Abstract
INTRODUCTION
Pulmonary aspergillosis occurs in the parenchymal cavities or ectatic airways. It rarely affects healthy people with an intact immune response. There have been few reports describing an aspergilloma mimicking a lung cancer.
PRESENTATION OF CASE
We experienced the case of an asymptomatic healthy 71-year-old female who was admitted with an abnormal lung shadow. Chest CT revealed an irregularly shaped solid lung nodule in the left upper lobe, which increased in size during the follow-up at a regional hospital. The pathology of the bronchial biopsy was negative for malignant cells, and the cultures were negative. Because a lung cancer was strongly suspected, video-assisted thoracic surgery was performed. Aspergillus was detected by a pathological study of the excised specimen, with no evidence of lung cancer.
DISCUSSION
It is difficult to make an accurate diagnosis of aspergilloma by imaging findings in healthy people with an intact immune response, and therefore a surgical resection allows both the pathological diagnosis and treatment to be performed concurrently.
CONCLUSION
An aspergilloma presenting a mass shadow on imaging may mimic a lung cancer in healthy people with intact immune response.
Keywords: Aspergilloma, Lung cancer, Imaging findings
1. Introduction
The classical CT features of an aspergilloma are characterized by the presence of a solid, round or oval mass with soft-tissue opacity within a lung cavity.1,2 Typically, the mass is separated from the wall of the cavity by an airspace of variable size and shape, resulting in the “air crescent” sign.1,2 The common sites of aspergillomas are the upper lobe and lower lobe superior segment.3 To the best of our knowledge, there have been few reports about aspergilloma mimicking lung cancer. In this report, we describe a case of aspergilloma that manifested as a pulmonary irregular nodule on imaging.
2. Presentation of case
An asymptomatic healthy 71-year-old female was admitted to our hospital with an abnormal lung shadow (Fig. 1). She was a never smoker and had no family history of malignancy, nor immunosuppressive disease. Chest CT revealed an irregularly shaped lung nodule approximately 3.0 cm in diameter in the left upper lobe (Fig. 2), which increased in size during a six month follow-up period at a regional hospital (Fig. 3). The nodule also appeared as a solid lesion through the bronchus (Fig. 2). The 2-[fluorine 18]fluoro-2-deoxy-d-glucose (FDG) uptake at positron emission tomography (PET) showed that the peak standardized uptake value (SUVmax) was 2.0. Radiologists did not diagnose the nodule as an aspergilloma. The pathological examination of the bronchial biopsy was negative for malignant cells, and the cultures were negative by bronchoscopic examinations performed three times during the follow-up period. Because lung cancer was strongly suspected, video-assisted thoracic surgery was performed. An upper division segmentectomy was performed, including the tumor in the left upper lobe. In the specimen, the tumor was necrotic and a pathological examination during operation had shown no evidence of malignancy. The final pathological examination showed the presence of an aspergilloma (Fig. 4). The postoperative evolution was therefore favorable.
Fig. 1.
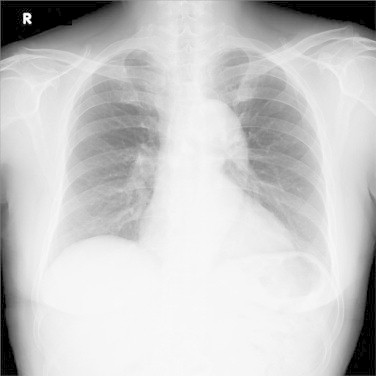
A frontal chest radiograph showed a nodule without a cavitary lesion in the left upper field.
Fig. 2.

Chest CT revealed an irregularly shaped lung nodule approximately 3.0 cm in diameter in the left upper lobe. The nodule also appeared as a solid lesion through the bronchus.
Fig. 3.
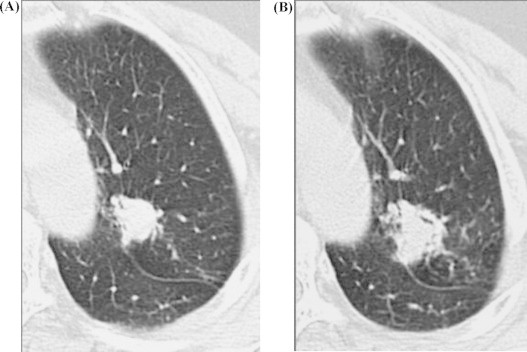
Chest CT showed that the nodule increased in size during the follow-up. (A) At the time when the patient was admitted to a regional hospital, (B) after six months of follow-up.
Fig. 4.
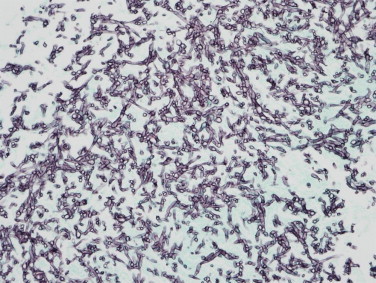
The pathological appearance of the tumor demonstrated dichotomously branching hyphae, compatible with Aspergillus (Gomori's methenamine silver nitrate stain; original magnification 400×).
3. Discussion
Aspergillomas are caused by Aspergillus infections without tissue invasion. These typically lead to the conglomeration of fungal hyphae admixed with mucinous and cellular debris within a preexistent pulmonary cavity or ectatic bronchus.1,2 In patients with a preexisting lung cavity from a variety of causes, such as pulmonary tuberculosis, sarcoidosis or pneumoconiosis, Aspergillus can colonize and grow into the cavity to form a pulmonary aspergilloma (fungus ball).
