Abstract
Background/Aims
Leptin may be an important link between obesity and many high-burden diseases, including cancer and cardiovascular disease, but leptin levels and correlates in individuals of diverse racial backgrounds have not been well characterized despite racial differences in incidence and mortality patterns for many obesity-related diseases.
Methods
In a cross-sectional study of 915 white and 892 black women enrolled in the Southern Community Cohort Study (age 40–79 years, half postmenopausal), serum leptin levels were compared between the race groups and across categories of body mass index (BMI). Potential correlates of leptin were assessed via race-stratified linear regression models.
Results
Blacks had higher unadjusted leptin levels than whites (geometric mean 22.4 vs. 19.0 ng/ml; p < 0.0001). Leptin increased with increasing BMI, and racial differences in leptin were most pronounced in women with BMI ≥25. Significant correlates of leptin included BMI, age, alcohol consumption, cigarette smoking, diabetes (both races) and fat consumption (black women only). Leptin remained higher in black women (22.7 vs. 18.8 ng/ml) after adjustment for these factors.
Conclusions
Persistent racial differences in leptin concentrations exist after adjustment for BMI and other factors. Leptin assessment may be informative in future studies that investigate racial differences in the development of obesity-related diseases.
Key Words: Leptin, Body mass index, Race, Adipokines
Introduction
Discovered in 1994 [1], leptin is one of several proteins produced in adipose tissue (known as adipokines) and is believed to play a critical role in regulating energy intake and energy expenditure [2]. Further, leptin may contribute to the pathogenesis of breast, endometrial, colorectal and potentially other cancers [3,4], many of which have marked differences in incidence and mortality patterns between white and black women [5]. Given that non-Hispanic black women have the highest prevalence of obesity [39% with body mass index (BMI) >30] and non-Hispanic white women have the lowest (22%) [6], characterization of leptin levels across race groups is an important step towards determining potential mechanisms by which leptin may contribute to racial disparities in obesity-related cancers and perhaps also cardiovascular disease and type 2 diabetes. While normal ranges for leptin levels in healthy individuals have been described [2], less research has been conducted to assess potential differences in leptin levels across race groups. Thus, the objectives of this study were to compare leptin levels between black and white women, to assess potential correlates of serum leptin levels separately for black and white women and, finally, to assess racial differences in leptin levels across a wide range of BMI while controlling for demographic and lifestyle factors that may differ between black and white women.
Methods
The Institutional Review Boards at Vanderbilt University and Meharry Medical College approved this study.
Southern Community Cohort Study
The Southern Community Cohort Study (SCCS) is a prospective epidemiologic cohort study designed to examine racial disparities in cancer incidence and mortality [7]. Study enrollment began in 2002 in 12 southeastern states of the USA at Community Health Centers (CHCs), which are government-funded facilities that provide health services primarily to low-income individuals in medically underserved populations [8]. Recruitment via CHCs makes the SCCS a unique cohort of black and white adults recruited from the same communities and of similar socioeconomic status. As described previously [7], participants were required to be aged between 40 and 79 years, English-speaking and not have undergone treatment for cancer within the past year.
Biomarker Substudy
A biomarker substudy was conducted in 2006 within the SCCS to investigate racial differences in biomarkers hypothesized to be relevant to cancer risk and progression. The substudy included a stratified random sample of 2,000 women who provided a blood sample at study enrollment and self-reported their race as either ‘Black/African American’ or ‘White’. The first 395 women were randomly selected equally across three strata (race, BMI and smoking status). A second random sample of 1,605 women was then selected to include equal numbers of black and white women across race, BMI and menopausal status categories. The biomarker substudy sample of 2,000 women was the basis of this analysis.
Data Collection
All SCCS participants completed a baseline in-person interview conducted at the CHC by a trained study interviewer. The structured questionnaire was administered with the aid of a computer-assisted interview with extensive skip patterns and range and logic checks. The interview elicited information including demographics, anthropometric measurements (including self-reported weight and height at the time of the interview) and several aspects of health and behavior. Physical activity was measured using a questionnaire developed for the SCCS to comprehensively assess active and sedentary behaviors at the time of the interview. Dietary intake in the year prior to the baseline interview was measured using an 89-item food frequency questionnaire designed specifically for the SCCS to elicit information about foods most commonly eaten in the southeastern USA [9,10]. For the 29% of women who were patients in the CHC on the day of the baseline interview, height and weight as measured in the clinic on the day of the baseline interview were abstracted from medical records for validation purposes.
BMI [weight (kg)]/height (m)2] at the time of the baseline interview was calculated from self-reported height and weight. Dietary intakes and total daily physical activity as obtained from the physical activity questionnaire and food frequency questionnaire administered as part of the baseline SCCS interview were categorized into quartiles based on the distribution of the entire sample. Other characteristics were categorized as shown in table 2.
Table 2.
