Abstract
Background
The authors conducted an observational cohort study to determine the levels of and examine the associations of oral health literacy (OHL) and oral health knowledge in low-income patients who were pregnant for the first time.
Methods
An analytic sample of 119 low-income patients who were pregnant for the first time completed a structured 30-minute, in-person interview conducted by two trained interviewers in seven counties in North Carolina. The authors measured OHL by means of a dental word recognition test and assessed oral health knowledge by administering a six-item knowledge survey.
Results
The authors found that OHL scores were distributed normally (mean [standard deviation], 16.4 [5.0]). The percentage of correct responses for each oral health knowledge item ranged from 45 to 98 percent. The results of bivariate analyses showed that there was a positive correlation between OHL and oral health knowledge (P < .01). Higher OHL levels were associated with correct responses to two of the knowledge items (P < .01).
Conclusions
OHL was low in the study sample. There was a significant association between OHL and oral health knowledge.
Clinical Implications
Low OHL levels and, thereby, low levels of oral health knowledge, might affect health outcomes for both the mother and child. Tailoring messages to appropriate OHL levels might improve knowledge.
Keywords: Vulnerable populations, health promotion, pregnancy, communication
More than six million women in the United States become pregnant annually,1 and approximately 40 percent of these women are pregnant for the first time.2 During pregnancy, women are at greater risk of experiencing poor oral health, which has been linked to adverse pregnancy outcomes including low birth weight and preterm birth delivery.3,4 Pregnant women also are susceptible to oral infections, pregnancy gingivitis, periodontitis and oral pyogenic granulomas.5,6 The investigators of a few studies reported that pregnant women in the United States have low levels of oral health knowledge about oral health during pregnancy and their children’s oral health.6–9
Health literacy is the degree to which people have the capacity to obtain, process and understand basic health information and services that are needed to make appropriate health decisions.10 The results of studies regarding health literacy showed that it had an association with health knowledge.11–14 In pregnant women, poor health knowledge resulting from low health literacy has the potential to influence the ease of self-care decisions and, thereby, health outcomes of both the woman and the fetus. Moreover, patients who are pregnant for the first time are considered to be a critical group of at-risk women who may be affected by low health literacy and therefore have poor health knowledge.15–20
Pregnant women with low health literacy have less pregnancy-related knowledge and poorer health behaviors.15–19 They also have less knowledge about prenatal screening tests for birth defects and the effects of smoking on the fetus.15–17 Pregnant women with pregestational diabetes and low health literacy are more likely to have unplanned pregnancy, fail to take folic acid to prevent birth defects and fail to consult a diabetes specialist or obstetrician before pregnancy.18 The results of studies showed that the prevalence of low health literacy among pregnant women ranged from 15 to 38 percent and was associated with older age and minority status.15,16,18,19
The National Institute of Dental and Craniofacial Research defines oral health literacy (OHL) as “the degree to which individuals have the capacity to obtain, process, and understand basic oral and craniofacial information and services needed to make appropriate health decisions.”21 The body of medical literature linking health literacy to health knowledge and behaviors continues to grow; however, far less is known about the influence of OHL on oral health knowledge. Just as health literacy affects a woman’s ability to understand and use pregnancy health information, we anticipate that OHL affects a women’s ability to understand and use oral health information during pregnancy. Studying the relationship between literacy and knowledge is particularly suited to dentistry because the maintenance of oral health relies on regular self-care behaviors that are influenced by oral health knowledge.
Preliminary evidence indicates that low OHL levels are associated with poor oral health knowledge9,22; however, this association has not been examined in pregnant women. Vann and colleagues9 found a significant positive correlation between OHL and oral health knowledge among low-income female caregivers. This finding was further supported by Macek and colleagues,22 who found an association between the word-recognition component of health literacy and oral health knowledge but not between reading comprehension and oral health knowledge.
In 2011, we reported OHL levels from the Carolina Oral Health Literacy (COHL) project parent study (N = 1,405), which included pregnant women.23 We believe that OHL has a greater impact on the oral health of patients who are pregnant for the first time compared with women who are not pregnant. Therefore, we decided to study the association between OHL and its correlates for women who are pregnant for the first time. The potential ramifications of low OHL levels and, thus, low levels of oral health knowledge are poorer health outcomes for both the pregnant woman and the fetus. In addition, investigators for the COHL project recruited participants from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), which is a health care network that has unique access to pregnant women and provides health services and information specifically related to pregnancy. WIC in North Carolina (NC) also provides oral health counseling and referrals for women and children, thus providing another population within WIC that may benefit from our study.
Assessment of OHL among patients who are pregnant for the first time has not been reported in the literature. We conducted a study to determine the levels of OHL among patients who were pregnant for the first time, the levels of oral health knowledge among patients who were pregnant for the first time, and the patterns of association between OHL and oral health know ledge among patients who were pregnant for the first time.
