Abstract
AIM: To perform a large-scale retrospective comparison of laparoendoscopic single-site cholecystectomy (LESSC) and three-port laparoscopic cholecystectomy (TPLC) in a single institution.
METHODS: Data were collected from 366 patients undergoing LESSC between January 2005 and July 2008 and were compared with the data from 355 patients undergoing TPLC between August 2008 and November 2011 in our department. Patients with body mass index greater than 35 kg/m2, a history of major upper abdominal surgery, signs of acute cholecystitis, such as fever, right upper quadrant tenderness with or without Murphy’s sign, elevated white blood cell count, imaging findings suggestive of pericholecystic fluid, gallbladder wall thickening > 4 mm, and gallstones > 3 cm, were excluded to avoid bias.
RESULTS: Altogether, 298 LESSC and 315 TPLC patients met the inclusion criteria. The groups were well matched with regard to demographic data. There were no significant differences in terms of postoperative complications (contusion: 19 vs 25 and hematoma at incision: 11 vs 19), hospital stay (mean ± SD, 1.4 ± 0.2 d vs 1.4 ± 0.7 d) and visual analogue pain score (mean ± SD, 8 h after surgery: 2.3 ± 1.4 vs 2.3 ± 1.3 and at day 1: 1.2 ± 0.4 vs 1.3 ± 1.2) between the LESSC and TPLC patients. Four patients required the addition of extra ports and 2 patients were converted to open surgery in the LESSC group, which was not significantly different when compared with TPLC patients converted to laparotomy (2 vs 2). LESSC resulted in a longer operating time (mean ± SD, 54.8 ± 11.0 min vs 33.5 ± 9.0 min), a higher incidence of intraoperative gallbladder perforation (56 vs 6) and higher operating cost (mean ± SD, 1933.7 ± 64.4 USD vs 1874.7 ± 46.2 USD) than TPLC. No significant differences in operating time (mean ± SD, 34.3 ± 6.0 min vs 32.7 ± 8.7 min) and total cost (mean ± SD, 1881.3 ± 32.8 USD vs 1876.2 ± 33.4 USD) were found when the last 100 cases in the two groups were compared. A correlation was observed between reduced operating time of LESSC and increased experience (Spearman rank correlation coefficient, -0.28). More patients in the LESSC group expressed satisfaction with the cosmetic result (98% vs 85%).
CONCLUSION: LESSC is a safe and feasible procedure in selected patients with benign gallbladder diseases, with the significant advantage of cosmesis.
Keywords: Cholecystectomy, Laparoscopy, Single site, Retrospective studies
Core tip: This is a large-scale retrospective randomized study aimed to explore the safety and feasibility of laparoendoscopic single-site cholecystectomy (LESSC) for the treatment of benign gallbladder diseases, compared with three-port laparoscopic cholecystectomy in clinical outcomes. It was found that LESSC is a safe and feasible procedure in selected patients, with the significant advantage of cosmesis.
INTRODUCTION
Laparoendoscopic single-site cholecystectomy (LESSC) has increased in popularity due to its potential cosmetic benefits and faster recovery. It is predicted that this technique may become a standard approach to cholecystectomy[1-3]. The aim of this study was to report our experience in the LESSC with the aid of suture suspension by performing a retrospective comparison with conventional three-port laparoscopic cholecystectomy (TPLC).
MATERIALS AND METHODS
Between January 2005 and November 2011, 366 patients underwent LESSC and 355 underwent TPLC in the Department of Hepatobiliary Surgery, Zhujiang Hospital, Guangzhou, China. Retrospective data were collected from both case notes and the operating theater database.
As the LESSC procedure is a new technique and we have performed TPLC for nearly 15 years at this hospital, to avoid bias, the exclusion criteria for both the LESSC and TPLC groups included patients with a body mass index greater than 35 kg/m2, history of major upper abdominal surgery, signs of acute cholecystitis, such as fever, right upper quadrant tenderness with or without Murphy’s sign, elevated white blood cell count, imaging findings suggestive of pericholecystic fluid, gallbladder wall thickening > 4 mm, and gallstones > 3 cm. This study protocol was approved by the Institutional Review Board of the Second Affiliated Hospital of Southern Medical University, Guangzhou, China in November 2009 (No. ZJYY-2012-GDEK-001). Written informed consent for the procedure was obtained from all patients.