Unadjusted serum leptin levels (ng/ml) according to race and categories of potential correlates of leptin among black and white women enrolled in the SCCS, 2002–2006
| Black women (n = 892) |
White women (n = 915) |
|||||
|---|---|---|---|---|---|---|
| n | median leptin level | 25th to 75th percentile | N | median leptin level | 25th to 75th percentile | |
| BMI1 | ||||||
| <25 | 243 | 10.8 | 6.0–18.7 | 248 | 9.7 | 5.5–15.2 |
| 25.0–29.9 | 235 | 26.2 | 16.2–38.8 | 245 | 19.0 | 11.9–27.8 |
| 30.0–34.9 | 225 | 38.2 | 23.5–50.8 | 225 | 29.0 | 19.1–43.2 |
| 35.0–45 | 189 | 45.9 | 31.4–57.1 | 197 | 39.3 | 26.4–55.1 |
| Age at interview | ||||||
| 40–44 years | 300 | 26.1 | 12.3–42.6 | 317 | 19.9 | 10.2–35.8 |
| 45–49 years | 233 | 26.0 | 14.1–41.8 | 224 | 21.8 | 12.1–36.5 |
| 50–54 years | 136 | 29.6 | 15.6–46.6 | 127 | 21.2 | 11.2–37.2 |
| 55–59 years | 99 | 29.6 | 16.7–42.1 | 111 | 24.0 | 11.5–41.3 |
| 60–64 years | 43 | 40.3 | 17.2–52.6 | 81 | 21.3 | 12.2–43.1 |
| 65–69 years | 42 | 30.5 | 14.6–52.5 | 23 | 27.7 | 15.1–47.1 |
| 70–74 years | 23 | 19.2 | 9.5–54.2 | 22 | 19.3 | 11.4–42.6 |
| 75–79 years | 16 | 37.4 | 12.4–52.8 | 10 | 16.5 | 14.2–23.7 |
| Annual household income | ||||||
| <15,000 USD | 557 | 26.5 | 12.7–44.4 | 540 | 20.0 | 10.6–35.9 |
| 15,000–25,000 USD | 211 | 29.6 | 17.2–46.2 | 188 | 22.4 | 12.4–38.3 |
| 25,000–50,000 USD | 101 | 26.4 | 14.1–43.9 | 123 | 22.1 | 11.3–38.6 |
| <p»50,000 USD | 15 | 26.4 | 15.1–40.7 | 60 | 25.8 | 14.3–44.2 |
| Education | ||||||
| <9 years | 70 | 25.9 | 13.1–46.2 | 77 | 22.8 | 14.2–39.2 |
| 9–11 years | 209 | 25.0 | 12.9–41.2 | 206 | 21.4 | 11.2–41.0 |
| 12 years | 379 | 27.0 | 14.0–45.1 | 378 | 20.5 | 11.2–37.2 |
| <p»12 years | 234 | 31.2 | 17.7–45.9 | 254 | 21.5 | 11.4–36.9 |
| Total daily physical activity | ||||||
| Q1 (<10.2 met-h/day) | 231 | 32.0 | 15.9–48.5 | 218 | 22.8 | 13.1–39.3 |
| Q2 (10.2–18.3 met-h/day) | 219 | 26.8 | 14.2–47.3 | 227 | 22.7 | 11.9–40.5 |
| Q3 (18.4–29.4 met-h/day) | 233 | 25.6 | 13.4–43.7 | 220 | 23.1 | 11.4–38.3 |
| Q4 (>29.5 met-h/day) | 205 | 26.0 | 12.9–41.5 | 245 | 18.2 | 10.2–35.2 |
| Energy intake | ||||||
| Q1 (<1,350 kcal/day) | 194 | 30.1 | 18.1–45.9 | 242 | 22.4 | 11.9–40.5 |
| Q2 (1,350–1,868 kcal/day) | 201 | 32.4 | 15.8–50.3 | 234 | 21.3 | 11.5–35.8 |
| Q3 (1,869–2,601 kcal/day) | 198 | 28.0 | 14.5–45.6 | 240 | 22.0 | 12.4–37.0 |
| Q4 (>2,602 kcal/day) | 256 | 22.1 | 10.7–36.0 | 180 | 20.1 | 9.7–38.0 |
| Total fat intake | ||||||
| Q1 (<49 g/day) | 196 | 30.9 | 17.8–45.8 | 240 | 21.0 | 11.5–41.1 |
| Q2 (49–70 g/day) | 209 | 35.5 | 15.8–51.9 | 227 | 22.5 | 13.5–34.9 |
| Q3 (71–102 g/day) | 199 | 27.0 | 14.4–45.4 | 238 | 20.4 | 10.3–37.6 |
| Q4 (>103 g/day) | 245 | 22.0 | 10.7–34.9 | 191 | 20.6 | 10.8–37.9 |
| Carbohydrate intake | ||||||
| Q1 (<171 g/day) | 188 | 29.0 | 16.0–44.3 | 248 | 21.1 | 11.5–40.1 |