METHODS
Two trained interviewers collected data from 132 pregnant women by means of a structured 30-minute interview as part of the COHL project, which was approved by the Biomedical Institutional Review Board at the University of North Carolina at Chapel Hill.22 The main goal of the COHL project was for investigators to examine OHL and its association with oral health knowledge and health outcomes among caregivers, infants and children enrolled in WIC in NC. Participants were clients from nine sites in seven counties, which investigators selected in a nonprobabilty sample to generate a large and diverse low-income WIC study population. They obtained written informed consent from all participants. COHL project investigators used a prospective cohort study design described by Lee and colleagues.23
We included in our study a subset of 132 COHL project participants who were pregnant rather than children and their caregivers (child-caregiver dyads). We excluded three pregnant women who had children (2.3 percent) and 10 pregnant women whose primary language was not English (7.6 percent). Our final sample was 119 patients who were pregnant for the first time.
The major outcome variable was OHL as measured by means of a validated word recognition test, the Rapid Estimate of Adult Literacy in Dentistry-30 (REALD-30). REALD-30 is an instrument with good convergent validity and internal consistency (Cronbach α = 0.87).24 REALD-30 scores range from 0 (lowest literacy) to 30 (highest literacy).
To assess oral health–related knowledge, we administered a six-item knowledge survey.25,26 We asked the women to answer “agree,” “disagree” or “don’t know” to knowledge-related statements such as “Fluoride helps prevent tooth decay” and “Tooth decay in baby teeth can cause infections that can spread to the face and other parts of the body.” We combined the response “don’t know” with incorrect responses when we compiled the composite knowledge score and conducted bivariate analyses. We derived a composite knowledge score from the sum of correct responses; the scores ranged from zero to six. We collapsed the composite knowledge scores by units of two a priori and reported them as a three-level categorical variable. Although only two participants were in the lowest composite knowledge score category, we believe it deserved to be a stand-alone category because the REALD-30 scores were sufficiently low to skew the REALD-30 score mean of the next categorical variable.
We collected demographic information for county of residence, race, ethnicity, education level, marital status and age. We coded race as white, African American (AA) and American Indian or Alaskan Native (AI). We coded ethnicity as Hispanic/Latino, non-Hispanic/non-Latino and unknown. We coded education as a three-level categorical variable (did not finish high school, received a high school or General Educational Development diploma, or completed some college or higher education). We coded marital status as a three-level categorical variable (single, married or separated or divorced). We measured age in years and coded it as a three-level categorical variable (18 years, 19–24 years or older than 24 years).
We used descriptive statistics to examine the distribution of participants’ demographic characteristics, and we measured OHL by using REALD-30 scores. We tested the normality assumption for REALD-30 scores by means of a combined skewness and kurtosis evaluation test by using the P < .05 criterion.27
We conducted a linear regression analysis to investigate bivariate associations between OHL and the following covariates: county of residence, race, ethnicity, education level, marital status, age and oral health knowledge. We used robust standard errors to adjust for heteroscedasticity. We conducted all analyses by using statistical software (STATA 10.1, StataCorp, College Station, Texas).
RESULTS
Table 1 shows the demographic characteristics of our analytic sample (N = 119) and the corresponding OHL levels (REALD-30 scores) are presented in Table 1. There was a 5:5:2 ratio of white, AA and AI patients. Owing to small numbers of participants in other racial groups, we report Hispanic ethnicity for white patients only (seven of 52 [13 percent]). The mean (standard deviation [SD]) age was 22.2 years (3.9).
TABLE 1.
Distribution of baseline REALD-30* scores, according to demographic characteristics among Carolina Oral Health Literacy study participants who were pregnant for the first time (N = 119).