Eligible patients were assigned to the LESSC group (n = 298) and the TPLC group (n = 315). Collected data included patient demographics, intra-operative data about estimated blood loss, intra-operative complications, conversion to multi-port laparoscopic cholecystectomy (LC) or open surgery, and operating time (in all patients and in the last 100 patients in both groups), and postoperative data about length of hospital stay, visual analogue pain score, post-operative complications (contusion: an injury around the port site and bruised skin; hematoma: a localized collection of blood in the port site), total cost (for all patients and for the last 100 patients in both groups) and cosmetic results. The total costs for all procedures in the study were calculated using hospital financial records, which consisted of the cost of operating room usage and hospital ward stay during the perioperative period. Postoperative pain was assessed using a standard visual analogue scale [range, 0 (no pain) to 10 (maximum pain)] at 8 h after surgery and on postoperative day 1. The cosmetic effect was evaluated at the 2-wk follow-up visit, where patients were asked to assess the cosmetic results (satisfied or not very satisfied) by identifying the number and site of scars[4]. All operations were performed by two experienced surgeons who had performed more than 200 LC procedures before this study.
Surgical procedure
LESSC was performed with the help of 2 slings of sutures, and included the following steps.
Under general anesthesia, a single curved intra-umbilical 20-mm incision was made. One 10-mm trocar (Tonglu Kanger Medical Instrument Co., Ltd., Hangzhou, China) was placed to allow the insertion of a 30-degree laparoscope (Olympus, Tokyo, Japan) through the abdomen at the left side of the incision and a 5-mm trocar (Tonglu Kanger Medical Instrument Co., Ltd., Hangzhou, China) was inserted at the right side for the harmonic scalpel (Ethicon Endosurgery, 5 mm, Cincinnati, OH, United States). Tissues between the trocars were preserved to prevent air leakage. The first suture using a straight needle was inserted through the right 7th inter-costal space in the anterior axillary line, and the seromuscular layer of the gallbladder fundus was punctured and retracted toward the anterior abdominal wall. Hartmann’s pouch was punctured and retracted using the second suture to expose Calot’s triangle (Figure 1). A harmonic scalpel was used to dissect Calot’s triangle. Once the cystic artery and duct were exposed, the cystic artery was cut using the harmonic scalpel, and the cystic duct was ligated by three 5-mm titanium clips (Tonglu Kanger Medical Instrument Co., Ltd., Hangzhou, China) and divided. The harmonic scalpel was used to dissect the gallbladder from the gallbladder fossa. The specimen was placed into a specimen bag (TK Medical, Guangzhou, China), and removed through the umbilical incision. The umbilical incision was closed without a drainage tube in place (Figure 2)
Figure 1.
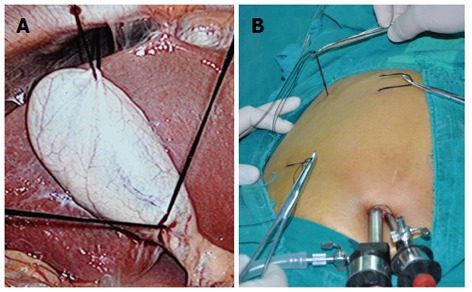
Suture suspension. A: The fundus and Hartmann’s pouch were punctured and retracted by two sutures to expose Calot’s triangle; B: Puncture spot at the superior chest wall along the costal margin in order to draw the liver up a bit more.
Figure 2.
