Abstract
Objective:
At-risk drinking and alcohol use disorders are common in primary care and may adversely affect the treatment of patients with diabetes and/or hypertension. The purpose of this article is to report the impact of dissemination of a practice-based quality improvement approach (Practice Partner Research Network-Translating Research into Practice [PPRNet-TRIP]) on alcohol screening, brief intervention for at-risk drinking and alcohol use disorders, and medications for alcohol use disorders in primary care practices.
Method:
Nineteen primary care practices from 15 states representing 26,005 patients with diabetes and/or hypertension participated in a group-randomized trial (early intervention vs. delayed intervention). The 12-month intervention consisted of practice site visits for academic detailing and participatory planning and network meetings for “best practice” dissemination.
Results:
At the end of Phase 1, eligible patients in early-intervention practices were significantly more likely than patients in delayed-intervention practices to have been screened (odds ratio [OR] = 3.30, 95% CI [1.15, 9.50]) and more likely to have been provided a brief intervention (OR = 6.58, 95% CI [1.69, 25.7]. At the end of Phase 2, patients in delayed-intervention practices were more likely than at the end of Phase 1 to have been screened (OR = 5.18, 95% CI [4.65, 5.76]) and provided a brief intervention (OR = 1.80, 95% CI [1.31, 2.47]). Early-intervention practices maintained their screening and brief intervention performance during Phase 2. Medication for alcohol use disorders was prescribed infrequently.
Conclusions:
PPRNet-TRIP is effective in improving and maintaining improvement in alcohol screening and brief intervention for patients with diabetes and/or hypertension in primary care settings.
At least 20% of primary care patients show signs of either at-risk drinking or an alcohol use disorder (AUD; abuse or dependence) (Manwell et al., 1998). Alcohol use to this extent causes or exacerbates a number of medical conditions seen in primary care. In particular, hypertension and diabetes mellitus—the first and third most common diagnoses in primary care, respectively (Woodwell and Cherry, 2004)—are especially sensitive to alcohol, which compromises clinical management of these conditions.
Primary care provides a unique opportunity for alcohol screening and intervention because the majority of adults visit a physician at least once a year (Pleis et al., 2010). Patients have an ongoing, trusting relationship with their physicians and expect to receive prevention and lifestyle advice from them (Miller et al., 2006b; Saitz et al., 2010). In addition, reimbursement for alcohol screening and brief intervention (SBI) is available through commercial insurance Current Procedural Terminology codes, Medicare G codes, and Medicaid Healthcare Common Procedure Coding System codes.
For nondependent, at-risk drinkers, SBI is effective in reducing alcohol consumption (Whitlock et al., 2004) and can lead to improvements in blood pressure control in hypertensive patients (Rose et al., 2008). Medications may also help reduce alcohol consumption. U.S. Food and Drug Administration (FDA)–approved medications include disulfiram, naltrexone (both oral or injectable), and acamprosate; topiramate is also effective, although not FDA approved for AUDs (Kenna et al., 2009; National Institute on Alcohol Abuse and Alcoholism, 2008). Although treatment effects are modest, medications for alcohol dependence in conjunction with either brief support or more extensive psychosocial therapy can be effective in both primary and specialty care medical settings (Miller et al., 2011). Current National Institute on Alcohol Abuse and Alcoholism (NIAAA) clinical guidelines encourage physicians to consider the use of medications and chronic disease management for their alcohol-dependent patients (NIAAA, 2007, 2008).
Alcohol SBI is not routinely integrated into primary care practice, although multi-component, theoretically sound (Damschroder and Hagedorn, 2011) practice-based inter ventions have been shown to improve alcohol SBI in these settings (Williams et al., 2011). One of these interventions is the Practice Partner Research Network-Translating Research into Practice (PPRNet-TRIP) model, which combines audit and feedback, practice site visits for academic detailing and participatory planning, and network meetings to share “best practice” approaches (Miller et al., 2006a; Rose et al., 2008). Additional research is needed, however, on the sustainability of such interventions over time and on interventions to increase the use of medications for AUDs in primary care. Particularly important are interventions among patients with hypertension and/or diabetes, given their prevalence and the adverse effects of at-risk drinking or AUDs on their clinical management discussed earlier.
