Abstract
The V3 loop of the simian immunodeficiency virus (SIV) envelope protein (Env) largely determines interactions with viral coreceptors. To define amino acids in V3 that are critical for coreceptor engagement, we functionally characterized Env variants with amino acid substitutions at position 324 in V3, which has previously been shown to impact SIV cell tropism. These changes modulated CCR5 engagement and, in some cases, allowed the efficient usage of CCR5 in the absence of CD4. The tested amino acid substitutions had highly differential effects on viral infectivity. Eleven of sixteen substitutions disrupted entry via CCR5 or the alternative coreceptor GPR15. Nevertheless, most of these variants replicated in the macaque T-cell line 221-89 and some also replicated in rhesus macaque peripheral blood monocytes, suggesting that efficient usage of CCR5 and GPR15 on cell lines is not a prerequisite for SIV replication in primary cells. Four variants showed enhanced entry into the macaque sMagi reporter cell line. However, sMagi cells did not express appreciable amounts of CCR5 and GPR15 mRNA, and entry into these cells was not efficiently blocked by a small-molecule CCR5 antagonist, suggesting that sMagi cells express as-yet-unidentified entry cofactors. In summary, we found that a single amino acid at position 324 in the SIV Env V3 loop can modulate both the efficiency and the types of coreceptors engaged by Env and allow for CD4-independent fusion in some cases.
Infection of rhesus macaques with simian immunodeficiency virus (SIVmac) induces an immunodeficiency syndrome comparable to AIDS in human patients, although with a more rapid onset (24). Because of the similarities in disease manifestations the infection of macaques with SIV has evolved into one of the most commonly used animal models for human immunodeficiency (HIV) infection in humans. HIV and SIV infection of target cells is mediated by multiple interactions of the viral envelope protein (Env) with the CD4 receptor and a coreceptor (3, 32, 40, 54). All HIV type 1 (HIV-1) strains described to date use the chemokine receptors CCR5 and/or CXCR4 as coreceptors for entry. CCR5 serves also as the major entry cofactor for SIV (7, 14, 26, 29). However, most SIV strains do not enter cells efficiently via CXCR4 (7, 14, 26, 29). In addition to the major coreceptors, many SIV- and HIV-2 strains can also use the alternative coreceptors GPR15 and CXCR6/STRL33 with high efficiency (11, 15, 35, 38). We have shown that SIVmac239 uses human but not rhesus macaque CXCR6/STRL33 for efficient entry, indicating that this receptor may not be important for SIV replication in rhesus macaques (41, 51).
With rare exceptions, all HIV-1 strains require CD4 for entry. Many HIV-2 and SIV strains, however, can infect target cells independently of CD4 via direct interactions with CCR5 or CXCR4 (16, 18, 46, 47). These viruses are thought to harbor partially triggered Envs, which contain multiple amino acid substitutions compared to the CD4-dependent wild-type (wt) virus, leading to the exposure of epitopes that mediate direct binding to a coreceptor (19). As a consequence, CD4-independent viruses can more efficiently infect target cells, such as macaque macrophages, that express low levels of CD4 (2, 34). However, they also exhibit high sensitivity to neutralizing antibodies, which likely recognize epitopes important for coreceptor engagement (17, 27, 30, 44).
The third variable loop (V3 loop) in the HIV Env is the major determinant of coreceptor choice (22, 36, 52, 60). The SIV V3 loop, which shares relatively little sequence homology with its HIV-1 counterpart (Fig. 1A), is also important for viral tropism, although amino acids outside V3 can also determine coreceptor usage (14, 20, 25). A positive net charge of the V3 loop has been associated with CXCR4 usage by HIV-1 (4, 8-10, 20, 23, 53) but does not confer CXCR4 usage to SIV (31). Single amino acid exchanges in the HIV V3 loop can cause a switch from CXCR4 to CCR5 usage and vice versa (10), indicating that specific amino acid residues can impact coreceptor engagement. We previously found that amino acid substitution I324L impaired SIVmac replication in peripheral blood mononuclear cells (PBMC) and CEMx174 cells but still allowed viral spread in the macaque T-cell line 221-89 (25). Thus, single amino acid exchanges that affect usage of specific SIV coreceptors can provide a powerful tool to study their importance for viral replication in vivo (42).
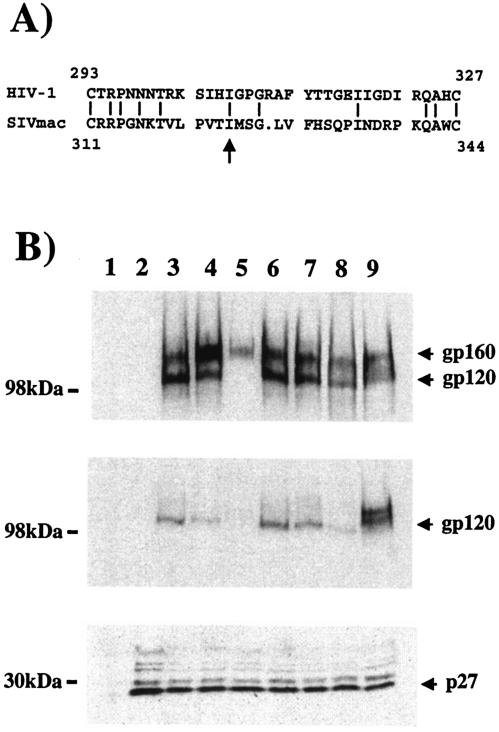
FIG. 1.
(A) Alignment of V3 sequences. An alignment of the V3 sequences of HIV-1 JR-FL (top) and SIVmac239 (bottom) is shown; the arrow indicates amino acid I324. (B) Env expression and virion incorporation. The following SIVmac239 proviral genomes were transiently transfected into 293T cells: mock (lane 1), ΔEnv (lane 2), wt (lane 3), 316Env (lane 4), I324S Env (lane 5), I324V Env (lane 6), I324L Env (lane 7), I324Y Env (lane 8), and I324H Env (lane 9). The transfected cells were lysed and Env expression in lysates was detected by Western blot with the DA6 monoclonal antibody (13) (top panel). Alternatively, viral supernatants normalized for equal amounts of p27 antigen were pelleted, lysed, and Env (middle panel) or p27 (lower panel) incorporation was assessed in parallel by Western blot analysis with DA6 (Env staining) or serum from SIVmac-infected rhesus macaques (p27 staining).
In the present study we more thoroughly investigated the impact of amino acid substitutions at position 324, since this position in the V3 loop appears to play an important role in mediating Env-coreceptor interactions. We show that amino acid 324 can determine CCR5 and GPR15 usage, as well as entry via an unidentified receptor on sMagi reporter cells. Moreover, some amino acid changes at position 324 imparted efficient CCR5 usage in the absence of CD4. Our data suggest an important role of amino acid residue 324 in coreceptor choice, cell tropism, and CD4-independent cell fusion.
MATERIALS AND METHODS
Construction of 324 variants.
The codons for the amino acids 321 and 324 in the SIVmac239 V3 loop were randomly mutagenized by using overlap-extension PCR. The fragments were gel purified and inserted into a SIVmac239 proviral clone as described previously (42). Sequence analysis was used to identify the introduced changes and to verify that the PCR-amplified sequences did not contain undesired mutations.
Cell culture.
J. Overbaugh (Seattle, Wash.) generously provided HeLa-derived Magi (for multinuclear activation of a galactosidase indicator) reporter cells, which express human CD4 in conjunction with CCR5 from pigtail macaques or human GPR15. In addition, sMagi cells were used, which are a derivative of the CMMT cell line, a rhesus macaque mammary tumor line (5). Magi cells contain the gene for β-galactosidase under control of the viral long terminal repeat. All Magi cell lines, as well as 293T and the quail derived QT6 cells, were cultured in Dulbecco modified Eagle medium, 10% fetal calf serum (FCS), glutamine, and antibiotics. CEMx174, C8166, and PM-1 cells were maintained in RPMI 1640 medium containing 10% FCS, glutamine, and antibiotics. 221-89 cells (1) were cultivated in RPMI 1640 medium supplemented with 20% FCS, glutamine, 100 U of interleukin-2 (IL-2)/ml, and antibiotics. PBMC from rhesus macaques were isolated from whole blood by using lymphocyte separation medium. The freshly isolated cells were stimulated with 5 μg of phytohemagglutinin/ml and 50 U of IL-2/ml in RPMI 1640 medium containing 20% FCS, glutamine, and antibiotics for 3 days. Thereafter, the medium was removed, and the cells were maintained in RPMI 1640 medium containing 20% FCS, 50 U of IL-2/ml, glutamine, and antibiotics.
