Abstract
Controversy exists regarding the potential regenerative influences of incretin therapy on pancreatic β-cells versus possible adverse pancreatic proliferative effects. Examination of pancreata from age-matched organ donors with type 2 diabetes mellitus (DM) treated by incretin therapy (n = 8) or other therapy (n = 12) and nondiabetic control subjects (n = 14) reveals an ∼40% increased pancreatic mass in DM treated with incretin therapy, with both increased exocrine cell proliferation (P < 0.0001) and dysplasia (increased pancreatic intraepithelial neoplasia, P < 0.01). Pancreata in DM treated with incretin therapy were notable for α-cell hyperplasia and glucagon-expressing microadenomas (3 of 8) and a neuroendocrine tumor. β-Cell mass was reduced by ∼60% in those with DM, yet a sixfold increase was observed in incretin-treated subjects, although DM persisted. Endocrine cells costaining for insulin and glucagon were increased in DM compared with non-DM control subjects (P < 0.05) and markedly further increased by incretin therapy (P < 0.05). In conclusion, incretin therapy in humans resulted in a marked expansion of the exocrine and endocrine pancreatic compartments, the former being accompanied by increased proliferation and dysplasia and the latter by α-cell hyperplasia with the potential for evolution into neuroendocrine tumors.
Type 2 diabetes mellitus (DM) is characterized by defective insulin secretion in the setting of insulin resistance, leading to hyperglycemia. This defect in insulin secretion is accompanied by a deficit in β-cell mass. However, the extent and relevance of this β-cell deficit has been questioned, in part due to the paucity of human pancreatic studies as well as to methodological differences among such efforts (1–3). Therapeutic hope for DM has recently been raised by the introduction of a glucagon-like peptide-1 (GLP-1) mimetic class of drugs widely referred to as incretins. Interestingly, beyond their effects on improved metabolic regulation, GLP-1 mimetic therapy was also noted to induce β-cell regeneration in rodents, thus portending the remarkable notion that the deficit in β-cell mass in DM might be overcome with such agents (4–7). However, given this ability was most evident in the period coincident with the postnatal expansion of β-cell mass in rodents, questions arose as to the relevance of this property of GLP-1 in adult humans (8,9). Moreover, β-cell replication was not detected in human islets exposed to high concentrations of GLP-1 in vitro (10). In contrast, there are concerns that the proproliferative actions of GLP-1 might induce deleterious effects on the exocrine pancreas, in which the capacity for the proproliferative actions of GLP-1 appears to be better retained into adult life (5,11,12).
To address this, we analyzed a series of high-quality (i.e., transplant grade) human pancreata obtained from brain-dead organ donors with and without DM, including a subgroup of the latter who underwent ≥1 year of incretin therapy (13). Our goals were to confirm that β-cell mass was indeed decreased with DM overall and to establish whether incretin therapy induced an expansion of the endocrine and/or exocrine pancreas.
RESEARCH DESIGN AND METHODS
Study subjects.
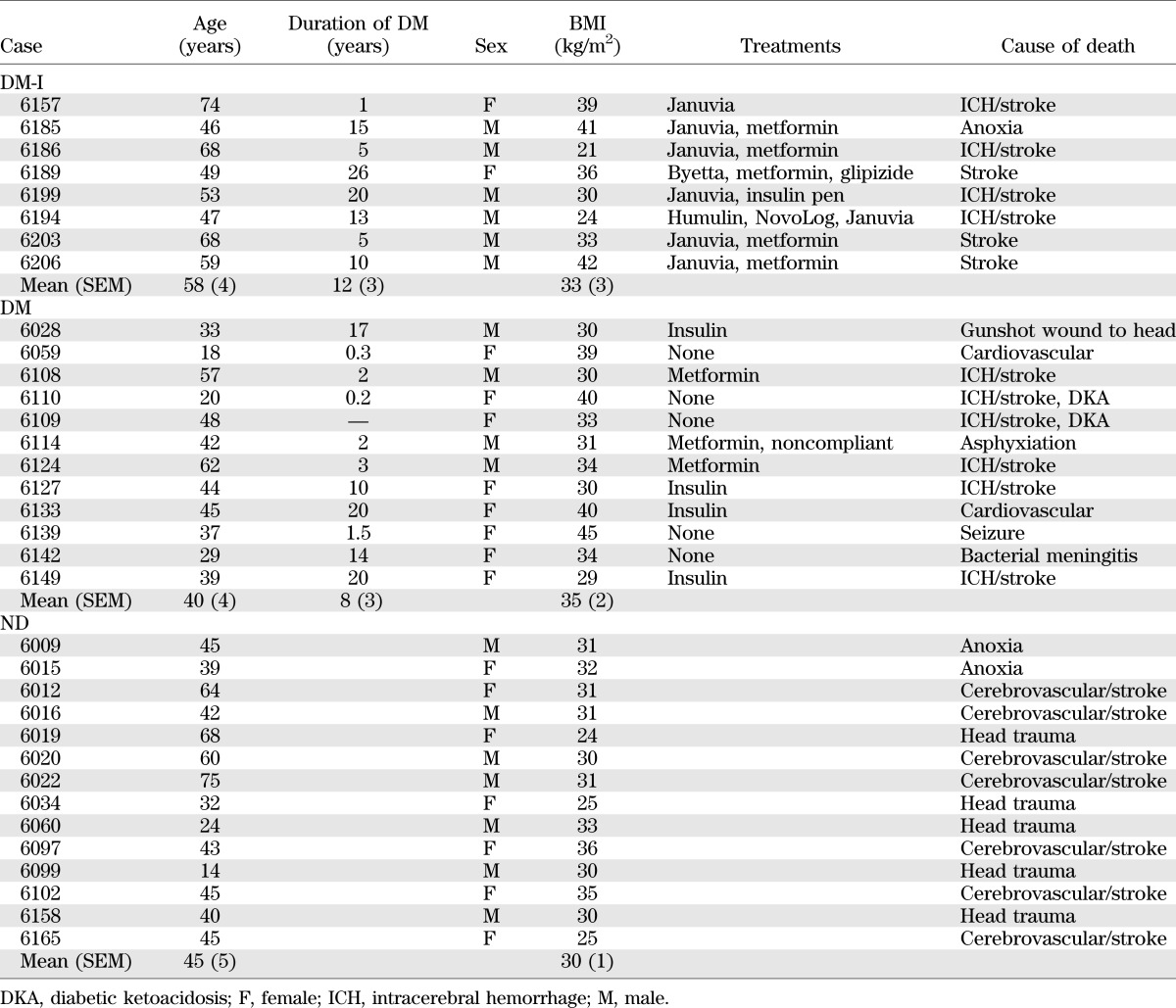
All pancreata were procured from brain-dead organ donors by the JDRF Network for Pancreatic Organ Donors with Diabetes (nPOD) coordinated through the University of Florida in Gainesville, Florida (Table 1) (13). All procedures were in accordance with federal guidelines for organ donation and the University of Florida Institutional Review Board. Pancreata were procured from 20 individuals with DM. These were subdivided into 12 who did not receive GLP-1 drugs (DM) and 8 who received incretin therapy (DM-I) for 1 year or more, 7 being treated with the dipeptidyl peptidase-4 (DPP-4) inhibitor sitagliptin (Januvia) and 1 with the GLP-1 mimetic exenatide (Byetta). Pancreata were also obtained from 14 nondiabetic (ND) control subjects matched by age, sex, and BMI with the two DM treatment groups.
