Abstract
Physical activity is frequently a component of interventions designed to diminish weight gain in children. It is essential to determine whether the energy expenditure (EE) elicited by these interventions is sufficient to reduce the rate of weight gain.
Purpose
To quantify the EE of the Physical Activity across the Curriculum (PAAC) intervention. This intervention involved two 10-min physically active academic lessons per day, taught by classroom teachers.
Methods
We assessed EE of PAAC in 19 males and 19 females using both an indirect calorimeter (IC) (COSMED K4b2) and an accelerometer (ActiGraph) (AC). Independent t-tests were used to evaluate gender differences. Dependent t-tests were used to examine the difference between EE assessed by IC and AC. The agreement between EE measured by IC and estimated by AC was evaluated using a Bland-Altman plot. A Pearson correlation between EE measured by IC and estimated by AC was calculated.
Results
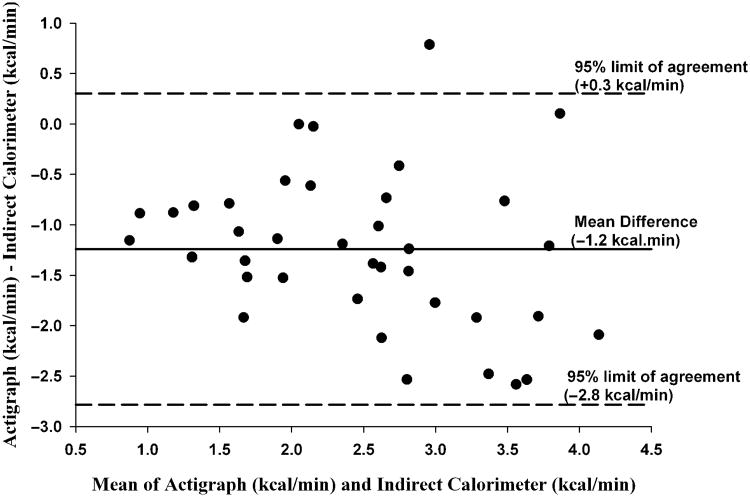
There were no significant gender differences for age, BMI, or EE; therefore, analyses by gender were not performed. The mean EE measured by IC was 3.1 ± 1.0 kcal/min(3.4 METs). Mean EE estimated by AC (1.8 ± 0.9 kcal/min) was significantly lower (P < 0.05) than EE measured by IC (mean underestimation = 1.3 kcal/min). The Bland-Altman plot suggested increased underestimation with increased levels of EE. The 95% limits of agreement were large (-2.8 to +0.3 kcal/min). The correlation between EE measured by IC and estimated by AC was r = 0.68 (P < 0.001).
Conclusion
PAAC elicited a level of EE that may prevent excessive weight gain in children. AC significantly underestimated the EE of PAAC lessons and may not provide useful EE estimates in this context.
Keywords: Indirect Calorimeter, Accelerometer, Classroom, School-Based
The prevalence of overweight, defined as 95th or greater body mass index (BMI) reference percentile, has increased in children of both genders and in all age groups (20). For example, the prevalence of overweight in female children and adolescents increased from 13.8% in 1999-2000 to 16.0% in the 2003-2004 National Health and Nutrition Examination Survey, and the prevalence of overweight in male children and adolescents increased from 14.0% to 18.2% during the same period (20).
Childhood overweight has been associated with a variety of diseases including insulin resistance (1,12,22), hypertension (24), and abnormal lipid profiles (13,26). Data show that overweight children will likely become overweight adults (10). Estimates of $117 billion in annual cost associated with treatments for overweight and obesity (25) support the need to prevent overweight in youth.
Studies have shown that physical activity patterns are inversely related to body weight in children (7,9). The current physical activity guidelines state that children should engage in at least 60 min of moderate-intensity physical activity per day (28). However, many children fail to meet this recommendation (5,21). The increased prevalence of overweight and inadequate levels of physical activity have focused its attention on developing effective strategies for increasing physical activity among children.
