Abstract
INTRODUCTION
Wandering spleen is a rare condition characterized by ectopic position of the spleen due to the absence or laxity of peritoneal ligaments that hold the organ within the left upper quadrant. Lower abdomen and pelvis are the most common locations of the wandering spleen. The disorder usually remains asymptomatic.
PRESENTATION OF CASE
We present a case of acute abdomen due to torsion of a wandering spleen in a primiparus, healthy female shortly after delivery. Diagnosis was based on ultrasonography and computed tomography and was confirmed later on surgery. Total splenectomy was performed successfully.
DISCUSSION
The rarity of the condition and the nonspecific clinical symptoms and signs make prompt diagnosis challenging.
CONCLUSION
Prompt recognition and intervention are necessary in order to minimize the risk of complications. For this reason physicians have to include the condition in the differential diagnosis of acute abdominal pain especially when they encounter females in a pregnancy or post-natal period.
Keywords: Wandering spleen, Torsion, Post-partum, Diagnosis, Management
1. Introduction
Wandering spleen represents a rare clinical entity characterized by abnormal location of the spleen in the lower abdomen or in the pelvic region due to the weakening or the absence of the splenic ligaments.1 Its clinical features are non specific and range from chronic abdominal pain to acute abdomen due to the torsion of the splenic pedicle.1 Diagnosis of wandering spleen is challenging.1 Here we present a case of splenic torsion in a postpartum female with wandering spleen.
2. Case report
A 19 year old postpartum Caucasian female was referred via her general practitioner to the emergency department of the Saint George General Hospital of Chania, Crete, 10 days after giving birth, complaining of a 12 h abdominal pain located in the lower abdominal quadrants without radiation. She had a spontaneous onset of labor at term, 1 h after spontaneous rupture of membranes, with a normal vaginal delivery. Antenatal there was no any history of surgery or trauma. Her vital signs on admission were as follows: temperature, 38.2 grade Celsius; pulse 105 beats/min; blood pressure, 145/90 mmHg; oxygen saturation, 98% while she was breathing ambient air. Laboratory evaluation disclosed: white blood cell count, 9.68 cells/μl (normal range: 4–11 K/μl); hemoglobin, 12.2 g/dl (normal range: 13.5–17.5 g/dl); hematocrit, 25.5% (normal range: 40–50%); platelet counts, 135 cells/μl (normal range: 150–450 K/μl). Urine analysis and urine culture were normal. Biochemical parameters were within normal limits except of C-reactive protein recording an abnormal value of 18.6 mg/dl (normal range: 0–0.5 mg/dl).
Physical examination revealed marked diffuse abdominal tenderness with guarding. Digital rectal examination was normal. Computed tomography of the abdomen was performed with the character of emergency and revealed absence of the spleen from its normal anatomic position and a heterogeneous enlarged soft tissue mass placed in the pelvis (Fig. 1). The patient underwent urgent exploratory laparotomy through a midline incision. Intra-operatively was discovered an enlarged spleen located in the pelvic area suffering clock torsion around the splenic pedicle with evident signs of ischemia (Fig. 2 and 3) and thrombosis of the splenic artery. A total splenectomy was performed. Histological examination demonstrated wide areas of spleen infarction and focal thrombosis of the splenic vein. The postoperative course was uneventful and the patient was discharged on the fifth postoperative day. Antibiotic chemoprophylaxis and vaccination against pneumococcus, meningococcus and Haemophilus influenza were prescribed.
Fig. 1.

Computer tomography image showing wandering spleen in the pelvic cavity.
Fig. 2.
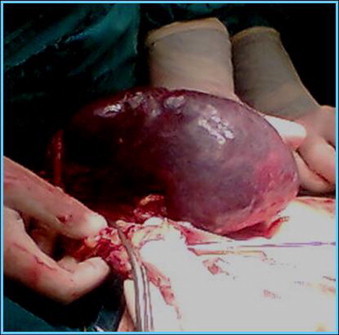
Intraoperative image of an enlarged congested spleen with evident sings of infarction.
