Abstract
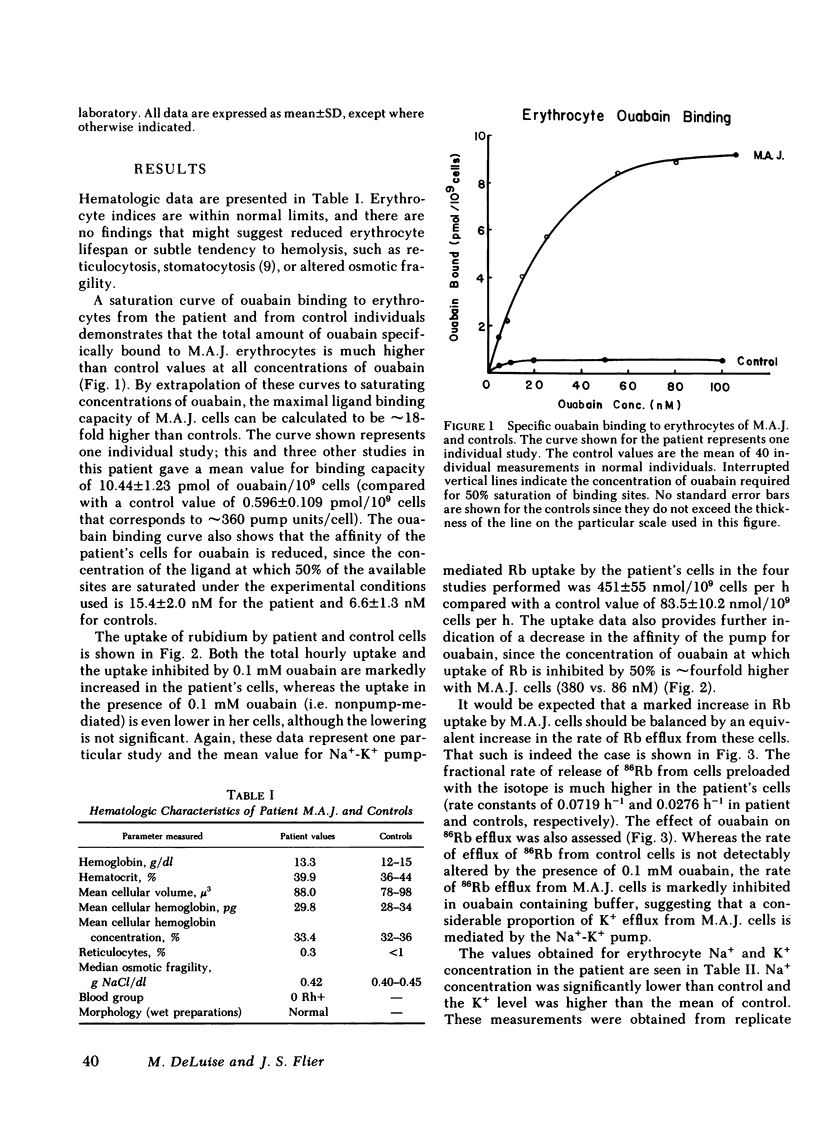
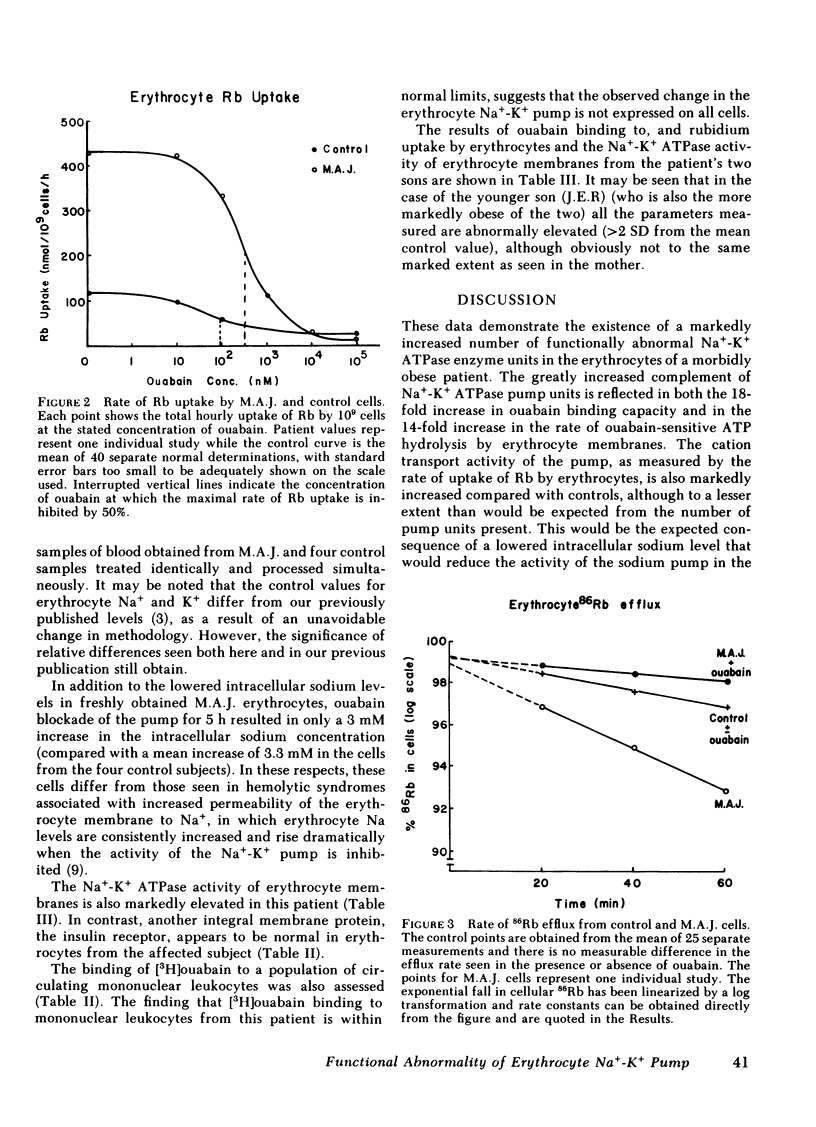
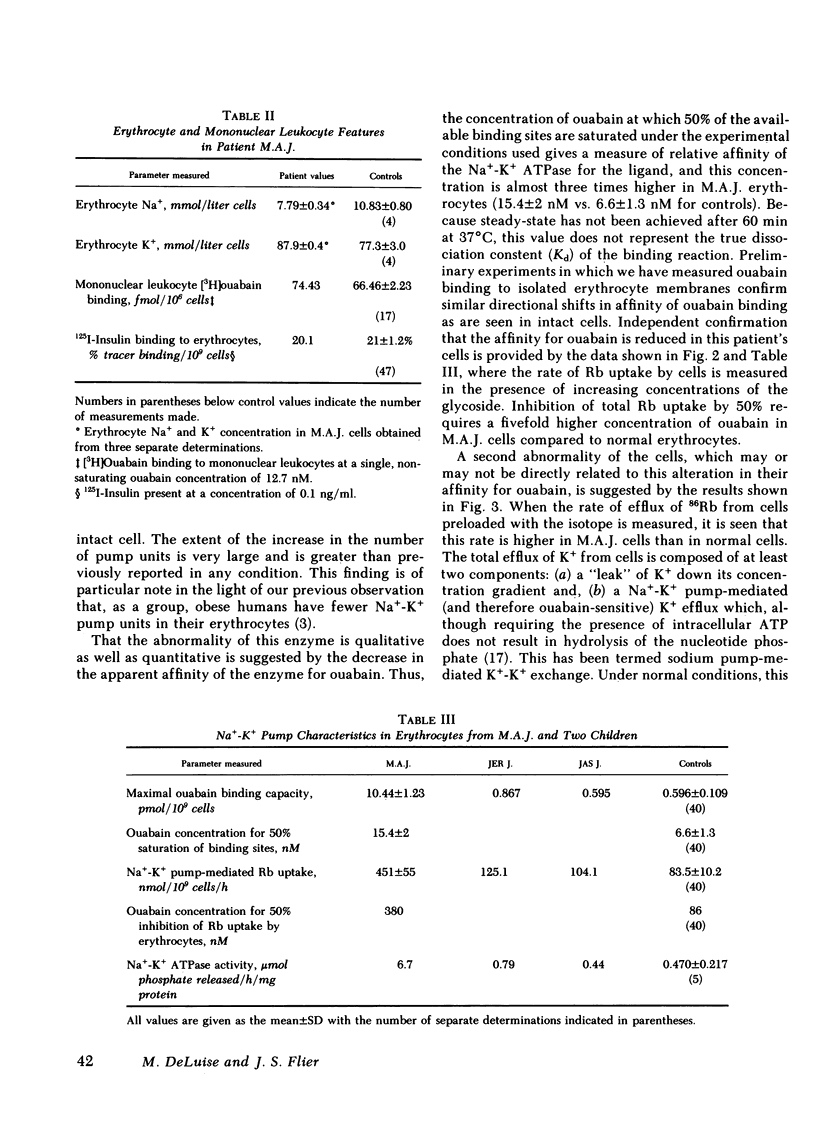
The Na+-K+ pump in the erythrocytes of a mordibly obese patient shows a unique constellation of functional abnormalities. The number of pump units, measured by [3H]ouabain binding to intact cells, as well as the enzymatic activity of the (Na+-K+)-dependent ATPase in erythrocyte membranes were found to be markedly increased compared with control cells (18-fold and 14-fold, respectively). There was a concomitant fivefold increase in the rate of pump-mediated uptake of 86Rubidium (a K analogue); this was balanced by an increased rate of 86Rb efflux. In striking contrast to normal cells, however, a major portion of this efflux (80%) was inhibited by ouabain, and thus appeared to be mediated by the Na+-K+ pump.