The primary objectives of the present study were to (a) assess the impact of an updated PPRNet-TRIP model on alcohol SBI and use of medication for AUDs in adult patients with diagnoses of hypertension and/or diabetes and (b) investigate the sustained effects of PPRNet-TRIP for 1 year after it was completed.
Method
Study design
The institutional review board of the Medical University of South Carolina approved the study. The study design was a delayed-intervention, group-randomized trial. It was conducted in 20 primary care practices throughout the United States from March 2009 to October 2011. The study assessed the impact of PPRNet-TRIP’s on-site visits and network meetings in comparison with passive dissemination of guidelines, electronic health record (EHR) tools, and audit and feedback on alcohol SBI and use of medications for AUDs. A crossover design was used in which the early-intervention group received on-site visits and participated in the network meeting during 1 year, and the delayed-intervention group served as the control. At the end of 1 year, the delayed-intervention group participated in a joint network meeting with the early-intervention group and received on-site visits, whereas the early-intervention group did not. This design allowed us to study the sustained effects of the on-site visit and network meeting interventions on the study outcomes. The study timeline is illustrated in Table 1.
Table 1.
Timeline of study activities
| Participants |
|||
| Activity | Dates | EI group | DI group |
| Pre-intervention on-site visit | 03/2009–05/2009 | X | X |
| Quarterly practice performance reports | 10/2009–10/2011 | X | X |
| Network meeting | 09/10/2009 | X | |
| Intervention on-site visits | 10/2009–12/2009 | X | |
| Intervention on-site visits | 04/2010–05/2010 | X | |
| Network meeting | 09/22/2010 | X | X |
| Intervention on-site visits | 10/2010–12/2010 | X | |
| Intervention on-site visits | 04/2011–05/2011 | X | |
Notes: EI = early intervention; DI = delayed intervention.
Setting and population
Twenty primary care practices were recruited from PPRNet, a nationwide, practice-based quality improvement and research network in which all practices use a common EHR system (Practice Partner, McKesson Corporation, Alpharetta, GA). Voluntary practice participation was solicited via email over the network list-serve. The first 20 practices volunteering for the study were matched on number of patient visits per full-time provider per week (a calculated variable to reflect the overall patient care load of the practice). After this matching, practices were randomized to either the early-intervention group (10 practices) or the delayed-intervention group (10 practices).
Pre-intervention on-site visit
All practices (both early intervention and delayed intervention) received a pre-intervention on-site visit by two study investigators (S.M.O., P.M.M., or A.M.W.) to explain the study and to ensure that EHR documentation by both groups could be captured within data extracted for analysis by the research team. Practices were provided with a point-of-care EHR alcohol screening/intervention template (devised by us based on the NIAAA guidelines) to provide a prompt for alcohol screening, brief intervention, and/or use of medication for AUDs. The point-of-care EHR also provided automatic documentation of these activities in structured fields to ensure recording of relevant data elements for analyses. The template was based on branching logic. It first asked whether the patient “sometimes drinks beer, wine, or other alcoholic beverages.” If the response was negative, the screening was complete. If the response was positive, the single-question at-risk drinking question (“How many times in the past year have you had five or more drinks in a day [for men]/four or more drinks in a day [for women]?”) was prompted. If that response was negative, the screening was complete; if not, there was additional branching logic to assess the presence of AUDs and make brief-intervention and treatment recommendations. The brief-intervention message recommended advising the patient that he or she was drinking more than what was medically safe and advised the patient to stay within safe drinking limits, specified based on gender. It also provided information about the “Rethinking Drinking” brochure (NIAAA, 2010) and website (http://rethinkingdrinking.niaaa.nih.gov) and suggested specific approaches for patients who were ready to cut down on their drinking and other approaches for those who were not. For patients with an AUD, recommendations were made to refer the patient to a self-help group such as Alcoholics Anonymous; for those with evidence of dependent drinking, the recommendation was to consider either referral to an addictions specialist or the use of medication.
Practices could choose to adopt the template as provided; to include its content in progress note templates for hypertension, diabetes, and/or general medical exams; or to have nursing staff document the initial screening question(s) in vital signs, which would prompt the EHR to embed the remainder of the template in that day’s point-of-care progress note for patients who screened positive for at-risk drinking.
During this pre-intervention visit, practices were asked to designate two practice-based project liaisons—one clinical provider and one nursing staff member—to assist in scheduling our on-site visits, to coordinate follow-through between the on-site visits, and to represent practices at network meetings.
