Abstract
Objectives
The purpose of this study is to report on long-term outcomes in a prospective study comparing the quality of life outcomes in smokers and non-smokers undergoing functional endoscopic sinus surgery.
Study Design
Prospective clinical trial.
Methods
A total of 235 patients were prospectively enrolled at a single tertiary academic center. Preoperative SNOT-20 scores and comprehensive demographic and smoking data were obtained. Preoperative SNOT-20 scores were compared to postoperative SNOT-20 scores.
Results
Long-term followup results were available in 111/185 nonsmokers (60%) and 26/50 smokers (52%). Non-smokers had a mean preoperative SNOT-20 score of 26.2, a short-term followup score of 10.1 (mean 3.1 months) and a long-term followup score of 11.4 (mean 44.2 months). Smokers had a mean preoperative SNOT-20 score of 27.8, a short-term followup score of 5.7 (mean 3.1 months) and a long-term followup score of 8.3 (mean 40.3 months). The mean improvement in SNOT-20 scores for smokers was significantly greater than non-smokers in short-term followup (p=.044), however no significant difference in improvement was seen between smokers and non-smokers at long-term followup.
Conclusions
Both smokers and non-smokers continue to maintain a highly significant improvement in SNOT-20 scores following endoscopic sinus surgery at long-term followup. While smoking remains a well documented cause of medical morbidity, smokers maintained an improvement in quality of life after long-term followup from endoscopic sinus surgery in this prospective study.
Keywords: smoking, endoscopic sinus surgery, SNOT-20, surgical outcomes, quality of life
Introduction
Smoking related complications constitute the greatest cause of preventable, premature death. Smoking is the leading risk factor for head and neck cancer and has been proven as a cause for multiple respiratory diseases. However, there are few studies examining the effects of smoking on surgical outcomes for chronic rhinosinusitis. A deeply influential study by Senior et. al.1 retrospectively examined the long-term surgical outcomes of patients following endoscopic sinus surgery with a mean followup of 7.8 years. A subset analysis of this cohort revealed that 18.3% of these patients required revision endoscopic sinus surgery. 27% of the patients in the revision group were smokers, versus 10% of smokers in the non-revision sinus surgery group. As a result of this study and anecdotal evidence, many endoscopic sinus surgeons refused to offer surgery to active smokers with chronic rhinosinusitis.
Expecting to further support these conclusions, we reviewed short-term surgical outcomes on prospectively collected data2 from 221 patients who underwent endoscopic sinus surgery from a single-institution between 2003 and 2006. We observed that both smokers and non-smokers had large, clinically meaningful reductions in SNOT-20 scores, however, we were surprised to report that smokers had statistically significant greater improvements in SNOT-20 measurements than non-smokers (mean followup: 3.1 months). We speculated that smokers may have pathophysiology (osteomeatal obstruction, mucociliary dysfunction, etc.) that was more amenable to short-term improvement from functional endoscopic surgery compared to pathophysiology seen in non-smokers (worse underlying mucosal problems, systemic immune dysfunction, etc.) This short-term outcome study did call into question the notion that active smokers with chronic rhinosinusitis were poor candidates for endoscopic sinus surgery. To further examine the outcomes of endoscopic sinus surgery in smokers, we report quality of life data on this cohort with longer-term followup (mean: 43.5 months).
Materials and Methods
Study Design
This study prospectively enrolled 235 adult patients at the Medical College of Georgia from 2003 to 2006 who were undergoing endoscopic sinus surgery by the senior author to participate in a study examining the molecular mechanisms of chronic rhinosinusitis. The study was approved by the institutional review board and all participants provided written informed consent.
Patient Population
All patients enrolled in this study had a diagnosis of chronic rhinosinusitis based on history, physical examination, and computed tomography (CT) findings. The diagnosis of chronic rhinosinusitis was made according to the criteria established by the Rhinosinusitis Task Force of the American Academy of Otolaryngology—Head and Neck Surgery3. Patients with persistent chronic rhinosinusitis after at least 4 weeks of medical therapy (inhaled nasal steroids, nasal saline irrigations, and antibiotics if there was evidence of purulence on endoscopic examination) were offered surgery. Detailed smoking histories were obtained by history pre-operatively. Patients were considered smokers if they reported current, ongoing smoking, and all were vigorously counseled on tobacco cessation. Patients who consented to endoscopic sinus surgery were invited to enroll in the database. Participants who were pregnant, unable to adequately give informed consent, and/or were less than 18 years of age were excluded from the study.