| Q2 (171–239 g/day) | 204 | 30.7 | 16.2–48.0 | 231 | 21.3 | 11.6–35.8 |
| Q3 (240–332 g/day) | 206 | 27.9 | 14.5–46.6 | 232 | 20.4 | 11.6–36.7 |
| Q4 (>333 g/day) | 251 | 22.5 | 11.7–39.8 | 185 | 22.9 | 10.7–38.2 |
| Protein intake | ||||||
| Q1 (<49 g/day) | 201 | 31.4 | 16.7–47.5 | 235 | 21.0 | 11.6–39.9 |
| Q2 (49–69 g/day) | 207 | 30.6 | 17.2–48.0 | 229 | 21.7 | 11.5–37.5 |
| Q3 (70–99 g/day) | 205 | 30.1 | 14.0–47.0 | 232 | 21.9 | 11.6–37.8 |
| Q4 (>100 g/day) | 236 | 22.0 | 10.7–34.7 | 200 | 20.6 | 10.8–37.3 |
| Fiber intake | ||||||
| Q1 (<11 g/day) | 198 | 30.2 | 16.7–46.8 | 237 | 22.6 | 12.7–39.4 |
| Q2 (11–16 g/day) | 207 | 28.3 | 14.7–45.1 | 230 | 21.4 | 11.5–36.6 |
| Q3 (17–23 g/day) | 204 | 26.5 | 13.7–47.6 | 234 | 19.5 | 9.6–37.6 |
| Q4 (>24 g/day) | 240 | 23.7 | 12.6–41.4 | 195 | 23.2 | 11.4–39.0 |
| Alcohol consumption | ||||||
| 0 drinks/day | 432 | 31.9 | 17.1–48.5 | 539 | 22.8 | 12.7–37.9 |
| <1 drink/day | 304 | 26.4 | 13.7–45.5 | 312 | 20.0 | 9.9–39.3 |
| 1–2.9 drinks/day | 70 | 21.5 | 8.9–36.3 | 36 | 16.4 | 10.4–24.9 |
| <p»3 drinks/day | 84 | 17.9 | 8.4–29.4 | 27 | 8.9 | 6.6–23.7 |
| Cigarette smoking status | ||||||
| Current | 348 | 20.7 | 10.6–34.9 | 420 | 16.0 | 8.8–31.4 |
| Former | 186 | 29.6 | 14.2–47.0 | 201 | 26.2 | 15.6–42.3 |
| Never | 357 | 34.1 | 19.1–50.7 | 292 | 24.8 | 13.4–42.6 |
| Menopausal status | ||||||
| Premenopausal | 453 | 26.2 | 14.0–42.4 | 461 | 20.3 | 11.5–37.1 |
| Postmenopausal | 439 | 28.9 | 14.2–46.2 | 454 | 22.4 | 11.3–39.0 |
| Number of live births | ||||||
| None | 94 | 24.6 | 11.1–38.9 | 94 | 20.7 | 10.2–34.1 |
| 1–2 | 304 | 26.1 | 14.0–44.3 | 439 | 20.4 | 11.3–38.0 |
| 3–4 | 311 | 28.9 | 15.8–45.1 | 294 | 21.9 | 11.5–37.9 |
| <p»5 | 183 | 29.1 | 13.8–47.6 | 88 | 23.5 | 12.6–42.9 |
| Diabetes2 | ||||||
| Yes | 193 | 27.9 | 17.0–45.4 | 144 | 23.4 | 14.1–40.0 |
| No | 699 | 26.8 | 13.4–45.1 | 771 | 20.6 | 11.2–37.6 |
| Heart disease2 | ||||||
| Yes | 38 | 34.5 | 22.1–46.3 | 45 | 25.9 | 14.6–42.3 |
| No | 854 | 26.8 | 14.0–45.1 | 870 | 21.2 | 11.4–37.5 |
| Hypertension2 | ||||||
| Yes | 528 | 31.8 | 17.0–46.2 | 414 | 24.5 | 14.0–40.2 |
| No | 364 | 22.9 | 10.8–40.7 | 501 | 18.8 | 9.8–34.0 |
| High cholesterol2 | ||||||
| Yes | 250 | 32.1 | 18.3–48.5 | 328 | 23.3 | 13.3–38.6 |
| No | 641 | 26.4 | 12.6–43.6 | 586 | 20.0 | 10.3–37.5 |
| Depression2 | ||||||
| Yes | 190 | 29.0 | 17.2–46.3 | 443 | 21.3 | 11.5–37.2 |
| No | 702 | 26.8 | 13.5–44.4 | 470 | 21.0 | 11.2–38.4 |
Q1 = First quartile; Q2 = second quartile; Q3 = third quartile; Q4 = fourth quartile; met-h = metabolic equivalent for energy expenditure per hour.
Only 18 women (10 white and 8 black) had BMI <18.5. For these women, median (25th to 75th percentile) values for leptin were 2.76 ng/ml (1.59–5.51) for whites and 2.74 ng/ml (1.41–9.67) for blacks.