Intervention Phase 1
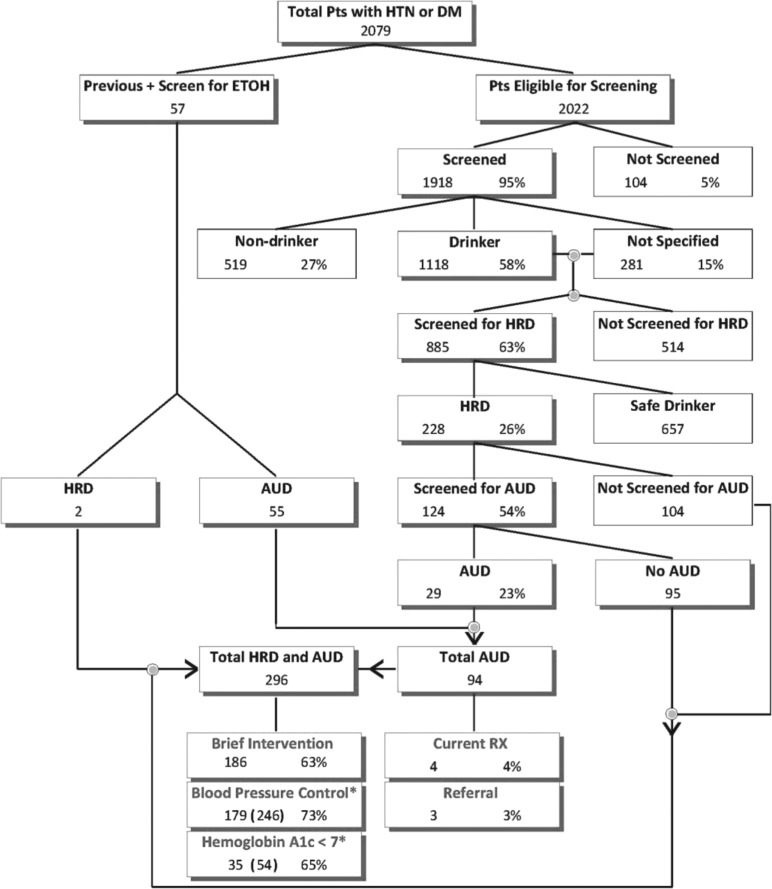
Intervention Phase 1 began in late September 2009 and ran for 1 year. Both early-intervention and delayed-intervention practices received quarterly practice performance reports detailing their screening, evaluation, and management processes for alcohol conditions for their patients with hypertension and/or diabetes. Performance reports were generated after quarterly data extracts from the EHR at each participating practice using an approach documented elsewhere (Ornstein et al., 2008). For this study, the reports, using a flowchart design, provided information on the proportion of appropriate patients screened for alcohol use, the proportion of drinkers screened for at-risk drinking, the proportion of at-risk drinkers for whom brief intervention was provided, and the proportion of patients diagnosed with AUDs who were prescribed medication. An example of this report is shown in Figure 1. In this phase, early-intervention practices also participated in one network meeting and received two on-site visits from study investigators. Delayed-intervention practices had no other study activities during this phase.
FIGURE 1.
Example of practice performance report. Pts = patients; HTN = hypertension; DM = diabetes mellitus; ETOH = ethanol; HRD = high-risk drinker; AUD = alcohol use disorder; RX = prescription. Screening, brief intervention, and/or referral were within 2 years. *Blood pressure control and/or hemoglobin A1c < 7 was within 6 months.
The network meeting was held in Charleston, SC. During the meeting, additional information beyond that discussed at the pre-intervention on-site visit was presented on topics including the EHR alcohol screening/intervention template, barriers and facilitators to SBI, referral, and medications for AUDs. Small group discussions among liaisons with similar roles were also conducted. The provider group shared early successes in implementing the revised NIAAA guidelines and overcoming barriers to alcohol SBI. The nursing staff group discussion also highlighted early successes and facilitators to screening, specifically regarding the use of “scripts” for alcohol screening. Ample time was provided for practice liaisons to discuss possible barriers and facilitators to alcohol SBI and medication use. Finally, each pair of practice liaisons developed an implementation plan to share with others in their practice. The plans included activities such as delegation of screening to nursing staff, staff and provider education on NIAAA guidelines, integration of patient education from the “Rethinking Drinking” website on practice websites or via brochures, and use of the alcohol screening/intervention template and embedding this template in other problem-based templates.