| DEMOGRAPHIC CHARACTERISTIC | PARTICIPANTS, NO.† (%) | REALD-30 SCORE, MEAN (STANDARD DEVIATION) | BIVARIATE REGRESSION COEFFICIENT, P VALUE |
|---|---|---|---|
|
| |||
| Total Sample | 119 (100) | 16.4 (5.0) | NA‡ |
| County of Residence | |||
| Buncombe | 8 (7) | 19.9 (4.3) | 3.71 (.001) |
| Burke | 3 (3) | 20.3 (5.8) | |
| New Hanover | 12 (10) | 17.3 (5.1) | |
| Orange | 12 (10) | 14.3 (2.4) | |
| Robeson | 31 (26) | 15.1 (5.7) | |
| Wake | 53 (45) | 16.7 (4.7) | |
|
| |||
| Race | |||
| White | 52 (44) | 18.1 (4.6) | 6.33 (.003) |
| African American | 47 (39) | 15.4 (4.6) | |
| American Indian | 20 (17) | 14.3 (5.4) | |
|
| |||
| Hispanic/Latino Ethnicity (Among White Participants [n = 52]) | |||
| Yes | 7 (13) | 20.4 (2.8) | 2.02 (.04) |
| No | 45 (87) | 17.8 (4.8) | |
|
| |||
| Education Level§ | |||
| Did not finish high school | 30 (25) | 13.6 (3.3) | 27.74 (< .001) |
| Received a high school or General Educational Development diploma | 36 (30) | 15.6 (4.7) | |
| Completed some college or higher education | 53 (45) | 18.5 (5.1) | |
|
| |||
| Marital Status | |||
| Single | 96 (81) | 15.8 (4.8) | 5.19 (.007) |
| Married | 16 (13) | 20.2 (5.3) | |
| Separated or divorced | 6 (5) | 16.0 (0.9) | |
|
| |||
| Age, Years¶ | |||
| 18 | 26 (22) | 14.7 (3.6) | 7.23 (.08) |
| 19–24 | 66 (55) | 16.5 (5.4) | |
| > 24 | 27 (23) | 17.8 (4.7) | |
REALD-30: Rapid Estimate of Adult Literacy in Dentistry-30.
Number of responses.
NA: Not applicable.
Values nay not add up to the total owing to missing information.
Mean (standard deviation) years, 22.2 (3.9); median years, 21.2; range, 18.1–39.3.
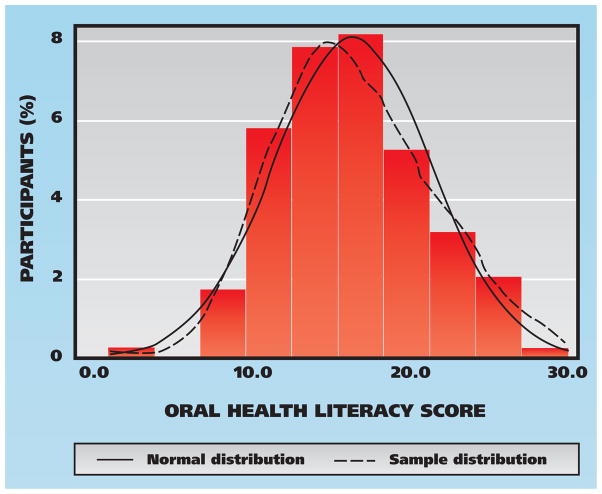
The overall distribution of REALD-30 scores among patients who were pregnant for the first time is shown in the figure (page 976). REALD-30 scores were distributed normally (χ2 = 1.12, P > .05), with a mean (SD) of 16.4 (5.0), a median of 16 and a range of one to 30. With regard to sociodemographic covariates, participants had higher REALD-30 scores if they were white or married or had completed some college or higher education (P < .05) (Table 1).
Figure.
Distribution of oral health literacy (Rapid Estimate of Adult Literacy in Dentistry-30) scores among Carolina Oral Health Literacy study participants who were pregnant for the first time (N = 119; mean [standard deviation], 16.4 [5.0]).
Participants’ knowledge scores were distributed nonnormally (χ2 = 7.20, P < .05), with a mean (SD) of 4.8 (1.0), a median of 5.0 and a range of two to six. More than two-thirds of participants correctly answered five or more oral health knowledge items (Table 2, page 977). The proportion of correct responses for each oral health knowledge item ranged from 45 to 98 percent. The oral health knowledge item “Fluoride disinfects water and makes it safe to drink” received the greatest number of incorrect responses (18 [15 percent]). The oral health knowledge item “Cleaning baby teeth is not important because they fall out anyway” received the greatest number of correct responses (117 [98 percent]).
TABLE 2.
Responses to dental knowledge items by Carolina Oral Health Literacy study participants who were pregnant for the first time (N = 119).
| DENTAL KNOWLEDGE ITEM | AGREE, NO. (%)OF PARTICIPANTS | DISAGREE, NO. (%)OF PARTICIPANTS | DON’T KNOW, NO. (%)OF PARTICIPANTS |
|---|---|---|---|
| Cleaning baby teeth is not important because they fall out anyway | 2 (2) | 117 (98)* | 0 (0) |
| A child’s overall health does not depend on whether he or she has cavities in baby teeth | 4 (3) | 114 (96)* | 1 (1) |
| Fluoride disinfects water and makes it safe to drink | 18 (15) | 53 (45)* | 48 (40) |
| A cavity in a baby tooth should be filled only when it hurts | 1 (1) | 109 (92)* | 9 (8) |
| Fluoride helps prevent tooth decay | 87 (73)* | 5 (4) | 27 (23) |
| Tooth decay in baby teeth can cause infections that can spread to the face and other parts of the body | 88 (74)* | 5 (4) | 26 (22) |
Correct response.