Response to the question: “Has a doctor ever told you that you have …?”.
On the same day as the baseline interview, a 10-ml blood sample was collected using EDTA-containing BD Vacutainer® tubes. Blood samples were shipped cold to Vanderbilt University in Nashville, Tenn., USA, where they were centrifuged and aliquoted for storage at −80°C. In this study, 84% of the blood samples were received the day following the blood draw and 98% were received within 2 days. The samples had been frozen for an average of 2.6 years (range 3 months to 5 years). Participants were not required to be fasting. For this study, the median time between the last reported meal and blood collection was 6.2 h (range 0–24 h; median for blacks, 6.1 h, and for whites, 6.3 h; p = 0.07), and for 44% of subjects, blood was collected more than 8 h after their last meal (considered fasting for this analysis). Fasting versus nonfasting leptin levels did not differ significantly in either race group [mean leptin for white women 24.9 vs. 26.3 ng/ml, p = 0.2 (t test); mean leptin for black women 31.4 vs. 29.7 ng/ml, p = 0.2 (t test)].
Laboratory Assays
Leptin levels were measured in serum by radioimmunoassay using the LINCOplex assay (Luminex® xMAP™ Technology, St. Louis, Mo., USA) in the Vanderbilt Hormone Assay and Analytical Services Core Laboratory in duplicate for each woman. For quality control purposes, duplicate sets of samples for 5 randomly selected women were assayed. Leptin levels were measured in 1,989 of the 2,000 samples. Among these, 182 samples were excluded because the measured value was greater than 10% above the upper limit of the detectable range of the assay, leaving 1,807 women for analysis (915 white and 892 black women). The intra-assay coefficient of variation was 13%.
Statistical Methods
For this cross-sectional analysis, data from 1,807 women with measured leptin were analyzed. The average of the two leptin measurements was used in all analyses when available. For 162 participants, only a single leptin measurement was obtained, and this was used in the analyses. Because of the skewed distribution of leptin levels, leptin was log-transformed to better meet modeling assumptions [11]. To ease presentation, back-transformed values are shown. The Wilcoxon signed rank test was used to compare crude leptin values between race groups.
Race-stratified linear regression models with log-transformed leptin as the outcome were developed to evaluate potential correlates of leptin. All models were adjusted for sample selection (395 selected for the SCCS pilot study vs. 1,605 selected later). Potential correlates as categorized in table 2 were added sequentially, and models were compared using Akaike's Information Criterion (AIC), which balances model fit with model complexity [12]. Correlates were added to the model as long as their addition resulted in an AIC value at least 1 unit lower than the AIC for the smaller-order model, indicating that the addition of the correlate improved model fit. Adjusted geometric means for leptin according to BMI were calculated from the final race-stratified models using a categorical measure of BMI (<18.5, 18.5–24.9, 25–29.9, 30–34.5, 35–39.9 and 40–45).
SAS/STAT software, version 9.1 of the SAS System for Windows (SAS Institute Inc., Cary, N.C., USA), was used for all analyses.
Results
By study design, the black and white women had very similar distributions of age, BMI and menopausal status (table 1). Black women more frequently reported a diagnosis of diabetes or hypertension than white women. Unadjusted serum leptin levels were higher in blacks than in whites (geometric mean 22.4 vs. 19.0 ng/ml, p < 0.0001; table 1). Similar racial differences were seen in the subset of 802 women with fasting blood samples (geometric mean 23.6 ng/ml in blacks vs. 18.3 ng/ml in whites; p < 0.0001). Leptin generally increased with increasing categories of BMI, age, income, education and prior diagnosis of diabetes, cardiovascular disease, hypertension and high cholesterol, although some patterns differed between black and white women. In contrast, leptin levels generally decreased over increasing categories of physical activity, total energy and fiber intake, alcohol consumption and cigarette smoking.
Table 1.
Descriptive characteristics of black and white women enrolled in the SCCS with measured leptin values, 2002–2006
| Black women (n = 892) | White women(n = 915) | |
|---|---|---|
| Age, years | 49.9±8.7 | 49.8±8.5 |
| BMI | 29.8±6.1 | 29.7±6.4 |
| Leptin (geometric mean) ng/ml | 22.4±2.5 | 19.0±2.4 |
| Postmenopausal | 453 (51) | 454 (50) |
| Diabetes1 | 193 (22) | 144 (16) |
| Hypertension1 | 528 (59) | 414 (45) |
Values are shown as means ± standard deviation or numbers of patients with percentages in parentheses, as appropriate.
Positive response to t he question: “Has a doctor ever told you that you have …?”.
