Abstract
INTRODUCTION
Thyroglossal duct carcinomas (TGDC) are rare, with approximately 274 reported cases since the first report in 1915. The prevalence of carcinomas in surgically removed thyroglossal duct cyst (TGD) is less than 1%. The usual recommended treatment for this condition is the Sistrunk operation, but controversies remain regarding the need for total or partial thyroidectomy.
PRESENTATION OF CASE
A 28-year-old woman was admitted to our hospital with the symptoms of painless midline neck swelling and growing mass. A preoperative computed tomography (CT) showed a 4 cm sized heterogeneous mass at the infrahyoid anterior neck. Ultrasonography of the neck additionally showed suspicious metastatic lymph node at right level VI, both level VI. The patient underwent a Sistrunk operation. The frozen section revealed papillary carcinoma arising from TGDC and also revealed metastatic papillary carcinoma in the right thyroid, at right level III and level VI. Total thyroidectomy, right modified radical neck dissection and central neck dissection were performed. The thyroid gland and TGD were confirmed papillary carcinoma. The dissected neck lymph nodes revealed metastatic papillary carcinoma.
DISCUSSION
The usual recommended treatment for TGD is the Sistrunk procedure. There is controversy regarding whether total or partial thyroidectomy should be performed.
CONCLUSION
Physicians should be aware of extended operation, including thyroidectomy and/or neck node dissection for TGDC with metastatic lesion of thyroid and neck node.
Keywords: Thyroglossal duct carcinoma, Papillary carcinoma, Lateral neck dissection, Sistrunk procedure
1. Introduction
Thyroglossal duct cyst (TDC) results from a developmental anomaly of the thyroid gland and accounts for 70% of congenital neck masses.1 The majority of patients present within the first two decades of life, but nearly a third of cases may manifest in young adulthood. (i.e. >20 years of age)2 TDC usually manifests as an enlarging painless neck mass in children or young adults, and in most circumstances diagnosis can be made by history and physical examination.3 However, thyroglossal duct carcinoma (TGDC) may be clinically indistinguishable from benign TGD, and the diagnosis in most cases is incidental after surgical resection. Fine needle aspiration cytology under ultrasound guidance may enhance preoperative diagnosis. The standard treatment is a Sistrunk procedure, but there is controversy regarding whether total or partial thyroidectomy should be performed.
2. Presentation of case
A 28-year-old woman presented with a painless midline neck swelling which had been progressively increasing in size for one year. On examination, an oval-shaped mass located in the upper part of the anterior neck was found. The mass moved with swallowing as well as on tongue protrusion. Tongue mobility was intact and no abnormalities were observed at the base of the tongue. Thyroid function test was within normal range and other baseline blood investigations were also normal. A clinical diagnosis of thyroglossal cyst was made. Ultrasonography of the neck revealed a cystic mass with internal calcified solid portion at anterior neck, measuring 3.4 cm × 2.8 cm, and it did not communicate with the thyroid gland. Ultrasonography of the neck additionally revealed suspicious metastatic lymph node at right level VI, both level VI. Computed tomography (CT) showed a 4 cm sized heterogeneous mass at the infrahyoid anterior neck. (Fig. 1) However, a clear demarcation was seen between the mass and the thyroid gland, and there were regional lymphadenopathy on right level III. The patient underwent Sistrunk operation. The frozen section revealed papillary carcinoma arising in a TGDC (Fig. 2) and also revealed metastatic papillary carcinoma in a right thyroid, right level III and level VI. Therefore, total thyroidectomy, central neck dissection and right modified radical neck dissection were performed. Histopathological examination identified papillary carcinoma that was confined to the cyst (Fig. 3). Non-neoplastic cystic spaces were partially lined by flattened epithelial cells. Pathologic analysis showed a 7 mm papillary carcinoma in the left lobe of the thyroid gland that lacked extrathyroidal extension (Fig. 4). Postoperative recovery was uneventful. Follow-up at 6 and 36 months after surgery did not reveal any clinical evidence of tumor recurrence, and serum thyroglobulin levels were within normal ranges.
Fig. 1.

Neck CT showing midline multicystic lesion anterosuperior to the thyroid gland.
Fig. 2.
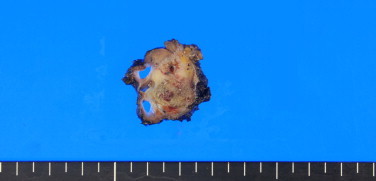
Gross finding of papillary carcinoma arising in a TGDC.
Fig. 3.