Objective and Quality of Life Clinical Outcome Measures
Medical records from the study participants and an institutionally-approved Rhinosinusitis – Endoscopic Sinus Surgery form were used to prospectively collect patient history information including age, sex, pre-operative medication use, history of asthma, aspirin sensitivity, nasal polyposis, history of prior sinus surgery, history of prior septoplasty, prior facial trauma, history of current and prior smoking, previous blood test results, and other relevant patient factors. All patients underwent pre-operative CT scanning and scans were graded according to the Lund-Mackay CT scoring system4. All patients received pre-operative and postoperative endoscopy using the Lund-Kennedy scoring system5. Participants completed a visual analog scale symptom score according to the Rhinosinusitis Task Force symptom criteria and the Sino-Nasal Outcome Test – 20 (SNOT-20), a clinically validated, disease-specific, health-related quality-of-life measure for chronic rhinosinusitis6. Participants completed the SNOT-20 upon enrollment pre-operatively, and at 3 month, 6 month, 1 year, 2 year, then annual intervals. In many cases, patients who did not maintain scheduled followup appointments were called to complete SNOT-20 scores via telephone. Two tailed Student’s t test analysis was performed using STATA 10 IC (College Station, TX) with alpha = 0.05.
Results
235 patients were enrolled in the study. Of these, 50 were smokers and 185 were non-smokers. This represented a smoking population of 21.3% which is similar to the national average of 20.9%.7 Table 1 presents the demographic and clinical characteristics for these study patients. Pre-operative SNOT-20 differences for smokers and non-smokers were not found to be statistically significant, with mean scores of 27.8 for non-smokers and 26.2 for smokers. Non-smokers had higher rates of requiring revision surgery (39% vs. 20%), presence of nasal polyposis (50% vs. 22%), and asthma (46% vs 20%), however, these differences did not reach statistical significance. In objective findings, non-smokers had worse pre-operative Lund-Mackay scores (9.2 vs 7.4), and pre-operative endoscopy scores (5.0 vs. 3.9), however, these differences also did not reach statistical significance.
Table 1.
Patient Characteristics
| Smokers n=50 21% |
Non-Smokers n=135 79% |
P value | |
|---|---|---|---|
|
| |||
| Age, yr (mean) | 48.9 | 46.7 | |
| Range | 29-79 | 19-82 | |
|
| |||
| Sex (%) | |||
| Male | 29 (58%) | 82 (61%) | |
| Female | 21 (42%) | 53 (39%) | |
|
| |||
| SNOT-20 score (mean) | 27.8 | 26.2 | p=.36 (smokers vs. non-smokers) |
|
| |||
| Revision surgery (%) | 10 (20%) | 53 (39%) | p=.38 (smokers vs. non-smokers) |
|
| |||
| Nasal Polyposis (%) | 11 (22%) | 67 (50%) | p=.14 (smokers vs. non-smokers) |
|
| |||
| Asthma (%) | 10 (20%) | 62 (46%) | p=.16 (smokers vs. non-smokers) |
|
| |||
| Preop Lund Mackay CT score (mean) | 7.4 | 9.2 | p=.15 (smokers vs. non-smokers) |
|
| |||
| Preop Endoscopy Score (mean) | 3.9 | 5.0 | p=.13 (smokers vs. non-smokers) |
|
| |||
| Follow-up, months (mean) | 40.3 | 44.2 | |
Of the 235 patients who enrolled in the study, 221 (94%) patients had short-term postoperative data, and 137 (58%) had long-term data available for evaluation. At short-term followup (mean = 3.1 months), both groups received a highly significant reduction in SNOT-20 scores (p<0.0005). Smokers had an improvement from a mean of 27.8 to 5.7 (mean improvement of 22.1). Non-smokers had an improvement from a mean of 26.2 to 10.1 (mean improvement of 16.1). Smokers had a statistically significant greater reduction (22.1 vs. 16.1) in SNOT-20 scores than non-smokers (p=.044). In short-term post-operative endoscopy scores, non-smokers improved from a mean of 5.0 pre-operatively to 0.8 post-operatively. Smokers improved from a mean of 3.9 pre-operatively to 0.1 post-operatively.
At long-term followup, 9 of 49 (18%) smokers reported that they were no longer smoking. 26 smokers had long-term data to evaluate (mean followup 40.3 months) and had a mean SNOT-20 score of 8.3. 115 of 185 (62%) non-smokers had long-term data to evaluate (mean followup 44.2 months). None reported that they began smoking. Non-smokers had a long-term mean SNOT-20 score of 11.4. See Table 2 and Figures 1 and 2.
