Abstract
INTRODUCTION
Ultrasound sonography (US)-guided navigation systems are widely used in various organs, including the breast and liver, to locate precisely lesions that are difficult to palpate or isolate after being identified by other imaging techniques. A recent new method, “volume navigation” (Vnav), delivers real-time image fusion of US with other modalities such as MRI, CT, and PET/CT to facilitate identification and excision of suspected pathology.
PRESENTATION OF CASE
The present report describes a novel navigation technique using Vnav-PET/CT, which delivers image fusion of US with PET/CT. To identify the axillary targets using Vnav-PET/CT, we set at least two landmarks then injected 0.2 ml viscous blue dye in and around the capsule, which resulted in precise resection. Case 1: A 53-year-old woman with 2 PET/CT-positive lymph nodes in the right axilla underwent easy identification of the targets using the navigation technique followed by lymph node dissection. Among 32 lymph nodes dissected, only the two lymph nodes stained by blue dye were shown histologically to be malignant. Case 2: A 68-year-old woman had a PET/CT-positive lymph node in the left axilla. Vnav-PET/CT easily identified the target, which was successfully dissected under local anaesthesia.
DISCUSSION
This navigation and marking using Vnav-PET/CT helped us easily approach the target, resulted in less surgical time, and avoided unsatisfactory axillary complications. These advances of the navigation system enable us to perform precise minimally invasive surgery.
CONCLUSION
This is the first report of navigation surgery using Vnav-PET/CT, which may assist minimally invasive procedures, especially in the axilla.
Keywords: Navigation surgery, Vnav, PET/CT, Axillary neoplasm, Sentinel node biopsy
1. Introduction
Navigation systems have been widely adopted in various fields for diagnostic and therapeutic interventions. Even in the surgical field, this method may provide precise anatomical information and permit minimally invasive surgery. Ultrasound sonography (US) guidance is essential for breast surgery, but a lesion of less than 1 cm in size may be difficult to identify, resulting in misdiagnosis. To overcome this problem, new technologies such as volume navigation (Vnav) or real-time virtual sonography (RVS) have been developed. These systems yield real-time image fusion of US with other modalities such as MRI or CT for identifying breast masses.1,2 We are interested in the application of real-time fusion of US with FDG-PET/CT in the surgical field. In this paper, we report the first experiences of navigation using US fused with PET/CT, called Vnav-PET/CT, in 2 cases of axillary neoplasm.
2. Presentation of cases
Method: The navigation technique was performed using a system configured with volume navigation equipment (LOGIQ E9; GE Healthcare, Milwaukee, WI, USA) in the operation room. To co-register the US image with that of the PET/CT dataset, at least two landmarks (e.g., nipple, pectoral muscle edge, the rib, etc.) were manually identified on the US image and the PET/CT dataset. A transformation matrix was used to display the multiplanar reconstructed (MPR) image from the PET/CT dataset corresponding to the live US image in the supine position. As the US image was moved, the MPR-PET/CT image tracked the movement in real time. Both US and PET/CT images were displayed side-by-side and activated alternately during the procedure, which enabled easy identification of the PET/CT-positive object before surgery. After we identified the target, we injected 0.2 ml blue dye gel (indigocarmine or indocyanin green (ICG) mixed with a similar quantity of lidocaine jelly) in and around the capsule of the lymph node using real-time US guidance (Fig. 1A and B). The aim of this method was explained and informed consent was obtained from each patient prior to surgery. This study was approved by the institutional Ethical Committee.
Fig. 1.
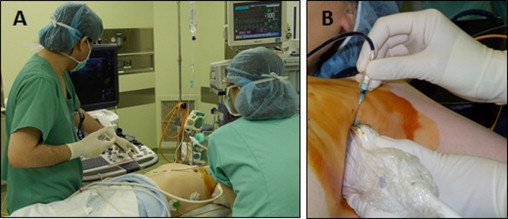
Navigation surgery using Vnav-PET/CT. (A) Navigation was performed in the operation room before surgery using LOGIC E9. (B) Blue dye gel was injected using real-time US guidance.
Case 1: In December 2011, a 53-year-old woman presented with PET/CT-positive (SUVmax: 10.89) right axillary masses (16 mm in size with an SUVmax of 9.28, 10 mm with 3.94) (Fig. 2A). At surgery under general anaesthesia, the targets were detected using Vnav-PET/CT followed by viscous blue dye injection through a 23-G fine needle under US guidance (Fig. 2B–E). During surgery, 2 blue spots were readily identified and completely removed during axillary lymph node dissection (ALND). Among 32 lymph nodes dissected, the 2 marked lymph nodes were histologically diagnosed as fibroblastic reticular cell tumour, a form of lymph node neoplasma.3 No other lymph nodes were involved (Fig. 2F and G).