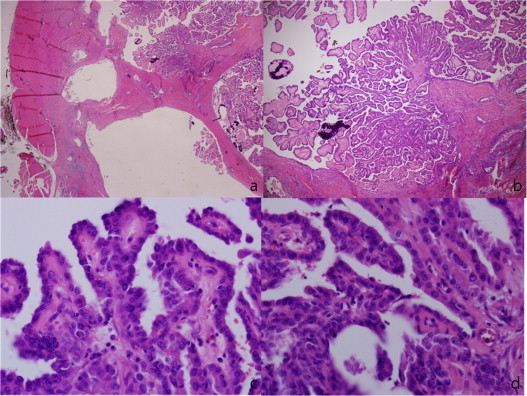
Papillary carcinoma evolving from a thyroglossal duct cyst. Microscopic finding of tumor showing ductal structures with papillary proliferation and psammoma bodies. Tumor cells show optically clear, large, and irregular nuclei with prominent grooving and intranuclear inclusions. (a) H&E, ×12; (b) H&E, ×40; (c and d) H&E, ×400.
Fig. 4.
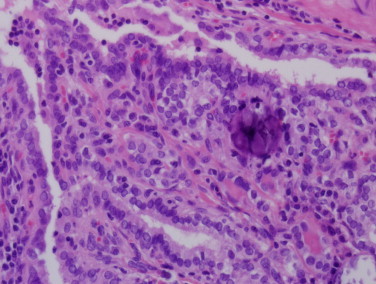
Papillary carcinoma in the left lobe of the thyroid (H&E, ×400).
3. Discussion
Thyroglossal duct cysts develop from persistence of the mid portion of the thyroglossal duct which is an embryonic structure that traces the path of the descent of the thyroid gland. The duct is normally obliterated at around the 8th–10th week of gestation, but if the duct fails to involute completely, the remaining epithelial tissue can develop a TGDC. Previous studies have suggested that this failure to involute occurs in approximately 7% of the population.4 Typically, TDC manifest as an enlarging, painless, midline neck mass in children or young adults that moves upward with tongue protrusion.2,3,5 Rarely, the cyst may localize to the floor of the mouth.6,7 Malignant transformation of TDC to TGDC is uncommon, and the incidence of TGDC carcinoma varies from 0.7% to 1% of all cases of TDC.8,9 According to Widström et al.10 the criteria for diagnosis of primary carcinoma of the thyroglossal duct includes the following: histological identification of TGDC by demonstration (i.e. epithelial lining of ducts with normal thyroid follicles within walls of the cysts), normal thyroid tissue adjacent to the tumor, and histopathological examination of the thyroid gland showing no sign of primary carcinoma.11 The histologic findings of thyroglossal duct carcinoma are most commonly papillary carcinoma (75–80%), but other thyroid tumors such as follicular, Hürthle cell, and mixed papillary–follicular carcinomas have been reported.12 Imaging diagnostic techniques, including ultrasound, scintigraphy and CT, are usually unable to preoperatively diagnose malignant disease11 and fine needle aspiration yields a correct result in only 66% of the cases.13 Nearly 4% of thyroglossal duct carcinomas were found to be locally invasive, while 11% were found to include metastasis to cervical lymph nodes. Contemporary appearance of thyroid carcinoma was described in about 20% of thyroglossal duct carcinomas.14 Reported treatment options for cancers arising in TDC have included mass resection, Sistrunk's procedure (a more involved resection removing the cyst, the body of the hyoid bone, and a cone of the base of the tongue muscle up to the foramen caecum), or a Sistrunk's procedure involving total (or subtotal) thyroidectomy. Sistrunk's procedure is now generally recommended for surgical treatment of benign thyroglossal duct cysts in children and adults.15 This procedure ensures complete resection of the lesion, which can often be found extending around the body of the hyoid bone and up to the base of tongue. The lesion follows the embryonic trajectory of the endodermal pouch of the foregut that gives rise to the thyroid gland (i.e. the thyroglossal duct).4,16 The Sistrunk's procedure can thus be considered as a first line treatment for papillary carcinoma arising in TDCs. In a retrospective study of 57 cases, Patel et al. concluded that the addition of total thyroidectomy to the Sistrunk operation did not have a significant impact on recurrence and survival.14 But some authors propose a more radical approach which involves local excision of the tumor in addition to total thyroidectomy because of occurrence of multicentric papillary carcinomas throughout the entire thyroid gland.17,18 A previous study proposed an algorithm for treatment of papillary carcinoma in TDC which involved a simple Sistrunk procedure in patients less