Table 2.
Post-operative Quality of Life Results
| Smokers | Non-smokers | ||
|---|---|---|---|
|
| |||
| Number of Patients (preop) | 49 | 172 | |
|
| |||
| Preop SNOT-20 (mean) | 27.8 | 26.2 | |
| 95% CI (24.3 to 31.3) | 95% CI (24.4 to 28.0) | ||
|
| |||
| Short Term Postop SNOT-20 | 5.7 | 10.1 | Smokers p<0.0005 |
| 95% CI (1.4 to 10.0) | 95% CI (8.2 to 12.1) | Non-smokers p<0.0005 | |
|
| |||
| Short Term SNOT-20 improvement | 22.1 | 16.1 | p=0.044 (smokers vs. non-smokers) |
|
| |||
| Long Term Postop SNOT-20 | 8.3 | 11.4 | |
| 95% CI (4.3 to 12.3) | 95% CI (9.0 to 13.8) | ||
|
| |||
| Short to Long Term Change in SNOT-20 score | 2.6 | 1.3 | Smokers p = .25 |
| Non-smokers p = .10 | |||
|
| |||
| Long Term SNOT-20 improvement | 19.5 | 14.8 | Smokers p <0.0001 |
| Non-smokers p <0.0001 | |||
Figure 1.
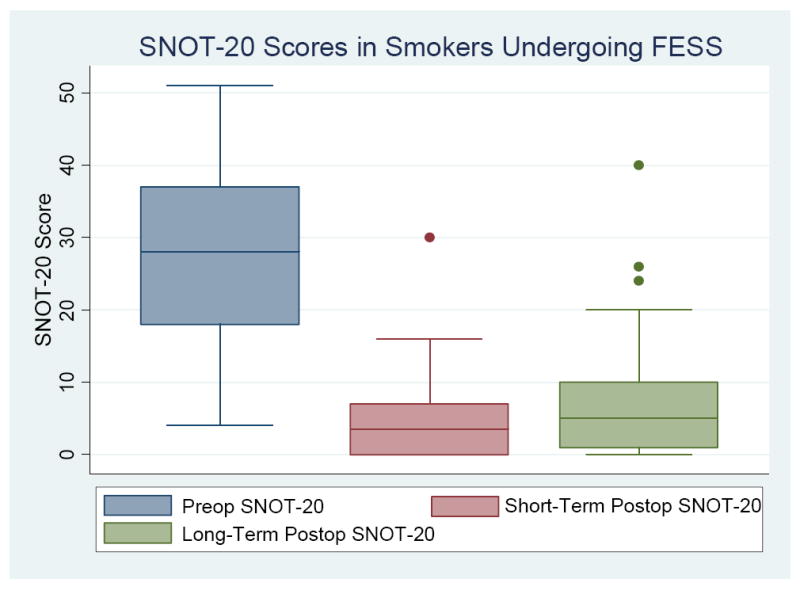
Boxplot of SNOT-20 Scores in Smokers Undergoing FESS
Figure 2.