TABLE 1.
Clinical characteristics of brain-dead organ donors
Pancreas fixation, embedding, and sectioning.
nPOD uses a standardized preparation procedure for pancreata recovered from cadaveric organ donors (13). The pancreas is divided into three main regions (head, body, and tail), followed by serial transverse sections throughout the medial to lateral axis, allowing for sampling of the entire pancreas organ while maintaining anatomical orientation. Because preparation is completed within 2 h, tissue integrity is maintained. Tissues intended for paraffin blocks are trimmed to pieces no larger than 1.5 × 1.5 cm and fixed in 10% neutral buffered formalin for 24 ± 8 h. Fixation is terminated by transfer to 70% ethanol, and samples are subsequently processed and embedded in paraffin. Mounted transverse sections were obtained from the head, body, and tail of the paraffin-embedded tissue blocks.
Immunostaining
In Florida.
Formalin-fixed paraffin-embedded sections were stained according to established procedures, as previously described (14). In brief, serial sections (4 μm) were deparaffinized and incubated with primary antibodies to Ki67 and insulin, or CD3 and glucagon, with antibody localization visualized with peroxidase-DAB and alkaline phosphatase-Fast Red polymer systems. Assays included positive and negative controls for each antibody, and new lots of reagents were validated to reproduce previous staining intensities using normal human spleen for Ki67 and CD3 and pancreata from the ND donors for insulin and glucagon.
In Los Angeles.
Sequential paraffin tissue sections from each region of pancreas from each subject were stained for 1) Ki67, insulin, and Alcian blue by immunohistochemistry and 2) Ki67 and glucagon by immunohistochemistry. In addition, a section of pancreas from each of the DM-I subjects and a section from a subset of the DM subjects not treated with incretin therapy (n = 5) and ND subjects (n = 6) were stained for insulin and glucagon by immunofluorescence and additional sections for glucagon, insulin, cytokeratin, and DAPI.
Briefly, the cytokeratin, insulin, and glucagon slides were stained as follows: CK-19 (mouse 1:50, 4ºC overnight; Dako, Carpinteria, CA), glucagon (rabbit 1:1000, 4ºC overnight; ImmunoStar Inc, Hudson, WI), and insulin (guinea pig 1:100, 4ºC overnight; Invitrogen, Grand Isle, NY). FITC, Cy3, and Cy5 followed incubation of each primary antibody, respectively (1:100, The Jackson Laboratory–West, Sacramento, CA). Slides were coverslipped with Vectashield with DAPI (Vector Laboratories, Burlingame, CA).
Morphometric analysis
In Florida.
Stained slides were scanned to create whole digital slide images with an Aperio ScanScope CS (Aperio Technologies, Vista, CA) and Spectrum Plus version 11 at ×20 magnification. Each image was reviewed and annotated using the Aperio ImageScope image viewing program. Regions with edge artifact or nonspecific staining were excluded from analysis. The Spectrum colocalization algorithm was used to estimate the proportion of insulin- and glucagon-stained area compared with total tissue area defined by the hematoxylin counterstain. Software parameter settings were optimized for detection of both hematoxylin and Fast Red chromogen. Data were averaged within regions and then averaged among all regions for a given donor pancreas. Cytonuclear IHC quantification software (Indica Laboratories, Albuquerque, NM) was used to quantify total cell numbers per pancreas section and total cell replication rates using Ki67 nuclear immunopositivity. Input parameters were set using an ImageScope plug-in tool that calculates optical densities of the underlying structures in RGB OD values. Total cell counts were estimated from nuclei stained with hematoxylin. Nuclei costained with Ki67 were counted and expressed as a percentage of the total.