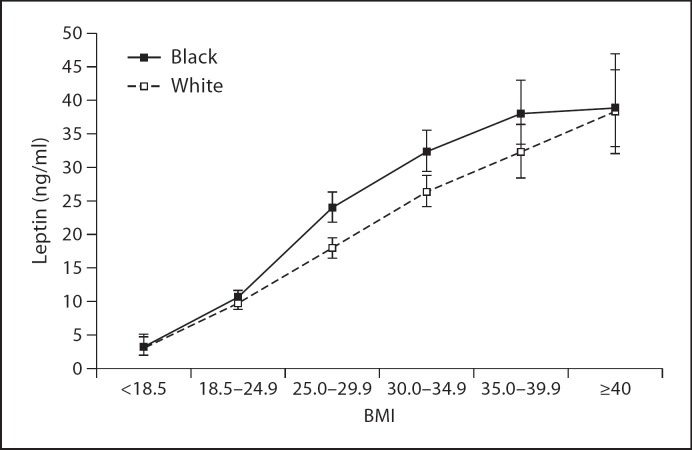
Unadjusted leptin levels increased substantially over increasing categories of BMI in both black and white women and were higher in black women than in white women at each BMI level (table 2). In multivariate models, this pattern persisted, with adjusted geometric means for leptin increasing as body size increased in both groups of women; leptin levels were similar for black and white women with BMIs <18.5 and 18.5–24.9 but were higher in overweight and obese black women compared to white women at the same BMI (fig. 1). Adjustment for fasting status did not alter these results (data not shown).
Fig. 1.
Adjusted geometric means (with 95% confidence intervals) for serum leptin according to categories of BMI from race-stratified linear regression models in women enrolled in the SCCS, 2002-2006. Models were adjusted for age at interview, alcohol consumption, cigarette smoking status and self-reported diabetes (as well as total fat consumption, for black women only). Test for trend: p < 0.0001 for black women and p < 0.0001 for white women.
Potential correlates of leptin were evaluated separately for black and white women, and a similar set of factors was identified as substantially increasing model fit for each race group (table 3). Based on AIC values comparing nested models, BMI and age were positively associated with leptin levels in both blacks and whites, while increasing alcohol consumption was associated with decreased leptin levels. Those women reporting a diabetes diagnosis had lower leptin levels than nondiabetics as did current smokers compared with nonsmokers. Total fat consumption was a significant correlate of leptin only in black women. The proportion of variation explained by these correlates was similar for both groups (R2 = 0.4 for each). Leptin levels adjusted for these factors remained higher in black women compared to whites (22.7 vs. 18.8 ng/ml).
Table 3.
Race-stratified multiple linear regression models for log-transformed serum leptin in black and white women enrolled in the SCCS, 2002–2006
| Characteristic | Black women |
White women |
|||||
|---|---|---|---|---|---|---|---|
| ß | p value | ß | p valu | ||||
| BMI | 0.080 | <0.0001 | 0.079 | <0.0001 | |||
| Age at interview (years) | 0.0076 | 0.0006 | 0.0087 | 0.01 | |||
| Alcohol consumption | |||||||
| 0 drinks/day | Ref. | 0.17 | Ref. | 0.24 | |||
| <1 drink/day | −0.054 | −0.044 | |||||
| 1–2.9 drinks/day | −0.202 | −0.044 | |||||
| <p»3 drinks/day | −0.256 | −0.370 | |||||
| Cigarette smoking status | |||||||
| Current | Ref. | 0.0017 | Ref. | 0.002 | |||
| Former | 0.139 | 0.221 | |||||
| Never | 0.187 | 0.190 | |||||
| Self-reported diabetes | −0.192 | <0.0001 | −0.190 | 0.0007 | |||
| Total fat consumption | |||||||
| Q1 (<49 g/day) | Ref. | 0.016 | not included | ||||
| Q2 (49–70 g/day) | 0.016 | ||||||
| Q3 (71–102 g/day) | −0.017 | ||||||
| Q4 (>103 g/day) | −0.167 | ||||||
| Adjusted R2 for model | 0.40 | 0.39 | |||||
ß estimates and corresponding p values were obtained from race-stratified linear regression models examining log-transformed leptin in relation to the entire set of variables listed in the table. The variables in the model were included if they resulted in a change in the model AIC of at least 1 unit (AIC balances model fit with model complexity). Each race-stratified model was additionally adjusted for sample selection (pilot versus Komen Obesity Project). Ref. = Reference value.
Discussion
In this large, cross-sectional study of black and white women from similar geographic and socioeconomic situations, we observed that black women had leptin levels that were approximately 20% higher than levels among whites even after adjustment for BMI and other significant correlates. Early comparisons of leptin levels across race groups generally utilized convenience samples, and conflicting results were reported, with some groups finding no difference in leptin levels according to race [13,14] and at least one finding lower levels in black women compared to white women [15]. In contrast, larger population-based studies have consistently found leptin levels to be higher in black women than in white women. In the Multiethnic Cohort Study, mean leptin levels were 27.9 ng/ml among 73 black women and 21.4 ng/ml among 71 white women [16]. Similar findings were reported from the Health, Aging, and Body Composition Study among 718 black and 840 white women aged 70–79 years (leptin geometric means 20.2 vs. 13.9 ng/ml, respectively) [17] and from the Atherosclerosis Risk in Communities study among 305 black males and females and 388 whites (median leptin 20.3 vs. 9.8 ng/ml) [18]. The largest study to date to examine racial differences in leptin levels was conducted using data from the third National Health and Nutrition Examination Survey, and mean leptin levels were found to be 16.4 ng/ml among 957 black women and 12.2 ng/ml among 1,441 white women [19].