The two on-site visits provided an opportunity for project investigators to work with all practice health care providers and staff. Approximately 2 hours were spent in a group session to present new literature concerning alcohol disorders in primary care, review their most recent practice performance report, and provide additional training and updating, if needed, of the EHR alcohol screening/intervention template. Additionally, evidence on the efficacy and practical use of medications for AUDs (i.e., dosing, tolerability, and cost), along with case examples from the project investigators’ practices, was reviewed. Specific focus was provided on helping individual clinicians and staff with SBI by asking them to discuss experiences they had recently had with these activities. Because most practices had delegated their clinical staff (mostly medical assistants) to conduct the initial screening, discussion frequently centered on successes and problems these individuals had encountered during screening. Health care providers were asked to discuss their experiences in the project with medication for AUDs for their patients. Visits concluded with participatory planning, where practice members set goals for the next phase of the project, deciding what implementation plans to continue and what processes needed refinement or warranted further improvement. Common plans during this phase included continuation or reinforcement of the nursing staff role in screening with reminders for specific wording of the single-question “at-risk” screen, provider commitment to improving recognition of patients eligible for brief intervention, referral and/or medication for AUDs, and consideration of prescribing medications in those patients. Project investigators and practice liaisons met following the group session to work through any practice-specific barriers to implementing these plans. In some practices, this included troubleshooting problems in the implementation of the alcohol screening/intervention EHR template and practice development consultation and coaching on team engagement or practice redesign of SBI processes.
Intervention Phase 2
Intervention Phase 2 began in late September 2010 and ran for 1 year. At the beginning, a joint network meeting was held in Charleston, SC. It was attended by project liaisons from all participating practices (i.e., both early intervention and delayed intervention). The purpose of this meeting was for researchers and the delayed-intervention group to learn from early-intervention practices about their experiences with alcohol SBI and medication use. In addition, they were to learn the strategies that were most useful for adopting these activities. The delayed-intervention practices group was asked to develop an implementation plan for its practices, and the early-intervention practices group was asked to develop plans for sustaining its existing strategies. For the remainder of Intervention Phase 2, the early-intervention practices group continued to receive quarterly practice performance reports but participated in no other study activities. The delayed-intervention practices group had two on-site visits during this phase, with the same purpose and format as discussed previously.
Outcomes
The primary outcomes of the study were documentation in the EHR for active patients with hypertension and/or diabetes of (a) screening for alcohol use; (b) brief intervention for those with at-risk drinking or an AUD; and (c) a prescription for disulfiram, naltrexone (oral or injectable), acamprosate, or topiramate for those with an AUD. At any time, an active patient was defined as one with a progress note in the EHR within the past 365 days. Outcomes were assessed at the end of the first and second intervention phases. SBI was defined as any such documentation in the prior 2 years from the assessment dates. Documentation of SBI was based on data in vital signs, health maintenance, laboratory tables, problem lists, risk tables, or any combination of the above. A prescription was defined as one with a date within the prior year that had not been discontinued and was based on data from the medication section of the EHR.
Statistical analysis
The primary analyses involved comparing the two study groups with regard to three study outcomes at the end of Intervention Phase 1. To assess the sustainability of the intervention, the secondary analyses compared early-intervention practice outcomes measured at the end of Intervention Phase 1 to those at the end of the second intervention phase. Generalized linear mixed models (McCulloch, 2001) were constructed for each outcome using SAS Version 9.3 (SAS Institute Inc., Cary, NC) to test the various study hypotheses. Generalized linear mixed models are ideal for handling clustering of patients within practices, and they allowed us to compare outcomes between patients in early-intervention and delayed-intervention practices and within patients over time. Compound symmetry covariance structures were used to model the correlation among outcomes on patients within the same practices and among outcomes within the same individuals.