Because children spend much of their time at school, the school environment represents a suitable setting for interventions intended to encourage physical activity (3.4.11.18.23.27). Unfortunately, the majority of the school-based physical activity interventions to prevent the development of obesity have produced modest results at best (29). A potential explanation for the limited success of the school-based physical activity interventions is a failure to achieve an increase in physical activity energy expenditure (EE) sufficient to impact energy balance.
Integrating physical activity into classroom academic lessons offers an innovative approach to increasing physical activity during the school day without decreasing the time devoted to academics. Three studies document the potential to increase physical activity in the school classroom setting (14.15.27). However, none of the three studies provided a direct assessment of EE elicited by the physical activity program. Two of the studies used accelerometers to estimate EE (14,27). Because different accelerometer equations provide inconsistent estimates of EE over a range of activity types and intensities (31), it is unknown if classroom physical activity measured by accelerometer is an accurate estimate. The primary aim of this study was to obtain an objective assessment of the EE of a school-based classroom physical activity intervention titled Physical Activity across the Curriculum (PAAC) using a portable indirect calorimeter (IC). The PAAC intervention was designed to provide two physically active academic lessons per day (intensity, 3-6 METs; duration, 10 min) delivered by elementary school classroom teachers. A detailed description of the PAAC intervention has been published (8).
Methods
Participants
A convenience sample from three schools involved in the PAAC intervention participated in this study. Classroom teachers from the three schools were asked to distribute parental consent and student assent forms to approximately 160 children in grades 2 through 5. Children were instructed by their teacher to share the information with their primary guardian and that their participation was optional. Signed consent and assent forms were received from 38 children. Study procedures were explained to each child and classroom teacher before the assessments. Children were tested in the order in which consents were returned. All procedures were approved by the Institutional Review Board at the University of Kansas.
Procedures
As part of the PAAC intervention, classroom teachers previously attended a 6-h training workshop that included strategies to incorporate learning through physically active academic lessons and instruction on required duration and intensity of PAAC lessons. For the current study, the EE of one PAAC lesson per participant, led by 19 different classroom teachers, was assessed in each of the 38 participants. Examples of PAAC lessons evaluated included jumping to an “invisible” jump rope or performing calisthenics such as jumping-jacks or squats while reciting multiplication tables. Geography (e.g., North, South, East, and West) was taught by having children walk or run to the appropriate area designated for each direction. Spelling was taught by having children jump on appropriate letters taped on the floor, etc.
Assessments/Instrumentation
EE—IC
EE was assessed using a previously validated portable, open-circuit IC system (Cosmed K4b2, Cosmed, Rome, Italy) that measures breath-by-breath ventilation, expired oxygen, and carbon dioxide (17). After a minimum of a 30-min warm up, the calorimeter was calibrated with known gases. The flow turbine was calibrated using a 3.00- L syringe. During the PAAC lesson, the participant breathed into a face mask that directed air into the unit housing the O2 and CO2 gas analyzers. The lightweight (∼ 1.5 kg) portable system was attached by a harness around the waist and shoulders of the child while the child performed PAAC lessons. The data were retrieved for analysis via serial port interface and software provided with the calorimeter. Calorimeter data were reduced to 20-s epochs, and the average values over the 10-min PAAC lesson are reported. Estimated resting EE and the subsequent MET values were calculated using both the standard value for resting EE (3.5 ml/kg/min) and resting EE estimated using the equations provided by the World Health Organization (WHO) (33). All participants were assessed with the same calorimeter.
EE—accelerometer
EE during PAAC lessons was estimated from accelerometer data (counts per minute) obtained from an ActiGraph ([AC] Model 7164; ActiGraph LLC, Pensacola, FL). The AC is small (5.1 × 3.8 × 1.5 cm) and light weight (42.6 gm), and powered by a 2430 lithium coin cell battery. One AC was used for all participants in this study. The AC was factory calibrated 10 months before the start of the study. After the data collection, the AC used was checked against four ActiGraphs that had been previously calibrated using a standardized treadmill walking protocol. The AC used in this study was found to be within 10% of the counts per minute average obtained from the 4 ActiGraphs used as the standard. The AC was worn during the 10-min PAAC lesson on an elastic belt above the iliac crest of the right hip. Data were collected in 1-min epochs and retrieved for analysis via a coded infrared beam of light via a PC reader interface unit connected to a serial port interface and software provided with the AC. EE (kcal/min) was estimated from AC data (counts per minute) and body mass using the regression equation developed by Trost et al. (30). The Trost equation was selected because it is a previously validated, youth-specific, AC energy expenditure prediction equation.