Erythrocytes from this patient had elevated levels of intracellular K+ and reduced levels of intracellular Na+. This finding, taken together with the ouabain inhibition of K+ efflux and the absence of associated abnormalities, argues against the possibility that the increased number of Na+-K+ pump units was a compensation for a primary increase in the permeability of the erythrocyte membrane to monovalent cations, as is seen in a variety of erythrocyte disorders. Further evidence for a primary abnormality of the enzyme was our observation that the cardiac glycoside ouabain bound to these cells with reduced affinity and had a right shifted dose response for pump inhibition. The markedly increased number of Na+-K+ pump units in these cells did not appear to extend to mononuclear leukocytes.
In conclusion, the erythrocytes from this patient have a very large number of functionally abnormal Na+-K+ ATPase units. A unique abnormality of the erythrocyte Na+-K+ ATPase of these cells is the most likely explanation for these findings.
Full text
PDF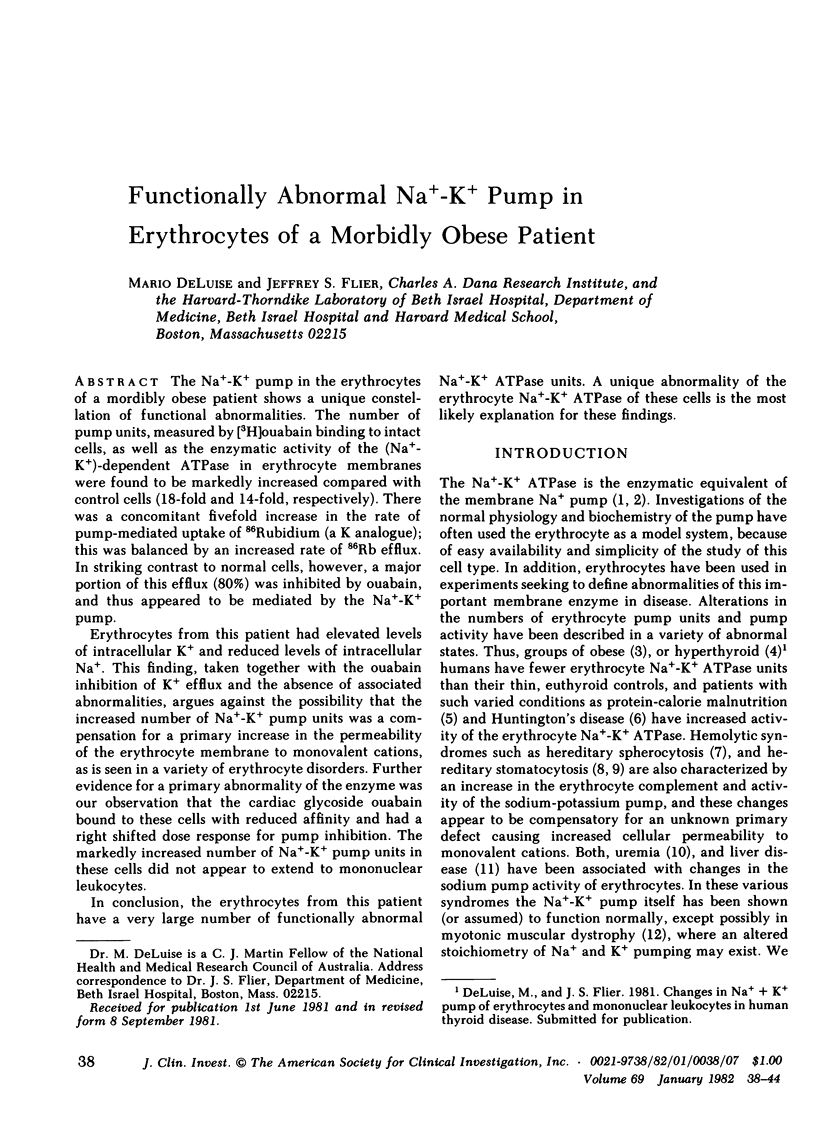

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alam A. N., Poston L., Wilkinson S. P., Golindano C. G., Williams R. A study in vitro of the sodium pump in fulminant hepatic failure. Clin Sci Mol Med. 1978 Oct;55(4):355–363. doi: 10.1042/cs0550355. [DOI] [PubMed] [Google Scholar]
- Bradford M. M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976 May 7;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- Butterfield D. A., Oeswein J. Q., Prunty M. E., Hisle K. C., Markesbery W. R. Increased sodium plus potassium adenosine triphosphatase activity in erythrocyte membranes in Huntington's disease. Ann Neurol. 1978 Jul;4(1):60–62. doi: 10.1002/ana.410040111. [DOI] [PubMed] [Google Scholar]
- Böyum A. Isolation of mononuclear cells and granulocytes from human blood. Isolation of monuclear cells by one centrifugation, and of granulocytes by combining centrifugation and sedimentation at 1 g. Scand J Clin Lab Invest Suppl. 1968;97:77–89. [PubMed] [Google Scholar]
- Cole C. H., Waddell R. W. Alteration in intracellular sodium concentration and ouabain-sensitive ATPase in erythrocytes from hyperthyroid patients. J Clin Endocrinol Metab. 1976 Jun;42(6):1056–1063. doi: 10.1210/jcem-42-6-1056. [DOI] [PubMed] [Google Scholar]
- De Luise M., Blackburn G. L., Flier J. S. Reduced activity of the red-cell sodium-potassium pump in human obesity. N Engl J Med. 1980 Oct 30;303(18):1017–1022. doi: 10.1056/NEJM198010303031801. [DOI] [PubMed] [Google Scholar]
- Gambhir K. K., Archer J. A., Bradley C. J. Characteristics of human erythrocyte insulin receptors. Diabetes. 1978 Jul;27(7):701–708. doi: 10.2337/diab.27.7.701. [DOI] [PubMed] [Google Scholar]
