Abstract
Overdose is a leading cause of death among illicit drug users. 924 injection drug users (IDUs) in Baltimore, Maryland, were interviewed to characterize overdose events and determine the circumstances under which they lead to drug treatment. Overall, 366 (39.7%) reported at least one non-fatal drug overdose. Most (96.2%) used heroin on the day of their last overdose and almost half (42.6%) used heroin and alcohol but few (4.1%) used tranquilizers or benzodiazepines. Five percent were in drug treatment when the overdose occurred and 7.1% had been incarcerated two weeks prior. One in four IDUs (26.2%) sought drug treatment within 30 days after their last overdose of whom 75% enrolled. Speaking with someone about drug treatment after the overdose was associated with treatment seeking (AOR 5.22; 95% CI: 3.12, 8.71). Family members were the most commonly cited source of treatment information (53.7%) but only those who spoke with spouses, crisis counselors and hospital staff were more likely to seek treatment. Not being ready for treatment (69.6%) and not viewing drug use as a problem (30.7%) were the most common reasons for not seeking treatment and being placed on a waiting list was the most common reason for not subsequently enrolling in treatment (66.7%). Of the IDUs treated by emergency medical technicians, emergency room staff, or hospital staff, only 17.3%, 26.2% and 43.2% reported getting drug treatment information from those sources, respectively. Interventions that provide drug treatment information and enhance motivation for treatment in the medical setting and policies that reduce barriers to treatment entry among motivated drug users are recommended.
1. Introduction
Overdose is a leading cause of death among illicit drug users (Gossop et al., 2002; Hser et al., 2001; Oppenheimer et al., 1994; Perucci et al., 1991; van Ameijden et al., 1999; Vlahov et al., 2004). Baltimore City has one of the highest overdose mortality rates in the U.S., estimated at 56.4 per 100,000 in 2002 (Substance Abuse and Mental Health Services Administration, 2004). In addition to fatal drug overdoses, 25–68% of injection drug users (IDUs) report ever experiencing a non-fatal overdose (Bennett and Higgins, 1999; Darke et al., 1996a; Latkin et al., 2004; Powis et al., 1999; Seal et al., 2001; Sergeev et al., 2003; Tobin and Latkin, 2003) and high rates of overdose-related morbidity have been documented (Warner-Smith et al., 2002). Variations in estimates of non-fatal overdose can be attributed to differences in the prevalence of overdose risk factors which include injection, polydrug use, and re-initiation of drug use after periods of abstinence (e.g. after incarceration or drug treatment) (Darke and Hall, 2003).
Rates of emergency medical response to overdose and witnesses’ attempts to revive the victim have been described elsewhere (Bennett and Higgins, 1999; Darke et al., 1996b; Davidson et al., 2002; McGregor et al., 1998; Sergeev et al., 2003; Tobin et al. 2005; Tracy et al., 2005). Less is known about whether the overdose event serves as an impetus for entering drug treatment or other changes in drug use behaviors. A study among IDUs in Baltimore found an association between recent non-fatal overdose and enrollment in detoxification treatment but could not establish temporality of the exposure and outcome (Schutz et al., 1994). In Sydney, Australia, 11% of overdose victims interviewed one week after overdose said they planned to seek drug treatment and an additional 34% said they would “try to stop” using drugs or “definitely stop completely”; however, the sample size (n=48) and response rate (34%) were low and the researchers did not follow participants to see who entered treatment (Zador et al., 2001). Another study of 138 overdose patients treated in a Swiss emergency room (ER) noted that more than 60% received no referral to drug treatment (Cook et al., 1998), suggesting that a valuable opportunity for referral had been lost.
Beyond description of non-fatal overdose experiences and likelihood of entering treatment, the primary purpose of this study was to identify factors that facilitate and impede using the overdose event to trigger treatment seeking and entry and to quantify “missed opportunities” for health care providers to provide drug treatment information following the drug overdose.
2. Methods
2.1. Study population
This study was conducted in the AIDS Link to Intravenous Experiences (ALIVE) study, a prospective cohort study of the natural history of HIV-1 infection among IDUs in Baltimore, Maryland; as described in detail elsewhere (Anthony et al., 1991; Vlahov et al., 1991). Briefly, 2960 IDUs were recruited between 1988 and 1989 via extensive community outreach efforts and word-of-mouth. Eligible participants were ≥18 years of age, reported injecting illicit drugs within the previous 11 years, and were AIDS-free at enrollment. In 1994 and 1998 and 2000, an additional 419, 246 and 50 participants, respectively, were recruited. Once enrolled, participants returned to the study clinic semiannually for interviews on sexual and drug use behaviors, medical history and health care utilization, as well as a physical examination and serological testing for HIV antibodies. The Johns Hopkins Bloomberg School of Public Health Committee on Human Research approved the study and all participants provided voluntary informed consent.