System for Observing Fitness Instruction Time (SOFIT)
PAAC lessons were scored using the SOFIT (16), a visual observation instrument previously validated as a measure of physical activity during physical education classes. Activity was coded at 1-min intervals using a 5-point Likert scale (1, Lying down; 2, Sitting; 3, Standing; 4, Walking; 5, Very Active). SOFIT was administered by one of the four research assistants who had been previously trained in this protocol and demonstrated an interrater reliability of 0.80 or greater. The final SOFIT score was the average of the ten 1-min scores.
Demographics
Before the EE assessments, age and gender were recorded and the participant was weighed to the nearest 0.1 kg on a digital scale (model #68987, Befour Inc., Saukville, WI) and height was measured to the nearest 0.1 cm by a portable stadiometer (model #IP0955, Invicta Plastics Limited, Leicester, England). BMI was calculated by dividing weight in kilograms by height in meters squared. BMI percentiles were calculated from the Centers for Disease Control and Prevention growth charts (6).
Analysis
Independent t-tests were used to evaluate potential gender differences for age, BMI, and EE. Dependent t-tests were used to assess differences between EE measured by IC or estimated by accelerometer. The effect size for the magnitude of the difference between measured and estimated EE was evaluated by Cohen's delta. A general linear model was used to compare EE by grade level. If the overall grade effect was significant, then post hoc Tukey adjusted pair-wise t-tests were used to compare grade levels. The agreement between EE measured by IC (kcal/min) and accelerometer (kcal min 1) was evaluated using a Bland- Altman plot (2). A Pearson correlation was calculated between the 10-min averages of EE measured by IC (kcal/min) and accelerometer (kcal min). An alpha level of 0.05 or less was used to indicate statistical significance. Values are reported as mean ± SD. SAS version 9.1 for Windows was used for all analyses.
Results
Data were obtained from 38 second grade through fifth grade children (19 female, 19 male; 34 white, 4 Hispanic).
Descriptive characteristics of the participants by gender and grade are presented in Table 1. There were no significant gender differences for any descriptive characteristic. Thirty- four percent of the sample (6 male, 7 female) were at risk for overweight or overweight (BMI > 85th reference percentile).
Table 1.
Descriptive characteristics of the participants.
| n | Age (yr) | Body Weight (kg) | BMI (kg-nT−2) | BMI (Percentile) | |
|---|---|---|---|---|---|
| Female | 19 | 9.3 ±1.3 | 34.4 ± 7.8 | 18.7 ±3.5 | 64.1 ±31.3 |
| Male | 19 | 8.9 ±1.4 | 33.8 ± 8.4 | 18.7 ±3.3 | 71.1 ±23.8 |
| n | Age * (yr) | Body Weight (kg) | BMI (kg-m−2) | BMI (Percentile) | |
| Grade 2 | 13 (6F, 7M) | 7.5 + 0.9 | 29.8 ± 7.7† | 18.4 ±3.9 | 68.2 ± 28.2 |
| Grade 3 | 7 (2F, 5M) | 8.9 ± 0.2 | 35.0 ± 3.7 | 19.4 ±2.5 | 83.4 ±11.6‡ |
| Grade 4 | 11 (6F, 5M) | 9.9 ± 0.5 | 37.6 ± 7.7 | 18.9 ±2.9 | 70.2 ± 23.7 |
| Grade 5 | 7 (5F, 2M) | 10.8 ±0.3 | 35.7 ± 9.7 | 17.9 ±4.0 | 46.4 ± 34.9 |
| TOTAL | 38 (19F, 19M) | 9.1 ±1.3 | 34.1 ± 8.0 | 18.7 ±3.3 | NA |
Values are means ± SD.