We found that higher REALD-30 scores were associated with correct responses to two oral health knowledge items (P < .01) (Table 3, page 978): “Fluoride helps prevent tooth decay” and “Tooth decay in baby teeth can cause infections that can spread to the face and other parts of the body.”
TABLE 3.
Distribution of baseline REALD-30* scores, according to dental knowledge among Carolina Oral Health Literacy study participants who were pregnant for the first time (N = 119).
| DENTAL KNOWLEDGE | PARTICIPANTS, NO.† (%) | REALD-30 SCORE, MEAN (STANDARD DEVIATION) | BIVARIATE REGRESSION COEFFICIENT, P VALUE |
|---|---|---|---|
|
| |||
| Total Sample | 119 (100) | 16.4 (5.0) | NA‡ |
|
| |||
| Dental Knowledge Score | |||
| Number of correct responses (total no. of items = 6) | |||
| 0–2 | 2 (2) | 5.0 (5.7) | 9.36 (.003) |
| 3–4 | 37 (31) | 15.1 (4.1) | |
| 5–6 | 80 (67) | 17.3 (4.9) | |
|
| |||
| Responses to Individual Items | |||
| Cleaning baby teeth is not important because they fall out anyway | |||
| Correct | 117 (98) | 16.4 (5.0) | 0.00 (.954) |
| Incorrect/Don’t know | 2 (2) | 16.5 (3.5) | |
| A child’s overall health does not depend on whether he or she has cavities in baby teeth | |||
| Correct | 114 (96) | 16.6 (4.8) | 2.92 (.09) |
| Incorrect/Don’t know | 5 (4) | 12.0 (6.6) | |
| Fluoride disinfects water and makes it safe to drink | |||
| Correct | 53 (45) | 15.9 (4.9) | 0.86 (.4) |
| Incorrect/Don’t know | 66 (55) | 16.8 (5.0) | |
| A cavity in a baby tooth should be filled only when it hurts | |||
| Correct | 109 (92) | 16.4 (4.9) | 0.14 (.7) |
| Incorrect/Don’t know | 10 (8) | 15.8 (5.5) | |
| Fluoride helps prevent tooth decay | |||
| Correct | 87 (73) | 17.2 (4.8) | 8.24 (.005) |
| Incorrect/Don’t know | 32 (27) | 14.3 (4.8) | |
| Tooth decay in baby teeth can cause infections that can spread to the face and other parts of the body | |||
| Correct | 88 (74) | 17.2 (5.0) | 9.65 (.002) |
| Incorrect/Don’t know | 31 (26) | 14.2 (4.4) | |
REALD-30: Rapid Estimate of Adult Literacy in Dentistry-30.
Number of people in stratum.
NA: Not applicable.
We found a positive correlation between REALD-30 scores and the composite oral health knowledge score, indicating that higher levels of knowledge are associated with higher levels of OHL in our sample (P < .01) (Table 3). The two participants who answered zero to two knowledge items correctly had a mean (SD) REALD-30 score of 5.0 (5.7). Comparatively, participants who answered three to four knowledge items correctly had a mean (SD) REALD-30 score of 15.1 (4.1) and five to six knowledge items correctly had a mean (SD) REALD-30 score of 17.3 (4.9).
DISCUSSION
We are the first to report OHL levels in patients who were pregnant for the first time, which means there are no samples of pregnant women with which to make comparisons. We consider our findings regarding OHL to be low compared with those of previous studies with sample populations that were not limited to pregnant women. OHL levels obtained by using the same REALD-30 instrument in a private dental office (mean [SD], 23.9 [1.3]),28 an outpatient medical clinic (mean [SD], 19.8 [6.4])24 and a dental school (mean [SD], 20.7 [5.5])29 were higher. The results of the COHL project parent study showed that the lowest quartile of REALD-30 scores was scores of less than 13, which was defined as low OHL.9 According to this threshold, in our study, 17 (23 percent) participants who were pregnant for the first time had low OHL levels (results not shown). The fact that the participants who were pregnant for the first time within this WIC population had low OHL levels compared with those of other study populations24,28,29 is important because of the potential adverse effects of low OHL levels on the health of the pregnant woman and the fetus.
Although norms of low functional health literacy are not yet established, the finding of low OHL levels among low-income pregnant women is consistent with low levels of general health literacy among low-income pregnant women in the medical literature.15,16,18,19 Despite the fact that there was no difference in education levels, 84 (28 percent) low-income pregnant AA women had health literacy below a seventh-grade reading level compared with 26 (9 percent) higher-income pregnant white women (P < .001).15 Cho and colleagues16 found that 38 (38 percent) low-income pregnant women had a health literacy level below the ninth-grade reading level. Comparatively, health information routinely is written at a 10th-grade reading level.30,31
One mechanism by which literacy affects knowledge is information seeking. According to Shieh and colleagues,19 “addressing health literacy has the potential to influence information seeking and subsequently, health knowledge and behaviors in pregnant women.” Patients who are pregnant for the first time are more likely to seek health information, which provides a window of opportunity for improving health knowledge.20 In addition, pregnant women are more motivated to reduce negative health behaviors, such as smoking, that might harm the developing fetus.32 Low health literacy, however, is a barrier to information seeking, which may explain why many pregnant women have low levels of oral health knowledge regarding pregnancy and children’s oral health.19,31 This finding suggests that the positive correlation of health literacy with information seeking may be more likely to lead to increased knowledge and healthy behaviors during pregnancy and vice versa.