Differences in leptin levels between black and white women could reflect physiological or genetic differences in the production of leptin in adipose tissue, but it is also possible that incomplete adjustment for fat distribution is responsible for the differences observed in this and other large population-based studies. Black women tend to have a higher proportion of subcutaneous fat than do white women [20,21], and leptin secretion is higher in subcutaneous fat than in visceral fat [22,23]. While BMI is a useful measure of overall fat mass in population-based studies, it is not able to distinguish between fat and lean mass or between the relative contribution of specific fat depots to overall adiposity [24]. Thus, in our analysis, adjustment for BMI may not completely account for racial differences in fat patterning that may affect leptin levels. However, in two previous studies, black women had modestly higher leptin levels than white women after adjustment for additional measures of adiposity such as percentage fat and visceral fat in one study [17] and skinfold thicknesses and waist and hip circumferences in another [19].
Beyond BMI, age, alcohol consumption, cigarette smoking status and diabetes were all found to be significant correlates of leptin levels in both black and white women in this study. Consistent with our results, many [13,25,26,27], but not all [28], studies have found lower leptin levels associated with cigarette smoking, possibly as a result of increased leptin sensitivity among smokers [26]. Few studies have examined alcohol consumption in relation to leptin in women but, as we found, alcohol intake has been observed to be inversely associated with leptin levels in some studies [13,25], although not all [27]. As we observed in crude tabulations, some early epidemiologic studies observed higher leptin levels in diabetics, but adjustment for body size has generally shown leptin levels to be lower among diabetics [18,27,29].
An important limitation of this study is the cross-sectional design, which does not allow us to ascertain whether the variables associated with leptin levels are actual determinants of circulating levels. This study is also potentially limited by the convenience blood sample used for the leptin measurement. While there is evidence to indicate that leptin secretion shows clear circadian variation [30], additional adjustment for time of day of blood collection did not alter the results of this study. Another potential limitation of the measurement of leptin is that it was not conducted exclusively in fasting samples; however, analyses limited to samples provided more than 8 h since the last meal did not show any appreciable differences from those using the entire population. An additional limitation is that we had available only a single measurement of leptin due to the infeasible nature of collecting multiple samples over time in a large cohort study. Finally, the use of self-reported height and weight measures is also a potential limitation. A recent review shows that height tends to be overreported and weight underreported in women [31]. However, analysis of 1999–2004 National Health and Nutrition Examination Survey data showed that underreporting of weight was more common in whites and among well-educated women [32], indicating that the BMI values obtained from women in the SCCS may be less vulnerable to bias than in other studies that include more highly educated participants. In this sample, we found no evidence of weight underreporting according to race; the mean difference in self-reported weight and measured weight as abstracted from medical records among the 518 women (29%) with both measures available was the same in both black and white women (−1.68 pounds; p = 0.99). There was a small but significant difference according to educational attainment in the same direction suggested by the National Health and Nutrition Examination Survey data. Among the 518 women with self-reported and measured values for weight, those with more than a high school education had a mean difference of −3.0 pounds compared with −1.3 pounds for those with a high school education or less (p = 0.04). Generally in the SCCS, BMI values calculated from self-reported height and weight were very highly correlated with BMI values calculated from medical record data overall (Pearson correlation coefficient >0.95) as well as across strata of race and BMI, indicating that the self-reported values are generally valid in both groups of women studied here.
A major strength of this study is the inclusion of both black and white women who, because of the design of the SCCS, come from similar geographic and socioeconomic backgrounds. This allows for the examination of racial differences with a minimum of socioeconomic status-driven confounding, a limiting factor in the interpretation of results from many previous studies with less similar groups of black and white participants. This study is also strengthened by the large sample size of black and white women and by the meaningful numbers of women representing a wide spectrum of body sizes.
In this large population of both black and white women, we observed higher leptin levels among black women compared to white women even after adjustment for BMI and other significant correlates including age, alcohol consumption, cigarette smoking and diabetes. Given the high prevalence of obesity in all populations, and especially among black women, the data presented herein strengthen the view that the adipokine leptin may be a useful biomarker to help inform future work within the SCCS and in other studies with diverse populations with regard to the roles of obesity in the development of cancer and other diseases.
Disclosure Statement
This project was funded in part by grant OP05-0927-DR1 from Susan G. Komen for the Cure. The SCCS is funded by grant R01 CA92447 from the National Cancer Institute. Serum sample preparation was conducted at the Survey and Biospecimen Shared Resource, which is supported in part by the Vanderbilt-Ingram Cancer Center (P30 CA68485).