Age is different between all grades (P < 0.05).
Grade 2 is different from 4 (P < 0.05).
Grade 3 is different from 5 (P < 0.05).
NA not applicable because percentiles are ordinal data.
The data for EE measured by IC and estimated by the AC are presented in Table 2. The mean EE of PAAC lessons measured by calorimeter was 3.1 ± 1.0 kcal/min (range = 1.4 - 5.2 kcal/min). The level of EE assessed during the first 5 (2.94 ± 1.88 kcal/min) and the last 5 min (3.12 ± 1.13 kcal/min) of the lesson was not significantly different. The mean EE of the PAAC lesson assessed by calorimeter was of moderate intensity (> 3METs) when METs were calculated using either the standard estimate of resting EE (3.5 mL/kg/min) or resting EE estimated from the equations from the WHO (33). When METs were calculated with the calorimeter using the standard estimate of resting EE, 97.3% of children engaged in moderate intensity activity compared with 60.5% of children when METs were calculated using the WHO estimate. The mean level of EE measured in the child wearing the IC likely provides a valid representation of the average level of EE achieved by all children in the classroom. This assertion is based on the results of assessment of physical activity during the PAAC lesson of the child wearing the calorimeter and two other randomly selected children in the classroom using SOFIT (16). Results indicated that SOFIT (scores) were nearly identical for the child wearing the calorimeter (3.83 ± 0.35) and the mean of the two randomly selected children (3.77 ± 0.39). The mean level of EE during the PAAC lesson did not differ by gender; however, significant differences in EE (kcal/min) between grades were observed. The between grade differences were not evident when EE was expressed in METs, suggesting that the observed differences were due to differences in body weight between grades (Table 2).
Table 2. Estimates of EE and PA level during PAAC lessons.
| n | IC (kcal min −1) | IC (METs-3.5) | IC (METs-WHO) | AC (kcal min −1) | AC (METs-3.5) | AC (METs-WHO) | AC (counts per minute) | |
|---|---|---|---|---|---|---|---|---|
| Female | 19 | 2.9 ± 0.8 | 4.7 ±1.0 | 3.2 ± 0.7 | 1.9 ±0.9 | 3.2 ±1.2 | 2.1 ±0.9 | 1686.5 ±883.7 |
| Male | 19 | 3.3 ±1.2 | 5.1 ±1.4 | 3.7 ±1.0 | 1.8 ±0.8 | 3.2 ±1.1 | 2.1 ±0.7 | 1692.5 ±664.5 |
| n | IC (kcal min−1) | IC (METs-3.5) | IC (METs-WHO) | AC (kcal min−1) | AC (METs) | AC (METs-WHO) | AC (counts per minute) | |
| Grade 2 | 13 (6F, 7M) | 2.4 ±1.0* | 4.7 ±1.3 | 3.0 ± 0.9 | 1.4 ±0.8* | 2.8 ±1.2 | 1.8 ±0.8 | 1672.5 ±615.4 |
| Grade 3 | 7 (2F, 5M) | 3.4 ± 0.9 | 5.7 ±1.5 | 3.8 ±1.0 | 1.8 ±0.6 | 3.1 ± 0.9 | 2.1 ±0.6 | 1540.9 ±617.0 |
| Grade 4 | 11 (6F, 5M) | 3.5 ± 0.8 | 5.2 ± 0.9 | 3.7 ± 0.7 | 2.4 ± 0.9 | 3.8 ±1.1 | 2.7 ± 0.8 | 2076.2 ± 782.0 |
| Grade 5 | 7 (5F, 2M) | 3.1 ±1.1 | 5.0 ±1.2 | 3.5 ± .09 | 1.6 ±0.7 | 2.8 ±1.0 | 1.9 ±0.7 | 1262.0 ±859.3 |
| TOTAL | 38 (19F, 19M) | 3.1 ±1.0 | 5.1 ±1.2 | 3.4 ±0.9 | 1.8 ±0.9 | 3.2 ±1.1 | 2.1 ±0.9 | 1689.5 ±743.6 |
METs-3.5 = 3.5 mL·kg−1·min−1 equals 1 MET.
