (65 %) (Fig. 2).
Figure 1.
Source of psychostimulant acquisition among medical students who have used psychostimulants (n = 184).
Figure 2.
Medical student reasons for psychostimulant use (n = 186). *Total responses represent data from 186 of the 198 eligible students who responded to this survey item. Twelve students declined to answer.
Correlations with Psychostimulant Use
Psychostimulant use was significantly correlated with use of other drugs (Table 1). Lifetime use of psychostimulants was significantly associated with male gender (21 % male (519/1,087) versus 15 % female (568/1,087), Chi squared p = 0.007, 28 no response). Students who mainly grew up outside the U.S. were significantly less likely to report any lifetime psychostimulant use than their U.S.-reared counterparts (outside of U.S. psychostimulant use prevalence = 4 % vs. 20 % U.S. reared; Chi squared p = 0.013). Overall prevalence of psychostimulant use while in medical school was significantly associated with current year in medical school, with first year students being least likely to report use compared to their second, third, fourth and fifth-year colleagues (41 % first year (n = 42/196), 66 % second year (n = 59/196), 60 % third year (n = 52/196), 71 % fourth year (n = 41/196), 50 % fifth year or beyond (n = 2/196); Chi squared p = 0.048, two no response). Students who self-reported attending a school that determined class rank were significantly more likely to respond that they had used psychostimulants while in medical school (class rank assessed 68 % versus no class rank 51 %, Chi squared p = 0.018). Items not significantly correlated with psychostimulant use included age, marital status, estimated class rank (split by quartiles), tobacco use, caffeine intake, or weight loss supplementation.
Table 1.
Moderate-to-Strong Correlations Among Variables Significantly Associated With Drug Use Among Medical Students
| Variable | Pearson’s r | Significance (p) |
|---|---|---|
| Psychostimulants consumed in the past 30 days by… | ||
| Barbiturates consumed in the past year | 0.488 | < 0.001 |
| Ecstasy consumed in the past year | 0.439 | < 0.001 |
| Tranquilizers consumed in the past year | 0.365 | 0.001 |
| Psychostimulants used in the past 12 months | 0.684 | < 0.001 |
| Psychostimulants used in one’s lifetime | 0.576 | < 0.001 |
| Marijuana consumed in the past year by… | ||
| LSD or other psychedelics consumed in the past year | 0.382 | < 0.001 |
| Alcohol consumed in a typical week by… | ||
| LSD or other psychedelics consumed in the past year | 0.95 | 0.002 |
Medical Student Perceptions of Psychostimulant Use
Half of respondents reported that they perceived “psychostimulant use to enhance academic performance” as a problem (50 % perceived as problem, 21 % did not perceive as problem, 28 % didn’t know, < 1 % no response). Sixty-nine percent (772) disagreed with the statement “it is okay for medical students to take psychostimulants to enhance academic performance;” 14 % (158) endorsed the statement as “okay;” and 16 % (81) were unsure (< 1 % no answer).
Of the 198 students who had used psychostimulants, 95 % (177/187, 11 no response) perceived that some improvement in academic standing could be gained by taking psychostimulants. When asked whether their experience with psychostimulants would impact their desire to prescribe psychostimulants for their patients, 16 % (3) said it would make them more likely to prescribe, 23 % (44) said it would make them less likely to prescribe, and 61 % (119) felt unsure. When asked whether they felt that they would be using psychostimulants 5 years from now, the majority 68 % (133) felt that they probably or definitely will not; 17 % (34) felt they probably or definitely will; and 15 % (29) were unsure. When compared to students using psychostimulants, non-users were more likely to report perceiving stimulant use to boost academic performance as a problem, [53 % (481/911) no lifetime use vs. 39 % (76/195) at least one lifetime use, nonsignificant].
DISCUSSION
To our knowledge, this study is the first investigation of cognitive enhancement drug use among U.S. medical students in over two decades. Our results indicate that on average 11 % of medical students sampled use psychostimulants while in medical school. The majority of these students acquire their medications from friends or relatives, and only a minority take these psychoactive substances under the direction of a doctor. These results indicate relatively high use prevalence among these future physicians.