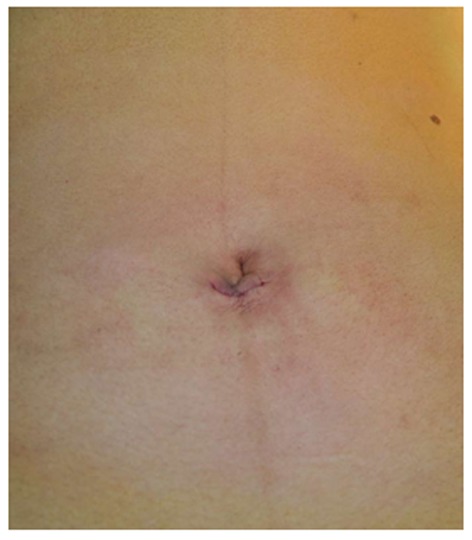
Umbilical incision was closed.
In the TPLC procedure, the same instruments were used as in the LESSC procedure. A sub-umbilical incision, ultimisternal incision and right sub-costal incision were made. A 10-mm trocar was inserted into the sub-umbilical incision to allow introduction of the laparoscope, and another two trocars, a 10-mm and a 5-mm, respectively, were inserted for the grasp and harmonic scalpel. The operation was performed following the routine three-port cholecystectomy procedure[5], however, the cystic artery was divided and cut using the harmonic scalpel instead of being clipped and divided.
Statistical analysis
Statistical analysis was accomplished using the SPSS program for Windows 12.0 (SPSS, Chicago, IL, United States). The χ2 test or t test was used as indicated. The Spearman rank correlation was used to investigate the relationship between operating time and experience. All data were presented as mean ± SD. P < 0.05 was considered statistically significant.
RESULTS
There were no significant differences regarding demographic variables between the two groups (Table 1). In the LESSC group, four patients required additional ports (one or two) to adequately expose Calot’s triangle. There were two conversions to open surgery in each group due to abnormal anatomy. There were no major intra- or post-operative complications such as bleeding, infection and bile leakage, however, LESSC resulted in a higher incidence of intraoperative gallbladder perforation than TPLC (56 cases vs 6 cases, P < 0.001). Overall, there were no significant differences in terms of surgical complications such as contusion (19 cases vs 25 cases, P = 0.4540) and hematoma at incision (11 cases vs 19 cases, P = 0.1790), hospital stay (1.4 ± 0.2 d vs 1.4 ± 0.7 d, P = 1.0000), and visual analogue pain score (8 h after surgery: 2.3 ± 1.4 vs 2.3 ± 1.3, P = 1.0000 and at day 1: 1.2 ± 0.4 vs 1.3 ± 1.2, P = 0.2042) between the LESSC and TPLC groups. LESSC resulted in a longer operating time (54.8 ± 11.0 min vs 33.5 ± 9.0 min, P < 0.0010). However, the operating time in the last 100 cases in the two groups was the same (34.3 ± 6.0 min vs 32.7 ± 8.7 min, P = 0.1589). A correlation was observed between reduced operating time and increased experience, with a Spearman rank correlation coefficient of -0.28.
Table 1.
Demographic data
| LESSC (n = 298) | TPLC (n = 315) | P value | |
| Age (yr) | 41.5 ± 14.0 | 42.3 ± 11.0 | 0.3997 |
| Female/male | 170/128 | 191/124 | 0.3670 |
| BMI (kg/m2) | 23.1 ± 4.0 | 23.5 ± 3.0 | 0.1279 |
| ASA | 1.4 ± 0.1 | 1.4 ± 0.2 | 1.0000 |
| Clinical diagnosis | 0.4530 | ||
| Cholecystolithiasis | 192 | 212 | |
| Cystic polyps | 106 | 103 |
ASA: American Society of Anesthesiology; LESSC: Laparoendoscopic single site cholecystectomy; TPLC: Three-port laparoscopic cholecystectomy; BMI: Body mass index.