In Los Angeles.
Whole sections of pancreas stained for insulin, Ki-67, and Alcian Blue and hematoxylin counterstain were digitally scanned using Aperio ScanScope. Analysis was performed using Aperio ImageScope version 11.0.2.725. With this software, the total area of the tissue was measured.
Full cross-sections of the pancreas head, body, and tail were evaluated for pancreatic intraepithelial neoplasia (PanIN) by a gastrointestinal pathologist blinded to clinical information and using the established consensus classification system for these precursor lesions (15). The total number of PanIN lesions and their grade were determined per lobular unit and scored as the highest-grade lesion within that lobule. The number of PanINs per pancreas section was then computed per unit area of pancreas (mm2 × 103).
Using the insulin-, Ki-67–, and Alcian blue–stained sections, 100 islets were analyzed per section, with an Olympus CX41 microscope (Olympus America, Center Valley, PA), to determine the frequency of Ki67 in the β-cells of islets and in the non–β-cell compartment of those islets. Similarly, using the glucagon- and Ki-67–stained sections, 100 islets per section were analyzed to determine the frequency of Ki67 in the α-cells of islets and in the non–α-cell compartment of those islets. The mean β- and α-cell diameter was determined in each individual using the insulin and glucagon immunostained sections from the pancreas body, as previously described (16). A total of 475 α-cells and 475 β-cells were evaluated.
To determine the percentage of β- and α-cells within pancreatic ducts, the insulin-Ki67-Alcian blue–stained slides and the glucagon-Ki67-hematoxylin–stained slides were used. The total number of duct cells per pancreatic section was counted manually, as was the total number of cells within the ducts that stained for insulin or glucagon, respectively. The results are expressed as the percentage of duct cells positive for insulin or glucagon.
Using the sections stained by immunofluorescence for insulin, glucagon, and DAPI, a minimum of 30 islets per section (range 31–45, mean 38.0 ± 1.0) were randomly selected, imaged at ×20 magnification, and stored using a Leica DM6000 fluorescent microscope (Leica Microsystems, Deerfield, IL) connected to a Macintosh computer loaded with Openlab software (Improvision, Lexington, MA). Each islet was analyzed to determine the number of β-cells, α-cells, and cells costaining for insulin and glucagon.
Confocal microscopy was performed where cells costaining for insulin and glucagon were detected for confirmation that insulin and glucagon granules were indeed both present in the same cells. Imaging was performed using a scanning confocal microscope equipped with argon, green and red helium-neon lasers (Leica). Images were acquired by sequential scanning using a ×20 objective and the appropriate filter combination. Z sections were captured with a 0.25-μm step size.
Statistical analysis.
Statistical analysis was performed using the Student t test with GraphPad Prism 5.0 software (GraphPad Software, La Jolla, CA). Data in graphs and tables are presented as means ± SEM. Findings were assumed statistically significant at P < 0.05.
RESULTS
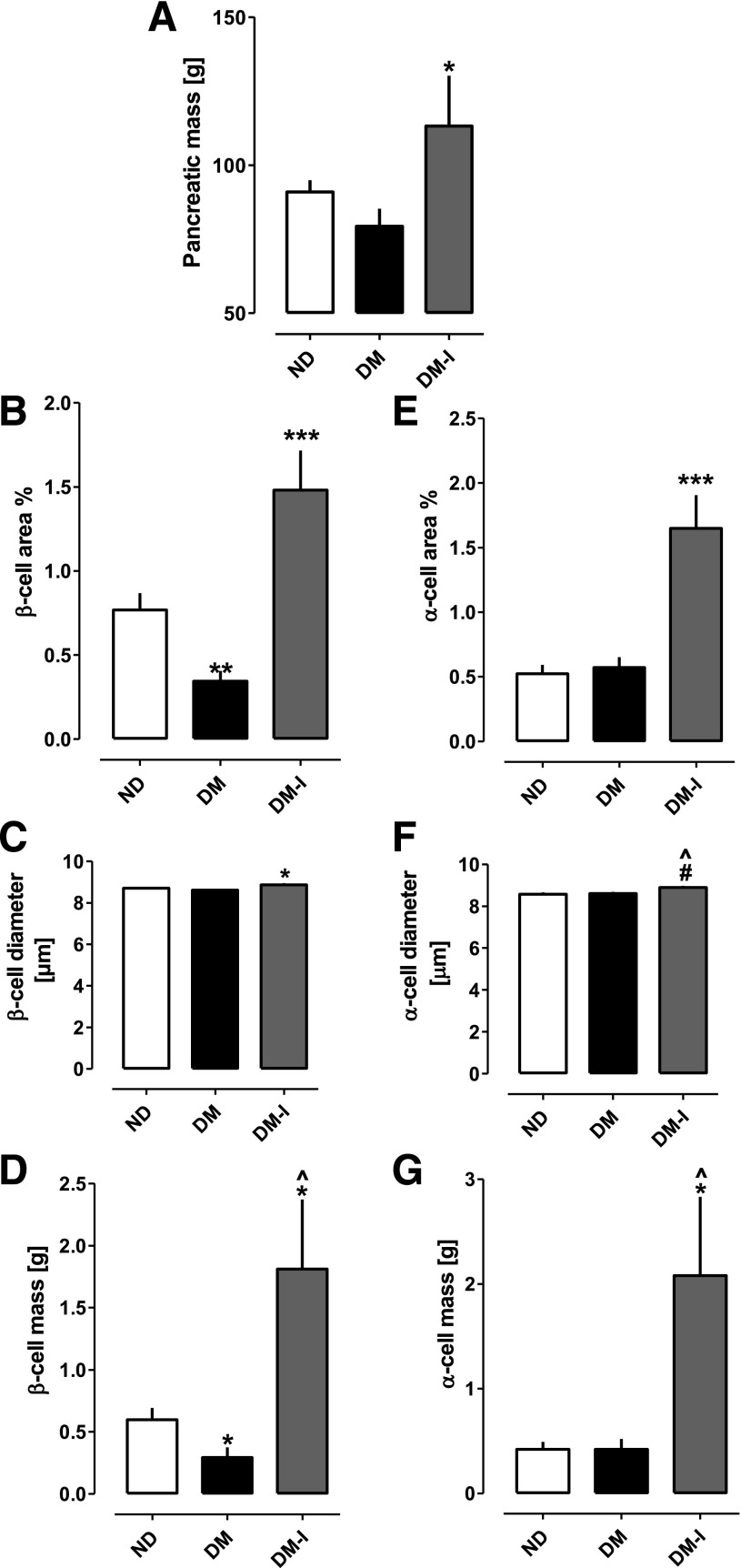