The funding bodies had no input in the study design, collection, analysis and interpretation of the data, writing of the manuscript or the decision to submit the manuscript for publication.
The authors declare that they have no potential conflicts of interest.
References
- 1.Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–432. doi: 10.1038/372425a0. [DOI] [PubMed] [Google Scholar]
- 2.Anubhuti Arora S. Leptin and its metabolic interactions: an update. Diabetes Obes Metab. 2008;10:973–993. doi: 10.1111/j.1463-1326.2008.00852.x. [DOI] [PubMed] [Google Scholar]
- 3.Koerner A, Kratzsch J, Kiess W. Adipocytokines: leptin – the classical, resistin – the controversical, adiponectin – the promising, and more to come. Best Pract Res Clin Endocrinol Metab. 2005;19:525–546. doi: 10.1016/j.beem.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 4.van Kruijsdijk RC, van der Wall E, Visseren FL. Obesity and cancer: the role of dysfunctional adipose tissue. Cancer Epidemiol Biomarkers Prev. 2009;18:2569–2578. doi: 10.1158/1055-9965.EPI-09-0372. [DOI] [PubMed] [Google Scholar]
- 5.Ries LAG, Harkins D, Krapcho M, Mariotto A, Miller BA, Feuer EJ, Clegg L, Eisner MP, Horner MJ, Howlader N, Hayat M, Hankey BF, Edwards BK, editors. SEER Cancer Statistics Review. Bethesda: National Cancer Institute; 1975-2003. http://seer.cancer.gov/csr/1975_2003/, based on November 2005 SEER data submission, posted to the SEER web site, 2006. [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Differences in prevalence of obesity among black, white, and Hispanic adults – United States, 2006–2008. MMWR Morb Mortal Wkly Rep. 2009;58:740–744. [PubMed] [Google Scholar]
- 7.Signorello LB, Hargreaves MK, Steinwandel MD, Zheng W, Cai Q, Schlundt DG, Buchowski MS, Arnold CW, McLaughlin JK, Blot WJ. Southern community cohort study: establishing a cohort to investigate health disparities. J Natl Med Assoc. 2005;97:972–979. [PMC free article] [PubMed] [Google Scholar]
- 8.Hargreaves MK, Arnold C, Blot WJ. Community health centers: their role in the treatment of minorities and in health disparities research. In: Satcher D, Pamies R, editors. Multicultural Medicine and Health Disparities. New York: McGraw-Hill; 2006. pp. 485–494. [Google Scholar]
- 9.Signorello LB, Munro HM, Buchowski MS, Schlundt DG, Cohen SS, Hargreaves MK, Blot WJ. Estimating nutrient intake from a food frequency questionnaire: incorporating the elements of race and geographic region. Am J Epidemiol. 2009;170:104–111. doi: 10.1093/aje/kwp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buchowski MS, Schlundt DG, Hargreaves MK, Hankin JH, Signorello LB, Blot WJ. Development of a culturally sensitive food frequency questionnaire for use in the Southern Community Cohort Study. Cell Mol Biol (Noisy-le-grand) 2003;49:1295–1304. [PubMed] [Google Scholar]
- 11.Kleinbaum DG, Kupper LL. Applied Regression Analysis and Other Multivariable Methods. North Scituate: Duxbury Press; 1978. [Google Scholar]
- 12.Akaike H. Fitting autoregressive models for prediction. Ann Inst Stat Math. 1969;21:243–247. [Google Scholar]
- 13.Donahue RP, Zimmet P, Bean JA, Decourten M, DeCarlo Donahue RA, Collier G, Goldberg RB, Prineas RJ, Skyler J, Schneiderman N. Cigarette smoking, alcohol use, and physical activity in relation to serum leptin levels in a multiethnic population: the Miami Community Health Study. Ann Epidemiol. 1999;9:108–113. doi: 10.1016/s1047-2797(98)00037-4. [DOI] [PubMed] [Google Scholar]
- 14.Perry HM, 3rd, Morley JE, Horowitz M, Kaiser FE, Miller DK, Wittert G. Body composition and age in African-American and Caucasian women: relationship to plasma leptin levels. Metabolism. 1997;46:1399–1405. doi: 10.1016/s0026-0495(97)90138-4. [DOI] [PubMed] [Google Scholar]
- 15.Nicklas BJ, Toth MJ, Goldberg AP, Poehlman ET. Racial differences in plasma leptin concentrations in obese postmenopausal women. J Clin Endocrinol Metab. 1997;82:315–317. doi: 10.1210/jcem.82.1.3659. [DOI] [PubMed] [Google Scholar]
- 16.DeLellis Henderson K, Rinaldi S, Kaaks R, Kolonel L, Henderson B, Le Marchand L. Lifestyle and dietary correlates of plasma insulin-like growth factor binding protein-1 (IGFBP-1), leptin, and C-peptide: the Multiethnic Cohort. Nutr Cancer. 2007;58:136–145. doi: 10.1080/01635580701328073. [DOI] [PubMed] [Google Scholar]