2.2. Overdose module
Between August 1, 2003 and September 30, 2004, all ALIVE participants who returned for a regularly scheduled semiannual study visit completed a one-time, interviewer-administered questionnaire regarding their drug overdose experiences. Participants were first asked whether they had ever overdosed. Those who did received specific questions regarding the circumstances surrounding their most recent overdose. For the purposes of the study, overdose was defined as “a situation where, after using, you or another person passed out and couldn’t wake up. The lips of the person who overdosed might have turned blue and their breathing was very slow or stopped.” Specific questions included the environment in which their most recent overdose occurred, substances used, whether they received medical treatment and what factors they perceived as contributing to the overdose. Participants were also asked about sources of information about entering drug treatment after their most recent overdose, whether they sought drug treatment in the 30 days following the event, whether they subsequently initiated treatment and the interval before starting to use drugs again. The questionnaire was structured with closed-ended, categorical responses and was piloted for content and length in a group of 15 ALIVE study volunteers during April 2003.
2.3. Statistical analysis
Descriptive statistics were used to characterize the demographics, drug use histories and overdose histories of the overall study population. Subsequent analyses were limited to participants who reported ever having an overdose. We used frequency distributions to characterize non-exclusive categorical responses to questions regarding circumstances of the overdose. We also calculated the proportion of IDUs who sought drug treatment in the 30 days following their overdose, as well those who said they talked about drug treatment with someone after their last overdose. This latter category was further broken down into several non-exclusive sources of drug treatment information (e.g., family member, crisis counselor, hospital staff).
Univariate logistic regression was used to identify exposures associated with recent overdose (<1 year), drug treatment seeking after overdose, treatment enrollment, and reinitiation of drug use following overdose. We also examined differences between men and women with regard to all reported circumstances preceding and following the most recent overdose event. In each of these analyses, exposures significant at the p<0.10 level were further explored using multiple logistic regression modeling to identify independent associations (p<0.05).
To quantify missed opportunities to provide drug treatment information in the medical setting, we calculated the percentage of IDUs who came in contact with a medical care provider (i.e., emergency medical technicians (EMTs), ER staff, hospital staff) as a result of their most recent overdose who did not report talking to that provider about drug treatment.
3. Results
The study population consisted of 924 subjects, of whom the majority was African American (92.9%) and male (67.1%). Median age was 47 years (IQR: 43–52). The median duration of injection career was 23 years (IQR: 17–31). Thirty-four percent had injected drugs in the prior 6 months; of the non-injectors, all had used heroin, cocaine or crack in the prior 6 months. Participants had undergone a median of 19 study visits (IQR: 13–27).
3.1. Circumstances of most recent overdose
Overall, 368 participants (39.8%) reported ever having an overdose. Two of these participants denied taking any drugs other than alcohol on the day of overdose and were dropped from further analysis. Among the remaining 366 participants, the median number of lifetime overdoses was 2 (IQR: 1–4). For most participants (92.3%) it had been more than one year since their last overdose. The 7.7% who overdosed within the past year were more likely to be African American, report that their most recent overdose took place while alone, and to believe the overdose was caused at least partially by lowered tolerance due to abstinence. Among the 275 IDUs who could estimate the date of last overdose, median time since overdose was 6.2 years (IQR: 3.1–10.6).
Notably, in the two weeks prior to their last overdose 26 IDUs (7.1%) reported being incarcerated, 4 (1.1%) were in drug treatment and 19 (5.2%) were enrolled in a drug treatment program when their overdose occurred. Of the 19, methadone maintenance was the most commonly cited treatment modality (47.4%), followed by other outpatient treatment programs (31.6%) and Narcotics Anonymous (31.6%). The vast majority of IDUs were in the company of others at the time of their last overdose. More than half (58.5%) were with a friend or acquaintance, 13.7% with a family member and 12.3% with a spouse or partner; however, 18.0% reported overdosing while alone. The location of last overdose was most commonly someone else’s home (38.3%), followed by the IDUs’ own home (30.6%), an abandoned house (16.9%), the street (6.3%) or a shooting gallery (4.1%).