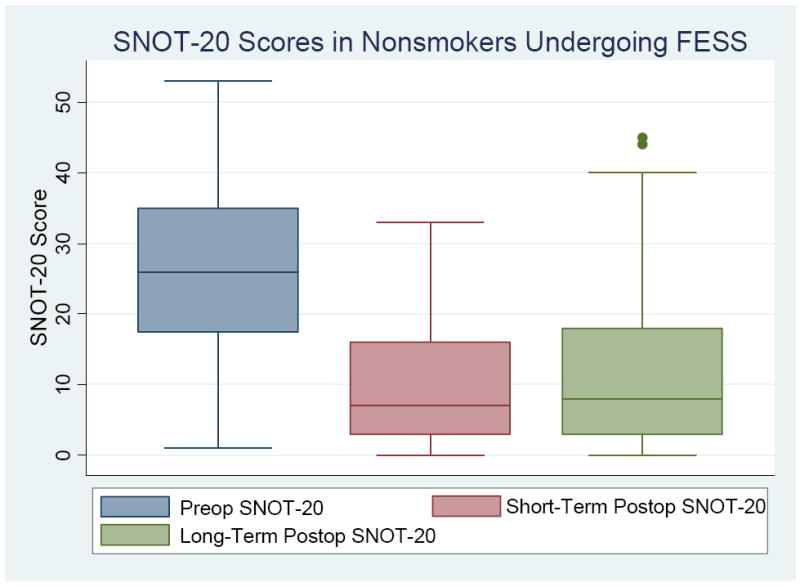
Boxplot of SNOT-20 Scores in Non-smokers Undergoing FESS
Discussion
Smoking remains the greatest cause of preventable medical morbidity and many rhinologists have refused to offer functional endoscopic sinus surgery to active smokers who suffer from chronic rhinosinusitis. Retrospective data analysis from Senior et.al.1 and other studies8 supported the notion that ongoing smokers had poorer outcomes from FESS compared to non-smokers. From 2003 to 2006, we prospectively enrolled patients undergoing functional endoscopic sinus surgery for chronic rhinosinusitis in a clinical outcomes study expecting to corroborate these earlier studies2. Initially, we evaluated short-term outcomes for smokers and non-smokers. We confirmed previously reported findings that both smokers and non-smokers obtain highly significant improvements in quality of life from functional endoscopic sinus surgery, however, we were surprised to see that smokers had a marginally statistically significant (though not clinically significant) improvement in SNOT-20 scores compared to non-smokers at short-term followup. At that time, we speculated that longer follow-up would be needed and that possibly, quality of life outcomes would deteriorate over time for ongoing smokers, which would be consistent with the trends seen in the long-term study from Senior et. al.1
Therefore, we have followed these cohorts and are now able to report on quality of life outcomes with a mean followup of 43.5 months. Both smokers and non-smokers maintained a highly statistically significant and clinically significant improvement in their SNOT-20 scores. While both smokers and non-smokers had a slight deterioration in the improvements obtained in their SNOT-20 scores, these were relatively small and likely of minimal clinical significance. These results are consistent with other prospective studies9 evaluating the benefits of endoscopic sinus surgery on quality of life.
It is important to note that from this study, it is not rational to conclude that continued smoking does not worsen outcomes following sinus surgery, nor that smokers have better outcomes from sinus surgery compared to non-smokers. Rather, smoke-induced chronic rhinosinusitis is likely a different subset of disease10 than that suffered by many non-smokers who seek rhinologic care for the management of their disease. Indeed, while both smokers and non-smokers had similar preop SNOT-20 scores in this prospective study, non-smokers had higher rates of nasal polyposis, asthma, and histories of multiple revision surgeries. The higher rate of nasal polyposis in our non-smoking population is different from a recent retrospective review of patients undergoing surgery for chronic rhinosinusitis which demonstrated that 32 light smokers had a higher risk for polyps but 21 heavy smokers had a reduced risk for polyps.11 Long-standing research has suggested that smoke-induced respiratory epithelial dysfunction is mediated through mucociliary dysfunction12; functional endoscopic sinus surgery is currently thought to be more effective in improving mucociliary clearance relative to other types of pathogenesis such as innate immune dysfunction, etc.
It is interesting that 9 of 49 (18.4%) patients quit smoking after their operation in this study. While this number of patients was too small to allow for robust statistical analysis, this would make for an interesting comparison group to active smokers. Comparing this group to patients who continued to smoke after their operation would give a better understanding of the deleterious effects of persistent smoking on sinus surgery outcomes.
This study is limited in its general applicability by occurring at a single, tertiary care institution, and by its significant dropout rate over the course of long-term followup in both cohorts. Initially, 94% of patients had short-term data to evaluate, whereas only 54% of patients had long-term data to evaluate. While smokers and non-smokers were expected to dropout for similar reasons, differences in dropout rates and causes between the two cohorts could introduce a significant reporting/treatment bias. In addition, many patients reported quality-of-life data via telephone surveys. This is somewhat understandable given the costs incurred by the patient for receiving endoscopic followup exams, for which the majority of patients had greatly improved symptoms. Also, the SNOT-20 does not contain questions regarding nasal congestion or blockage. There are currently less than 30 patients in the smoking cohort with long-term endoscopy scores, precluding robust statistical comparisons on long-term objective outcomes between cohorts. Nevertheless, what can be concluded from this prospective study is that both smokers and non-smokers obtained a clinically significant and highly statistically significant (P<0.0001) improvement in their SNOT-20 scores that was present at both short-term and long-term followup. As a result, it does not appear rational to deny active smokers the option of functional endoscopic sinus surgery for chronic rhinosinusitis if the main goal of this surgery is improvement in quality of life.