The total cost for LESSC per patient was 1933.7 USD compared with 1874.1 USD for the TPLC procedure (1933.7 ± 64.4 USD vs 1874.7 ± 46.2 USD, P < 0.001), and the overall cost of LESSC was approximately 57.8 USD more than the TPLC technique. However, no significant difference was found when the last 100 cases in the two groups were compared (1881.3 ± 32.8 USD vs 1876.2 ± 33.4 USD, P = 0.0571), suggesting that the cost difference was mainly due to the increased operating time.
Most patients were surprised by the reduced number of sites, and more patients who underwent LESSC satisfied with the cosmetic result than those who underwent TPLC (98% vs 85%, P = 0.0010) (Table 2).
Table 2.
Patient outcomes
| LESSC (n = 298) | TPLC (n = 315) | P value | |
| Conversions to open surgery | 2 | 2 | 1.0000 |
| EBL (mL) | 14 ± 6.0 | 15 ± 4.0 | 0.2643 |
| Gallbladder perforation during surgery | 56 | 6 | < 0.001 |
| Operating time (min) | 54.8 ± 11.0 | 33.5 ± 9.0 | < 0.001 |
| Operating time of the last 100 cases (min) | 34.3 ± 6.0 | 32.7 ± 8.7 | 0.1589 |
| VAS (1–10) | |||
| 8 h after surgery | 2.3 ± 1.4 | 2.3 ± 1.3 | 1.0000 |
| Day 1 | 1.2 ± 0.4 | 1.3 ± 1.2 | 0.2042 |
| Complications | |||
| Contusion at incision | 19 | 25 | 0.4540 |
| Hematoma at incision | 11 | 19 | 0.1790 |
| Hospital stay (d) | 1.4 ± 0.2 | 1.4 ± 0.7 | 1.0000 |
| Cosmetic result | 98% | 85% | 0.0010 |
| Total cost (USD) | 1933.7 ± 64.4 | 1874.7 ± 46.2 | < 0.0010 |
| Total cost of the last 100 cases (USD) | 1881.3 ± 32.8 | 1876.2 ± 33.4 | 0.0571 |
EBL: Estimated blood loss; LESSC: Laparoendoscopic single site cholecystectomy; TPLC: Three-port laparoscopic cholecystectomy; VAS: Visual analogue score.
DISCUSSION
Laparoendoscopic single-site surgery has attracted wide attention due to the decreased number of incisions needed and potentially good cosmetic results[6-13]. Recently, more studies have focused on comparing LESSC with multi-port LC and have reached an agreement that LESSC may become the gold standard treatment[14,15]. However, there is still a long way to go before this approach becomes the gold standard treatment as the standardization, safety, and other outcomes of LESSC require further validation[16-19].
Standardization is a prerequisite for clinical popularization of a surgical approach. Approaches to LESSC are technically immature. For example, to expose Calot’s triangle, trials on the use of sutures, Kirschner wires and loop retractors have been reported. The devices used in surgery vary from one surgeon to another: some use common trocars[20,21], some tend to use LESSC multi-ports[22] and others favor self-designed devices such as sterile gloves[23], in addition, there are differences in manipulative instruments such as routine instruments and reticulating instruments[22]. For example, to prevent air leakage, we have tried tri-ports and gel-ports at our center, but discontinued these due to high cost and longer trans-umbilical incision. We have used routine trocars because they are effective in preventing air leakage and are more cost-effective. With regard to surgical instruments, we have tried flexible forceps and laparoscopes, but have finally resorted to suture suspension assisted technology in LESSC, for which only one 30-degree laparoscope and one manipulative instrument are needed, eliminating the clashing of more instruments intra-operatively.
An appropriate method to place the sutures is essential for the operation. To achieve an ideal exposure of surgical site, we choose a puncture site at the superior chest wall along the costal margin so that the suture can draw the liver up a bit more, which is different from view of Piskun et al[23] that the puncture spot should be at the inferior costal margin. In addition, the use of harmonic scalpel is effective in occluding 3-mm blood vessels and dissecting tissues[24]. At our center, the cystic arteries were all cut using the harmonic scalpel, indicating the safety of this scalpel.