3. Discussion
Historically, the condition was firstly described among others by Józef Dietl in 1854.2 Spleen is attached to the posterior part of the left hypochondrium through the splenic pedicle which is formed by the gastrosplenic and splenorenal ligaments and includes the splenic artery and vein and the tail of the pancreas.1,3 Absence or elongation of the suspensory splenic ligaments results to a long splenic mesentery and increased splenic mobility.1,3 Etiology may be congenital or acquired.4 In case of congenital absence occurs a failure of fusion of the dorsal mesogastrium with the posterior abdominal wall during the second month of embryogenesis.4 Acquired risk factors that predispose to wandering spleen include pregnancy, trauma and splenomegaly.1 Remarkably, Satydas et al., reported a splenic weight >500 g in more than 8 out of 10 cases.5 Wandering spleen has an incidence of <0.25% of splenectomies4 and occurs more often in females between the second to fourth decade of life and children.1 Interestingly, it has been reported that one out of three cases of wandering spleen appears in children bellow the age of 10 years old.6 Weakening of the abdominal wall and hormonal variations during pregnancy are the suggested etiological mechanisms for the ligamentous strengthening and the increased incidence of this rare condition in pregnant and post partum females.1
In regard to clinical presentation, the condition may be asymptomatic or may be manifested as acute abdominal pain due to the splenic torsion with secondary infarction.1 More frequently, patients are admitted due to a non specific chronic abdominal discomfort along with a palpable abdominal mass resulting from splenic congestion due to splenic torsion.1 Laboratory investigations are non-specific.1 Thrombocytopenia, through a mechanism of spleen enlargement secondary to compression of the splenic pedicle is rarely found.7 Ultrasonography and computed tomography are the preferred radiographic studies for the diagnosis.5 Acute torsion of the splenic pedicle with splenic infarction are the most common complications of wandering spleen.1 Acute pancreatitis due to the obstruction of the pancreatic tail and upper gastrointestinal hemorrhage from rupture of gastric fundus varices (formed secondary to splenic vein compression) represent unusual occurrences.8
The treatment of choice for the torsion of wandering spleen is surgical.1 Martin performed the first successful splenectomy for a wandering spleen in 18779 while Ludwik Rydygier reported the first successful splenopexy in 1895.10 Surgical management consists of spleen removal especially in symptomatic cases with splenic torsion, infarction, thrombosis of the splenic vessels and suspicion of malignancy.3,11 Spleen preserving strategy with splenopexy is highly recommended in pediatric patients in order to minimize the risk for post-splenectomy septicaemia.12 In this direction, a surgical technique of splenopexy without using mesh has been reported by Soleimani et al., as a safe and curative procedure that may prevent the risk of infection and reaction of foreign material.12 More specifically according to this strategy, a flap is created from the parietal peritoneum and the spleen is settled in the fossa splenica.12 The free edges of this flap are sutured to the stomach, the left end of transverse colon and the beginning of the descending colon.12 Stomach body is stitched to the abdominal wall for preventing volvulus, while the fundus is attached to the diaphragm for splenic support.12
The rarity of the disorder and the non-specific clinical presentation makes prompt diagnosis challenging. Furthermore, although wandering spleen has been repeatedly reported in the medical literature, it is often neglected or misdiagnosed especially in the pediatric population.2 Torsion of wandering spleen represents a life-threatening abdominal emergency3 that requires urgent surgical intervention. A ‘detective judgment’ from the involved physicians is always required especially for rare conditions with non-specific clinical presentation.13 For this reason the entity must be considered in the differential diagnosis of acute abdominal pain especially in females in pregnancy and post-partum.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this manuscript and accompanying images. A copy of the written consent form is available for review by the Editor-in-Chief of this journal.
Author contributions
Dimitrios Anyfantakis and Miltiades Kastanakis prepared the first draft of the manuscript. Nikolaos Katsougris and Emmanouil Bobolakis performed the operation and provided substantial clinical information. George Petrakis and Alexandros Papadomichelakis were involved with the revision and editing of the final manuscript.
All authors have read and approved the final manuscript.
References
- 1.Qazi S.A., Mirza S.M., Muhammad A.M., Al Arrawi M.H., Al-Suhaibani Y.A. Wandering spleen. Saudi Journal of Gastroenterology. 2004;10:1–7. [PubMed] [Google Scholar]
- 2.Magowska A. Wandering spleen: a medical enigma, its natural history and rationalization. World Journal of Surgery. 2013;37:545–550. doi: 10.1007/s00268-012-1880-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewis G.A., Byrne M.P. Wandering spleen. American Surgeon. 1981;47:275–277. [PubMed] [Google Scholar]
- 4.Lam Y., Yuen K.K., Chong L.C. Acute torsion of a wandering spleen. Hong Kong Medical Journal. 2012;18:160–162. [PubMed] [Google Scholar]
- 5.Satydas T., Nasir N., Bradpiece H.A. Wandering spleen: case report and literature review. Journal of the Royal College of Surgeons of Edinburgh. 2002;47:512–514. [PubMed] [Google Scholar]
- 6.Buehner M., Baker M.S. The wandering spleen. Collective review. Surgery Gynecology and Obstetrics. 1992;175:373–387. [PubMed] [Google Scholar]
- 7.Mirkes C., Nguyen G., Cable C. The wandering spleen: an unusual case of thrombocytopenia. Journal of Blood Medicine. 2011;2:161–163. doi: 10.2147/JBM.S24168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singla V., Galwa R.P., Khandelwal N., Poornachandra K.S., Dutta U., Kochhar R. Wandering spleen presenting as bleeding gastric varices. American Journal of Emergency Medicine. 2008;26:637. doi: 10.1016/j.ajem.2007.10.026. [DOI] [PubMed] [Google Scholar]
- 9.Martin A. A successful case of splenotomy. British Journal of Medical. 1878;61:191–192. doi: 10.1136/bmj.1.893.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rydygier D. Die Behandlung der Wandermilz durchsplenopexis. Archiv fur Klinische Chirurgie. 1895;50:880–886. [Google Scholar]
- 11.Tan H.H., Ooi L.L., Tan D., Tan C.K. Recurrent abdominal pain in a woman with a wandering spleen. Singapore Medical Journal. 2007;48:e122–e124. [PubMed] [Google Scholar]
- 12.Soleimani M., Mehrabi A., Kashfi A., Fonouni H., Büchler M.W., Kraus T.W. Surgical treatment of patients with wandering spleen: report of six cases with a review of the literature. Surgery Today. 2007;37:261–269. doi: 10.1007/s00595-006-3389-0. [DOI] [PubMed] [Google Scholar]
- 13.Anyfantakis D., Symvoulakis E.K., Cristodoulakis E.V., Frantzeskakis G. Ruling in the diagnosis of methanol intoxication in a young heavy drinker: a case report. Journal of Medicine and Life. 2012;5:332–334. [PMC free article] [PubMed] [Google Scholar]