Pancreatic mass was increased (P < 0.05) ∼40% in DM-I patients compared with that in individuals with DM not treated with such agents (Fig. 1A). The pancreatic fractional insulin area was ∼60% reduced in DM patients not treated with incretin therapy compared with ND control subjects (0.34 ± 0.10 vs. 0.79 ± 0.10%; P < 0.001) (Fig. 1B). In contrast, the pancreatic fractional insulin area was approximately fivefold increased in DM-I patients compared with individuals not treated with incretin therapy (1.60 ± 0.41 vs. 0.34 ± 0.10%; P < 0.0001).
FIG. 1.
Pancreas, β-cell, and α-cell mass. A: Mean pancreatic weight. *P < 0.05 DM-I vs. DM. B: Pancreatic fractional insulin area. ***P < 0.0001 DM-I vs. DM, **P < 0.001 DM vs. ND. C: β-Cell diameter. *P < 0.05 DM-I vs. DM. D: β-Cell mass. ^P < 0.01 DM-I vs. DM, *P < 0.05 DM-I vs. ND, *P < 0.05 DM vs. ND. E: Pancreatic fractional glucagon area. ***P < 0.0001 DM-I vs. DM and ND. F: α-Cell diameter. ^P < 0.01 DM-I vs. DM, #P < 0.005 DM-I vs. ND. G: α-Cell mass. ^P < 0.01 DM-I vs. DM. *P < 0.05 DM-I vs. ND. Pancreatic weight was 40% increased in DM-I compared with DM (P < 0.05). β-Cell mass was decreased in DM compared with ND but was approximately sixfold increased in DM-I compared with DM. α-Cell mass was comparable in DM and ND but was approximately fivefold increased in DM-I compared with DM. The increase in β-cell and α-cell mass with incretin treatment was predominantly due to endocrine hyperplasia rather than hypertrophy.
The β-cell mass, computed from the product of the pancreatic fractional insulin-positive area and pancreatic mass, was 55% decreased in DM patients not on incretin therapy in comparison with ND control subjects (0.29 ± 0.08 vs. 0.60 ± 0.10 g; P < 0.05) (Fig. 1D). In contrast, β-cell mass was increased sixfold in DM-I patients (1.81 ± 0.56 vs. 0.29 ± 0.08 g; P < 0.01). Moreover, β-cell mass was threefold greater in DM-I individuals compared with ND control subjects (1.81 ± 0.56 vs. 0.60 ± 0.10 g; P < 0.05). The sixfold increase in β-cell mass in DM-I subjects was almost all due to increased β-cell numbers rather than β-cell size, although there was a 3% increase in β-cell size with incretin therapy (8.9 ± 0.1 vs. 8.6 ± 0.1 μm, DM vs. DM-I; P < 0.05) (Fig. 1C). The pancreatic fractional area immunostained for glucagon was comparable between DM individuals not subject to incretin therapy and ND control subjects (0.57 ± 0.12 vs. 0.52 ± 0.08%; P = NS) (Fig. 1E). However, the pancreatic fractional area immunostained for glucagon was markedly increased in DM-I individuals compared with DM patients on other therapy (1.65 ± 0.39 vs. 0.57 ± 0.12%; P < 0.0001) as well as compared with ND control subjects (1.65 ± 0.39 vs. 0.52 ± 0.08%; P < 0.0001). The pattern of the calculated glucagon mass followed that of the pancreatic fractional area, being comparable in individuals with DM not treated with incretin therapy and control subjects, but fivefold increased in DM-I individuals compared with DM patients not treated with incretin therapy (2.08 ± 0.75 vs. 0.45 ± 0.10 g, DM-I vs. DM; P < 0.01) (Fig. 1G). The marked increase in α-cell mass, like that of β-cell mass, was almost completely due to an increase in the number of α-cells, although again, there was a 4% increase in α-cell size (8.9 ± 0.1 vs. 8.6 ± 0.1 μm, DM-I vs. DM; P < 0.01) (Fig. 1F).