Almost all participants (96.2%) reported heroin use on the day of the last overdose, with 53% reporting injecting heroin in combination with cocaine (speedball). Other drugs included cocaine used alone (14.5%), crack (4.6%), marijuana (4.1%), tranquilizers (including benzodiazepines) (3.8%) and methadone (1.9%). Approximately one-third (36.9%) used only one drug on the day of last overdose and more than half (54.1%) used two drugs. Almost all participants (97.8%) reported at least one drug taken by injection. Slightly less than half (44.3%) reported using alcohol on the day of last overdose (median 4 drinks; IQR 4–8) and concomitant use of heroin and alcohol was common (42.6%).
Study participants were asked to identify any factors they perceived as contributing to their last overdose. Drug strength was the most frequently cited perceived contributor (63.9%), followed by drug quantity (51.6%), using alcohol and drugs together (37.2%), polydrug use (excluding alcohol) (35.5%), being in poor health (13.7%) and not testing the drug before using (12.3%). Only 9 participants (2.5%) reported intentional overdose.
Regarding medical response, 168 (45.9%) participants said an ambulance responded to their last overdose and 122 (33.3%) went to an ER for treatment. Forty-four (12.0%) were admitted to the hospital (median stay 2 days; IQR: 1–7).
Compared with men, women were less likely to report using alcohol (AOR=0.52; 95% CI: 0.32, 0.85), overdosing in the street (AOR=0.07; 95% CI: 0.01, 0.53), and overdosing in an abandoned building (AOR=0.21; 95% CI: 0.09, 0.47) and more likely to report speedballing (AOR=2.32; 95% CI: 1.43, 3.78).
3.2. Drug treatment seeking and enrollment after overdose
Table 1 shows 149 (40.7%) IDUs who reported that someone talked to them about drug treatment following their most recent overdose. Drug treatment discussions occurred most frequently with family members (53.7%) and friends (41.6%). Overall, 96 IDUs (26.2%) sought drug treatment in the 30 days following their last overdose. Of the 149 IDUs who reported talking to someone about drug treatment, 67 (45.0%) subsequently sought treatment. In univariate analysis, the following characteristics were associated with drug treatment seeking: talking with someone about drug treatment (OR=5.30, 95% CI: 3.19, 8.79), using alcohol on the day of the overdose (OR=1.93; 95% CI: 1.20, 3.09), being attended by an ambulance (OR=1.98; 95% CI: 1.23, 3.17), treated in the ER (OR=1.74; 95% CI: 1.08, 2.81) or admitted to the hospital (OR=2.42; 95% CI: 1.26, 4.63). In a multiple logistic regression model, talking with someone about drug treatment (AOR=5.22; 95% CI: 3.12, 8.71) and alcohol use (AOR=1.83; 95% CI: 1.10, 3.05) were independently associated with increased likelihood of seeking drug treatment after controlling for race (AOR=1.56; 95% CI: 0.55, 4.47) and sex (AOR=0.95; 95% CI: 0.54, 1.66).
Table 1.
Drug treatment information sources and treatment seeking after overdose
| Reported as source (n=149) | Sought drug treatment (n=96) | Adjusted odds of seeking treatment | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Any source† | # | % | # | % | AOR | 95% CI |
|
| ||||||
| 149 | 100 | 67 | 45.0 | 5.22 | 3.12, 8.71*** | |
|
|
||||||
| Source type†† | ||||||
| Family | 80 | 53.7 | 38 | 47.5 | 1.29 | 0.67, 2.50 |
| Friend | 62 | 41.6 | 23 | 37.1 | 0.58 | 0.30, 1.13 |
| ER staff | 34 | 22.8 | 17 | 50.0 | 1.4 | 0.63, 3.10 |
| Hospital staff | 34 | 22.8 | 22 | 64.7 | 3.03 | 1.35, 6.83** |
| EMT | 30 | 20.1 | 13 | 43.3 | 0.96 | 0.42, 2.17 |
| Spouse/partner | 29 | 19.5 | 21 | 72.4 | 4.54 | 1.83, 11.29*** |
| Crisis counselor | 17 | 11.4 | 12 | 70.6 | 3.63 | 1.19, 11.08* |
| Needle exchange | 12 | 8.1 | 6 | 50.0 | 1.34 | 0.40, 4.43 |
| Police | 9 | 6.0 | 6 | 66.7 | 2.55 | 0.61, 10.70 |
| Other | 13 | 8.7 | 8 | 61.5 | 2.20 | 0.67, 7.17 |
Adjusted for sex, race and alcohol use on day of overdose
Adjusted for sex and race
p<0.05
p<0.01
p≤0.001
When we further examined the specific source of drug treatment information, only those who reported talking with a spouse or partner, a crisis counselor or hospital staff were significantly more likely to seek drug treatment after adjusting for race and sex (Table 1). Alcohol use was not independently associated with treatment seeking in any of the source-specific analyses. Of the IDUs who reported that someone talked to them about drug treatment, 44.6% reported talking to one source, 26.4% to two sources, 11.5% to three sources and 17.6% to four or more sources. Getting information from more than one source did not significantly increase the likelihood of seeking drug treatment.