METs-WHO = resting energy estimated by WHO.
Values are means ± SD.
Grade 2 is different from Grade 4 (P < 0.05).
The mean EE (kcal/min) during the PAAC lesson estimated by the AC (1.8 + 0.9 kcal/min) was significantly lower than the EE measured by calorimeter (3.1 + 1.0 kcal/min) (P < 0.05) with a large effect size (Cohen's delta = 1.36). On average, the AC underestimated mean EE by 1.2 kcal/min. A Bland-Altman plot (Fig. 1) suggests that the degree of underestimation of EE by the AC increased as the level of EE increased. The 95% limits of agreement were large (-2.8 to 0.3 kcal/min). The Pearson correlation between EE measured by IC and AC (kcal/min) was 0.68 (P < .001).
Figure 1.
Bland–Altman Plot depicting mean difference and limits of agreement for the AC accelerometer.
Discussion
This study was the first to assess the EE associated with physically active classroom-based academic lessons using an IC. PAAC lessons elicited a mean EE of 3.1 ± 1.0 kcal/min, which represented on average, moderate- intensity activity in elementary school children. This level of EE was observed across both genders and grade levels (grades 2-5). Our estimates of EE during PAAC lessons are not likely biased toward increased or decreased activity in the child wearing the calorimeter as indicated by observation of nearly identical SOFIT scores for the participant and two other randomly selected children from the same class. Completing two 10-min PAAC lessons per day, which was the goal of the PAAC intervention, would expend approximately 62 kcal/d. This would eliminate approximately 50% of the positive energy balance (110-165 kcal/d) suggested by Wang et al. (32) to be responsible for the increase in body weight among children in the United States. Our results suggest that the level of EE achieved during classroom-based activity may aid in the prevention of weight gain in children, and that additional strategies to increase classroom physical activity should be developed and evaluated.
The AC significantly underestimated EE during PAAC lessons compared to that measured by IC. There are several possible explanations for this finding. Given the hypothesized sporadic nature of physical activity in this age group, the use of epochs shorter than the 1-min epochs used in this study has been suggested (19). Also, the regression equation used to estimate EE for AC counts may be inappropriate for use with the types of activities performed in PAAC lesson. The regression equation used in this study was developed in a laboratory setting and involved activities such as walking and jogging on a treadmill (30). These activities are different from those performed during a PAAC lesson, which included hopping, jumping, skipping, etc. at a variety of intensities, thus likely contributing to prediction error. The underestimation of EE by the AC may also be potentially explained by the inclusion of PAAC activities that primarily involve the upper extremities, activity which would not be detected by an AC worn at the waist. For example, PAAC lessons may include doing “jumping jacks” while performing math calculations or “arm circles” while participating in spelling lessons activities that would not be detected by the AC and may partially explain the significant underestimation of EE by the AC observed in this study.
Potential study limitations include the use of 1 AC, AC calibration procedure, and the inability to assess the EE of identical PAAC lessons delivered by different classroom teachers. One AC, selected from our inventory of approximately 65 units, was used for this study. The use of 1 AC, while eliminating the problem of inter-unit variability, may introduce a potential bias if the AC used was not in calibration. Although unlikely, as the AC used in our study was factory calibrated before use, and the calibration was assessed after completion of data collection, the potential for inaccurate calibration is not completely eliminated. Our reported EE for classroom-based physical activity as instituted during the PAAC intervention were derived by evaluating several different PAAC activities delivered by 19 different classroom teacher. We are therefore unable to assess the reliability to our EE estimated either within or between teachers.
In summary, our results indicate that EE of moderate intensity can be generated during physically active academic lessons taught by classroom teachers, and the level of EE elicited by PAAC lessons may be sufficient to aide in preventing excess weight gain in children. We have also shown that the AC using the Trost prediction equation (30) significantly underestimates EE during PAAC lessons suggesting that the AC may not be appropriate when assessing physical activity EE during classroom-based activity. In conclusion, our results suggest that future interventions to increase classroom physical activity should include an assessment of EE using indirect calorimetry rather than estimates of EE obtained from accelerometers. This information will allow investigators to evaluate the association between the level of EE delivered and change in body weight and to document the degree to which insufficient levels of EE may be responsible for the failure of the intervention to prevent weight gain.