Another mechanism by which literacy may affect knowledge is the lack of appropriate health education and communication techniques that practitioners can use with patients with low health literacy. Study results have shown the need for better patient education and communication regarding dental care,33 especially during pregnancy.34 Buerlein and colleagues35 reported that “plain language, a cornerstone for increasing oral health literacy, must be used to explain concepts.” For pregnant women, having the correct knowledge to prevent and control oral disease during pregnancy and early childhood is of great importance because it affects both the mother and the child. In addition, dentists perceive that there are barriers to communicating with pregnant women such as cultural and linguistic differences,36 inadequate insurance reimbursement37,38 and having incorrect professional knowledge,37,38 all of which compound the difficulty of providing timely and literacy level–appropriate health information to pregnant women.
In our study, there was a variation in the number of correct responses to oral health knowledge items related to fluoride. Seventy-three percent of participants (n = 87) correctly responded to the knowledge item “Fluoride helps prevent tooth decay,” and 45 percent of participants (n = 53) correctly responded to the knowledge item “Fluoride disinfects water and makes it safe to drink.” A study conducted by Boggess and colleagues39 had similar results for the same questions (87 percent and 50 percent, respectively), but their sample was pregnant women at an academic health center who were not enrolled in WIC. Their finding suggests that pregnant women generally are aware that fluoride is good for their teeth, but they may not understand why it is beneficial, how to use it and why it is provided through different vehicles. Buerlein and colleagues35 conducted a qualitative study and found that “messages promoting consumption of tap water for its fluoride content created confusion and were ineffective, because many participants believed that tap water is to be avoided due to its lead content.” This example of a conflicting public health message may be more difficult to navigate in a population with low literacy levels. Thus, the difference in knowledge scores between the fluoride knowledge items in our study may reflect the difficulty of conveying particular information to an audience with low OHL levels.
Because the oral health knowledge item, “Fluoride disinfects water and makes it safe to drink,” received the greatest number of incorrect responses, fluoride should be the target of anticipatory guidance counseling regarding perinatal and infant oral health. Prenatal programs for low-income minority women at high risk of developing caries can lead to improved oral health knowledge.40 There also is evidence that the effect of educational interventions regarding knowledge can be modified by health literacy.41 In other words, health knowledge improves when health education programs are tailored to people with low health literacy.41
Improving patients’ knowledge about fluoride has the potential to improve oral health for low-income pregnant women who are at high risk of developing caries and who have access to fluoridated tap water. Fluoridated tap water also is an economical alternative to bottled water for low-income pregnant women. Not only can a patient’s oral health knowledge be improved by tailoring health messages to her OHL level, but also OHL may be the key to explaining why the efforts to increase access to care do not lead to improved care-seeking behaviors and oral health outcomes in pregnant women.
Limitations and strengths
The results of our study should be considered in light of the study’s limitations. COHL project investigators collected the data from a nonprobability sample of patients who were pregnant for the first time and who were enrolled in WIC in NC. Although sample characteristics limit external validity, women enrolled in WIC are an important population to examine. WIC is uniquely positioned to identify low-income pregnant women and provide services to those with low health literacy levels. WIC serves more than 270,000 women, infants and children monthly in NC,42 and more than 8 million people annually in the United States.43 WIC also serves more than one-quarter of all infants born in the United States today and a majority of young pregnant women.44 For example, 22 percent of the women in our sample were 18 years old and would be expected to be less educated because they most likely had graduated only from high school by that age. As we anticipated, the women in this group also had lower OHL. This finding underscores the ramifications that health promotion strategies may have in this population of women.