Production of virus stocks and infection of cell lines and PBMC.
Virus stocks were produced by transient transfection of 293T cells as described previously (26). Briefly, 293T cells were transfected with plasmids containing the entire SIVmac239 genome by using a CaPO technique. The culture medium was changed 1 day after transfection, and the culture supernatant was harvested the following day. Residual cells in the supernatants were pelleted, the supernatants were passed through 0.45-μm-pore-size filters and stored at −70°C. The content of viral p27 antigen was quantified by p27 capture enzyme-linked immunosorbent assay obtained from the AIDS Reagent Program. PM-1, CEMx174, C8166, and 221-89 cells and PBMC were seeded in 48-well dishes and infected with equal volumes of viral supernatants containing 5 ng of p27 antigen. PBMC were stimulated for 3 days prior to infection. One day after infection the medium was changed, and culture supernatants were collected in regular intervals and stored at −70°C. The extent of viral replication was determined by using a radioactive reverse transcription (RT) assay as previously described (43). Magi cells were seeded in 48-well dishes and infected with equal volumes of viral supernatants containing 50 ng of viral antigen. The medium was removed 1 day after infection and replaced with fresh Dulbecco modified Eagle medium. Three days after transfection, the cells were lysed and β-galactosidase activity in the cell lysates was determined by using a commercially available kit (Tropix).
RT-PCR analysis of coreceptor expression.
Total cellular RNA was extracted from 1.6 × 107 sMAGI cells by using the RNEasy Mini Kit (Qiagen) according to the manufacturer's instructions. To remove trace genomic DNA contaminations, the RNA was treated with DNase I (Invitrogen). First-strand cDNA was synthesized from this RNA with Superscript II RNase H− reverse transcriptase (Invitrogen) with an oligo(dT) (15) primer (Promega). Reverse transcriptase was omitted from the cDNA synthesis reaction as a negative control. Coreceptor DNA was PCR amplified by using 0.5 μl of cDNA as a template and Platinum Pfx DNA polymerase (Invitrogen) according to the manufacturer's protocol.
Cell-cell fusion assay.
The cell-cell fusion assay was carried out as described previously (48, 49). Briefly, QT6 effector cells were infected with vaccinia virus vTF101 and subsequently transfected with Env expression plasmids. vTF101 harbors the gene for T7 polymerase, which drives Env expression in effector cells. Target cells were transfected with plasmids encoding the viral receptors and luciferase, the latter is expressed under control of the T7 promoter. One day after transfection, effector and target cells were mixed and incubated for 8 h at 37°C. The cocultures were lysed, and the luciferase activity in the lysates determined by using a commercially available kit (Promega).
Entry inhibition by small-molecule coreceptor inhibitors.
One day prior to infection Magi cell lines were seeded in 96-well plates. The cells were preincubated with TAK-779 or AMD 3100 at final concentrations of 5 and 1 μM, respectively, and infected with equal volumes of viral supernatants containing 4 ng of viral p24 antigen. The medium was changed after an overnight incubation and the cells lysed 3 days after infection. The β-galactosidase activity in the lysates was determined by using a commercially available kit (Tropix). Similarly, 221-89 cells were seeded in 96 wells, incubated with TAK-779, and infected with equal volumes of viral supernatants normalized for equal content of p27 antigen. The inhibitor was replenished during the culture, and reverse transcriptase activity in culture supernatants was assessed as described above.
Western blot analysis of Env expression.
293T cells were transiently transfected in T-25 flasks, the medium was changed 12 to 16 h after transfection and cells were harvested 48 h after transfection. The cells were rinsed with phosphate-buffered saline and lysed in sodium dodecyl sulfate sample buffer. Expression of Env in lysates was detected by immunoblotting with DA6 anti-Env antibody (13) at a dilution of 1:2,000. Virion incorporation of Env and p27 antigen was assessed by pelleting equal volumes of viral supernatants normalized for p27 content by enzyme-linked immunosorbent assay. The pelleted virus particles were lysed as described above, and Env and p27-antigen were detected by immunoblotting with DA6 or serum from SIV-infected macaques (p27-staining) at a 1:2,000 dilution.
RESULTS
Generation and characterization of viral variants with single amino acid substitutions at position 324
The amino acid residue isoleucine 324 in the SIVmac239 V3 loop has previously been shown to impact cell tropism and was therefore selected for detailed analysis (25). Notably, 23 of 29 HIV-1 V3 sequences (79%) analyzed in a previous study (39) also contained an isoleucine at the corresponding position, suggesting that this residue is to some degree conserved between HIV-1 and SIV and therefore likely to be important for Env function (Fig. 1A). The codon for amino acid 324 in a SIVmac239 proviral clone was randomly mutagenized, and coreceptor usage of the resulting viral variants was analyzed by infection of different Magi cell lines (Table 1). CCR5 and GPR15 usage was investigated by infection of HeLa cell-derived Magi cell lines stably expressing human CD4 in conjunction with CCR5 from macaques or GPR15 of human origin. Entry of the wt virus into these cells was readily detectable, whereas parental CD4-positive, coreceptor-negative Magi cells did not support SIV infection (Table 1 and data not shown). Infection of the rhesus macaque-derived simian Magi (sMagi) cell line was also analyzed. This macaque mammary tumor cell line was engineered to stably express human CD4 and is readily infectable by SIV and some HIV-2 strains (5). However, it is unknown which coreceptor(s) mediates viral entry.
TABLE 1.
Analysis of SIVmac239 variants with substitutions of isoleucine 324a
| aa exchange | Mean coreceptor usage ± SD
|
Replicationb
|
Group | ||||||
|---|---|---|---|---|---|---|---|---|---|
| R5mne | GPR15hu | sMagi | rhPBMC | 221-89 | CEMx174 | C8166 | PM-1 | ||
| I | 100 | 100 | 100 | ++ | ++ | ++ | ++ | ++ | wt |
| K | 0.5 ± 0.1 | 2.0 ± 0.5 | 1.4 ± 0.2 | − | − | − | − | − | I |
| R | 0.8 ± 0.3 | 0.6 ± 0.3 | 1.2 ± 0.9 | − | +, dd | − | − | − | I |
| S | 0.4 ± 0.1 | 1.7 ± 0.2 | 1.1 ± 0.2 | − | − | − | − | − | I |
| V | 149.5 ± 53.4 | 83.4 ± 23.5 | 134.2 ± 38.5 | ++ | ++ | ++, d | ++, d | ++ | II |
| C | 9.9 ± 1.5 | 4.2 ± 0.3 | 3.1 ± 0.2 | +, d | ++, dd | ++, d | ND | +, d | III |
| E | 4.1 ± 0.8 | 5.7 ± 1.1 | 7.6 ± 1.4 | (+) | ++ | − | ND | +, d | III |
| Y | 1.4 ± 0.6 | 0.9 ± 0.1 | 1.7 ± 0.7 | ++, dc | +, d | − | ++, dd | − | III |
| H | 2.2 ± 0.3 | 5.2 ± 1.2 | 2.2 ± 1.0 | − | ++ | − | ND | ++, d | IV |
| N | 1.2 ± 0.1 | 4.6 ± 0.5 | 3.7 ± 0.7 | − | ++ | − | ND | +, d | IV |
| P | 1.7 ± 0.21 | 4.7 ± 0.8 | 4.1 ± 0.5 | − | ++ | +, d | ND | +, d | IV |
| W | 1.3 ± 0.1 | 5.5 ± 0.9 | 4.2 ± 0.7 | − | ++, d | − | ND | +, d | IV |
| F | 49.5 ± 5.4 | 27.6 ± 1.7 | 193.3 ± 47.7 | ++, dd | ++, d | ++, dd | ++, dd | +, dd | V |
| L | 19.1 ± 2.6 | 17.1 ± 1.7 | 260.3 ± 6.9 | − | ++, d | − | ++, dd | (+), dd | V |
| M | 11.8 ± 1.2 | 22.1 ± 2.6 | 384.2 ± 40.5 | − | ++, d | ++, d | ND | +, d | V |
| T | 33.1 ± 3.6 | 9.5 ± 1.9 | 113.4 ± 12.4 | ++, dd | ++ | − | (+), dd | ++ | V |
The results of a representative experiment are shown; comparable results were obtained in an independent experiment. aa, amino acid. Coreceptor usage and replication are shown relative to 239wt activity.