than 45 years of age with tumors less than 1.5 cm that are confined to the cyst and who show an ultrasonographically normal thyroid gland and no suspicious lymph nodes.19 Total thyroidectomy with neck dissection performed only when lymph node metastases are found on ultrasound or during surgery followed by radioiodine is recommended for those not fitting the criteria detailed above. A previous study reported many similarities between papillary carcinoma in TDC and general papillary carcinoma, suggesting that TDC carcinoma is similar to other papillary carcinomas in terms of its multifocality, lymph node metastasis, and prognosis.20 Than they recommend Sistrunk's procedure may be sufficient for carcinoma in TDC measuring up to 1 cm, with total thyroidectomy, and central compartment neck dissection for larger tumors, keeping in mind that a lateral neck dissection may be needed secondarily in some cases, for these midline tumors.20 In the present case, the mass was 3.5 cm and nodal involvement of the tumor was seen on preoperative radiological and intraoperative histopathological studies, which indicated papillary carcinoma. Therefore, a Sistrunk's operation, total thyroidectomy, right modified radical neck dissection, and central compartment neck dissection were performed in this case. The prognosis for papillary TGDC carcinoma is excellent, with occurrence of metastatic lesions occurring in less than 2% of cases.9 Follow-up consists of physical examination, ultrasound of the surgical region and thyroid, and total body scintigraphy.
4. Conclusion
Because of the rarity of TGDC, this diagnosis may be missed, drastically affecting the appropriateness of the treatment provided. Surgeons should be aware of TGDC in surgical planning and postoperative treatment and should include this pathology in differential diagnosis of anterior midline neck mass. Regular follow-up to detect any recurrence in the thyroid gland is essential, particularly in cases where the thyroid gland is not resected.
Conflict of interest statement
The authors have no conflict of interests to declare.
Funding
None.
Ethical approval
Consent from patient available.
Authors’ contributions
SIY collected the information, researched the literature, and wrote the article, KKP and JHK helped with the literature research and in preparing the manuscript. JHK helped in the literature research and edited the final version of manuscript. All authors read and approved the final manuscript.
Contributor Information
Song-I Yang, Email: tonybin@daum.net.
Kwang-Kuk Park, Email: minga00@daum.net.
Jeung-Hoon Kim, Email: kkparkys2@gmail.com.
References
- 1.Allard R.H. The thyroglossal cyst. Head and Neck Surgery. 1982;5(2):134–146. doi: 10.1002/hed.2890050209. [DOI] [PubMed] [Google Scholar]
- 2.Telander R.L., Deane S.A. Thyroglossal and branchial cleft cysts and sinuses. Surgical Clinics of North America. 1977;57(4):779–791. doi: 10.1016/s0039-6109(16)41288-0. [Epub 1977/08/01] [DOI] [PubMed] [Google Scholar]
- 3.Davenport M. ABC of general surgery in children: lumps and swellings of the head and neck. British Medical Journal. 1996;312(7027):368–371. doi: 10.1136/bmj.312.7027.368. [Epub 1996/02/10] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ellis P.D., van Nostrand A.W. The applied anatomy of thyroglossal tract remnants. Laryngoscope. 1977;87(5 Pt 1):765–770. doi: 10.1002/lary.5540870512. [Epub 1977/05/01] [DOI] [PubMed] [Google Scholar]
- 5.Telander R.L., Filston H.C. Review of head and neck lesions in infancy and childhood. Surgical Clinics of North America. 1992;72(6):1429–1447. doi: 10.1016/s0039-6109(16)45889-5. [Epub 1992/12/01] [DOI] [PubMed] [Google Scholar]
- 6.Reede D.L., Bergeron R.T., Som P.M. CT of thyroglossal duct cysts. Radiology. 1985;157(1):121–125. doi: 10.1148/radiology.157.1.4034956. [Epub 1985/10/01] [DOI] [PubMed] [Google Scholar]