- Glynn I. M. Membrane adenosine triphosphatase and cation transport. Br Med Bull. 1968 May;24(2):165–169. doi: 10.1093/oxfordjournals.bmb.a070620. [DOI] [PubMed] [Google Scholar]
- Hull K. L., Jr, Roses A. D. Stoichiometry of sodium and potassium transport in erythrocytes from patients with myotonic muscular dystrophy. J Physiol. 1976 Jan;254(1):169–181. doi: 10.1113/jphysiol.1976.sp011227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplay S. S. Erythrocyte membrane Na+ and K+ activated adenosine triphosphatase in protein-calorie malnutrition. Am J Clin Nutr. 1978 Apr;31(4):579–584. doi: 10.1093/ajcn/31.4.579. [DOI] [PubMed] [Google Scholar]
- McCans J. L., Lindenmayer G. E., Pitts B. J., Ray M. V., Raynor B. D., Butler V. P., Jr, Schwartz A. Antigenic differences in (Na+, K+)-ATPase preparations isolated from various organs and species. J Biol Chem. 1975 Sep 25;250(18):7257–7265. [PubMed] [Google Scholar]
- Miller D. S., Kinter W. B., Peakall D. B. Enzymatic basic for DDE-induced eggshell thinning in a sensitive bird. Nature. 1976 Jan 15;259(5539):122–124. doi: 10.1038/259122a0. [DOI] [PubMed] [Google Scholar]
- Parker J. C., Welt L. G. Pathological alterations of cation movements in red blood cells. Arch Intern Med. 1972 Feb;129(2):320–332. [PubMed] [Google Scholar]
- Simons T. J. Potassium: potassium exchange catalysed by the sodium pump in human red cells. J Physiol. 1974 Feb;237(1):123–155. doi: 10.1113/jphysiol.1974.sp010474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweadner K. J., Goldin S. M. Active transport of sodium and potassium ions: mechanism, function, and regulation. N Engl J Med. 1980 Apr 3;302(14):777–783. doi: 10.1056/NEJM198004033021404. [DOI] [PubMed] [Google Scholar]
- WELT L. G., SACHS J. R., MCMANUS T. J. AN ION TRANSPORT DEFECT IN ERYTHROCYTES FROM UREMIC PATIENTS. Trans Assoc Am Physicians. 1964;77:169–181. [PubMed] [Google Scholar]
- Wiley J. S. Co-ordinated increase of sodium leak and sodium pump in hereditary spherocytosis. Br J Haematol. 1972 May;22(5):529–542. doi: 10.1111/j.1365-2141.1972.tb05700.x. [DOI] [PubMed] [Google Scholar]
- Wiley J. S., Ellory J. C., Shuman M. A., Shaller C. C., Cooper R. A. Characteristics of the membrane defect in the hereditary stomatocytosis syndrome. Blood. 1975 Sep;46(3):337–356. [PubMed] [Google Scholar]
- Zarkowsky H. S., Oski F. A., Sha'afi R., Shohet S. B., Nathan D. G. Congenital hemolytic anemia with high sodium, low potassium red cells. I. Studies of membrane permeability. N Engl J Med. 1968 Mar 14;278(11):573–581. doi: 10.1056/NEJM196803142781101. [DOI] [PubMed] [Google Scholar]