As noted above, for many IDUs it had been several years since their last overdose (median 6.2 years). To explore the possibility that differential recall biased our findings, we compared the overdose characteristics of IDUs who were able to estimate the date of their last overdose (n=275) to those who could not (n=91). In a univariate analysis, IDUs in the latter group were less likely to recall using alcohol on the day of the overdose (34.7% vs. 47.6%, p=0.024), being attended by an ambulance (35.2% vs. 49.6%, p=0.018), talking to someone about drug treatment (27.5% vs. 45.1%, p= 0.003) and seeking drug treatment (17.6% vs. 29.1%, p=0.031). However, after excluding these IDUs from a second multiple logistic regression analysis the findings were largely unchanged. Talking to someone about treatment remained a significant predictor of treatment seeking (AOR=4.74; 95% CI: 2.67, 8.39) and those who spoke specifically to spouses or partners (AOR=4.69; 95% CI: 1.67, 13.19) or crisis counselors (AOR=4.14; 95% CI: 1.21, 14.10) remained significantly more likely to seek treatment. Speaking with hospital staff retained a marginal association with treatment seeking (AOR=2.43; 95% CI: 1.00, 5.91).
Table 2 shows that of the 270 IDUs (73.8%) who did not seek treatment after their most recent overdose, not being ready for treatment (69.6%) and not viewing drug use as a problem (30.7%) were the most commonly cited reasons for not seeking treatment. Systemic barriers to treatment, such as cost and treatment availability, were less frequently cited. A majority (75.0%) of those who sought drug treatment subsequently enrolled in treatment. Among those who sought but did not initiate treatment, most (66.7%) said it was because they were placed on a waiting list. Those who enrolled were more likely than those who did not to have talked with someone about treatment after their overdose (AOR=4.07; 95% CI: 1.35, 12.29) and to cite low tolerance as contributing to the overdose (AOR=4.23; 95% CI: 1.16, 15.40), and less likely to cite drug contamination as a contributing factor (AOR=0.14; 95% CI: 0.03, 0.70), after controlling for sex (AOR=2.61; 95% CI: 0.78, 8.79) and race (AOR=0.61; 95% CI: 0.06, 6.65).
Table 2.
Reasons for not seeking or enrolling in drug treatment after overdose
| Did not seek treatment (n=270) | Sought treatment but did not enroll (n=24) | |||
|---|---|---|---|---|
|
| ||||
| # | % | # | % | |
|
| ||||
| Not ready for treatment | 188 | 69.6 | 9 | 37.5 |
| Drug use isn’t a problem | 77 | 30.7 | 2 | 8.3 |
| Failed treatment before | 59 | 21.9 | 6 | 25.0 |
| Can’t afford treatment | 43 | 15.9 | 9 | 37.5 |
| Don’t think treatment will work | 31 | 11.5 | 3 | 12.5 |
| Preferred treatment not available | 29 | 10.7 | 9 | 37.5 |
| On a waiting list | 23 | 8.5 | 16 | 66.7 |
| Didn’t know where to go | 23 | 8.5 | 4 | 16.7 |
| Turned down | 21 | 7.8 | 7 | 29.2 |
| No program nearby | 20 | 7.4 | 1 | 4.2 |
| Other | 25 | 9.3 | 5 | 20.8 |
A majority of IDUs started using drugs again on the same day as their overdose (28.1%) or on the day following the overdose (36.6%); 9.0% reported no further use. These 9% were more likely to have talked to someone about drug treatment after the overdose (AOR=2.60; 95% CI: 1.22, 5.54) but less likely to report using heroin only on the day of the overdose (AOR=0.39; 95% CI: 0.18, 0.86) after controlling for sex (AOR=1.57; 95% CI: 0.74, 3.33) and race (AOR=0.47; 95% CI: 0.15, 1.52). Those who reported seeking drug treatment within 30 days of the overdose had a longer median time to re-initiation of drug use – within the next week for those who sought treatment compared to the next day for those who did not - and a larger proportion (19.8%) of those who sought treatment reported never using drugs again compared to those who did not seek treatment (5.3%).