Peak reverse transcriptase activity: 60 to 100%; ++; 30 to 60%, +; 10 to 30%, (+), <10%, −; d, peak in reverse transcriptase activity 3 to 6 days delayed; dd, peak in reverse transcriptase activity more than 6 days delayed; ND, not done.
Result obtained with PBMC from one of four donor animals tested.
Replication of the 324 variants was also assessed in rhesus macaque (rh) PBMC and cell lines known to be permissive for SIVmac239. The coreceptor expression pattern of these cell lines has been characterized in previous studies. The human T/B hybrid cell line CEMx174 and the human T-cell line C8166 express CXCR4 and GPR15 but not CCR5 (11, 15, 26), whereas rhPBMC, 221-89, and PM-1 cells express CCR5 (S. Pöhlmann and R. W. Doms, unpublished data) (15, 28), probably in conjunction with alternative cofactors.
Random mutagenesis of amino acid 324 yields viral variants with marked differences in coreceptor utilization and cell tropism.
We investigated the impact of substitutions at amino acid position 324 on viral entry and replication. Random mutagenesis of this amino acid yielded 15 viral variants. The effects of these amino acid substitutions on virus entry and replication were highly differential and resulted in the identification of five functional groups (Table 1). The viral variants summarized in group I harbor amino acid changes that either severely diminished or abolished replication in all cell lines tested and reduced entry into reporter cells close to background levels (Table 1). Group II contained a single variant, I324V, which exhibited similar activity as the wt virus (Table 1).
Replication-competent viral variants that entered CCR5, GPR15, or sMagi cells with <10% of wt efficiency form functional groups III and IV (Table 1). The amino acid changes I324C, -E (borderline in replication), and -Y, comprising group III, surprisingly preserved the ability to replicate in macaque PBMC and 221-89 cells (Table 1); however, I324Y replication was limited to PBMC from one of the four donor animals tested. Conversely, the amino acid substitutions I324H, -N, -P, and -W, comprising group IV, abolished replication in macaque PBMC but still allowed efficient viral spread in 221-89 cells (Table 1). The readily detectable replication of the variants of group III and IV in PBMC or immortalized T cells suggest that the efficiency of CCR5 usage in infectivity assays does not necessarily predict the efficiency of SIV spread in macaque T cells. Group V comprises variants that exhibited reduced entry into CCR5- or GPR15-expressing cells but infected sMagi cells more efficiently than the wt virus (Table 1). For instance, entry of the I324L variant into CCR5- or GPR15-expressing Magi cells was at least 80% reduced compared to the wt virus, and replication of this variant was limited to 221-89 and C8166 cells (Table 1). However, the I324L variant infected sMagi cells more efficiently than the wt virus, suggesting that entry was mediated by one of the known alternative coreceptors or an as-yet-unidentified coreceptor.
Finally, we assessed whether amino acid changes at position 324 impact Env processing and virion incorporation. To this end, 293T cells were transfected with proviral genomes of viral variants representing all functional groups, and Env expression and virion incorporation were assessed as described in Materials and Methods. With the exception of I324S, all glycoproteins tested were expressed efficiently in transfected cells and were incorporated with roughly comparable efficiencies into viral particles (Fig. 1B). Only small amounts of uncleaved I324S glycoprotein were observed in cell lysates, and no Env was detected in I324S virions despite normal p27 content, indicating that the I324S mutation inhibited Env processing (Fig. 1B). These results suggest that the amino acid substitutions summarized in functional group I might affect Env expression and thereby render viral particles noninfectious. No evidence was obtained, however, that the amino acid changes summarized in functional groups II, III, IV, and V significantly impact Env expression, indicating that their effects on infection and replication truly reflect alterations in Env function.
Amino acid exchanges at position 324 in SIV Env modulate CCR5 engagement.
The variants I324Y, I324H, and I324L, which represent functional groups III, IV, and V, were unable to use CCR5 efficiently in infectivity assays but still showed robust replication in certain cell lines (Table 1). We analyzed whether these mutations impact CCR5 engagement in a vaccinia virus-based cell-cell fusion assay (Fig. 2A) (48). The env genes of 239wt and the I324Y, I324H, and I324L variants were cloned into pcDNA3 and transiently expressed on quail QT6 cells. The Env-expressing cells were mixed with QT6 cells transiently expressing CD4 and CCR5, and fusion of effector and target cells was quantified. Under these conditions the I324Y and I324H Envs mediated fusion via CCR5 with similar efficiencies compared to 239wt, whereas the I324L mutation diminished fusion to ca. 20% relative to 239wt (Fig. 2A). Thus, these V3 mutations greatly diminished CCR5 usage in the context of virion-associated Env but had a less-profound effect on CCR5 usage in a sensitive cell-cell fusion assay, in which high levels of Env and coreceptor are expressed.
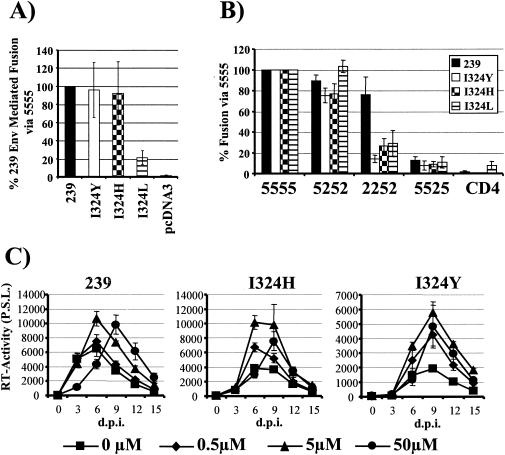
FIG. 2.
Amino acid substitutions at position 324 modulate CCR5 engagement. (A) Usage of wt CCR5 for cell-cell fusion. Effector cells were transiently transfected with the indicated Env expression plasmids and infected with vaccinia virus encoding T7 polymerase. Target cells were transfected with rhesus macaque CD4, human CCR5, and an expression plasmid encoding luciferase under control of the T7 promoter. Effector and target cells were mixed, and luciferase production, indicating cell-cell fusion, was quantified. The average ± the standard error of the mean (SEM) of three independent experiments carried out in triplicates is shown. (B) Usage of CCR5/CCR2 chimeric receptors for cell-cell fusion. The fusion assay was carried out as described above; however, the indicated CCR5/CCR2 chimeras were used as coreceptors. The average ± the SEM of four independent experiments carried out in triplicates is presented. (C) Impact of CCR5 inhibition on replication in T cells. The macaque T-cell line 221-89 was incubated with the indicated concentrations of the small-molecule inhibitor TAK-779 and infected with 5 ng of either SIVmac239wt or the I324Y and I324H variants. Inhibitor was replenished during cultivation, and reverse transcriptase activity in the culture supernatants was assessed. The average ± the SEM of three experiments performed in parallel is indicated.
To investigate whether the 239wt Env and the V3 variants used CCR5 differently, we tested their ability to use chimeras between the CCR5 and CCR2 receptors (49) as coreceptors for fusion (Fig. 2B). Although CCR5 is the major SIV coreceptor, the structurally related CCR2 cannot be used by SIV Env for efficient membrane fusion. The exchange of the first and third extracellular loops between CCR5 and CCR2 (chimera 5252) did not significantly impact engagement of this receptor by the wt and the mutant Envs, whereas the exchange of the second variable loop (chimera 5525) greatly diminished fusion of all Envs tested. In contrast, the introduction of the second extracellular loop of CCR5 into the CCR2 receptor was sufficient for engagement of this receptor by 239wt Env but not by the I324Y, I324H, and I324L Envs. Thus, the V3 variants seem to use CCR5 differently than the wt Env, being more susceptible to perturbations in CCR5 sequence and/or structure.