Results
After randomization and pre-intervention site visits, but before any study interventions, one of the delayed-intervention practices closed and was withdrawn from the study. Nineteen practices (10 early intervention and 9 delayed intervention) completed Phase 1 of the study. These practices were located in 15 states, in both rural and urban areas. The number of providers per practice ranged from 1 to 10; in all, there were 77 providers (63 physicians, 9 nurse practitioners, and 5 physician assistants). For early-intervention practices, 15,053 patients were active during the study. Mean age was 60.6 years (SD = 15.0), with 43.3% being male. For delayed-intervention practices, 10,952 patients were active during the study. Mean age was 60.0 years (SD = 15.0), with 44.6% being male. Using a generalized linear mixed model to account for patients within practices, no differences in age or gender were found between the groups. During Intervention Phase 2, one early-intervention practice closed, one delayed-intervention practice closed, and another delayed-intervention practice withdrew its agreement to participate because of staffing changes. These three withdrawals left nine early-intervention practices and seven delayed-intervention practices with complete data at the end of Phase 2.
Study outcome measures are summarized in Table 2. At the end of Phase 1, eligible patients in early-intervention practices were significantly more likely than patients in delayed-intervention practices to have been screened for alcohol use (odds ratio [OR] = 3.30, 95% CI [1.15, 9.50]) and more likely to have been provided a brief intervention (OR = 6.58, 95% CI [1.69, 25.7]). At the end of Phase 1, use of medications for AUDs was low among patients in both early-intervention (2.6%) practices and delayed-intervention practices (0.0%). At the end of Phase 2, patients in delayed-intervention practices were significantly more likely than at the end of Phase 1 to have been screened for alcohol use (OR = 5.18, 95% CI [4.65, 5.76]) and more likely to have been provided a brief intervention (OR = 1.80, 95% CI [1.31, 2.47]). At the end of Phase 2, use of medications in delayed-intervention practices had increased to the level seen in early-intervention practices after Phase 1. During Phase 2, alcohol SBI remained high and relatively unchanged among early-intervention practices; use of medications significantly increased (OR = 2.24, 95% CI [1.03, 4.88]) during Phase 2.
Table 2.
Results of the multivariable statistical analyses on screening, brief intervention, and medication use across two phases of the study
| DI practices |
EI practices |
||||||
| Study outcome | End of Phase 1: % (n total eligible patients) | End of Phase 2: % (n total eligible patients) | aOR: Phase 2 vs. Phase 1 [95% CI] | End of Phase 1: % (n total eligible patients) | End of Phase 2: % (n total eligible patients) | aOR: Phase 2 vs. Phase 1 [95% CI] | aOR: EI vs. DI practices, end of Phase 1 [95% CI] |
| Screening for alcohol use | 69.4% (8,741) | 91.1% (7,916) | 5.18 [4.65, 5.76] | 81.6% (12,252) | 82.2% (11,712) | 1.07 [1.00, 1.15] | 3.30a [1.15, 9.50] |
| Brief intervention for ARD or AUD | 30.9% (362) | 47.1% (713) | 1.80 [1.31, 2.47] | 58.1% (1,278) | 56.2% (1,371) | 0.90 [0.76, 1.06] | 6.58a [1.69, 25.7] |
| Medication prescription for AUD | 0.0% (280) | 2.4% (297) | n.e. | 2.6% (383) | 5.5% (380) | 2.24a [1.03, 4.88] | n.e. |
Notes: DI = delayed intervention; EI = early intervention; aOR = adjusted odds ratio; CI = confidence interval; ARD = at-risk drinking; AUD = alcohol use disorder; n.e. = not estimable because of small proportions of subjects receiving medication.
p < .05 by F test from generalized linear mixed model.
Discussion
Three important findings are evident from this study. First, a more intensive intervention—adding on-site visits for academic detailing, training on tools and techniques, and participatory planning plus network meetings for “best practice” dissemination—is more effective than passive dissemination of guidelines, EHR tools, and audit and feedback on alcohol SBI and use of medications for AUDs. Second, the impact of the more intensive intervention is sustained for at least 1 year after it ends. Third, adoption of prescribing medications for AUDs occurs more slowly than SBI. During the study, the vast majority of patients with diabetes mellitus and/or hypertension were screened for alcohol misuse. More than half of those with at-risk drinking or an AUD received brief intervention. A small but increasing proportion of those with AUDs was prescribed medication. Medication use may be infrequent because medications currently are approved by the FDA to treat only alcohol dependence, not at-risk drinking or alcohol abuse.