First year students reported significantly lower rates of prescription stimulant use than their second, third, or fourth year colleagues. This may be due to the timing of the survey; with most medical schools starting the year in August, many first-year students may not have had significant interaction with their classmates to have knowledge of these medications. Our data supports this theory, with 22 % of students reporting their first use of these medications in medical school, and an approximately equivalent increase in stimulant use between the first and second year classes (41 % first year to 66 % in second year). Years with standardized testing (USMLE step 1 and USMLE step 2) had the highest reported use of stimulants.
Medical students are at a unique juncture in their medical and professional endeavors. Their pre-medical career takes place in an intensely competitive academic environment, in which many have adapted methods that ensure academic success, such as the use of cognitive-enhancing medications to supplement study habits. Once students enter medical school, additional stresses24–26 to obtain competitive residencies or to maintain high academic performance in an even more competitive environment can reinforce continued drug use by becoming an additional coping mechanism to tackle academic challenges.22,27 This idea is consistent with other literature, which indicates that a highly competitive college environment is predictive of ADD prescription misuse,3 as well as by our findings that the self-reported use of class rank is significantly associated with use of prescription nootropic substances. Mental health may also play a role in stimulant susceptibility, with depression rates among medical students more than double rates seen in the general public (20 % versus 8.7 %).28,29
Paramount in the discussion of stimulant use is the idea of medical safety, as our study results indicate that often these substances are not being used in a best-practice fashion. A high proportion of students gave away or sold these restricted medications to others, indicating that individuals with true contraindications, such as undiagnosed cardiac disease, hyperthyroidism, or mood disorders, may be put at unnecessary risk. Additionally, use was significantly associated with use of recreational drugs.
Mounting literature supports the theory of short-term memory enhancement with prescription stimulant use.30 Similar to the example of steroids among professional athletes, drug-induced cognitive enhancement may be perceived as providing an unfair advantage to some students. While data suggests that amphetamines most benefit memory in individuals with average cognitive functioning, some users actually experience impairment in overall cognition.30 Some argue that the majority of individuals seeking these medications from physicians during college and medical school may have a legitimate medical reason, given that ADD is estimated to affect 3 to 5 % of adults, and only 10 % of affected individuals currently have a diagnosis.31 Certainly for those students, overall performance would be significantly diminished without the appropriate use of these drugs, and there should be caution to avoid stigmatizing them. However, many of these students endorsed being prescribed these stimulants without an actual diagnosis, contrary to current Food and Drug Administration (FDA) guidelines and proper medical practice. Although not assessed, it is likely that side effects are present among this population and may represent another relative contraindication to widespread use.
Psychoactive substance use among medical students represents an unstudied policy concern for the medical profession. In a recent, controversial article in Nature, Greely et. al. advocated the use of cognitive-enhancing drugs by individuals in occupations in which one person’s life is dependent upon another. Specifically, the authors targeted the medical profession, stating that it would be ethically sound to require surgeons to take a drug in order to “save more patients” (p. 703).31 With the controversy regarding work hour restrictions among residents, some have called for the use of a wakefulness-promoting stimulant, modafinil, as an alternative to reduced hospital hours to reduce residency-induced fatigue.32 As the policy making bodies in sports have done to regulate the use of performance enhancing substances, it may be time for the major professional organizations in medicine to do the same. A discussion amongst the AAMC (Association of American Medical Colleges), ACGME (Accreditation Council on Graduate Medical Education), ABMS (American Board of Medical Specialties) and FSMB (Federation of State Medical Boards) would be welcome to examine this issue of nootropic drug use amongst students, residents, and practicing physicians.
This study has several limitations. Given that student’s responses are self-reported and non-medically prescribed stimulant use is illegal, misreporting is a potential concern in this survey. However, the survey did not distinguish between giving away (illegal) or selling (criminal) these drugs. Previous studies have indicated that anonymous self-reported surveys have low misreporting rates.33 The response rate of this investigation is low at 41 %, and little data from non-responders is available, given the anonymous survey design. Our data included sampling of students only in the Chicago area, impacting our ability to generalize about students in other geographic regions or in nonurban settings. However, the individuals who responded are representative of the overall student population at each school, and likely provide good representation of the total medical student population in this geographic area.