Env proteins that bind to CCR5 efficiently are less susceptible to inhibition by small-molecule CCR5 inhibitors than Env variants that elicit relatively weak binding to CCR5 (45). Therefore, the differential CCR5 utilization by the 239wt, I324Y, and I324H Envs might result in differential susceptibilities to the small-molecule CCR5 inhibitor TAK-779. We addressed this question by assessing replication of the respective viral variants in 221-89 cells in the presence of the indicated concentrations of TAK-779. 221-89 cells express CCR5 (Pöhlmann and Doms, unpublished), probably in conjunction with alternative cofactors. Generally, the addition of TAK-779 had only moderate effects on viral replication; in fact, the addition of drug seemed to increase virion production to some extent (Fig. 2C). At a concentration of 50 μM, TAK-779 delayed peak replication of the 239wt virus and the I324H variant but not of the I324Y variant (Fig. 2C). In contrast, the same concentration of TAK-779 reduced cell-cell fusion with target cells, which only express the CD4 and CCR5 receptors, between 10 (239wt) and 100-fold (I324Y) (data not shown). Thus, either replication of the I324Y variant in 221-89 T cells does not significantly depend on CCR5 or ligand binding to CCR5 on cell lines does not adequately reflect ligand interaction with CCR5 on T cells.
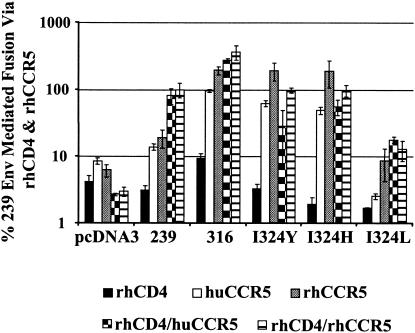
Amino acid 324 can confer CD4-independent cell-cell fusion.
SIVmac239 requires CD4 for the infection of target cells. During the course of SIV infection of macaques viral variants can arise that infect cells expressing low levels or no CD4 that do not typically support efficient virus infection (2, 33, 34). The ability to directly engage CCR5 in the absence of CD4 and to infect macrophages in vitro has been associated with specific amino acid changes in the viral Env protein (33, 44). We addressed the question of whether amino acid changes at position 324 modulate the requirement of CD4 for cell-cell fusion. Fusion via rhesus macaque and human CCR5 was assessed in the presence or absence of CD4 (Fig. 3). Although the 239wt Env required both CD4 and CCR5 for optimal fusion, the CD4-independent 316 Env mediated efficient fusion in the absence of CD4. In agreement with previous results, 316 used CCR5 of rhesus macaque origin more efficiently for CD4-independent fusion than human CCR5. The I324Y and I324H Envs were also capable of using CCR5 for efficient fusion in the absence of CD4, with rhesus macaque CCR5 allowing higher levels of fusion than did human CCR5 (Fig. 3). In contrast, fusion mediated by the I324L Env was generally more CD4 dependent. No efficient cell-cell fusion was measured when control effector cells were transfected with pcDNA3, confirming that fusion was indeed driven by the Env proteins tested. Finally, we investigated whether CD4-independent fusion of the 324 Env variants correlated with efficient infection of primary macrophages by the respective viral variants. Both the I324H and I324Y variants did not infect human macrophages appreciably (data not shown). Infection of the I324L variant was detectable; however, replication of the I324L variant in rhesus macaque macrophages was inefficient compared to the macrophage-tropic 316 variant (data not shown). Thus, some amino acid substitutions at position 324 can confer CD4 independent fusion; however, they are not sufficient to allow efficient replication in macrophages.
FIG. 3.
Amino acid 324 can confer CD4-independent cell fusion. The ability of 239wt Env and the I324Y, I324H, and I324L Envs to mediate fusion via human and rhesus macaque CCR5 in the presence or absence of rhesus macaque CD4 was assessed in a cell-cell fusion assay as described in the legend to Fig. 2. The results from a representative experiment carried out in triplicate is shown, with error bars indicating the standard deviation. Comparable results were obtained in two different experiments.
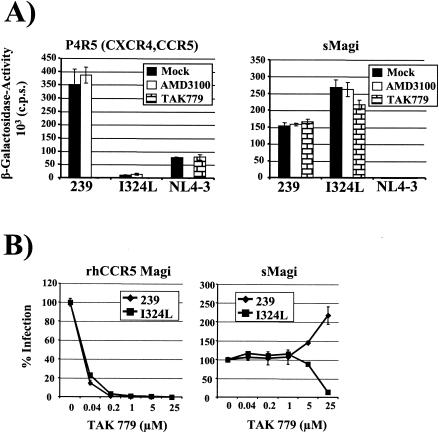
Evidence that entry into sMagi reporter cells is mediated by as-yet-unidentified cofactors.
To further explore the effects of amino acid exchanges at position 324 on coreceptor engagement, we investigated the determinants of SIV entry into sMagi cells a derivative of a rhesus macaque mammary tumor cell line (CMMT) engineered to express human CD4 (5). The I324L variant, as well as the other variants summarized in functional group V, did not replicate in rhPBMC nor use CCR5 or GPR15 efficiently in infectivity experiments but infected sMagi reporter cells with higher efficiency than the wt virus (Table 1).
We first explored whether entry into sMagi cells depends on CCR5 or CXCR4. HeLa cell-derived P4R5 Magi cells, which express human CD4, CCR5, and CXCR4, and sMagi cells were infected with SIVmac239wt, the SIVmac239 I324L variant, and the X4-tropic HIV-1 clone NL4-3 in the presence or absence of small-molecule coreceptor inhibitors (Fig. 4A). TAK-779 blocks entry via CCR5 and AMD3100 inhibits infection via CXCR4. SIVmac239 entered P4R5 cells with high efficiency, whereas entry of the I324L variant was ∼15-fold reduced. The infection of both viruses was abolished by TAK-779, whereas AMD3100 had no appreciable impact on infection efficiency. Finally, AMD3100 but not TAK-779 efficiently blocked NL4-3 entry into P4R5 cells (Fig. 4A). In contrast to the results obtained with P4R5 cells, the I324L variant entered sMagi cells more efficiently than the wt virus, and the entry of both viruses was not efficiently blocked by TAK-779 or AMD3100. In agreement with published data, the infection of sMagi cells with HIV-1 NL4-3 did not result in appreciable induction of reporter gene activity (5).
FIG. 4.
Coreceptor determinants for SIV entry into sMagi cells. (A) Inhibition of infection by small-molecule inhibitors. P4R5 reporter cells expressing human CD4, CCR5, and CXCR4 and sMagi cells were infected with the indicated p24/p27-normalized virus stocks in the presence or absence (Mock) of the CCR5 inhibitor TAK-779 (5 μM) or the CXCR4 inhibitor AMD3100 (1 μM). The β-galactosidase activity as a readout for infection was determined 3 days later. The results of a representative experiment are shown, and similar results were obtained in an independent experiment. (B) Inhibition of entry into sMagi cells by different concentrations of TAK-779. rhCCR5 Magi cells, which express human CD4, together with pigtailed macaque CCR5, and sMagi cells were infected as described above. Similar results were obtained in an independent experiment.
To further characterize the role of CCR5 in the SIV infection of sMagi cells, we performed inhibition studies with different doses of TAK-779 (Fig. 4B). Blocking of sMagi infection was compared to the inhibition of infection of HeLa cell-derived rhCCR5 Magi cells, which express human CD4 in conjunction with pigtailed macaque CCR5. The amino acid sequences of pigtailed and rhesus macaque CCR5 are identical. Whereas nanomolar concentrations of TAK-779 efficiently blocked rhCCR5 Magi infection by 239wt and the I324L variant, infection of sMagi cells was not readily reduced by the same concentrations of inhibitor (Fig. 4B). However, at the highest concentration examined, TAK-779 reduced infection by the I324L variant ∼10-fold but enhanced entry of SIVmac239 ∼2-fold, suggesting that both viruses enter sMagi cells via different receptors or engage the same receptor differentially.