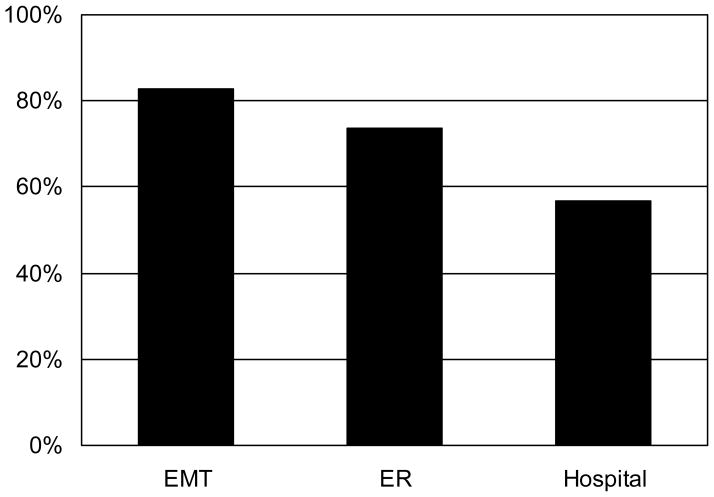
3.3. Missed opportunities to promote drug treatment
As seen in Figure 1, missed opportunities to provide drug treatment information in the medical setting following overdose were frequent. Of the 168 IDUs who were attended by an ambulance in response to their most recent overdose, 82.7% said they did not receive information about drug treatment from an EMT. Similarly, 73.8% of the 122 IDUs who visited an emergency room did not receive drug treatment information from ER staff, and 56.8% of the 44 hospitalized IDUs denied receiving drug treatment information from hospital staff.
Figure 1.
Missed Opportunities to Provide Drug Treatment Information after Overdose
4. Discussion
This study found that nearly half of the IDUs we studied reported having ever experienced a non-fatal overdose, which is consistent with the 25–68% range established by previous studies conducted in the United States, United Kingdom, Australia and Russia (Bennett and Higgins, 1999; Darke et al., 1996a; Latkin et al., 2004; Powis et al., 1999; Seal et al., 2001; Sergeev et al., 2003; Tobin and Latkin, 2003). Similar to other studies, the majority of overdoses took place when someone else was present in a home setting, providing an opportunity for bystander interventions. However, nearly one-fifth reported being alone the last time they overdosed and 17% were in abandoned buildings, which lack telephones and thus substantially reduce the likelihood of timely emergency response. The dangers of using drugs under these circumstances should be emphasized in overdose prevention programs.
Only 16% of the IDUs in our study reported using drugs other than heroin but almost half (43%) reported concomitant use of heroin and alcohol, making this combination an important target for overdose prevention. Only 4% reported using tranquilizers or benzodiazepines – a much lower level than the 18–43% reported in other studies (Darke et al., 1996b; Powis et al., 1999; Seal et al., 2001) but consistent with the most recent data on overdose mortality in Baltimore which found benzodiazepines present in only 4% of overdose deaths (Substance Abuse and Mental Health Services Administration, 2004). This suggests that Baltimore’s overdose prevention programs might not give the same attention as other cities to benzodiazepine but allow greater emphasis on other more prevalent risk factors (e.g., alcohol use). Other localities may find similar studies of overdose characteristics useful for tailoring their overdose prevention programs.
Seven percent of the IDUs in our study were incarcerated during the two weeks prior to their overdose. Re-initiation of drug use upon release from prison is an acknowledged risk factor for fatal drug overdose (Bird and Hutchinson, 2003; Seaman et al., 1998). In Baltimore, where 80% of those sentenced to prison have substantial substance abuse problems and at least 40% have a history of injection drug use (Drug Strategies, 2000), drug treatment during incarceration is sparse. Further, no comprehensive programs have been established to provide incarcerants with overdose prevention information or links to drug treatment upon release. Such information seems warranted.
Although infrequent, overdoses were reported among those in or recently released from drug abuse treatment. These findings are consistent with reports of elevated overdose risk after detoxification treatment (Seal et al., 2001; Strang et al., 2003) and immediately after initiating or re-initiating methadone maintenance therapy (Caplehorn and Drummer, 1999; Buster et al., 2002). With almost 22,000 substance abuse treatment admissions in Baltimore in 2002, of which more than 15,000 involved heroin (Maryland Alcohol and Drug Abuse Administration, 2003), overdose related to treatment is not trivial; it is important that drug users admitted to treatment receive information on how to reduce their risk of overdose. Specifically, treatment programs should inform participants that using heroin or other opiates while on methadone increases the risk of overdose and that re-initiating drug use after completion of, or withdrawal from, a drug treatment program increases overdose risk. These messages emphasize abstinence from illicit drug use and are thus consistent with treatment programs’ cessation goals. Studies that match Baltimore’s overdose mortality records with drug treatment program admission records may help identify types of programs that should be prioritized for overdose prevention interventions.