This study improves our understanding of nootropic drug use among medical students. Future studies should examine the prevalence and correlates of nootropic use among students in other medical schools, residents and practicing physicians. Monitoring performance under the influence of these substances, in simulations and even in actual patient care, is indicated. There is a growing need for evidence-based policy making among this special population.
Acknowledgements
The authors wish to thank Marina Wolf, Ph.D., Department of Neuroscience, Rosalind Franklin University of Medicine and Science, for her contributions to the study conception and to manuscript preparation, and Holly Geyer, M.D., Department of Internal Medicine, Mayo Clinic, for her contributions to the study conception.
Funding was provided with support from Rosalind Franklin University of Medicine and Science.
Ethical approval has been granted for this study from Institutional Review Boards of all participating schools.
The contents of this article do not represent the views of the Department of Veterans Affairs or the United States Government.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
The contents of this article do not represent the views of the Department of Veterans Affairs or the United States Government. Funding for this project was provided through an educational development fund at Rosalind Franklin University of Medicine and Science.
REFERENCES
- 1.Butcher J. Cognitive enhancement raises ethical concerns. Academics urge pre-emptive debate on neurotechnologies. Lancet. 2003;362(9378):132–3. doi: 10.1016/S0140-6736(03)13897-4. [DOI] [PubMed] [Google Scholar]
- 2.Prescription drug abuse: a fast-growing problem. NIH Medline Plus. 2011;6(3):21.
- 3.Wilens TE, Adler LA, Adams J, et al. Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry. 2008;47(1):21–31. doi: 10.1097/chi.0b013e31815a56f1. [DOI] [PubMed] [Google Scholar]
- 4.Kollins SH. ADHD, substance use disorders, and psychostimulant treatment: current literature and treatment guidelines. J Atten Disord. 2008;12(2):115–25. doi: 10.1177/1087054707311654. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Family Physicians Conditions A to Z. Attention Deficit Hyperactivity Disorder (ADHD) and Attention Deficit Disorder (ADD) 2009.; http://online.statref.com/document.aspx?fxid=99&docid=11. Accessed Feburary 23, 2012.
- 6.Ropper A, Brown R. Adams and Victor’s Principles of Neurology. 8. New York: The McGraw-Hill Publishing Company; 2005. [Google Scholar]
- 7.Zeeuws I, Deroost N, Soetens E. Effect of an acute d-amphetamine administration on context information memory in healthy volunteers: evidence from a source memory task. Hum Psychopharmacol. 2010;25(4):326–34. doi: 10.1002/hup.1120. [DOI] [PubMed] [Google Scholar]
- 8.Soetens E, Casaer S, D’Hooge R, Hueting JE. Effect of amphetamine on long-term retention of verbal material. Psychopharmacology. 1995;119(2):155–62. doi: 10.1007/BF02246156. [DOI] [PubMed] [Google Scholar]
- 9.Zeeuws I, Soetens E. Verbal memory performance improved via an acute administration of D-amphetamine. Hum Psychopharmacol. 2007;22(5):279–87. doi: 10.1002/hup.848. [DOI] [PubMed] [Google Scholar]
- 10.Soetens E, D’Hooge R, Hueting JE. Amphetamine enhances human-memory consolidation. Neurosci Lett. 1993;161(1):9–12. doi: 10.1016/0304-3940(93)90127-7. [DOI] [PubMed] [Google Scholar]
- 11.Porter RS. The Merk Manual Home Health Handbook. In: Porter RS, ed. Amphetamines: Merk; 2011: http://www.merckmanuals.com/home/special_subjects/drug_use_and_abuse/amphetamines.html?qt=amphetamines&alt=sh. Accessed Feburary 23, 2012.
- 12.Volkow ND, Fowler JS, Logan J, et al. Effects of modafinil on dopamine and dopamine transporters in the male human brain: clinical implications. JAMA. 2009;301(11):1148–54. doi: 10.1001/jama.2009.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United States Congress. U.S. Substances Control Act. Vol 84 Stat. 12421970.