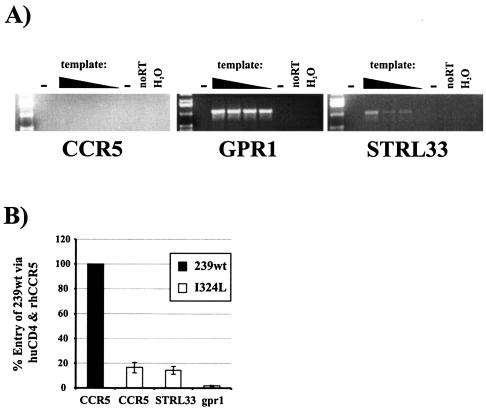
RT-PCR analysis was performed to investigate whether sMagi cells express known SIV coreceptors. Total RNA from sMagi cells was prepared, DNase treated, and diluted as shown, and coreceptor sequences were PCR amplified (Fig. 5A). No signal was detected when primers specific for APJ, CCR8, CXCR4, and GPR15 were used, although these primers efficiently amplified the coreceptor sequences when plasmid DNA was used as a template (data not shown). A faint signal was detected for CCR5, suggesting that sMagi cells might express small amounts of this receptor (Fig. 5A). In contrast, a strong signal for GPR1 was observed even at the highest template dilution, suggesting that the sMagi cells express high levels of GPR1. Amplification of CXCR6/STRL33 also yielded readily detectable bands; however, their intensity diminished upon template dilution.
FIG. 5.
Coreceptor expression in sMagi cells and coreceptor usage of the I324L variant. (A) Analysis of coreceptor expression in sMagi cells. Total RNA was prepared from sMagi cells, DNase treated, diluted as indicated, and subjected to RT-PCR analysis with primers specific for the indicated coreceptors. (B) Coreceptor usage of the I324L variant. 293T cells were transiently cotransfected with human CD4 and the indicated coreceptors of rhesus macaque origin. The transfected cells were infected with 50 ng of the indicated luciferase reporter viruses and luciferase activity quantified. The results are shown relative to SIVmac239 entry via CD4 and CCR5 and similar results were obtained in an independent experiment.
Finally, we investigated whether entry via CCR5, CXCR6/STRL33, and GPR1 could account for the efficient infection of sMagi cells by the I324L variant. The indicated coreceptors of rhesus macaque origin, along with human CD4, were cotransfected into 293T cells, and the cells were infected with replication-competent luciferase reporter viruses. Infection of CD4- and CCR5-expressing target cells by the wt virus was highly efficient (>30,000 counts/s [luciferase activity]), whereas CD4-transfected control cells were resistant to infection (5 counts/s [luciferase activity]) (Fig. 5B). Compared to entry of 239wt into CD4- and CCR5-expressing cells, the I324L variant infected target cells expressing CD4 and one of the indicated coreceptors with at least fivefold reduced efficiency (Fig. 5B). Thus, CCR5, CXCR6/STRL33, and GPR1 are unlikely to mediate the highly efficient entry of the I324L variant into sMagi cells.
DISCUSSION
We investigated the impact of multiple changes at a single amino acid position in the V3 loop of SIVmac239 on CD4 dependency, coreceptor choice, mode of coreceptor engagement, and cellular tropism. Our analysis focused on amino acid 324, a residue we had previously found to impact viral tropism (25). Analysis of viral variants harboring changes at this position revealed that residue 324 can not only determine cellular tropism by modulating coreceptor choice but can also impart efficient coreceptor usage in the absence of the primary receptor CD4. Moreover, our findings suggest that as-yet-unidentified coreceptors can allow efficient SIV entry into some cell lines. Such coreceptors might facilitate SIV infection of certain tissues in vivo. Thus, we demonstrate that the SIVmac V3 loop, similar to its counterpart in HIV-1 Env, plays a critical role in Env-coreceptor interactions and that V3 sequences can mediate CD4-independent coreceptor engagement, a function previously believed to require amino acid exchanges in multiple domains of SIVmac239 Env (33).
Random mutagenesis of position 324 yielded SIV variants that differed widely in replicative capacity, infectivity, and coreceptor choice. In contrast, mutagenesis of position 321, which is known to modulate usage of GPR15 (42), yielded either viral variants with reduced GPR15 usage or variants with wt properties (data not shown). These findings, along with previous studies (25), suggest that whereas single amino acid changes in SIVmac V3 frequently impact cellular tropism and choice of alternative coreceptors, only a few can dramatically alter CCR5 usage, highlighting the robust interaction of Env with CCR5. Thus, the multiple effects of the 324 exchanges on CCR5 and CD4 engagement indicate that this amino acid resides in a position critical for Env interaction with viral receptors.
Notably, not all mutations that strongly reduced usage of macaque CCR5 in an infectivity assay abolished replication in primary cells. Thus, entry of variants I324C and Y into a CCR5-expressing cell line was at least 90% reduced compared to the wt virus, but both variants still replicated to some extent in PBMC. These data suggest that the Env CCR5 interaction tolerates perturbations to some degree without severe reduction of viral spread in primary cells. A similar result has been documented for an HIV-1 variant resistant to a small-molecule CCR5 inhibitor (59). This virus replicates efficiently in PBMC in a CCR5-dependent fashion; however, entry into a CCR5 expressing CD4-positive cell line is severely reduced. Alternatively, the I324C and Y variants might engage alternative cofactors for replication in PBMC. Notably, spread of the I324Y variant in the T-cell line 221-89, which was derived from herpesvirus saimiri immortalized macaque PBMC, was not blocked by a small-molecule CCR5 inhibitor, suggesting use of alternative cofactors. Indeed, SIVmac spread in CCR5-negative human PBMC has been observed and SIVrcm uses CCR2 for efficient CCR5-independent replication in vivo (6, 61).
The dramatic reduction of CCR5 usage by I324C and I324Y variants in infectivity assays is contrasted by the efficient usage of CCR5 in a cell-cell fusion assay. However, important differences exist between these two assays. For one, Env and coreceptor are overexpressed in the fusion assay, with the vaccinia virus-driven Env expression being considerably more efficient than Env expressed under control of the cytomegalovirus promoter (B. A. Puffer, S. Pöhlmann, and R. W. Doms, unpublished observations). Second, the interacting surfaces in the fusion assay are much larger than in the infectivity assay. Thus, the fusion assay is the more robust system, allowing the demonstration of relatively inefficient interactions. Under these conditions I324C and I324Y Env engage CCR5 with almost wt efficiency, suggesting that the interaction with CCR5 might be altered but not abolished and that the defect introduced by the mutations can be overcome under optimized conditions. In contrast, CCR5 usage by the I324L Env was clearly reduced in both infectivity and fusion assays, suggesting that the subtle change from I to L is sufficient to profoundly alter Env engagement of CCR5. Indeed, usage of chimeras between the CCR2 and CCR5 receptors in fusion experiments revealed differential coreceptor engagement by the wt Env and the 324 variants. Thus, the presence of the second extracellular loop of CCR5 was sufficient to allow 239 Env wt-driven fusion, whereas fusion by the I324 variants required both the CCR5 N terminus and the second extracellular loop. These observations indicate that the substitutions at position 324 not only modulate the efficiency of CCR5 engagement but also modulate the way Env interacts with CCR5. A similar finding has been documented for HIV-1, in which a single amino acid change in the V3 loop determined which domains of CCR5 were required for membrane fusion (21).
The 239 Env protein is known to require binding to CD4 for subsequent coreceptor engagement and membrane fusion (16, 44). In contrast, 316 Env, a derivative of 239 Env, mediates infection in the absence of CD4 and allows entry into macaque macrophages, which express very small amounts of CD4 (2, 34, 44). CD4 independence is thought to be associated with increased affinity to CD4, allowing usage of very low levels of surface CD4, and exposure of the CCR5 binding site, facilitating binding to CCR5 in the absence of CD4 (2, 34, 44). The latter feature might be responsible for increased neutralization sensitivity, a property usually associated with CD4 independence (30, 44). Notably, none of the multiple amino acid changes selected in vivo in the CD4-independent 316 variant resides in V3. However, there is evidence that the orientation of the V3 loop in SIVmac239 and 316 Env determines CD4 independence and neutralization efficiency (30). Thus, efficient CD4-independent membrane fusion mediated by the I324H and I324Y variants might reflect changes in the V3 orientation or structure. Indeed, mutations in the tip of HIV-1 V3 have been found to massively impact V3 structural organization and Env interactions with CCR5 (21). However, it is unknown if these changes in V3 lead to CD4 independence of HIV-1. Despite the efficient CD4-independent CCR5 usage of the I324H and I324Y Envs, these changes did not confer macrophage tropism to the respective viral variants, indicating that other determinants are required for infection of this cell type. Further studies are needed to clarify whether the I324H and I324Y Envs exhibit increased binding to CCR5 in the absence of CD4 and whether these Envs are more sensitive to neutralization by antibodies.