One quarter of the IDUs in this study sought drug treatment within 30 days after their most recent overdose. These IDUs were significantly more likely than those who did not seek treatment to report talking to someone about drug treatment after the overdose and most of them (75%) successfully enrolled. Interestingly, the most commonly cited barriers to seeking drug treatment (i.e., not ready for treatment, not viewing drug use as a problem) reflect low motivation to change drug use behaviors while the most common barriers to enrollment were of a systemic nature (e.g., treatment availability, cost). Reducing systemic barriers to drug treatment for motivated IDUs and undertaking interventions to enhance motivation for others could transform the overdose event into a catalyst for drug treatment enrollment.
Longabaugh and colleagues have deemed events that draw an association between substance use and adverse health events “teachable moments” in which patients may be more motivated to change their harmful behaviors (Longabaugh et al., 1995). Brief interventions to enhance motivation after an alcohol–related event have been implemented in emergency room and hospital settings with some success (D’Onofrio and Degutis, 2002; Dunn and Ries, 1997; Gentilello et al., 1999; Longabaugh et al., 2001; Wright et al., 1998) but few have extended this interventional approach to include drug-related events (Bernstein et al., 1997). Future studies should evaluate whether motivational interventions administered in the medical setting generally, and among overdose victims specifically, can increase motivation to change drug use behaviors and improve the likelihood of drug treatment seeking and enrollment. Optimal timing is that these interventions occur before, not after, release from the emergency room or hospital as most IDUs in this study started using drugs again within 24–48 hours of their last overdose.
Unfortunately, opportunities to promote drug treatment among overdose victims are frequently missed in the medical setting. About half of the IDUs we interviewed said an ambulance responded to their last overdose, but only 17% said the EMTs talked to them about drug treatment. The proportions that received treatment information from ER staff or hospital staff were similarly low. While some of the missed opportunities among EMTs may be attributed to patients’ lack of consciousness and the nature of the EMT’s role, which is to stabilize and transfer the patient as quickly as possible, expanding the role of ER and hospital personnel to – at a minimum – provide information on drug treatment appears warranted. In this study, hospital staff and crisis counselors appeared particularly influential in linking IDUs with drug treatment.
Several study limitations should be noted. First, since the median time since last overdose was 6.2 years, it is possible that some participants could not recall the specific details of overdose events that happened in the distant past. Comparison of past year overdoses to those that occurred in the more distant past did not detect any differences that could be attributed to recall bias. We did detect differential response patterns when comparing those who were able to estimate the date of their last overdose with those who were not; however, these differentials did not significantly affect our overall findings regarding the effect of providing treatment information on treatment seeking. A possibility remains that those who sought drug treatment following their last overdose were more likely to remember talking with someone about treatment, thus exaggerating the influence of these interactions on subsequent treatment seeking. It also should be noted that our study population was predominantly older, African American drug users with a long history of drug use. Their experiences may not be representative of dissimilar populations of drug users, particularly younger users and new initiates.
In conclusion, we found that the prevalence of overdose among IDUs in Baltimore is similar to frequencies reported elsewhere but that these overdoses had certain characteristics that should be considered in the development of local overdose prevention programs. While it does not appear that experiencing an overdose serves as a common impetus for seeking drug treatment or otherwise changing drug use behaviors, the barriers to treatment identified by our study may be amenable to interventions in the medical setting. At a minimum, there is clearly a need for medical care providers to capitalize upon the contact with IDUs that occurs after overdose to provide information on drug treatment that might be useful for those individuals who are ready to seek treatment.
Acknowledgments
The authors wish to acknowledge the contributions of the ALIVE participants and interview staff. Dr. Pollini’s research training and the ALIVE studies are funded by National Institute on Drug Abuse grants T32 DA07292, R01 DA12568 and R01 DA04334.