A typical radiological finding of an aspergilloma is a solid, round or oval mass with soft-tissue opacity within a lung cavity, manifesting an “air crescent sign” without significant enhancement.1,2 In our case, it was difficult to distinguish the nodule because there was no air crescent sign of aspergilloma, and it was therefore suspected to be a lung cancer (Fig. 2). Furthermore, the nodule increased in size during the six month follow-up period (Fig. 3). Park, et al. reported that there were differences in the computed tomography (CT) findings of an intracavitary aspergilloma and a cavitating lung cancer.3 The CT findings of 12 patients with cavitating lung cancer and 26 patients with intracavitary aspergilloma were retrospectively reviewed. They concluded that whether a mural nodule within a cavitary lesion is contrast-enhanced or not is one of the most important features that should be assessed when making a differential diagnosis between these diseases. In our case, the nodule was solid. Yoon et al. also reported the CT findings of pulmonary aspergillosis in immunocompetent patients without an air-meniscus or underlying lung disease.4 They analyzed the imaging findings of seven patients with surgically resected pulmonary aspergillosis. All lesions presented as a nodule or mass unable to be differentiated from malignancy. Most lesions had well-defined margins (4 of 7), appeared as solid lesions (7 of 7), and were located in the upper lobe (5 of 7). Satellite nodules (2 of 7), a CT halo sign (1 of 7), and hypodense signs (4 of 7) were found. Only one lesion increased in size during the follow-up. In our case, the nodule was noted to be a solid lesion, was located in the upper lobe, and increased in size during a six month period (Figs. 1 and 2). However, it was difficult to distinguish whether the tumor was an aspergilloma or lung cancer based on the imaging findings alone.
FDG-PET is an imaging modality that facilitates the distinction between benign and malignant lesions, especially for single nodules.5 However, FDG-PET sometimes shows accumulation in inflammatory and granulomatous conditions, such as aspergilloma.6 Recently, FDG-PET accumulation in cases of pulmonary aspergillosis mimicking lung cancer was reported.7 In the three cases reported in that study, the FDG uptake during PET scans showed an SUVmax ranging from 4.0 to 8.3, and suggested a tendency for high FDG accumulation in 10 cases. On the other hand, some cases, including our present case, showed low FDG accumulation in PET scans.8 Further clinical experiences are needed to clarify the imaging findings and the clinicopathological features associated with this low/high accumulation.
4. Conclusions
We herein reported a case of aspergilloma presenting as a mass shadow on imaging, and indicate that an aspergilloma may mimic a lung cancer in healthy people with an intact immune response. Chest CT in our case revealed an irregularly shaped solid lung nodule in the left upper lobe without the meniscus sign, and the nodule increased in size during a six month follow-up period. It is difficult to make an accurate diagnosis of aspergilloma by imaging findings in healthy people with an intact immune response, so surgical resection allows for both the pathological diagnosis and treatment to be performed concurrently.
Conflict of interest statement
All authors have no competing interests.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report.
Author contributions
M.Y. drafted and wrote the article. A.N. supervised the writing of the manuscript. A.H. and G.S. are members of the surgical team. All authors read and approved the final manuscript.
References
- 1.Gefter W.B. The spectrum of pulmonary aspergillosis. Journal of Thoracic Imaging. 1992;7:56–74. doi: 10.1097/00005382-199209000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Aquino S.L., Lee S.T., Warnock M.L., Gamsu G. Pulmonary aspergillosis: imaging findings with pathologic correlation. American Journal of Roentgenology. 1994;163:811–815. doi: 10.2214/ajr.163.4.8092014. [DOI] [PubMed] [Google Scholar]
- 3.Park Y., Kim T.S., Yi C.A., Cho E.Y., Kim H., Choi Y.S. Pulmonary cavitary mass containing a mural nodule: differential diagnosis between intracavitary aspergilloma and cavitating lung cancer on contrast-enhanced computed tomography. Clinical Radiology. 2007;62:227–232. doi: 10.1016/j.crad.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Yoon S.H., Park C.M., Goo J.M., Lee H.J. Pulmonary aspergillosis in immunocompetent patients without air-meniscus sign and underlying lung disease: CT findings and histopathologic features. Acta Radiologica. 2011;52:756–761. doi: 10.1258/ar.2011.100481. [DOI] [PubMed] [Google Scholar]
- 5.Lowe V.J., Fletcher J.W., Gobal L., Lawson M., Kirchner P., Valk P. Prospective investigation of positron emission tomography in lung nodules. Journal of Clinical Oncology. 1998;16:1075–1084. doi: 10.1200/JCO.1998.16.3.1075. [DOI] [PubMed] [Google Scholar]
- 6.Kawabe J., Okamura T., Koyama K., Shakudo M., Sakamoto H., Kobashi T. Relatively high F-18 fluorodeoxyglucose uptake in paranasal sinus aspergillosis: a PET study. Annals of Nuclear Medicine. 1998;12:145–148. doi: 10.1007/BF03164779. [DOI] [PubMed] [Google Scholar]
- 7.Baxter C.G., Bishop P., Low S.E., Baiden-Amissah K., Denning D.W. Pulmonary aspergillosis: an alternative diagnosis to lung cancer after positive [18F]FDG positron emission tomography. Thorax. 2011;66:638–640. doi: 10.1136/thx.2010.155515. [DOI] [PubMed] [Google Scholar]
- 8.Ahn B.C., Lee S.W., Lee J., Kim C. Pulmonary aspergilloma mimicking metastasis from papillary thyroid cancer. Thyroid. 2011;21:555–558. doi: 10.1089/thy.2010.0448. [DOI] [PubMed] [Google Scholar]