Conclusion
Both smokers and non-smokers continue to maintain a highly significant improvement (p<0.0001) in SNOT-20 scores following endoscopic sinus surgery at long-term followup. While smoking remains a well documented cause of medical morbidity, smokers maintained an improvement in quality of life after long-term followup (mean 40.3 months) from endoscopic sinus surgery in this prospective study. Therefore, smoking status by itself should not be an absolute contraindication to functional endoscopic sinus surgery as a treatment for chronic rhinosinusitis.
Acknowledgments
This work was supported, in part, by a grant from the National Institutes of Health (Das)
Footnotes
This work was performed at the Medical College of Georgia, Augusta, GA.
This work was presented at the 2009 Middle Section Meeting of the Triological Society, Bonita Springs, Florida, January 8-11, 2009
Contributor Information
Subinoy Das, Department of Otolaryngology-Head and Neck Surgery, The Ohio State University, Columbus, Ohio.
Sunny S. Khichi, Department of Otolaryngology-Head and Neck Surgery, Medical College of Georgia, Augusta, Georgia.
Helen Perakis, Department of Otolaryngology-Head and Neck Surgery, Medical College of Georgia, Augusta, Georgia.
Troy Woodard, Department of Otolaryngology-Head and Neck Surgery, Medical College of Georgia, Augusta, Georgia.
Stilianos E. Kountakis, Department of Otolaryngology-Head and Neck Surgery, Medical College of Georgia, Augusta, Georgia.
Bibliography
- 1.Senior BA, Kennedy DW, Tanabodee J, et al. Long-term Results of Functional Endoscopic Sinus Surgery. Laryngoscope. 1998 Feb;108(2):151–157. doi: 10.1097/00005537-199802000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Das S, Becker AM, Perakis H, Prosser JD, Kountakis SE. The Effects of Smoking on Short-Term Quality of Life Outcomes in Sinus Surgery. Laryngoscope. 2007 Dec;117(12):2229–2232. doi: 10.1097/MLG.0b013e318145388f. [DOI] [PubMed] [Google Scholar]
- 3.Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997;117:S1–S7. doi: 10.1016/S0194-59989770001-9. [DOI] [PubMed] [Google Scholar]
- 4.Lund VJ, Mackay IS. Staging in Rhinosinusitis. Rhinology. 1993;31(4):183–184. [PubMed] [Google Scholar]
- 5.Lund VJ, Kennedy DW. Quantification for staging sinusitis. International Conference on Sinus Disease: terminology, staging, therapy. Ann Otol Rhinol Laryngol. 1995;1004(suppl):17–21. [PubMed] [Google Scholar]
- 6.Piccirillo JF, Merritt MG, Richards ML. Psychometric and clinimetric validity of the 20-item Sino-Nasal Outcome Test (SNOT-20) Otolaryngol Head Neck Surg. 2002;126:41–47. doi: 10.1067/mhn.2002.121022. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Cigarette smoking among adults–United States, 2004. MMWR. 2005;54:1121–4. [PubMed] [Google Scholar]
- 8.Briggs RD, Wright ST, Cordes S, et al. Smoking in Chronic Rhinosinusitis: A Predictor of Poor Long-Term Outcome After Endoscopic Sinus Surgery. Laryngoscope. 2004;114(1):126–128. doi: 10.1097/00005537-200401000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Smith TL, Mendolia-Loffredo S, Loehrl TA, Sparapani R, Laud PW, Nattinger AB. Predictive factors and outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2005 Dec;115(12):2199–205. doi: 10.1097/01.mlg.0000182825.82910.80. [DOI] [PubMed] [Google Scholar]
- 10.Kennedy DW. Pathogenesis of chronic rhinosinusitis. Ann Otol Rhinol Laryngol Suppl. 2004 May;193:6–9. doi: 10.1177/00034894041130s503. [DOI] [PubMed] [Google Scholar]
- 11.Houser SM, Keen KJ. The Role of Allergy and Smoking In Chronic Rhinosinusitis and Polyposis. Laryngoscope. 2009 Jan;118(9):1521–7. doi: 10.1097/MLG.0b013e31817d01b8. [DOI] [PubMed] [Google Scholar]
- 12.Cohen D, Arai SF, Brain JD. Smoking impairs long-term dust clearance from the lung. Science. 1979;204:514–517. doi: 10.1126/science.432655. [DOI] [PubMed] [Google Scholar]