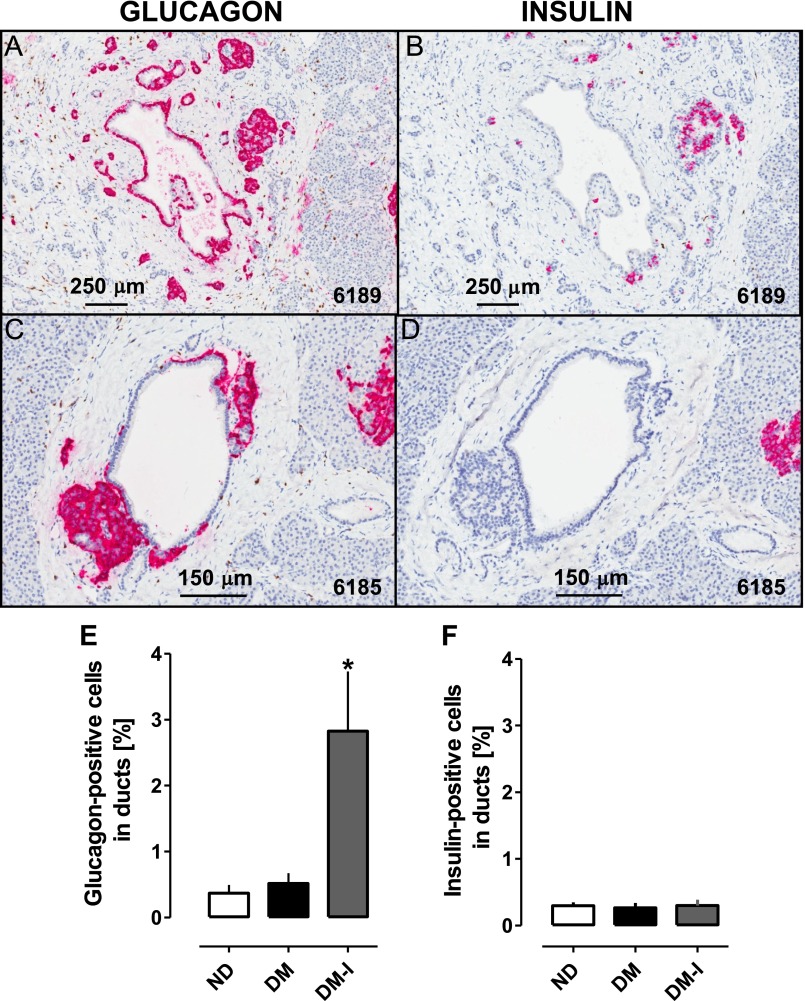
There were two immediately striking findings on inspection of the pancreatic sections of the DM-I subjects: a subset of enlarged and often eccentrically shaped islets as well as increased numbers of endocrine cells in association with duct structures (Figs. 2–4). The impression of a subset of enlarged islets was confirmed quantitatively, the 12 largest islets per section in the DM-I subjects being almost twice the cross-sectional area of those in the DM subjects not treated by incretins (82,270 ± 10,330 vs. 44,770 ± 6,986 μmol/L2; P < 0.01). While examples of insulin immunoreactive cells related to ductal structures could be found in individuals from all three groups, the percentage of such cells within ducts was not increased in DM-I versus DM subjects without incretin therapy (0.30 ± 0.09 vs. 0.27 ± 0.07%; P = NS) (Figs. 3 and 4). However, glucagon-immunoreactive cells were frequently found in long linear groups or solid nests of cells either within the duct itself or in the immediate periductal location. In addition, these glucagon-positive cells also formed intraductal luminal projections, as previously described in chronic pancreatitis (17) (Fig. 2A). There were also regions with multiple small ducts that had glucagon-expressing tubular- and islet-like structures directly contiguous to the ducts. Of note, there were cells expressing both cytokeratin and glucagon at the interface of these α-cell tubular projections from ducts (Fig. 2F–I). The percentage of cells immunoreactive for glucagon in ducts was increased in DM-I versus DM with no incretin therapy (2.8 ± 0.9 vs. 0.5 ± 0.2%; P < 0.05) (Fig. 3E). Thus, while the exuberant increase in glucagon immunoreactive cells with incretin treatment was frequently observed in the periductal areas, the increased numbers of insulin immunoreactive cells with incretin therapy tended to be most abundant more remote from these periductal endocrine complexes (Fig. 3B and D). The pancreas from the single individual treated with exenatide also revealed exuberant α-cell hyperplasia (Fig. 4).
FIG. 2.
Glucagon immunohistochemistry in pancreas in DM after incretin therapy. A–E: Sections of pancreas from DM-I donors (cases 6185, 6186, 6206, and 6203 with sitagliptin) immunostained for glucagon (pink) with hematoxylin counterstain. Exuberant expansion of glucagon immunoreactive cells is seen as enlarged eccentrically shaped islets as well as nodular and linear aggregates of cells intimately associated with ducts and demonstrating variable extension into duct lumens (arrow). C–E: Higher-power images show glucagon immunoreactivity in cells lining ducts. F–I: Pancreas sections from DM-I donors (case 6199, sitagliptin; 6189, exenatide) show immunofluorescent costaining for cytokeratin (green), glucagon (red), and DAPI nuclear counterstain (blue). Glucagon-expressing cells are present within and adjacent to keratin-positive duct structures. G: One cell costaining for cytokeratin and glucagon is indicated by the arrow.
FIG. 3.
Distribution of α-cells and β-cells in relation to ducts in DM-I donors. Serial adjacent sections of pancreas from DM-I donors (case 6189, exenatide; 6185, sitagliptin) were immunostained for glucagon (A and C) or insulin (B and D) with hematoxylin counterstain. These serial sections indicate that the exuberant endocrine growth associated with ducts is predominantly comprised of glucagon immunoreactive cells. The percentage of glucagon-positive cells in ducts (E) and insulin-positive cells in ducts (F) is shown. The percentage of glucagon-positive cells in ducts was increased in the DM-I group compared with the DM and ND groups (*P < 0.05). In contrast, the percentage of insulin-positive cells in ducts was unchanged in the DM-I group.