Our sample was limited to English-speaking patients because REALD-30 has been validated in English only. We also acknowledge that reliance on self-reported data is a potential study limitation. For example, it is possible that pregnant women who do not value oral health may report less accurate oral health information. Another limitation is the small sample size; however, investigators in studies in the medical literature regarding general health literacy in pregnant women have reported that their studies had similar sample sizes.15,16,18,19
The results of our study add to the knowledge base by reporting the OHL level of a previously unstudied population: pregnant women. Millions of pregnant women have oral diseases, and oral diseases in general affect minority and low-income women at a higher rate.1,5,6,45 Our findings establish a strong case for addressing OHL with pregnant women and setting the stage for potential OHL interventions for these women. Health care professionals and public health workers, both within and outside of WIC, can spearhead the effort to create OHL interventions for pregnant women. Dentists and staff members who are in private practice can adjust their communications to the literacy levels of their patients, with particular attention paid to pregnant women, owing to the heightened repercussions of having oral diseases to the woman and fetus during pregnancy. Investigators in future studies should examine effective social cognitive approaches that can be used to tailor messages during counseling sessions that can assist pregnant women to overcome barriers in OHL.
CONCLUSIONS
Among women who were pregnant for the first time, OHL levels were associated significantly with oral health knowledge. Because OHL levels were low in this at-risk population, dental professionals and public health workers should be aware that messages can be tailored to the patients’ OHL levels to improve oral health knowledge effectively in this vulnerable group.
Acknowledgments
The research was supported by National Institute of Dental and Craniofacial Research grants RO1DE018045 and T32DE017245.
ABBREVIATION KEY
- AA
African American
- AI
American Indian or Alaskan Native
- COHL
Carolina Oral Health Literacy
- NC
North Carolina
- OHL
Oral health literacy
- REALD-30
Rapid Estimate of Adult Literacy in Dentistry-30
- WIC
Special Supplemental Nutrition Program for Women, Infants, and Children
Footnotes
Disclosure. None of the authors reported any disclosures.
Contributor Information
Dr. Jacqueline M. Hom, Department of Pediatric Dentistry, School of Dentistry, and a doctoral candidate, Department of Health Policy and Management, Gillings School of Global Public Health, University of North Carolina at Chapel Hill.
Dr. Jessica Y. Lee, Department of Pediatric Dentistry, School of Dentistry, and a professor, Department of Health Policy and Management, Gillings School of Global Public Health, University of North Carolina at Chapel Hill. She was an associate professor, Department of Pediatric Dentistry, School of Dentistry, and an associate professor, Department of Health Policy and Management, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, when this article was written.
Dr. Kimon Divaris, Department of Pediatric Dentistry, School of Dentistry, University of North Carolina at Chapel Hill. He was a PhD candidate, Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, when this article was written.
Ms. A. Diane Baker, Department of Pediatric Dentistry, School of Dentistry, University of North Carolina at Chapel Hill.
Dr. William F. Vann, Jr., Department of Pediatric Dentistry, School of Dentistry, University of North Carolina at Chapel Hill.
References
- 1.Ventura SJ, Abma JC, Mosher WD, Henshaw S. Estimated pregnancy rates for the United States, 1990–2000: an update. Natl Vital Stat Rep. 2004;52(23):1–9. [PubMed] [Google Scholar]
- 2.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Osterman MJ. Births: final data for 2008. Natl Vital Stat Rep. 2010;59(1):1, 3–71. [PubMed] [Google Scholar]
- 3.Vergnes JN, Sixou M. Preterm low birth weight and maternal periodontal status: a meta-analysis. Am J Obstet Gynecol. 2007;196(2):135.e1–e7. doi: 10.1016/j.ajog.2006.09.028. [DOI] [PubMed] [Google Scholar]
- 4.Xiong X, Buekens P, Fraser WD, Beck J, Offenbacher S. Periodontal disease and adverse pregnancy outcomes: a systematic review. BJOG. 2006;113(2):135–143. doi: 10.1111/j.1471-0528.2005.00827.x. [DOI] [PubMed] [Google Scholar]
- 5.Barak S, Oettinger-Barak O, Oettinger M, Machtei EE, Peled M, Ohel G. Common oral manifestations during pregnancy: a review. Obstet Gynecol Surv. 2003;58(9):624–628. doi: 10.1097/01.OGX.0000083542.14439.CF. [DOI] [PubMed] [Google Scholar]