The rhesus macaque epithelial cell line sMagi was engineered to express human CD4 and allows entry of multiple HIV-2 and SIV strains but is not permissive for HIV-1 (5). Our analysis, as well as previous studies, suggests that these cells express very little if any CCR5 and no CXCR4 (56, 57). Nevertheless, the I324L variant and the 239wt virus infected sMagi cells efficiently. Notably, entry of I324L, which exhibited clearly reduced CCR5 usage, was more efficient than infection by the wt virus, suggesting that entry into these cells is not mediated by CCR5. Indeed, the CCR5 inhibitor TAK-779 was unable to block entry of both viruses at a concentration of 5 μM. However, a very high concentration of 25 μM reduced the entry of the I324L variant, whereas entry of the wt virus was enhanced. This finding can be explained in three ways. Both viruses could enter sMagi cells via the same coreceptor, which is sensitive to high concentrations of TAK-779, but engage this receptor differentially, or the viruses could use different receptors for entry, with the receptor allowing entry of I324L being blocked by high concentrations of this inhibitor. TAK-779 has been shown to bind to CCR2 and inhibit entry of SIVrcm, illustrating that the compound can engage receptors that are structurally related to CCR5 (12). Alternatively, high doses of TAK-779 could modulate expression of various receptors or attachment factors and thereby differentially modulate infection by the viruses tested. Clearly, the elusive receptor on sMagi cells requires further investigation, especially since the I324T and I324M changes that enhance entry into sMagi cells can arise in vivo (37, 55, 58) and might be associated with enhanced SIV replication in the brain (58). Notably, the respective brain-derived SIV isolates do not replicate in CEMx174 cells, suggesting that the dominant effect of the I324 mutation on coreceptor usage might be preserved in the context of several other mutations in Env associated with SIV neurotropism (58). Thus, the receptor expressed on sMagi cells might play a role in SIV infection of neuronal cells, although the inefficient replication of the I324L variant in PBMC suggests that this receptor might not contribute to SIV spread in T cells in vivo.
Our findings that the SIVmac V3 loop can control coreceptor engagement in the presence or absence of CD4 and that SIVmac can use unidentified receptors for entry shed light on Env function and SIV cellular tropism. However, the replacement of I324 with structurally related amino acids did not result in viral variants with similar functional properties, highlighting that the structural basis for the observed viral phenotypes is unclear. The V3 loop in HIV Env has recently been shown to share structural motifs with chemokines (50). Thus, the V3 loop of an R5-tropic virus was shown to contain a β-hairpin structure also found in the CCR5 ligands MIP-1α and MIP-1β, whereas the V3 loop of a R4-tropic virus formed a β-hairpin structure similar to that found in the CXCR4 ligand SDF-1 (50). One could therefore imagine that some amino acid exchanges at position 324 alter a structural motif also found in CCR5 ligands and thereby modulate CCR5 engagement. Other substitutions, however, could induce a more dramatic conformational change, creating a structure shared with a ligand of an alternative SIV cofactor and thus facilitate usage of this receptor. Further studies are required to elucidate the mechanism behind V3-controlled coreceptor engagement and CD4-independent fusion and to identify the receptors allowing entry of SIVmac into the sMagi cell line.
Acknowledgments
Some reagents were provided by the AIDS Research and Reference Reagent Program. We thank Julie Overbaugh for Magi cell lines, Ronald C. Desrosiers for 221-89 cells, and Nicola Bailer and Karin Strecker for excellent technical assistance.
R.W.D. was supported by the NIH and AI, by a Burroughs Wellcome Fund Translational Research Award, and by an Elizabeth Glaser Scientist Award from the Pediatric AIDS Foundation. F.K. was supported by the DFG, the IZKF Ulm, and the Landesstiftung Baden-Württemberg. S.P. was supported by a fellowship from the DFG and SFB 466.
REFERENCES
- 1.Alexander, L., Z. Du, M. Rosenzweig, J. U. Jung, and R. C. Desrosiers. 1997. A role for natural simian immunodeficiency virus and human immunodeficiency virus type 1 nef alleles in lymphocyte activation. J. Virol. 71:6094-6099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bannert, N., S. Craig, M. Farzan, D. Sogah, N. V. Santo, H. Choe, and J. Sodroski. 2001. Sialylated O-glycans and sulfated tyrosines in the NH2-terminal domain of CC chemokine receptor 5 contribute to high-affinity binding of chemokines. J. Exp. Med. 194:1661-1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berger, E. A., P. M. Murphy, and J. M. Farber. 1999. Chemokine receptors as HIV-1 coreceptors: roles in viral entry, tropism, and disease. Annu. Rev. Immunol. 17:657-700. [DOI] [PubMed] [Google Scholar]
- 4.Bieniasz, P. D., R. A. Fridell, I. Aramori, S. S. Ferguson, M. G. Caron, and B. R. Cullen. 1997. HIV-1-induced cell fusion is mediated by multiple regions within both the viral envelope and the CCR-5 coreceptor. EMBO J. 16:2599-2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chackerian, B., N. L. Haigwood, and J. Overbaugh. 1995. Characterization of a CD4-expressing macaque cell line that can detect virus after a single replication cycle and can be infected by diverse simian immunodeficiency virus isolates. Virology 213:386-394. [DOI] [PubMed] [Google Scholar]
- 6.Chen, Z., D. Kwon, Z. Jin, S. Monard, P. Telfer, M. S. Jones, C. Y. Lu, R. F. Aguilar, D. D. Ho, and P. A. Marx. 1998. Natural infection of a homozygous delta24 CCR5 red-capped mangabey with an R2b-tropic simian immunodeficiency virus. J. Exp. Med. 188:2057-2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen, Z., P. Zhou, D. D. Ho, N. R. Landau, and P. A. Marx. 1997. Genetically divergent strains of simian immunodeficiency virus use CCR5 as a coreceptor for entry. J. Virol. 71:2705-2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choe, H., M. Farzan, Y. Sun, N. Sullivan, B. Rollins, P. D. Ponath, L. Wu, C. R. Mackay, G. LaRosa, W. Newman, N. Gerard, C. Gerard, and J. Sodroski. 1996. The beta-chemokine receptors CCR3 and CCR5 facilitate infection by primary HIV-1 isolates. Cell 85:1135-1148. [DOI] [PubMed] [Google Scholar]
- 9.Cocchi, F., A. L. DeVico, A. Garzino-Demo, A. Cara, R. C. Gallo, and P. Lusso. 1996. The V3 domain of the HIV-1 gp120 envelope glycoprotein is critical for chemokine-mediated blockade of infection. Nat. Med. 2:1244-1247. [DOI] [PubMed] [Google Scholar]
- 10.de Jong, J. J., A. de Ronde, W. Keulen, M. Tersmette, and J. Goudsmit. 1992. Minimal requirements for the human immunodeficiency virus type 1 V3 domain to support the syncytium-inducing phenotype: analysis by single amino acid substitution. J. Virol. 66:6777-6780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deng, H. K., D. Unutmaz, V. N. Kewalramani, and D. R. Littman. 1997. Expression cloning of new receptors used by simian and human immunodeficiency viruses. Nature 388:296-300. [DOI] [PubMed] [Google Scholar]
- 12.Dragic, T., A. Trkola, D. A. Thompson, E. G. Cormier, F. A. Kajumo, E. Maxwell, S. W. Lin, W. Ying, S. O. Smith, T. P. Sakmar, and J. P. Moore. 2000. A binding pocket for a small molecule inhibitor of HIV-1 entry within the transmembrane helices of CCR5. Proc. Natl. Acad. Sci. USA 97:5639-5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edinger, A. L., M. Ahuja, T. Sung, K. C. Baxter, B. Haggarty, R. W. Doms, and J. A. Hoxie. 2000. Characterization and epitope mapping of neutralizing monoclonal antibodies produced by immunization with oligomeric simian immunodeficiency virus envelope protein. J. Virol. 74:7922-7935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edinger, A. L., A. Amedee, K. Miller, B. J. Doranz, M. Endres, M. Sharron, M. Samson, Z. H. Lu, J. E. Clements, M. Murphey-Corb, S. C. Peiper, M. Parmentier, C. C. Broder, and R. W. Doms. 1997. Differential utilization of CCR5 by macrophage and T-cell tropic simian immunodeficiency virus strains. Proc. Natl. Acad. Sci. USA 94:4005-4010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edinger, A. L., T. L. Hoffman, M. Sharron, B. Lee, B. O'Dowd, and R. W. Doms. 1998. Use of GPR1, GPR15, and STRL33 as coreceptors by diverse human immunodeficiency virus type 1 and simian immunodeficiency virus envelope proteins. Virology 249:367-378. [DOI] [PubMed] [Google Scholar]