Acknowledgments
This work was supported by grant NIHDK61489 from the National Institute of Diabetes and Digestive and Kidney Disease, Bethesda MD, awarded to Dr. Joseph E. Donnelly.
References
- 1.Bergstrom E, Hernell O, Persson LA, Vessby B. Insulin resistance syndrome in adolescents. Metabolism. 1996;45:908–14. doi: 10.1016/s0026-0495(96)90168-7. [DOI] [PubMed] [Google Scholar]
- 2.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 3.Brownell KD, Kaye FS. A school-based behavior modification, nutrition education, and physical activity program for obese children. Am J Clin Nutr. 1982;35:277–83. doi: 10.1093/ajcn/35.2.277. [DOI] [PubMed] [Google Scholar]
- 4.Caballero B, Clay T, Davis SM, et al. Pathways: a school-based randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Center for Disease Control and Prevention. Youth risk behavior surveillance—United States, 1997. Morbidity and Mortality Weekly Report. 1998;47:1–89. [PubMed] [Google Scholar]
- 6.Center for Disease Control and Prevention Web site [Internet] Atlanta (GA): 2000 Center for Disease Control Growth Charts; [cited 2007 June 1] www.cdc.gov/growthcharts/ [Google Scholar]
- 7.Dencker M, Thorsson O, Karlsson MK, et al. Daily physical activity related to body fat in children aged 8-11 years. JPediatr. 2006;149:38–42. doi: 10.1016/j.jpeds.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Dubose KD, Mayo MS, Gibson CA, et al. Physical activity across the curriculum (PAAC): Rationale and design. Contemp Clin Trials. 2007;29:83–93. doi: 10.1016/j.cct.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Goldfield GS, Mallory R, Parker T, et al. Effects of open-loop feedback on physical activity and television viewing in overweight and obese children: a randomized, controlled trial. Pediatrics. 2006;118:e157–66. doi: 10.1542/peds.2005-3052. [DOI] [PubMed] [Google Scholar]
- 10.Gortmaker SL, Dietz WH, Jr, Sobol AM, Wehler CA. Increasing pediatric obesity in the United States. Am JDis Child. 1987;141:535–40. doi: 10.1001/archpedi.1987.04460050077035. [DOI] [PubMed] [Google Scholar]
- 11.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153:409–18. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 12.Jiang X, Srinivasan SR, Berenson GS. Relation of obesity to insulin secretion and clearance in adolescents: the Bogalusa Heart Study. Int J Obes Relat Metab Disord. 1996;20:951–6. [PubMed] [Google Scholar]
- 13.Jiang X, Srinivasan SR, Webber LS, Wattigney WA, Berenson GS. Association of fasting insulin level with serum lipid and lipoprotein levels in children, adolescents, and young adults: the Bogalusa Heart Study. Arch Intern Med. 1995;155:190–6. [PubMed] [Google Scholar]
- 14.Liu AL, Hu XQ, Ma GS, et al. Report on childhood obesity in China (6) evaluation of a classroom-based physical activity promotion program. Biomed Environ Sci. 2007;20:19–23. [PubMed] [Google Scholar]
- 15.Mahar MT, Murphy SK, Rowe DA, Golden J, Shields AT, Raedeke TD. Effects of a classroom-based program on physical activity and on-task behavior. Med Sci Sports Exerc. 2006;38(12):2086–94. doi: 10.1249/01.mss.0000235359.16685.a3. [DOI] [PubMed] [Google Scholar]
- 16.McKenzie TL, Sallis JF, Nader PR. SOFIT: system for observing fitness instruction time. J Teach Phys Educ. 1991;11:195–205. [Google Scholar]
- 17.McLaughlin JE, King GA, Howley ET, Basset DR, Jr, Ainsworth BE. Validation of the COSMED K4 b2 portable metabolic system. Int J Sports Med. 2001;22:280–4. doi: 10.1055/s-2001-13816. [DOI] [PubMed] [Google Scholar]