- 6.New York State Department of Health. Oral Health Care During Pregnancy and Early Childhood: Practice Guidelines. New York City: New York State Department of Health; 2006. [Accessed July 11, 2012]. www.health.state.ny.us/publications/0824.pdf. [Google Scholar]
- 7.Al Habashneh R, Guthmiller JM, Levy S, et al. Factors related to utilization of dental services during pregnancy. J Clin Periodontol. 2005;32(7):815–821. doi: 10.1111/j.1600-051X.2005.00739.x. [DOI] [PubMed] [Google Scholar]
- 8.Gilbert BC, Shulman HB, Fischer LA, Rogers MM. The pregnancy risk assessment monitoring system (PRAMS): methods and 1996 response rates from 11 states. Matern Child Health J. 1999;3(4):199–209. doi: 10.1023/a:1022325421844. [DOI] [PubMed] [Google Scholar]
- 9.Vann WF, Jr, Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: impact on oral health outcomes in early childhood. J Dent Res. 2010;89(12):1395–1400. doi: 10.1177/0022034510379601. (published online ahead of print Oct. 5, 2010) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2. Washington: U.S. Government Printing Office; 2000. pp. 11–20. [Google Scholar]
- 11.Dennison CR, McEntee ML, Samuel L, et al. Adequate health literacy is associated with higher heart failure knowledge and self-care confidence in hospitalized patients. J Cardiovasc Nurs. 2011;26(5):359–367. doi: 10.1097/JCN.0b013e3181f16f88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124(suppl 3):S265–S274. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 13.Macabasco-O’Connell A, DeWalt DA, Broucksou KA, et al. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure (published online ahead of print March 3, 2011) J Gen Intern Med. 2011;26(9):979–986. doi: 10.1007/s11606-011-1668-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Intern Med. 1998;158(2):166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 15.Arnold CL, Davis TC, Berkel HJ, Jackson RH, Nandy I, London S. Smoking status, reading level, and knowledge of tobacco effects among low-income pregnant women. Prev Med. 2001;32(4):313–320. doi: 10.1006/pmed.2000.0815. [DOI] [PubMed] [Google Scholar]
- 16.Cho RN, Plunkett BA, Wolf MS, Simon CE, Grobman WA. Health literacy and patient understanding of screening tests for aneuploidy and neural tube defects. Prenat Diagn. 2007;27(5):463–467. doi: 10.1002/pd.1712. [DOI] [PubMed] [Google Scholar]
- 17.Gazmararian JA, Parker RM, Baker DW. Reading skills and family planning knowledge and practices in a low-income managed-care population. Obstet Gynecol. 1999;93(2):239–244. doi: 10.1016/s0029-7844(98)00431-1. [DOI] [PubMed] [Google Scholar]
- 18.Endres LK, Sharp LK, Haney E, Dooley SL. Health literacy and pregnancy preparedness in pregestational diabetes. Diabetes Care. 2004;27(2):331–334. doi: 10.2337/diacare.27.2.331. [DOI] [PubMed] [Google Scholar]
- 19.Shieh C, Mays R, McDaniel A, Yu J. Health literacy and its association with the use of information sources and with barriers to information seeking in clinic-based pregnant women. Health Care Women Int. 2009;30(11):971–988. doi: 10.1080/07399330903052152. [DOI] [PubMed] [Google Scholar]
- 20.Shieh C, McDaniel A, Ke I. Information-seeking and its predictors in low-income pregnant women. J Midwifery Womens Health. 2009;54(5):364–372. doi: 10.1016/j.jmwh.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 21.National Institute of Dental and Craniofacial Research, National Institutes of Health, U S. Public Health Service, Department of Health and Human Services. The invisible barrier: literacy and its relationship with oral health—a report of a workgroup sponsored by the National Institute of Dental and Craniofacial Research, National Institutes of Health, U.S Public Health Service, Department of Health and Human Services. J Public Health Dent. 2005;65(3):174–182. doi: 10.1111/j.1752-7325.2005.tb02808.x. [DOI] [PubMed] [Google Scholar]
- 22.Macek MD, Haynes D, Wells W, Bauer-Leffler S, Cotten PA, Parker RM. Measuring conceptual health knowledge in the context of oral health literacy: preliminary results. J Public Health Dent. 2010;70(3):197–204. doi: 10.1111/j.1752-7325.2010.00165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JY, Divaris K, Baker AD, Rozier RG, Lee SY, Vann WF., Jr Oral health literacy levels among a low-income WIC population. J Public Health Dent. 2011;71(2):152–160. doi: 10.1111/j.1752-7325.2011.00244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee JY, Rozier RG, Lee SY, Bender D, Ruiz RE. Development of a word recognition instrument to test health literacy in dentistry: the REALD-30—a brief communication. J Public Health Dent. 2007;67(2):94–98. doi: 10.1111/j.1752-7325.2007.00021.x. [DOI] [PubMed] [Google Scholar]