FIG. 4.
Evidence for a direct role of GLP-1 mimetic action in α-cell hyperplasia. Images of pancreatic sections (A–F) are provided to illustrate a similar pattern of α-cell hyperplasia in the donor treated with exenatide (6189) as in the sitagliptin-treated donors, implying a role for GLP-1 action independent of DPP-4 inhibition in α-cell hyperplasia. Enlarged and often eccentrically shaped islets are apparent, as well as increased numbers of glucagon immunoreactive cells associated with and surrounding ductal structures.
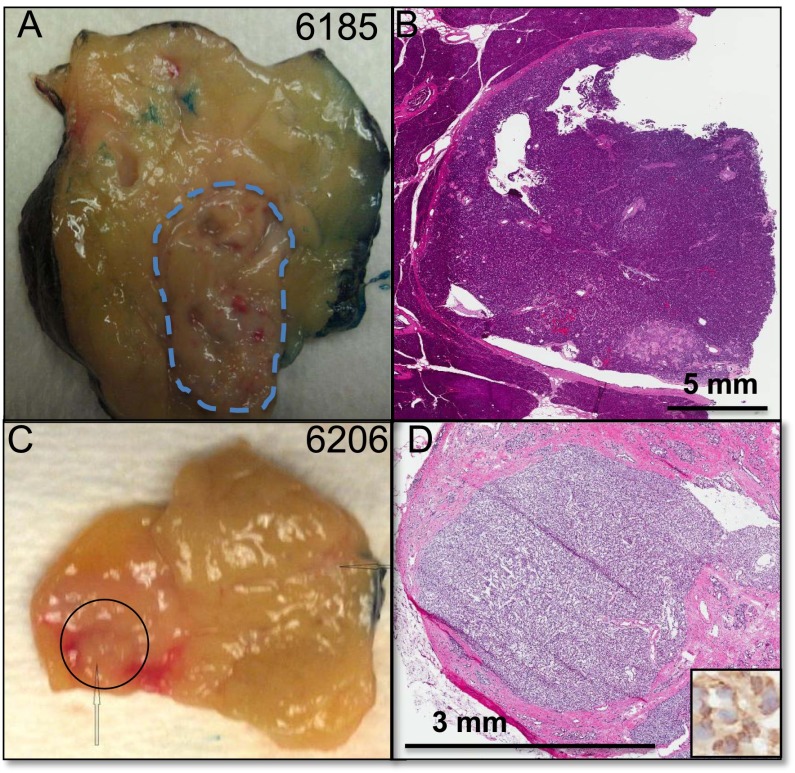
In one individual with DM treated with sitagliptin (nPOD case 6185), a 1.5-cm α-cell/glucagon-producing neuroendocrine tumor (grade 1, World Health Organization, 2010) not appreciated in life was identified in the body of the pancreas after resection at brain death (Fig. 5). Glucagon-producing microadenomas were also detected in the same individual (case 6185) and in two other DM-I individuals (cases 6157 and 6206) (Supplementary Fig. 3), whereas hyperplastic islets with predominant glucagon staining were noted in seven of eight of the DM-I individuals. No neuroendocrine tumors or glucagon-producing microadenomas were detected in ND control subjects or in DM subjects not treated with incretin therapy.
FIG. 5.
Pancreatic glucagon expressing neuroendocrine tumor and microadenoma. Grossly visible lesion (A) and corresponding section stained with hematoxylin and eosin (B) of the clinically undetected glucagon-expressing neuroendocrine tumor in the pancreas of a DM-I donor (nPOD case 6185) after sitagliptin therapy. Gross specimen (C) and corresponding hematoxylin and eosin–stained section (D) of a glucagon-expressing microadenoma in nPOD case 6206, DM after sitagliptin therapy. The inset shows high-power view of representative cells stained for glucagon by immunohistochemistry. (See Supplementary Fig. 3 for an additional image of microadenoma in case 6206.)
Inspection of pancreatic sections immunostained with either insulin or glucagon from the DM-I individuals gave the impression that numerous cells within these islets were immunoreactive for both hormones. When quantified in sections double-immunostained for glucagon and insulin by confocal microscopy for this purpose (Fig. 6, Supplementary Figs. 1 and 2), the percentage of insulin-positive cells in DM-I individuals that were also glucagon immunoreactive were indeed markedly increased when compared with those with DM not treated with incretin therapy (16.8 ± 5.0 vs. 3.2 ± 1.4%; P < 0.05). Interestingly, there was also an increase in double immunoreactive-positive cells in individuals with DM not treated with incretin therapy when compared with the ND control subjects (3.2 ± 1.4 vs. 0.4 ± 0.1%; P < 0.05). As in prior human studies (2), the frequency of Ki67-positive nuclei in islet endocrine cells was extremely rare (all less than 0.01 cells per islet section), with no significant differences in this very low frequency of β- or α-cell replication among any of the three groups studied.
FIG. 6.

Insulin and glucagon coexpression. Co-immunofluorescent images of islets from case 6185, sitagliptin (A–H) show endocrine cells coexpressing insulin (green) (A and E), glucagon (red) (B and F), and merged (D and H). The proportion of endocrine cells per islet that were thus detected as coexpressing insulin and glucagon was markedly increased in DM-I. Confocal images are shown of an islet from case 6185 stained for insulin (green) (I) and glucagon (red) (J), and a merged image (K) shows a mixture of cells, some expressing insulin or glucagon only (arrowheads) and some showing coexpression (arrows). DAPI nuclear counterstain (blue).