- 14.Teter CJ, McCabe SE, LaGrange K, Cranford JA, Boyd CJ. Illicit use of specific prescription stimulants among college students: prevalence, motives, and routes of administration. Pharmacotherapy. 2006;26(10):1501–10. doi: 10.1592/phco.26.10.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baldwin DC, Jr, Hughes PH, Conard SE, Storr CL, Sheehan DV. Substance use among senior medical students. A survey of 23 medical schools. JAMA. 1991;265(16):2074–8. doi: 10.1001/jama.1991.03460160052028. [DOI] [PubMed] [Google Scholar]
- 16.Croen LG, Woesner M, Herman M, Reichgott M. A longitudinal study of substance use and abuse in a single class of medical students. Acad Med. 1997;72(5):376–81. doi: 10.1097/00001888-199705000-00017. [DOI] [PubMed] [Google Scholar]
- 17.Flaherty JA, Richman JA. Substance use and addiction among medical students, residents, and physicians. Psychiatr Clin N Am. 1993;16(1):189–97. [PubMed] [Google Scholar]
- 18.Rai D, Gaete J, Girotra S, Pal HR, Araya R. Substance use among medical students: time to reignite the debate? Nat Med J India. 2008;21(2):75–8. [PubMed] [Google Scholar]
- 19.Kumar P, Basu D. Substance abuse by medical students and doctors. J Indian Med Assoc. 2000;98(8):447–52. [PubMed] [Google Scholar]
- 20.Shyangwa PM, Joshi D, Lal R. Alcohols and other substance use/abuse among junior doctors and medical students in a teaching institute. JNMA. 2007;46(167):126–9. [PubMed] [Google Scholar]
- 21.Newbury-Birch D, Walshaw D, Kamali F. Drink and drugs: from medical students to doctors. Drug Alcohol Depend. 2001;64(3):265–70. doi: 10.1016/S0376-8716(01)00128-4. [DOI] [PubMed] [Google Scholar]
- 22.Harris S. “I Don’t See It as a Problem”: More Medical Students Taking Prescription Stimulants, Few See Cause for Concern. AAMC Reporter. 2009;June Edition.
- 23.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national survey results on drug use, 1975–2011. Annu Vol Trends Drug Use Relat Factors. 2012;2:314. [Google Scholar]
- 24.Dutta AP, Pyles MA, Miederhoff PA. Stress in health professions students: myth or reality? A review of the existing literature. J Natl Black Nurses Assoc. 2005;16(1):63–8. [PubMed] [Google Scholar]
- 25.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354–73. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Dyrbye LN, Thomas MR, Huntington JL, et al. Personal life events and medical student burnout: a multicenter study. Acad Med. 2006;81(4):374–84. doi: 10.1097/00001888-200604000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Webb J, Thomas J, Valaseck M. Contemplating cognitive enhancement in medical students and residents. Perspect Biol Med. 2010;53(2):200–14. doi: 10.1353/pbm.0.0154. [DOI] [PubMed] [Google Scholar]
- 28.Goebert D. Depressive symptoms in medical students and residents: a multi-school study. Acad Med. 2009;84(2):236–41. doi: 10.1097/ACM.0b013e31819391bb. [DOI] [PubMed] [Google Scholar]
- 29.Strine TW. Metropolitan and micropolitan statistical area estimates of depression and anxiety using the patient health questionaire-8 in the 2006 behavioral risk factor surveillance system. Int J Public Health. 2009;54(2):117–24. doi: 10.1007/s00038-009-8026-4. [DOI] [PubMed] [Google Scholar]
- 30.Smith ME, Farah MJ. Are prescription stimulants “smart pills”? The epidemiology and cognitive neuroscience of prescription stimulant use by normal healthy individuals. Psychol Bull. 2011;137(5):717–41. doi: 10.1037/a0023825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greely H, Sahakian B, Harris J, et al. Towards responsible use of cognitive-enhancing drugs by the healthy. Nature. 2008;456(7223):702–5. doi: 10.1038/456702a. [DOI] [PubMed] [Google Scholar]
- 32.Rose SH, Curry TB. Fatigue, countermeasures, and performance enhancement in resident physicians. Mayo Clin Proc. 2009;84(11):955–7. doi: 10.1016/S0025-6196(11)60665-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marsden P, Wright J. Handbook of Survey Research. 2nd ed: Emerald Publishing Group Limited; 2010.