References
- Anthony JC, Vlahov D, Nelson KE, Cohn S, Astemborski J, Solomon L. New evidence on intravenous cocaine use and the risk of infection with human immunodeficiency virus type 1. Am J Epidemiol. 1991;134:1175–1189. doi: 10.1093/oxfordjournals.aje.a116021. [DOI] [PubMed] [Google Scholar]
- Bennett GA, Higgins DS. Accidental overdose among injecting drug users in Dorset, UK. Addiction. 1999;94:1179–1190. doi: 10.1046/j.1360-0443.1999.94811798.x. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J, Levenson S. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann Emerg Med. 1997;30:181–189. doi: 10.1016/s0196-0644(97)70140-9. [DOI] [PubMed] [Google Scholar]
- Bird SM, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison: Scotland, 1996–99. Addiction. 2003;98:185–190. doi: 10.1046/j.1360-0443.2003.00264.x. [DOI] [PubMed] [Google Scholar]
- Buster MCA, van Brussel GHA, van den Brink W. An increase in overdose mortality during the first 2 weeks after entering or re-entering methadone treatment in Amsterdam. Addiction. 2002;97:993–1001. doi: 10.1046/j.1360-0443.2002.00179.x. [DOI] [PubMed] [Google Scholar]
- Caplehorn JRM, Drummer OH. Mortality associated with New South Wales methadone programs in 1994: lives lost and saved. Med J Aust. 1999;170:104–109. doi: 10.5694/j.1326-5377.1999.tb127675.x. [DOI] [PubMed] [Google Scholar]
- Cook S, Moeschler O, Michaud K, Yersin B. Acute opiate overdose: characteristics of 1990 consecutive cases. Addiction. 1998;93:1559–1565. doi: 10.1046/j.1360-0443.1998.9310155913.x. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: I. Prevalence and correlates of non-fatal overdose. Addiction. 1996a;91:405–11. [PubMed] [Google Scholar]
- Darke S, Ross J, Hall W. Overdose among heroin users in Sydney, Australia: II. Responses to overdose. Addiction. 1996b;91:413–417. doi: 10.1046/j.1360-0443.1996.91341310.x. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall W. Heroin overdose: research and evidence-based intervention. J Urban Health. 2003;80:189–200. doi: 10.1093/jurban/jtg022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson PJ, Ochoa KC, Hahn JA, Evans JL, Moss AR. Witnessing heroin-related overdoses: the experiences of young injectors in San Francisco. Addiction. 2002;97:1511–1156. doi: 10.1046/j.1360-0443.2002.00210.x. [DOI] [PubMed] [Google Scholar]
- D’Onofrio G, Degutis LC. Preventive care in the emergency department: screening and brief intervention for alcohol problems in the emergency department: a systematic review. Acad Emerg Med. 2002;9:627–638. doi: 10.1111/j.1553-2712.2002.tb02304.x. [DOI] [PubMed] [Google Scholar]
- Drug Strategies. Smart Steps: Treating Baltimore’s Drug Problem. Drug Strategies; Washington, DC: 2000. [Google Scholar]
- Dunn CW, Ries R. Linking substance abuse service with general medical care: integrated, brief interventions with hospitalized patients. Am J Drug Alcohol Abuse. 1997;23:1–13. doi: 10.3109/00952999709001684. [DOI] [PubMed] [Google Scholar]
- Gentilello LM, Rivara FP, Donovan DM, Jurkovich GJ, Daranciang E, Dunn CW, Villaveces A, Copass M, Ries RR. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230:473–483. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Treacy S, Marsden J. A prospective study of mortality among drug misusers during a 4-year period after seeking treatment. Addiction. 2002;97:39–47. doi: 10.1046/j.1360-0443.2002.00079.x. [DOI] [PubMed] [Google Scholar]
- Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch Gen Psy. 2001;58:503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Hua W, Tobin K. Social network correlates of self-reported non-fatal overdose. Drug Alcohol Depend. 2004;73:61–67. doi: 10.1016/j.drugalcdep.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Minugh PA, Nirenberg TD, Clifford PR, Becker B, Wollard R. Injury as a motivator to reduce drinking. Acad Emerg Med. 1995;2:817–825. doi: 10.1111/j.1553-2712.1995.tb03278.x. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Woolard RF, Nirenberg TD, Minugh AP, Becker B, Clifford PR, Carty K, Sparadeo F, Gogineni A. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol. 2001;62:806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- Maryland Alcohol and Drug Abuse Administration, Department of Health and Mental Hygiene. Alcohol and Drug Abuse Administration Publication No 03-2-001. Catonsville, MD: 2003. Outlook and Outcomes: 2003 Annual Report. [Google Scholar]