- 18.Mo-Suwan L, Pongprapai S, Junjana C, Puetpaiboon A. Effects of a controlled trial of a school-based exercise program on the obesity indexes of preschool children. Am J Clin Nutr. 1998;68:1006–11. doi: 10.1093/ajcn/68.5.1006. [DOI] [PubMed] [Google Scholar]
- 19.Nilsson A, Ekelund U, Yngve A, Sjostrom M. Assessing physical activity among children with accelerometers using different time sampling intervals and placement. Pediatr Exerc Sci. 2002;14:87–97. [Google Scholar]
- 20.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 21.Pate RR, Long BJ, Heath G. Descriptive epidemiology of physical activity in adolescents. Pediatr Exerc Sci. 1994;6:434–47. [Google Scholar]
- 22.Richards GE, Cavilli A, Meyer WJ, Peters EJ, Stuart CA, Smith ER. Obesity, aconthosis nigricans, insulin resistance and hyper- androgemia: pediatric perspectives and natural history. J Pediatr. 1985;107:893–7. doi: 10.1016/s0022-3476(85)80182-7. [DOI] [PubMed] [Google Scholar]
- 23.Sahota P, Rudolf MCJ, Dixey R, Hill AJ, Barth JH, Cade J. Randomized controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ. 2001;323:1–5. doi: 10.1136/bmj.323.7320.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Srinivasan SR, Boa W, Wattigney WA, Berenson GS. Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors: The Bogalusa Heart Study. Metabolism. 1996;45:235–40. doi: 10.1016/s0026-0495(96)90060-8. [DOI] [PubMed] [Google Scholar]
- 25.Stein CJ, Colditz GA. The epidemic of obesity. J Clin Endocrinol Metab. 2004;89:2522–25. doi: 10.1210/jc.2004-0288. [DOI] [PubMed] [Google Scholar]
- 26.Steinberger J, Moorehead C, Katch V, Rocchinin AP. Relationship between insulin resistance and abnormal lipid profiles in obese adolescents. J Pediatr. 1995;126:690–5. doi: 10.1016/s0022-3476(95)70394-2. [DOI] [PubMed] [Google Scholar]
- 27.Stewart JA, Dennison DA, Kohl HW, Doyle JA. Exercise level and energy expenditure in the TAKE 10! in-class physical activity program. J Sch Health. 2004;74:397–400. doi: 10.1111/j.1746-1561.2004.tb06605.x. [DOI] [PubMed] [Google Scholar]
- 28.Strong WB, Malina RM, Blimkie CJ, et al. Evidence based physical activity for school-age youth. J Pediatr. 2005;146:732–7. doi: 10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 29.Thomas H. Obesity prevention programs for children and youth: why are their results so modest? Health Educ Res. 2006;21:783–95. doi: 10.1093/her/cyl143. [DOI] [PubMed] [Google Scholar]
- 30.Trost SG, Ward DS, Moorehead SM, Watson PD, Riner W, Burke JR. Validity of the computer science and applications (CSA) activity monitor in children. Med Sci Sports Exerc. 1998;30(4):629–33. doi: 10.1097/00005768-199804000-00023. [DOI] [PubMed] [Google Scholar]
- 31.Trost SG, Way R, Okely AD. Predictive validity of three ActiGraph energy expenditure equations for children. Med Sci Sports Exerc. 2006;38(2):380–7. doi: 10.1249/01.mss.0000183848.25845.e0. [DOI] [PubMed] [Google Scholar]
- 32.Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the energy gap among US children: a counterfactual approach. Pediatrics. 2006;118:e1721–33. doi: 10.1542/peds.2006-0682. [DOI] [PubMed] [Google Scholar]
- 33.WHO. World Health Organization. WHO Technical Report. 1985. Energy and Protein Requirements; report of Joint FAO/WHO/UNU Expert Consultation. [PubMed] [Google Scholar]