- 16.Edinger, A. L., J. L. Mankowski, B. J. Doranz, B. J. Margulies, B. Lee, J. Rucker, M. Sharron, T. L. Hoffman, J. F. Berson, M. C. Zink, V. M. Hirsch, J. E. Clements, and R. W. Doms. 1997. CD4-independent, CCR5-dependent infection of brain capillary endothelial cells by a neurovirulent simian immunodeficiency virus strain. Proc. Natl. Acad. Sci. USA 94:14742-14747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edwards, T. G., T. L. Hoffman, F. Baribaud, S. Wyss, C. C. LaBranche, J. Romano, J. Adkinson, M. Sharron, J. A. Hoxie, and R. W. Doms. 2001. Relationships between CD4 independence, neutralization sensitivity, and exposure of a CD4-induced epitope in a human immunodeficiency virus type 1 envelope protein. J. Virol. 75:5230-5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Endres, M. J., P. R. Clapham, M. Marsh, M. Ahuja, J. D. Turner, A. McKnight, J. F. Thomas, B. Stoebenau-Haggarty, S. Choe, P. J. Vance, T. N. Wells, C. A. Power, S. S. Sutterwala, R. W. Doms, N. R. Landau, and J. A. Hoxie. 1996. CD4-independent infection by HIV-2 is mediated by fusin/CXCR4. Cell 87:745-756. [DOI] [PubMed] [Google Scholar]
- 19.Hoffman, T. L., C. C. LaBranche, W. Zhang, G. Canziani, J. Robinson, I. Chaiken, J. A. Hoxie, and R. W. Doms. 1999. Stable exposure of the coreceptor-binding site in a CD4-independent HIV-1 envelope protein. Proc. Natl. Acad. Sci. USA 96:6359-6364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffman, T. L., E. B. Stephens, O. Narayan, and R. W. Doms. 1998. HIV type I envelope determinants for use of the CCR2b, CCR3, STRL33, and APJ coreceptors. Proc. Natl. Acad. Sci. USA 95:11360-11365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu, Q., J. O. Trent, G. D. Tomaras, Z. Wang, J. L. Murray, S. M. Conolly, J. M. Navenot, A. P. Barry, M. L. Greenberg, and S. C. Peiper. 2000. Identification of ENV determinants in V3 that influence the molecular anatomy of CCR5 utilization. J. Mol. Biol. 302:359-375. [DOI] [PubMed] [Google Scholar]
- 22.Hwang, S. S., T. J. Boyle, H. K. Lyerly, and B. R. Cullen. 1991. Identification of the envelope V3 loop as the primary determinant of cell tropism in HIV-1. Science 253:71-74. [DOI] [PubMed] [Google Scholar]
- 23.Isaka, Y., A. Sato, S. Miki, S. Kawauchi, H. Sakaida, T. Hori, T. Uchiyama, A. Adachi, M. Hayami, T. Fujiwara, and O. Yoshie. 1999. Small amino acid changes in the V3 loop of human immunodeficiency virus type 2 determines the coreceptor usage for CXCR4 and CCR5. Virology 264:237-243. [DOI] [PubMed] [Google Scholar]
- 24.Kestler, H., T. Kodama, D. Ringler, M. Marthas, N. Pedersen, A. Lackner, D. Regier, P. Sehgal, M. Daniel, and N. King. 1990. Induction of AIDS in rhesus monkeys by molecularly cloned simian immunodeficiency virus. Science 248:1109-1112. [DOI] [PubMed] [Google Scholar]
- 25.Kirchhoff, F., K. Mori, and R. C. Desrosiers. 1994. The “V3” domain is a determinant of simian immunodeficiency virus cell tropism. J. Virol. 68:3682-3692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kirchhoff, F., S. Pöhlmann, M. Hamacher, R. E. Means, T. Kraus, K. Überla, and P. DiMarzio. 1997. Simian immunodeficiency virus variants with differential T-cell and macrophage tropism use CCR5 and an unidentified cofactor expressed in CEMx174 cells for efficient entry. J. Virol. 71:6509-6516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kolchinsky, P., E. Kiprilov, and J. Sodroski. 2001. Increased neutralization sensitivity of CD4-independent human immunodeficiency virus variants. J. Virol. 75:2041-2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee, B., M. Sharron, L. J. Montaner, D. Weissman, and R. W. Doms. 1999. Quantification of CD4, CCR5, and CXCR4 levels on lymphocyte subsets, dendritic cells, and differentially conditioned monocyte-derived macrophages. Proc. Natl. Acad. Sci. USA 96:5215-5220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marcon, L., H. Choe, K. A. Martin, M. Farzan, P. D. Ponath, L. Wu, W. Newman, N. Gerard, C. Gerard, and J. Sodroski. 1997. Utilization of C-C chemokine receptor 5 by the envelope glycoproteins of a pathogenic simian immunodeficiency virus, SIVmac239. J. Virol. 71:2522-2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Means, R. E., T. Matthews, J. A. Hoxie, M. H. Malim, T. Kodama, and R. C. Desrosiers. 2001. Ability of the V3 loop of simian immunodeficiency virus to serve as a target for antibody-mediated neutralization: correlation of neutralization sensitivity, growth in macrophages, and decreased dependence on CD4. J. Virol. 75:3903-3915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meister, S., C. Otto, A. Papkalla, M. Krumbiegel, S. Pöhlmann, and F. Kirchhoff. 2001. Basic amino acid residues in the V3 loop of simian immunodeficiency virus envelope alter viral coreceptor tropism and infectivity but do not allow efficient utilization of CXCR4 as entry cofactor. Virology 284:287-296. [DOI] [PubMed] [Google Scholar]
- 32.Moore, J. P., and M. Stevenson. 2000. New targets for inhibitors of HIV-1 replication. Nat. Rev. Mol. Cell Biol. 1:40-49. [DOI] [PubMed] [Google Scholar]
- 33.Mori, K., D. J. Ringler, T. Kodama, and R. C. Desrosiers. 1992. Complex determinants of macrophage tropism in env of simian immunodeficiency virus. J. Virol. 66:2067-2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mori, K., M. Rosenzweig, and R. C. Desrosiers. 2000. Mechanisms for adaptation of simian immunodeficiency virus to replication in alveolar macrophages. J. Virol. 74:10852-10859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morner, A., A. Bjorndal, J. Albert, V. N. Kewalramani, D. R. Littman, R. Inoue, R. Thorstensson, E. M. Fenyo, and E. Bjorling. 1999. Primary human immunodeficiency virus type 2 (HIV-2) isolates, like HIV-1 isolates, frequently use CCR5 but show promiscuity in coreceptor usage. J. Virol. 73:2343-2349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O'Brien, W. A., Y. Koyanagi, A. Namazie, J. Q. Zhao, A. Diagne, K. Idler, J. A. Zack, and I. S. Chen. 1990. HIV-1 tropism for mononuclear phagocytes can be determined by regions of gp120 outside the CD4-binding domain. Nature 348:69-73. [DOI] [PubMed] [Google Scholar]
- 37.Overbaugh, J., and L. M. Rudensey. 1992. Alterations in potential sites for glycosylation predominate during evolution of the simian immunodeficiency virus envelope gene in macaques. J. Virol. 66:5937-5948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Owen, S. M., D. Ellenberger, M. Rayfield, S. Wiktor, P. Michel, M. H. Grieco, F. Gao, B. H. Hahn, and R. B. Lal. 1998. Genetically divergent strains of human immunodeficiency virus type 2 use multiple coreceptors for viral entry. J. Virol. 72:5425-5432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Papkalla, A., J. Münch, C. Otto, and F. Kirchhoff. 2002. Nef enhances human immunodeficiency virus type 1 infectivity and replication independently of viral coreceptor tropism. J. Virol. 76:8455-8459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pöhlmann, S., and R. W. Doms. 2002. Evaluation of current approaches to inhibit HIV entry. Curr. Drug Targets Infect. Disord. 2:9-16. [DOI] [PubMed] [Google Scholar]
- 41.Pöhlmann, S., B. Lee, S. Meister, M. Krumbiegel, G. Leslie, R. W. Doms, and F. Kirchhoff. 2000. Simian immunodeficiency virus utilizes human and sooty mangabey but not rhesus macaque STRL33 for efficient entry. J. Virol. 74:5075-5082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pöhlmann, S., N. Stolte, J. Munch, P. ten Haaft, J. L. Heeney, C. Stahl-Hennig, and F. Kirchhoff. 1999. Co-receptor usage of BOB/GPR15 in addition to CCR5 has no significant effect on replication of simian immunodeficiency virus in vivo. J. Infect. Dis. 180:1494-1502. [DOI] [PubMed] [Google Scholar]
- 43.Potts, B. J. 1999. “Mini” reverse transcriptase (RT) assay, p. 103-106. In A. Aldovini and B. Walker (ed.), Techniques in HIV research. Stockton, New York, N.Y.