Fig. 2.
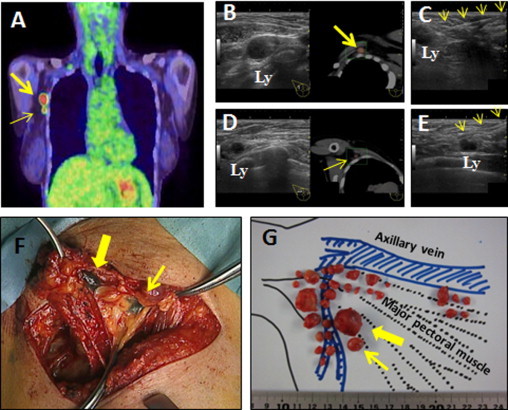
Presentation of Case 1. (A) Coronal PET/CT view. Two positive lymph nodes were detected in the right axilla. (B) Fusion image of real-time US (left) and PET/CT (right) of the rostral large lymph node. Ly and arrow indicate the target lymph node. (C) Injection of blue dye. The arrow indicates the fine needle. (D) Fusion image of the caudal small target. (E) Injection of blue dye. (F) Operative findings. Two blue spots were easily identified and dissected. (G) Mapping of dissected lymph nodes. Two blue-stained lymph nodes were indicated by arrows. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
Case 2: In September 2012, a 68-year-old woman presented with a 16-mm axillary mass with a high SUVmax (6.15) on PET/CT (Fig. 3A). Vnav-PET/CT was performed followed by blue dye injection in the target lymph node (Fig. 3B and C). The target lymph node was easily removed under local anaesthesia and was diagnosed as B-cell lymphoma (Fig. 3D).
Fig. 3.
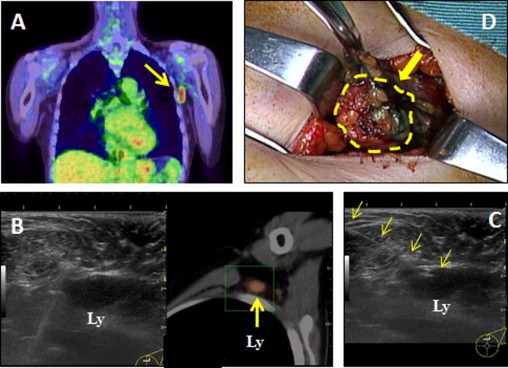
Presentation of Case 2. (A) Coronal PET/CT view. One positive lymph node was detected in the left axilla. (B) Fusion image of real-time US (left) and PET/CT (right). (C) Injection of blue dye. The arrow indicates the fine needle. (D) Operative findings. The dotted line encloses the target lymph node showing a blue spot. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
Mammography, US, and MRI revealed no evidence of breast cancer in these cases.
3. Discussion
Sentinel lymph node biopsy (SLNB) is superior to ALND for axillary evaluation in early breast cancer patients.4 In accordance with minimally invasive surgery, SLNB should be carefully performed to prevent unfavourable complications such as lymphedema of the upper limb. Various methods have been employed to identify the SLN such as use of blue dye or radioisotopes (RIs), and fluorescence imaging (FI) using ICG or computed tomography lymphoscintigraphy (CT-LG), indicating that navigation is critical in SLNB.5–7 These methods greatly assist SLNB, but the target may be missed because of a fatty axilla or disruption of afferent lymphatic vessels. Even if we recognise the target on US, more time may be required to identify it during surgery. Thus, we described a combination of Vnav and PET/CT as navigation for axillary surgery. This navigation and marking helped us easily approach the target even under local anaesthesia, resulted in less surgical time, and avoided unsatisfactory axillary complications. The target lymph nodes ranged from 10 to 16 mm in our cases, but we believe this method would be suitable for lesions more than 5 mm in size as long as they are detectable by US. As is frequently used in partial mastectomy, the injection of viscous blue dye allows easy identification of the target during surgery because the dye does not disperse to the surrounding tissue.