- 17.Ruhl CE, Everhart JE, Ding J, Goodpaster BH, Kanaya AM, Simonsick EM, Tylavsky FA, Harris TB, Health, Aging, and Body Composition Study Serum leptin concentrations and body adipose measures in older black and white adults. Am J Clin Nutr. 2004;80:576–583. doi: 10.1093/ajcn/80.3.576. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt MI, Duncan BB, Vigo A, Pankow JS, Couper D, Ballantyne CM, Hoogeveen RC, Heiss G, ARIC Investigators Leptin and incident type 2 diabetes: risk or protection? Diabetologia. 2006;49:2086–2096. doi: 10.1007/s00125-006-0351-z. [DOI] [PubMed] [Google Scholar]
- 19.Ruhl CE, Everhart JE. Leptin concentrations in the United States: relations with demographic and anthropometric measures. Am J Clin Nutr. 2001;74:295–301. doi: 10.1093/ajcn/74.3.295. [DOI] [PubMed] [Google Scholar]
- 20.Kanaley JA, Giannopoulou I, Tillapaugh-Fay G, Nappi JS, Ploutz-Snyder LL. Racial differences in subcutaneous and visceral fat distribution in postmenopausal black and white women. Metabolism. 2003;52:186–191. doi: 10.1053/meta.2003.50024. [DOI] [PubMed] [Google Scholar]
- 21.Wagner DR, Heyward VH. Measures of body composition in blacks and whites: a comparative review. Am J Clin Nutr. 2000;71:1392–1402. doi: 10.1093/ajcn/71.6.1392. [DOI] [PubMed] [Google Scholar]
- 22.Hube F, Lietz U, Igel M, Jensen PB, Tornqvist H, Joost HG, Hauner H. Difference in leptin mRNA levels between omental and subcutaneous abdominal adipose tissue from obese humans. Horm Metab Res. 1996;28:690–693. doi: 10.1055/s-2007-979879. [DOI] [PubMed] [Google Scholar]
- 23.Montague CT, Prins JB, Sanders L, Digby JE, O’Rahilly S. Depot- and sex-specific differences in human leptin mRNA expression: implications for the control of regional fat distribution. Diabetes. 1997;46:342–347. doi: 10.2337/diab.46.3.342. [DOI] [PubMed] [Google Scholar]
- 24.Willett WC. Nutritional Epidemiology. ed 2. New York: Oxford University Press; 1998. [Google Scholar]
- 25.De Silva A, De Courten M, Zimmet P, Nicholson G, Kotowicz M, Pasco J, Collier GR. Lifestyle factors fail to explain the variation in plasma leptin concentrations in women. Nutrition. 1998;14:653–657. doi: 10.1016/s0899-9007(98)00065-3. [DOI] [PubMed] [Google Scholar]
- 26.Wei M, Stern MP, Haffner SM. Serum leptin levels in Mexican Americans and non-Hispanic whites: association with body mass index and cigarette smoking. Ann Epidemiol. 1997;7:81–86. doi: 10.1016/s1047-2797(96)00114-7. [DOI] [PubMed] [Google Scholar]
- 27.Marques-Vidal P, Bochud M, Paccaud F, Mooser V, Waeber G, Vollenweider P. Distribution of plasma levels of adiponectin and leptin in an adult Caucasian population. Clin Endocrinol (Oxf) 2010;72:38–46. doi: 10.1111/j.1365-2265.2009.03628.x. [DOI] [PubMed] [Google Scholar]
- 28.Ganji V, Kafai MR, McCarthy E. Serum leptin concentrations are not related to dietary patterns but are related to sex, age, body mass index, serum triacylglycerol, serum insulin, and plasma glucose in the US population. Nutr Metab (Lond) 2009;6:3. doi: 10.1186/1743-7075-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Panarotto D, Ardilouze JL, Tessier D, Maheux P. The degree of hyperinsulinemia and impaired glucose tolerance predicts plasma leptin concentrations in women only: a new exploratory paradigm. Metabolism. 2000;49:1055–1062. doi: 10.1053/meta.2000.7745. [DOI] [PubMed] [Google Scholar]
- 30.Sinha MK, Sturis J, Ohannesian J, Magosin S, Stephens T, Heiman ML, Polonsky KS, Caro JF. Ultradian oscillations of leptin secretion in humans. Biochem Biophys Res Commun. 1996;228:733–738. doi: 10.1006/bbrc.1996.1724. [DOI] [PubMed] [Google Scholar]
- 31.Gorber SC, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8:307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 32.Craig BM, Adams AK. Accuracy of body mass index categories based on self-reported height and weight among women in the United States. Matern Child Health J. 2009;13:489–496. doi: 10.1007/s10995-008-0384-7. [DOI] [PMC free article] [PubMed] [Google Scholar]