- 25.Mathu-Muju KR, Lee JY, Zeldin LP, Rozier RG. Opinions of Early Head Start staff about the provision of preventive dental services by primary medical care providers. J Public Health Dent. 2008;68(3):154–162. doi: 10.1111/j.1752-7325.2007.00052.x. [DOI] [PubMed] [Google Scholar]
- 26.Shick EA, Lee JY, Rozier RG. Determinants of dental referral practices among WIC nutritionists in North Carolina. J Public Health Dent. 2005;65(4):196–202. doi: 10.1111/j.1752-7325.2005.tb03018.x. [DOI] [PubMed] [Google Scholar]
- 27.D’Agostino RB, Belanger A, D’Agostino RB., Jr A suggestion for using powerful and informative tests of normality. Am Statistician. 1990;44(4):316–321. [Google Scholar]
- 28.Jones M, Lee JY, Rozier RG. Oral health literacy among adult patients seeking dental care. JADA. 2007;138(9):1199–1208. doi: 10.14219/jada.archive.2007.0344. [DOI] [PubMed] [Google Scholar]
- 29.Miller E, Lee JY, DeWalt DA, Vann WF., Jr Impact of caregiver literacy on children’s oral health outcomes (published online ahead of print June 14, 2010) Pediatrics. 2010;126(1):107–114. doi: 10.1542/peds.2009-2887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arnold CL, Davis TC, Frempong JO, et al. Assessment of newborn screening parent education materials. Pediatrics. 2006;117(5 pt 2):S320–S325. doi: 10.1542/peds.2005-2633L. [DOI] [PubMed] [Google Scholar]
- 31.D’Allesandro DM, Kingsley P, Johnson-West J. The readability of pediatric patient education materials on the World Wide Web. Arch Pediatr Adolesc Med. 2001;155(7):807–812. doi: 10.1001/archpedi.155.7.807. [DOI] [PubMed] [Google Scholar]
- 32.Curry SJ, McBride C, Grothaus L, Lando H, Pirie P. Motivation for smoking cessation among pregnant women. Psychol Addict Behav. 2001;15(2):126–132. doi: 10.1037//0893-164x.15.2.126. [DOI] [PubMed] [Google Scholar]
- 33.Rozier RG, Horowitz AM, Podschun G. Dentist-patient communication techniques used in the United States: the results of a national survey. JADA. 2011;142(5):518–530. doi: 10.14219/jada.archive.2011.0222. [DOI] [PubMed] [Google Scholar]
- 34.Strafford KE, Shellhaas C, Hade EM. Provider and patient perceptions about dental care during pregnancy. J Matern Fetal Neonatal Med. 2008;21(1):63–71. doi: 10.1080/14767050701796681. [DOI] [PubMed] [Google Scholar]
- 35.Buerlein JK, Horowitz AM, Child WL. Perspectives of Maryland women regarding oral health during pregnancy and early childhood. J Public Health Dent. 2011;71(2):131–135. doi: 10.1111/j.1752-7325.2010.00211.x. [DOI] [PubMed] [Google Scholar]
- 36.Da Costa EP, Lee JY, Rozier RG, Zeldin L. Dental care for pregnant women: an assessment of North Carolina general dentists. JADA. 2010;141(8):986–994. doi: 10.14219/jada.archive.2010.0312. [DOI] [PubMed] [Google Scholar]
- 37.Huebner CE, Milgrom P, Conrad D, Lee RS. Providing dental care to pregnant patients: a survey of Oregon general dentists. JADA. 2009;140(2):211–222. doi: 10.14219/jada.archive.2009.0135. [DOI] [PubMed] [Google Scholar]
- 38.Lee RS, Milgrom P, Huebner CE, Conrad DA. Dentists’ perceptions of barriers to providing dental care to pregnant women. Womens Health Issues. 2010;20(5):359–365. doi: 10.1016/j.whi.2010.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boggess KA, Urlaub DM, Moos MK, Polinkovsky M, El-Khorazaty J, Lorenz C. Knowledge and beliefs regarding oral health among pregnant women. JADA. 2011;142(11):1275–1282. doi: 10.14219/jada.archive.2011.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaste LM, Sreenivasan D, Koerber A, Punwani I, Fadavi S. Pediatric oral health knowledge of African American and Hispanic of Mexican origin expectant mothers. Pediatr Dent. 2007;29(4):287–292. [PubMed] [Google Scholar]
- 41.Kandula NR, Nsiah-Kumi PA, Makoul G, et al. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program (published online ahead of print April 22, 2009) Patient Educ Couns. 2009;75(3):321–327. doi: 10.1016/j.pec.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 42.North Carolina Nutrition Services Branch. North Carolina special supplemental nutrition program for women, infants, and children. [Accessed July 11, 2012];Women, infants & children: WIC history. 2011 www.nutritionnc.com/wic/history.htm.
- 43.Kresge J. WIC Participant and Program Characteristics PC2002: Executive Summary. U.S. Department of Agriculture, Food and Nutrition Service, Office of Analysis, Nutrition and Evaluation; 2003. [Accessed July 11, 2012]. p. iv. www.fns.usda.gov/ora/menu/published/wic/FILES/PC2002ExecSum.pdf. [Google Scholar]
- 44.FY 2013 Budget Summary and Annual Performance Plan. Washington: U.S. Department of Agriculture; 2012. [Accessed July 11, 2012]. p. 60. www.obpa.usda.gov/budsum/FY13budsum.pdf. [Google Scholar]
- 45.Oral Health in America: A Report of the Surgeon General. Rockville, Md: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. pp. 61–89. [Google Scholar]