From our observations at site visits and discussions at the network meetings, we speculate that the key strategy most responsible for SBI successes was the decision by all practices to delegate at least some portion of the screening process to their nursing staff, in many cases recording the finding as a vital sign. This specific approach has been shown by others to increase the proportion of patients screened (Seale et al., 2010). For the most part, physicians retained the responsibility for doing the assessment for AUDs and providing brief intervention, although nursing staff were often involved in providing education tools (e.g., “Rethinking Drinking”).
Given the heterogeneous designs of other studies, it is difficult to compare our findings with others. Based on a recent review (Williams et al., 2011), our SBI proportions are comparable to the best results of other studies. Indeed, one of these studies was our prior intervention (Rose et al., 2008), and our screening proportions in the current study are much higher than the 64.5% found in that study. A possible reason for this improvement in comparison with our earlier study is that we have fine-tuned our intervention to include more of the constructs thought to be associated with successful implementation as described in the recently developed Consolidated Framework for Implementation Research (Damschroder and Hagedorn, 2011).
In the terminology of the Consolidated Framework for Implementation Research, the strengths of our initial model retained in the present study were in the “inner setting” and “implementation process.” The inner setting strengths refer to the use of the EHR system for both clinical decision support and documentation of relevant outcomes, provision of goals and feedback, and meetings to share best practice approaches in a learning environment. The implementation process strengths include utilizing participatory planning with each practice, engaging internal implementation leaders as practice champions, using external change agents, and utilizing ongoing reflection on the impact of the practice efforts on clinical outcomes. In the present study, we focused additional attention on “characteristics of individuals” and “intervention characteristics.” To enhance our emphases on the characteristics of individuals, we attended to both clinician and staff knowledge and beliefs about the importance of SBI, encouraged participants to share positive experiences during network meetings to build enthusiasm for the intervention, addressed their self-efficacy through role-playing at site visits, and stressed the importance of clinical staff viewing themselves as health care providers. To improve the intervention characteristics, we stressed the relative advantage of the one-question screen, limited the complexity of the EHR tools, and suggested that practices try different approaches to screening and adapt the best approach to their unique circumstances.
Although the number of prescriptions for medication for AUDs increased over time, unfortunately, recent primary-care alcohol prescription data with which to compare our findings are not currently available. An estimate from retail sales data now 10 years old suggested that, at most, approximately 9% of the population needing alcoholism treatment received the equivalent of a single prescription in 1 year (Mark et al., 2009), and many of these prescriptions were written by psychiatrists.
There are several limitations of our study. First, participating practices were volunteers from among members of a practice-based research network, users of a common fully functional EHR. These practices may not be representative of average primary care practices in the community. Second, we combined the diagnoses “alcohol abuse disorder” and “alcohol dependence” into a single “alcohol use disorder” for our academic detailing, EHR template, and analyses. Such an approach is simpler for the primary care clinician and is being proposed for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (American Psychiatric Association, 2012), but it is not yet in widespread use. Finally, as with any research using data from EHR, the findings represent what is documented in the EHR and are not corroborated by other data sources, such as patient interviews or prescription fill sources.
Nonetheless, our findings suggest that primary care practices provided with a comprehensive yet simple model can successfully implement SBI for alcohol disorders and sustain these interventions after active support is withdrawn. Implementation research in a larger number of primary care practices is needed to test the effectiveness of our model for SBI more broadly, as are other studies focused on appropriate use of medication for AUDs.
Footnotes
This study was funded by National Institute on Alcohol Abuse and Alcoholism Grant R01AA016768.