- 44.Puffer, B. A., S. Pöhlmann, A. L. Edinger, D. Carlin, M. D. Sanchez, J. Reitter, D. D. Watry, H. S. Fox, R. C. Desrosiers, and R. W. Doms. 2002. CD4 independence of simian immunodeficiency virus Envs is associated with macrophage tropism, neutralization sensitivity, and attenuated pathogenicity. J. Virol. 76:2595-2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reeves, J. D., S. A. Gallo, N. Ahmad, J. L. Miamidian, P. E. Harvey, M. Sharron, S. Pöhlmann, J. N. Sfakianos, C. A. Derdeyn, R. Blumenthal, E. Hunter, and R. W. Doms. 2002. Sensitivity of HIV-1 to entry inhibitors correlates with envelope/coreceptor affinity, receptor density, and fusion kinetics. Proc. Natl. Acad. Sci. USA 99:16249-16254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reeves, J. D., S. Hibbitts, G. Simmons, A. McKnight, J. M. Azevedo-Pereira, J. Moniz-Pereira, and P. R. Clapham. 1999. Primary human immunodeficiency virus type 2 (HIV-2) isolates infect CD4-negative cells via CCR5 and CXCR4: comparison with HIV-1 and simian immunodeficiency virus and relevance to cell tropism in vivo. J. Virol. 73:7795-7804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reeves, J. D., A. McKnight, S. Potempa, G. Simmons, P. W. Gray, C. A. Power, T. Wells, R. A. Weiss, and S. J. Talbot. 1997. CD4-independent infection by HIV-2 (ROD/B): use of the 7-transmembrane receptors CXCR-4, CCR-3, and V28 for entry. Virology 231:130-134. [DOI] [PubMed] [Google Scholar]
- 48.Rucker, J., B. J. Doranz, A. L. Edinger, D. Long, J. F. Berson, and R. W. Doms. 1997. Cell-cell fusion assay to study role of chemokine receptors in human immunodeficiency virus type 1 entry. Methods Enzymol. 288:118-133. [DOI] [PubMed] [Google Scholar]
- 49.Rucker, J., M. Samson, B. J. Doranz, F. Libert, J. F. Berson, Y. Yi, R. J. Smyth, R. G. Collman, C. C. Broder, G. Vassart, R. W. Doms, and M. Parmentier. 1996. Regions in beta-chemokine receptors CCR5 and CCR2b that determine HIV-1 cofactor specificity. Cell 87:437-446. [DOI] [PubMed] [Google Scholar]
- 50.Sharon, M., N. Kessler, R. Levy, S. Zolla-Pazner, M. Gorlach, and J. Anglister. 2003. Alternative conformations of HIV-1 V3 loops mimic beta hairpins in chemokines, suggesting a mechanism for coreceptor selectivity. Structure 11:225-236. [DOI] [PubMed] [Google Scholar]
- 51.Sharron, M., S. Pöhlmann, K. Price, E. Lolis, M. Tsang, F. Kirchhoff, R. W. Doms, and B. Lee. 2000. Expression and coreceptor activity of STRL33/Bonzo on primary peripheral blood lymphocytes. Blood 96:41-49. [PubMed]
- 52.Shioda, T., J. A. Levy, and C. Cheng-Mayer. 1991. Macrophage and T cell-line tropisms of HIV-1 are determined by specific regions of the envelope gp120 gene. Nature 349:167-169. [DOI] [PubMed] [Google Scholar]
- 53.Shioda, T., J. A. Levy, and C. Cheng-Mayer. 1992. Small amino acid changes in the V3 hypervariable region of gp120 can affect the T-cell-line and macrophage tropism of human immunodeficiency virus type 1. Proc. Natl. Acad. Sci. USA 89:9434-9438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simmons, G., J. D. Reeves, S. Hibbitts, J. T. Stine, P. W. Gray, A. E. Proudfoot, and P. R. Clapham. 2000. Co-receptor use by HIV and inhibition of HIV infection by chemokine receptor ligands. Immunol. Rev. 177:112-126. [DOI] [PubMed] [Google Scholar]
- 55.Slade, A., S. Jones, A. Jenkins, J. Bootman, A. Heath, P. Kitchin, and N. Almond. 1995. Similar patterns of simian immunodeficiency virus env sequences are found in the blood and lymphoid tissues of chronically infected macaques. AIDS Res. Hum. Retrovir. 11:1509-1511. [DOI] [PubMed] [Google Scholar]
- 56.Sol, N., F. Ferchal, J. Braun, O. Pleskoff, C. Treboute, I. Ansart, and M. Alizon. 1997. Usage of the coreceptors CCR-5, CCR-3, and CXCR-4 by primary and cell line-adapted human immunodeficiency virus type 2. J. Virol. 71:8237-8244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sol, N., C. Treboute, E. Gomas, F. Ferchal, B. Shacklett, and M. Alizon. 1998. The rhesus macaque CCR3 chemokine receptor is a cell entry cofactor for HIV-2, but not for HIV-1. Virology 240:213-220. [DOI] [PubMed] [Google Scholar]
- 58.Stephens, E. B., Z. Q. Liu, G. W. Zhu, I. Adany, S. V. Joag, L. Foresman, N. E. Berman, and O. Narayan. 1995. Lymphocyte-tropic simian immunodeficiency virus causes persistent infection in the brains of rhesus monkeys. Virology 213:600-614. [DOI] [PubMed] [Google Scholar]
- 59.Trkola, A., S. E. Kuhmann, J. M. Strizki, E. Maxwell, T. Ketas, T. Morgan, P. Pugach, S. Xu, L. Wojcik, J. Tagat, A. Palani, S. Shapiro, J. W. Clader, S. McCombie, G. R. Reyes, B. M. Baroudy, and J. P. Moore. 2002. HIV-1 escape from a small molecule, CCR5-specific entry inhibitor does not involve CXCR4 use. Proc. Natl. Acad. Sci. USA 99:395-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Westervelt, P., H. E. Gendelman, and L. Ratner. 1991. Identification of a determinant within the human immunodeficiency virus 1 surface envelope glycoprotein critical for productive infection of primary monocytes. Proc. Natl. Acad. Sci. USA 88:3097-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang, Y., B. Lou, R. B. Lal, A. Gettie, P. A. Marx, and J. P. Moore. 2000. Use of inhibitors to evaluate coreceptor usage by simian and simian/human immunodeficiency viruses and human immunodeficiency virus type 2 in primary cells. J. Virol. 74:6893-6910. [DOI] [PMC free article] [PubMed] [Google Scholar]