- McGregor C, Darke S, Ali R, Christie P. Experience of non-fatal overdose among heroin users in Adelaide, Australia: circumstances and risk perceptions. Addiction. 1998;93:701–711. doi: 10.1046/j.1360-0443.1998.9357016.x. [DOI] [PubMed] [Google Scholar]
- Oppenheimer E, Tobutt C, Taylor C, Andrew T. Death and survival in a cohort of heroin addicts from London clinics: a 22-year follow-up study. Addiction. 1994;89:1299–1308. doi: 10.1111/j.1360-0443.1994.tb03309.x. [DOI] [PubMed] [Google Scholar]
- Perucci CA, Davoli M, Rapiti E, Abeni DD, Forastiere F. Mortality of intravenous drug users in Rome: a cohort study. Am J Public Health. 1991;81:1307–1310. doi: 10.2105/ajph.81.10.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powis B, Strang J, Griffiths P, Taylor C, Williamson S, Fountain J, Gossop M. Self-reported overdose among injecting drug users in London: extent and nature of the problem. Addiction. 1999;94:471–478. doi: 10.1046/j.1360-0443.1999.9444712.x. [DOI] [PubMed] [Google Scholar]
- Schutz CG, Rapiti E, Vlahov D, Anthony JC. Suspected determinants of enrollment into detoxification and methadone maintenance treatment among injection drug users. Drug Alcohol Depend. 1994;36:129–138. doi: 10.1016/0376-8716(94)90095-7. [DOI] [PubMed] [Google Scholar]
- Seal KH, Kral AH, Gee L, Moore LD, Bluthenthal RN, Lorvick J, Edlin BR. Predictors and prevention of non-fatal overdose among street-recruited injection heroin users in the San Francisco bay area, 1998–1999. Am J Public Health. 2001;91:1842–1846. doi: 10.2105/ajph.91.11.1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seaman SR, Brettle RP, Gore SM. Mortality from overdose among injecting drug users recently released from prison: database linkage study. BMJ. 1998;316:426–428. doi: 10.1136/bmj.316.7129.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sergeev B, Karpets A, Sarang A, Tikhonov M. Prevalence and circumstances of opiate overdose among injection drug users in the Russian Federation. J Urban Health. 2003;80:212–219. doi: 10.1093/jurban/jtg024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J, McCambridge J, Best D, Beswick T, Bearn J, Rees S, Gossop M. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ. 2003;326:959–960. doi: 10.1136/bmj.326.7396.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies. DAWN Series D-25, DHHS Publication No (SMA) 04-3875. Rockville, MD: 2004. Mortality Data from the Drug Abuse Warning Network, 2002. [Google Scholar]
- Tobin KE, Davey MA, Latkin CA. Calling emergency medical services during drug overdose: an examination of individual, social and setting correlates. Addiction. 2005;100:397–404. doi: 10.1111/j.1360-0443.2005.00975.x. [DOI] [PubMed] [Google Scholar]
- Tobin KE, Latkin CA. The relationship between depressive symptoms and nonfatal overdose among a sample of drug users in Baltimore, Maryland. J Urban Health. 2003;80:220–229. doi: 10.1093/jurban/jtg025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy M, Piper TM, Ompad D, Bucciarelli A, Coffin PO, Vlahov D, Galea S. Circumstances of witnessed drug overdose in New York City: implications for intervention. Drug Alcohol Depend. 2005;79:181–90. doi: 10.1016/j.drugalcdep.2005.01.010. [DOI] [PubMed] [Google Scholar]
- van Ameijden EJ, Krol A, Vlahov D, Flynn C, van Haastrecht HJ, Coutinho RA. Pre-AIDS mortality and morbidity among injection drug users in Amsterdam and Baltimore: an ecological comparison. Subst Use Misuse. 1999;34:845–865. doi: 10.3109/10826089909037245. [DOI] [PubMed] [Google Scholar]
- Vlahov D, Anthony JC, Munoz A, Margolick J, Nelson KE, Celentano DD, Solomon L, Polk BF. The ALIVE study: a longitudinal study of HIV-1 infection in intravenous drug users: description and methods. NIDA Res Monogr. 1991;107:75–100. [PubMed] [Google Scholar]
- Vlahov D, Wang C, Galai N, Bareta J, Mehta SH, Strathdee SA, Nelson KE. Mortality risk among new onset injection drug users. Addiction. 2004;99:946–954. doi: 10.1111/j.1360-0443.2004.00780.x. [DOI] [PubMed] [Google Scholar]
- Warner-Smith M, Darke S, Day C. Morbidity associated with non-fatal heroin overdose. Addiction. 2002;97:963–967. doi: 10.1046/j.1360-0443.2002.00132.x. [DOI] [PubMed] [Google Scholar]
- Wright S, Moran L, Meyrick M, O’Connor R, Touquet R. Intervention by an alcohol health worker in an accident and emergency department. Alcohol Alcohol. 1998;33:651–656. doi: 10.1093/alcalc/33.6.651. [DOI] [PubMed] [Google Scholar]
- Zador D, Sunjic S, McLennan J. Circumstances and users’ perceptions of heroin overdose at the time of the event and at one-week follow-up in Sydney, Australia: implications for prevention. Addict Res Theory. 2001;9:407–423. [Google Scholar]