In this study, the groups were not randomized or operated on at the same time periods, thus inevitably increasing the risk of bias[25]. For example, TPLC was performed earlier than LESSC at our institution, suggesting a difference in operating experience between LESSC and TPLC. Many patients with signs of acute cholecystitis and other complications successfully underwent TPLC in our institution, but few patients with these complications successfully underwent LESSC during the study period. Therefore, exclusion criteria were applied, where patients with a history of major upper abdominal surgery, signs of acute cholecystitis, and gallstones > 3 cm, were excluded to minimize bias. However, despite the use of selection criteria, this study remains retrospective and was affected by the well-known bias due to this design.
Our results showed that the LESSC technique was more expensive and time-consuming than the TPLC technique. However, the comparisons in the last 100 patients between the two groups demonstrated that these differences were minimized through improvement of surgical skills. Analyses of operating time and total cost demonstrated a relationship between reduced operating time and increased experience, and a relationship between reduced total cost and increased experience. It is concluded that LESSC with the aid of suture suspension will not add a financial burden to the patient if the operator is skilled in this technique.
In conclusion, this large-scale retrospective trial demonstrated that LESSC with the aid of suture suspension is a safe and feasible procedure in selected patients. However, the limitations of the retrospective nature in this study preclude us from drawing a firm conclusion that LESSC is as safe as TPLC in terms of major complications, such as the bile duct injury, and from demonstrating its potential advantages, such as improved result, reduced postoperative pain and patient satisfaction. Therefore, more large-scale and multi-center randomized studies comparing LESSC with multi-port LC are needed to investigate the safety, potential benefits and clinical application of LESSC.
COMMENTS
Background
Recently, surgeons have begun performing laparoscopic cholecystectomy through a single umbilical incision, which is known as laparoendoscopic single-site cholecystectomy (LESSC). The potential benefits of this approach include reduced postoperative pain, improved cosmetic result and earlier return to normal life. Some investigators have predicted that LESSC may become an alternative standard approach for benign gallbladder diseases. However, there are still controversies with regard to its safety and efficiency, although increasing literatures demonstrate that single-incision laparoscopic surgery is a feasible and safe approach. This retrospective study explored the safety and efficiency of LESSC for the treatment of benign gallbladder diseases in selected patients compared with the three-port laparoscopic cholecystectomy (TPLC) in clinical outcomes.
Research frontiers
LESSC has attracted wide attention because of its potential advantages in cosmetic result and faster rehabilitation. However, whether LESSC could be an alternative to multi-port laparoscopic cholecystectomy remains unknown, and therefore it is necessary to compare the clinical outcome of LESSC and multiple-port laparoscopic cholecystectomy in a large cohort.
Innovations and breakthroughs
This is a large-scale retrospective study to explore the safety and efficiency of LESSC for the management of benign gallbladder diseases compared with the TPLC in selected patients.
Applications
LESSC is a safe and effective approach in selected patients with benign gallbladder diseases. LESSC has a better cosmetic benefit than TPLC.
Terminology
LESSC is a complementary approach to laparoscopic cholecystectomy, in which all operating procedures are completed through a single 15-25 mm incision around the navel. However, unlike the traditional multi-port laparoscopic approach, LESSC leaves only a single small scar.
Peer review
The authors have presented for an interesting manuscript in which they retrospectively compare a single incision laparoscopic cholecystectomy vs conventional 3 port cholecystectomy. The main strength of this study is the large simple size of considered groups of patients. The authors have compared the outcomes of interest in a total of 613 eligible patients, 298 in the single incision group (LESSC) vs 315 in the three port group (TPLC). The procedures have been performed by two high experienced surgeons on laparoscopic cholecystectomy who have performed more than 200 laparoscopic cholecystectomy before this study. The authors have evaluated all necessary outcomes and they have accurately described the details of the performed surgical procedures. The study has concluded that LESSC is more expensive than TPLC, it requires longer operating time and it is a safe and feasible procedure in selected patients and in expert hands. Overall, the manuscript is well structured, clear and concise.