References
- American Psychiatric Association. DSM-5 Development. 2012 Retrieved from http://www.dsm5.org/Pages/Default.aspx. [Google Scholar]
- Damschroder LJ, Hagedorn HJ. A guiding framework and approach for implementation research in substance use disorders treatment. Psychology of Addictive Behaviors. 2011;25:194–205. doi: 10.1037/a0022284. [DOI] [PubMed] [Google Scholar]
- Kenna GA, Lomastro TL, Schiesl A, Leggio L, Swift RM. Review of topiramate: An antiepileptic for the treatment of alcohol dependence. Current Drug Abuse Reviews. 2009;2:135–142. doi: 10.2174/1874473710902020135. [DOI] [PubMed] [Google Scholar]
- Manwell LB, Fleming MF, Johnson K, Barry KL. Tobacco, alcohol, and drug use in a primary care sample: 90-day prevalence and associated factors. Journal of Addictive Diseases. 1998;17:67–81. doi: 10.1300/J069v17n01_07. [DOI] [PubMed] [Google Scholar]
- Mark TL, Kassed CA, Vandivort-Warren R, Levit KR, Kranzler HR. Alcohol and opioid dependence medications: Prescription trends, overall and by physician specialty. Drug and Alcohol Dependence. 2009;99:345–349. doi: 10.1016/j.drugalcdep.2008.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCulloch CESS. Generalized, linear, and mixed models. New York, NY: John Wiley & Sons; 2001. [Google Scholar]
- Miller PM, Book SW, Stewart SH. Medical treatment of alcohol dependence: A systematic review. International Journal of Psychiatry in Medicine. 2011;42:227–266. doi: 10.2190/PM.42.3.b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller PM, Stockdell R, Nemeth L, Feifer C, Jenkins RG, Liszka H, Wessell A. Initial steps taken by nine primary care practices to implement alcohol screening guidelines with hypertensive patients: The AA-TRIP project. Substance Abuse. 2006a;27:61–70. doi: 10.1300/J465v27n01_08. [DOI] [PubMed] [Google Scholar]
- Miller PM, Thomas SE, Mallin R. Patient attitudes towards self-report and biomarker alcohol screening by primary care physicians. Alcohol and Alcoholism. 2006b;41:306–310. doi: 10.1093/alcalc/agl022. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician’s guide, updated 2005 edition (NIH Publication No. 07–3769) 2007 Retrieved from http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Prescribing medications for alcohol dependence. Excerpt from Helping patients who drink too much: A clinician’s guide, October 2008 update (NIH Publication No. 07–3769) 2008 Retrieved from http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/PrescribingMeds.pdf. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Rethinking drinking (NIH Publication No. 10–3370) Bethesda, MD: Author; 2010. Retrieved from http://pubs.niaaa.nih.gov/publications/RethinkingDrinking/Rethinking_Drinking.pdf. [Google Scholar]
- Ornstein S, Nietert PJ, Jenkins RG, Wessell AM, Nemeth LS, Rose HL. Improving the translation of research into primary care practice: Results of a national quality improvement demonstration project. Joint Commission Journal on Quality and Patient Safety. 2008;34:379–390. doi: 10.1016/s1553-7250(08)34048-3. [DOI] [PubMed] [Google Scholar]
- Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. Hyattsville, MD: U.S. Department of Health and Human Services; 2010. [PubMed] [Google Scholar]
- Rose HL, Miller PM, Nemeth LS, Jenkins RG, Nietert PJ, Wessell AM, Ornstein S. Alcohol screening and brief counseling in a primary care hypertensive population: A quality improvement intervention. Addiction. 2008;103:1271–1280. doi: 10.1111/j.1360-0443.2008.02199.x. [DOI] [PubMed] [Google Scholar]
- Saitz R, Alford DP, Bernstein J, Cheng DM, Samet J, Palfai T. Screening and brief intervention for unhealthy drug use in primary care settings: Randomized clinical trials are needed. Journal of Addiction Medicine. 2010;4:123–130. doi: 10.1097/ADM.0b013e3181db6b67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seale JP, Shellenberger S, Velasquez MM, Boltri JM, Okosun I, Guyinn M, Johnson JA. Impact of vital signs screening & clinician prompting on alcohol and tobacco screening and intervention rates: A pre-post intervention comparison. BMC Family Practice. 2010;11(1):18. doi: 10.1186/1471-2296-11-18. Retrieved from http://www.biomedcentral.com/1471-2296/11/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock EP, Polen MR, Green CA, Orleans T, Klein J the U.S. Preventive Services Task Force. April 6). Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2004;140:557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- Williams EC, Johnson ML, Lapham GT, Caldeiro RM, Chew L, Fletcher GS, Bradley, KA. Strategies to implement alcohol screening and brief intervention in primary care settings: A structured literature review. Psychology of Addictive Behaviors. 2011;25:206–214. doi: 10.1037/a0022102. [DOI] [PubMed] [Google Scholar]
- Woodwell DA, Cherry DK. National ambulatory medical care survey: 2002 Summary. Advance data from vital and health statistics. Hyattsville, MD: National Center for Health Statistics; 2004. [PubMed] [Google Scholar]