These advanced features of the navigation system enable us to perform precise minimally invasive surgery. However, PET/CT may not be useful in micrometastatic lymph nodes due to low sensitivity,8 and SLNB is indicated in patients with clinically node-negative breast cancer. On the other hand, clinical data from Z0011 trial would suggest the possibility of omitting ALND, even in cases with micrometastasis.9 Z0011 is a phase 3 non-inferiority trial that compares women with invasive breast cancer and sentinel node metastasis who underwent ALND with those who did not undergo ALND. Thus, non-surgical approaches, such as needle/core biopsy proposed by Sever et al. may also be feasible for preoperative axillary evaluation.10 Therefore, our system can be used as a useful navigation technique for appropriate SLNB if these problems are resolved. Further modifications and investigations are required.
4. Conclusion
We applied a novel navigation technique using Vnav-PET/CT. This US image fusion technique may facilitate minimally invasive surgery, especially in the axilla.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patients for publication of this case report and accompanying images.
Author contributions
Manabu Futamura, a surgeon for navigation surgery, contributed towards acquisition of data including figures, critical revision, and final review. Kasumi Morimitsu, Masahito Nawa, Masako Kanematsu, surgeons for navigation surgery, helped in critical revision. Naoe Goto, a physician and pathologist, diagnosed axillar neoplasma and played a significant part in critical revision. Kazuhiro Yoshida contributed in critical revision of manuscript and final review.
References
- 1.Fausto A., Rizzatto G., Preziosa A., Gaburro L., Washburn M.J., Rubello D. A new method to combine contrast-enhanced magnetic resonance imaging during live ultrasound of the breast using volume navigation technique: a study for evaluating feasibility, accuracy and reproducibility in healthy volunteers. Eur J Radiol. 2012;81:e332–e337. doi: 10.1016/j.ejrad.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Nakano S., Kousaka J., Fujii K., Yorozuya K., Yoshida M., Mouri Y. Impact of real-time virtual sonography, a coordinated sonography and MRI system that uses an image fusion technique, on the sonographic evaluation of MRI-detected lesions of the breast in second-look sonography. Breast Cancer Res Treat. 2012;134:1179–1188. doi: 10.1007/s10549-012-2163-9. [DOI] [PubMed] [Google Scholar]
- 3.Andriko J.A.W., Kaldjian E.P., Tsokos M., Abbondanzo S.L., Jaffe E.S. Reticulum cell neoplasms of lymph nodes. Am J Surg Pathol. 1998;22:1048–1058. doi: 10.1097/00000478-199809000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Veronesi U., Paganelli G., Viale G., Path F.R.C., Luini A., Zurrida S. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. New Engl J Med. 2003;349:546–553. doi: 10.1056/NEJMoa012782. [DOI] [PubMed] [Google Scholar]
- 5.Jung E.M., Friedrich C., Hoffstetter P., Dendl L.M., Klebl F., Agha A. Volume navigation with contrast enhanced ultrasound and image fusion for percutaneous interventions: first results. PLoS ONE. 2012;7:e33956. doi: 10.1371/journal.pone.0033956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kitai T., Inomoto T., Miwa M., Shikayama T. Fluorescence navigation with indocyanine green for detecting for sentinel lymph node in breast cancer. Breast Cancer. 2005;12:212–215. doi: 10.2325/jbcs.12.211. [DOI] [PubMed] [Google Scholar]
- 7.Tangoku A., Yamamoto S., Suga K., Ueda K., Nagashima Y., Hida M. Sentinel lymph node biopsy using computed tomography–lymphography in patients with breast cancer. Surgery. 2004;135:258–265. doi: 10.1016/j.surg.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Veronesi U., Cicco C.D., Galimberti V.E., Fernandez J.R., Rotmensz N., Viale G. A comparative study on the value of FDG-PET and sentinel node biopsy to identify occult axillary metastases. Ann Oncol. 2007;18:473–478. doi: 10.1093/annonc/mdl425. [DOI] [PubMed] [Google Scholar]
- 9.Giuliano A.E., Hunt K.K., Ballman K.V., Beitsch P.D., Whitworth P.W., Blumencranz P.W. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis. A randomized clinical trial. JAMA. 2012;305:569–575. doi: 10.1001/jama.2011.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sever A.R., Mills P., Weeks J., Jones S.E., Fish D., Jones P.A. Preoperative needle biopsy of sentinel lymph nodes using intradermal microbubbles and contrast-enhanced ultrasound in patients with breast cancer. Am J Roentogenol. 2012;199:465–470. doi: 10.2214/AJR.11.7702. [DOI] [PubMed] [Google Scholar]