The increased pancreatic mass in DM induced by incretin therapy was accompanied by increased whole pancreas cell proliferation (0.25 ± 0.03 vs. 0.12 ± 0.01%, DM-I vs. DM; P < 0.0001) and an increase in the presence of PanINs (11.9 ± 2.6 vs. 4.9 ± 1.7, DM-I vs. DM, PanINs/mm2 × 103; P < 0.01) (Fig. 7). PanIN lesions were also not infrequently detected in or close to these areas with ductular α-cell complexes (Fig. 7). Inspection of pancreas sections in DM-I individuals revealed small foci of increased Ki67 immunostaining in and around ducts and sometimes in areas of exocrine dysplasia (Supplementary Fig. 4). Given the focal and often dysplastic nature of these areas of increased cell replication, it was not possible to attribute the increased replication to a particular tissue compartment of the pancreas (e.g., ducts, acinar cells).
FIG. 7.
Pancreatic intraepithelial neoplasia, endocrine complexes, and cellular replication. Photomicrographs show sections with immunohistochemical staining for Ki67 (brown) and glucagon (pink) in PanIN lesions (A and C) with hematoxylin counterstain or Ki67 (brown) and insulin (pink) (B and D) with Alcian blue counterstain to highlight mucin. Glucagon-expressing endocrine cells are shown intimately associated with PanIN lesions to varying degrees. Foci of replication (arrows, Ki67 nuclei) are also apparent. (See Supplementary Fig. 4 for additional examples of foci of increased replication in incretin treated pancreas.) E: Pancreas cell replication is increased in DM-I (Ki67). ***P < 0.0001 DM-I vs. DM and ND. F: Frequency of PanIN1 and 2 (lesions/mm2 ×103 of pancreas) is increased in DM-I. ^P < 0.01 DM-I vs. DM, ***P < 0.0001 DM-I vs. ND.
DISCUSSION
In this study, we took advantage of the unique resource of pancreata procured by the JDRF nPOD program (13) to re-evaluate the question of β-cell mass in DM and, in addition, to address the potential actions of the incretin drugs on the endocrine and exocrine compartments. In the individuals with DM not using incretin drugs, we report a 60% deficit in β-cell mass but unchanged α-cell mass. Perhaps not surprisingly, given methodological differences, previous reports suggest a wide range of change in β- and α-cell mass (or pancreatic fractional area) in DM (1–3,18–20).
A striking finding in the present studies is the marked expansion of the exocrine and endocrine compartments of the pancreas with incretin therapy. The DPP-4 inhibitor sitagliptin acts to increase endogenous GLP-1 levels (21). It is not known whether the actions of sitagliptin reported here were mediated by increased circulating GLP-1 levels, increased GLP-1 levels produced by the newly formed α-cells acting in a paracrine manner, or due to the actions of signaling peptides other than GLP-1 that are degraded by DPP-4. The one individual treated by exenatide available to us here showed a pattern of changes comparable to those observed in the sitagliptin-treated individuals (Fig. 4), implying that a direct action of GLP-1 is likely involved. However, to fully address this question, it will be important to obtain more pancreata from individuals who have been treated with GLP-1 mimetic therapy.
The pancreatic mass of the DM-I individuals was increased by 40% compared with patients with DM not treated with incretin therapy, consistent with prior rodent studies that revealed proliferative actions of GLP-1 on the exocrine pancreas now extended here to humans (5,12). Also of particular concern, incretin therapy was associated with an increase in pancreatic dysplastic PanIN lesions, consistent with the prior finding that GLP-1 receptors are expressed not only in the human exocrine pancreas but also in PanINs and that GLP-1 induces proliferative signaling in human pancreatic duct epithelial cells (12). Moreover, GLP-1 accelerated mPanIN formation in the KrasG12D mouse model (12). Of interest, PanINs and ductal endocrine complexes in DM-I donors were often seen in close proximity (Fig. 7), which could suggest a common underlying dysplastic process that perhaps adds insight into the admixture of endocrine cells often noted within pancreatic adenocarcinoma (22). The increased cellular proliferation observed in the whole pancreas sections of DM-I patients (Fig. 7E) could theoretically be due to a contribution of intrapancreatic GLP-1 released by newly formed α-cells. It is unlikely that brain-dead individuals in an intensive care unit setting for the week before organ procurement would be treated by incretin therapy. To more precisely elucidate the direct action of those therapies on proliferation in the human pancreas and to investigate the cellular subcompartments in which they induce this action, it will also be important to seek opportunities to obtain pancreata from individuals who had incretin therapy up until the pancreas was obtained, perhaps via surgery.
The marked α-cell hyperplasia, glucagon-expressing microadenomas, and glucagon-expressing neuroendocrine tumor noted in DM-I individuals are also of concern. These findings reproduce the α-cell hyperplasia, abnormal α-cell distribution, and predisposition to glucagon-expressing neuroendocrine tumors previously reported with suppressed glucagon secretion or signaling (23–25). It is of note that a consistent action of incretin therapy is to suppress glucagon secretion. As in prior reports of decreased glucagon secretion or action, the expansion in α-cell mass in DM-I subjects was prominently distributed as tubular outgrowths of glucagon-expressing cells from small duct-like structures within the lining of (or surrounding) larger ducts occasionally forming intraductal projections within the lumen. The latter possibly contribute to the reported increased incidence of pancreatitis in incretin-treated patients (11). Pancreatitis has previously been reported in humans with unexplained α-cell hyperplasia (26), and intraductal endocrine cell projections have been reported previously in chronic pancreatitis (17). Therefore, incretin therapy–induced intra- and periductal α-cell proliferations are now added to incretin therapy–induced expansion of PanIN lesions as plausible mechanistic links to the induction of pancreatitis through obstruction of the outflow of pancreatic enzymes.