- 7.Dolata J. Thyroglossal duct cyst in the mouth floor: an unusual location. Otolaryngology: Head and Neck Surgery. 1994;110(6):580–583. doi: 10.1177/019459989411000618. [Epub 1994/06/01] [DOI] [PubMed] [Google Scholar]
- 8.Heshmati H.M., Fatourechi V., van Heerden J.A., Hay I.D., Goellner J.R. Thyroglossal duct carcinoma: report of 12 cases. Mayo Clinic Proceedings. 1997;72(4):315–319. doi: 10.4065/72.4.315. [Epub 1997/04/01] [DOI] [PubMed] [Google Scholar]
- 9.Fernandez J.F., Ordonez N.G., Schultz P.N., Samaan N.A., Hickey R.C. Thyroglossal duct carcinoma. Surgery. 1991;110(6):928–934. discussion 34–5. [Epub 1991/12/01] [PubMed] [Google Scholar]
- 10.Widstrom A., Magnusson P., Hallberg O., Hellqvist H., Riiber H. Adenocarcinoma originating in the thyroglossal duct. Annals of Otology, Rhinology, and Laryngology. 1976;85(2 (pt 1)):286–290. doi: 10.1177/000348947608500215. [Epub 1976/03/01] [DOI] [PubMed] [Google Scholar]
- 11.Martin-Perez E., Larranaga E., Marron C., Monje F. Primary papillary carcinoma arising in a thyroglossal duct cyst. European Journal of Surgery. 1997;163(2):143–145. [Epub 1997/02/01] [PubMed] [Google Scholar]
- 12.Van Vuuren P.A., Balm A.J., Gregor R.T., Hilgers F.J., Loftus B.M., Delprat C.C. Carcinoma arising in thyroglossal remnants. Clinical Otolaryngology and Allied Sciences. 1994;19(6):509–515. doi: 10.1111/j.1365-2273.1994.tb01279.x. [Epub 1994/12/01] [DOI] [PubMed] [Google Scholar]
- 13.Bardales R.H., Suhrland M.J., Korourian S., Schaefer R.F., Hanna E.Y., Stanley M.W. Cytologic findings in thyroglossal duct carcinoma. American Journal of Clinical Pathology. 1996;106(5):615–619. doi: 10.1093/ajcp/106.5.615. [Epub 1996/11/01] [DOI] [PubMed] [Google Scholar]
- 14.Patel S.G., Escrig M., Shaha A.R., Singh B., Shah J.P. Management of well-differentiated thyroid carcinoma presenting within a thyroglossal duct cyst. Journal of Surgical Oncology. 2002;79(3):134–139. doi: 10.1002/jso.10059. discussion 40–1. [Epub 2002/03/01] [DOI] [PubMed] [Google Scholar]
- 15.Mohan P.S., Chokshi R.A., Moser R.L., Razvi S.A. Thyroglossal duct cysts: a consideration in adults. The American Journal of Surgery. 2005;71(6):508–511. [Epub 2005/07/28] [PubMed] [Google Scholar]
- 16.LiVolsi V.A., Perzin K.H., Savetsky L. Carcinoma arising in median ectopic thyroid (including thyroglossal duct tissue) Cancer. 1974;34(4):1303–1315. doi: 10.1002/1097-0142(197410)34:4<1303::aid-cncr2820340442>3.0.co;2-s. [Epub 1974/10/01] [DOI] [PubMed] [Google Scholar]
- 17.Tradati N., DePaoli F., Benazzo M., Andrle J., Calabrese L., Giugliano G. Papillary carcinoma in thyroglossal duct remnants: presentation of four cases and decision procedure for prophylactic thyroid gland dissection. Oncology Reports. 2000;7(6):1349–1353. doi: 10.3892/or.7.6.1349. [Epub 2000/10/18] [DOI] [PubMed] [Google Scholar]
- 18.Miccoli P., Minuto M.N., Galleri D., Puccini M., Berti P. Extent of surgery in thyroglossal duct carcinoma: reflections on a series of eighteen cases. Thyroid. 2004;14(2):121–123. doi: 10.1089/105072504322880355. [Epub 2004/04/08] [DOI] [PubMed] [Google Scholar]
- 19.Plaza C.P., Lopez M.E., Carrasco C.E., Meseguer L.M., Perucho Ade L. Management of well-differentiated thyroglossal remnant thyroid carcinoma: time to close the debate? Report of five new cases and proposal of a definitive algorithm for treatment. Annals of Surgical Oncology. 2006;13(5):745–752. doi: 10.1245/ASO.2006.05.022. [Epub 2006/03/16] [DOI] [PubMed] [Google Scholar]
- 20.Hartl D.M., Al Ghuzlan A., Chami L., Leboulleux S., Schlumberger M., Travagli J.P. High rate of multifocality and occult lymph node metastases in papillary thyroid carcinoma arising in thyroglossal duct cysts. Annals of Surgical Oncology. 2009;16(9):2595–2601. doi: 10.1245/s10434-009-0571-9. [Epub 2009/07/01] [DOI] [PubMed] [Google Scholar]