Footnotes
Supported by Science and Technology Projects of Haizhu District of Guangzhou, China, No. 2012-cg-26
P- Reviewer Trastulli S S- Editor Gou SX L- Editor A E- Editor Ma S
References
- 1.Emami CN, Garrett D, Anselmo D, Torres M, Nguyen NX. Single-incision laparoscopic cholecystectomy in children: a feasible alternative to the standard laparoscopic approach. J Pediatr Surg. 2011;46:1909–1912. doi: 10.1016/j.jpedsurg.2011.03.066. [DOI] [PubMed] [Google Scholar]
- 2.Jacob DA, Raakow R. Single-port transumbilical endoscopic cholecystectomy: a new standard? Dtsch Med Wochenschr. 2010;135:1363–1367. doi: 10.1055/s-0030-1262419. [DOI] [PubMed] [Google Scholar]
- 3.Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P. Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc. 2012;26:1205–1213. doi: 10.1007/s00464-011-2051-0. [DOI] [PubMed] [Google Scholar]
- 4.Sarli L, Iusco D, Gobbi S, Porrini C, Ferro M, Roncoroni L. Randomized clinical trial of laparoscopic cholecystectomy performed with mini-instruments. Br J Surg. 2003;90:1345–1348. doi: 10.1002/bjs.4315. [DOI] [PubMed] [Google Scholar]
- 5.Trichak S. Three-port vs standard four-port laparoscopic cholecystectomy. Surg Endosc. 2003;17:1434–1436. doi: 10.1007/s00464-002-8713-1. [DOI] [PubMed] [Google Scholar]
- 6.Pan M, Jiang Z, Cheng Y, Xu X, Zhang Z, Zhou C, He G, Xu T, Liu H, Gao Y. Single-incision laparoscopic hepatectomy for benign and malignant hepatopathy: initial experience in 8 Chinese patients. Surg Innov. 2012;19:446–451. doi: 10.1177/1553350612438412. [DOI] [PubMed] [Google Scholar]
- 7.Sajid MS, Ladwa N, Kalra L, Hutson KK, Singh KK, Sayegh M. Single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: meta-analysis and systematic review of randomized controlled trials. World J Surg. 2012;36:2644–2653. doi: 10.1007/s00268-012-1719-5. [DOI] [PubMed] [Google Scholar]
- 8.Garg P, Thakur JD, Raina NC, Mittal G, Garg M, Gupta V. Comparison of cosmetic outcome between single-incision laparoscopic cholecystectomy and conventional laparoscopic cholecystectomy: an objective study. J Laparoendosc Adv Surg Tech A. 2012;22:127–130. doi: 10.1089/lap.2011.0391. [DOI] [PubMed] [Google Scholar]
- 9.Sasaki K, Watanabe G, Matsuda M, Hashimoto M. Original single-incision laparoscopic cholecystectomy for acute inflammation of the gallbladder. World J Gastroenterol. 2012;18:944–951. doi: 10.3748/wjg.v18.i9.944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saad S, Strassel V, Sauerland S. Randomized clinical trial of single-port, minilaparoscopic and conventional laparoscopic cholecystectomy. Br J Surg. 2013;100:339–349. doi: 10.1002/bjs.9003. [DOI] [PubMed] [Google Scholar]
- 11.Lai EC, Yang GP, Tang CN, Yih PC, Chan OC, Li MK. Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Am J Surg. 2011;202:254–258. doi: 10.1016/j.amjsurg.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 12.Wong JS, Cheung YS, Fong KW, Chong CC, Lee KF, Wong J, Lai PB. Comparison of postoperative pain between single-incision laparoscopic cholecystectomy and conventional laparoscopic cholecystectomy: prospective case-control study. Surg Laparosc Endosc Percutan Tech. 2012;22:25–28. doi: 10.1097/SLE.0b013e318242ea44. [DOI] [PubMed] [Google Scholar]
- 13.Trastulli S, Cirocchi R, Desiderio J, Guarino S, Santoro A, Parisi A, Noya G, Boselli C. Systematic review and meta-analysis of randomized clinical trials comparing single-incision versus conventional laparoscopic cholecystectomy. Br J Surg. 2013;100:191–208. doi: 10.1002/bjs.8937. [DOI] [PubMed] [Google Scholar]
- 14.Fronza JS, Linn JG, Nagle AP, Soper NJ. A single institution’s experience with single incision cholecystectomy compared to standard laparoscopic cholecystectomy. Surgery. 2010;148:731–734; discussion 734-736. doi: 10.1016/j.surg.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Vidal O, Valentini M, Ginestà C, Espert JJ, Martinez A, Benarroch G, Anglada MT, García-Valdecasas JC. Single-incision versus standard laparoscopic cholecystectomy: comparison of surgical outcomes from a single institution. J Laparoendosc Adv Surg Tech A. 2011;21:683–686. doi: 10.1089/lap.2011.0047. [DOI] [PubMed] [Google Scholar]
- 16.Vestweber B, Alfes A, Paul C, Haaf F, Vestweber KH. Single-incision laparoscopic surgery: a promising approach to sigmoidectomy for diverticular disease. Surg Endosc. 2010;24:3225–3228. doi: 10.1007/s00464-010-1090-2. [DOI] [PubMed] [Google Scholar]
- 17.Phillips MS, Marks JM, Roberts K, Tacchino R, Onders R, DeNoto G, Rivas H, Islam A, Soper N, Gecelter G, et al. Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg Endosc. 2012;26:1296–1303. doi: 10.1007/s00464-011-2028-z. [DOI] [PubMed] [Google Scholar]
- 18.Joseph M, Phillips MR, Farrell TM, Rupp CC. Single incision laparoscopic cholecystectomy is associated with a higher bile duct injury rate: a review and a word of caution. Ann Surg. 2012;256:1–6. doi: 10.1097/SLA.0b013e3182583fde. [DOI] [PubMed] [Google Scholar]
- 19.Hall TC, Dennison AR, Bilku DK, Metcalfe MS, Garcea G. Single-incision laparoscopic cholecystectomy: a systematic review. Arch Surg. 2012;147:657–666. doi: 10.1001/archsurg.2012.814. [DOI] [PubMed] [Google Scholar]
- 20.Kirschniak A, Bollmann S, Pointner R, Granderath FA. Transumbilical single-incision laparoscopic cholecystectomy: preliminary experiences. Surg Laparosc Endosc Percutan Tech. 2009;19:436–438. doi: 10.1097/SLE.0b013e3181c3f12b. [DOI] [PubMed] [Google Scholar]
- 21.Pan MX, Jiang ZS, Cheng Y, Xu XP, Zhang Z, Qin JS, He GL, Xu TC, Zhou CJ, Liu HY, et al. Single-incision vs three-port laparoscopic cholecystectomy: prospective randomized study. World J Gastroenterol. 2013;19:394–398. doi: 10.3748/wjg.v19.i3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ponsky TA. Single port laparoscopic cholecystectomy in adults and children: tools and techniques. J Am Coll Surg. 2009;209:e1–e6. doi: 10.1016/j.jamcollsurg.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 23.Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A. 1999;9:361–364. doi: 10.1089/lap.1999.9.361. [DOI] [PubMed] [Google Scholar]
- 24.Roberts KE, Solomon D, Duffy AJ, Bell RL. Single-incision laparoscopic cholecystectomy: a surgeon’s initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg. 2010;14:506–510. doi: 10.1007/s11605-009-1116-z. [DOI] [PubMed] [Google Scholar]
- 25.Chow A, Purkayastha S, Aziz O, Pefanis D, Paraskeva P. Single-incision laparoscopic surgery for cholecystectomy: a retrospective comparison with 4-port laparoscopic cholecystectomy. Arch Surg. 2010;145:1187–1191. doi: 10.1001/archsurg.2010.267. [DOI] [PubMed] [Google Scholar]