The source of new α-cells in prior studies of impaired glucagon secretion or signaling was deemed most likely as arising from progenitor cells because no increase in α-cell replication was detected (23–25). We were also unable to detect any increase in α-cell replication in DM-I specimens to account for α-cell hyperplasia. Although again it should be noted that the study subjects were likely not exposed to incretin drugs immediately before pancreas procurement, a prior study suggests that sitagliptin therapy suppresses rather than enhances α-cell replication (27). Given that α-cells are epigenetically relatively unstable (28) and that most glucagonomas display malignant behavior, the present finding calls into question the safety of long-term suppression of glucagon secretion or action. Moreover, because the standard of care of a pancreatic neuroendocrine tumor is surgical resection, due to the risk of conversion to malignancy, even if benign, patients exposed to incretin therapy would seem to be at increased risk of requiring pancreatic surgery.
The present finding of an increased pancreatic mass, increased PanIN lesions, and endocrine proliferations encircling and sometimes encroaching on pancreatic ducts in response to GLP-1 mimetic therapy does add to concerns already raised regarding the potential adverse actions of GLP-1 mimetic therapy to induce pancreatitis and accelerate pancreatic dysplasia (11). Prior reports of potentially concerning pancreas changes with incretin therapy were confined to studies of rodent pancreas but are now here extended to humans with the added concern of the risk of neuroendocrine tumors. Because newly formed α-cells in response to impaired glucagon secretion have been shown to secrete high levels of GLP-1 (23–25), the local GLP-1 concentrations in the pancreas in patients treated with DPP-4 inhibitors may be very high, particularly where these cells are abundant in and around dysplastic ducts. This may account for the observed increase in pancreatitis and pancreatic tumors registered with the U.S. Food and Drug Administration’s adverse event reporting system for GLP-1 mimetics and DPP-4 inhibitors, in contrast to the signal for thyroid tumors being restricted to GLP-1 mimetics (11). It also may explain the expansion of the exocrine pancreas in glucagon receptor–null mice (and mutant human), exocrine proliferation being noted in both, as well as high GLP-1 release by newly formed α-cells (23–25).
At first sight, the increase in β-cell mass with incretin therapy in DM in ND subjects would appear to be an exciting finding in relation to the potential for disease reversal. Unfortunately, these insulin-expressing cells are presumably not functionally mature because the DM-I individuals still had DM. It will be important to establish the molecular signature of the insulin-expressing cells in future studies. The marked expansion of the β-cell mass in individuals with DM treated with sitagliptin or exenatide for a year or more is in contrast to the findings of the effects of these drugs on β-cell function in DM (29,30). Although β-cell function benefits to some extent in patients with DM with any therapy that lowers blood glucose values (31,32), no data to date suggest that there is a disease-modifying action of incretin therapy in DM over that of any other glucose-lowering agent with regard to recovery of β-cell function (29,30). It is plausible that GLP-1 directly induced proliferation of β-cells, as has been reported in animal studies (4,5). However, these studies were in juvenile rodents, and GLP-1 did not induce proliferation in human islets in vitro (10). Also, β-cell replication did not differ among the groups in this study. However, as stated previously, because incretin therapy was likely not administered during the last week of life in the present donors, it is not possible to exclude incretin-induced β-cell replication from this study. Likewise, it is conceivable that the increase in β-cell number in DM-I may be due in part to GLP-1–mediated inhibition of β-cell apoptosis.
Another striking finding in the islets of the DM-I individuals is a high proportion of cells that expressed both insulin and glucagon. This has been described in the newly forming endocrine pancreas at week 20 of gestation in humans (33) and thus might be an indication of newly formed immature endocrine cells from presumptive progenitors. Alternatively, lineage-tracing studies in diabetic mice have established that α-cells have the capacity to transdifferentiate toward a β-cell phenotype (34). A third possible source of these double hormone–expressing cells could be β-cells that have partially transdifferentiated toward an α-cell fate. The epigenetic basis of this interconversion has been established (35).
In summary, we confirm that in humans with DM, β-cell mass is deficient while α-cell mass is no different from that in ND individuals. We note that both the exocrine and endocrine pancreas are markedly enlarged in DM-I individuals, with increased exocrine cell proliferation. The α-cell hyperplasia and neuroendocrine tumor and microadenoma formation is consistent with chronic inhibition of glucagon secretion by GLP-1. These findings lend additional weight to concerns regarding the effects of long-term GLP-1–related therapy with respect to unintended proliferative actions on the exocrine pancreas and now also a possible increased risk of neuroendocrine tumors. In addition to the surveillance previously recommended for the potential association of GLP-1–based therapy and pancreatic cancer risk, the current data imply that surveillance for a possible increased risk of pancreatic neuroendocrine tumors is warranted. On the other hand, the finding that there is a capacity to form large numbers of insulin-expressing cells in adult humans offers an impetus to the hopes of the goal of inducing β-cell regeneration in either type 1 or 2 diabetes. It is clear that a priority will be to establish the pathway by which these cells are formed and how to favor an endocrine versus exocrine cell lineage and, within the latter, a β-cell lineage. Moreover, further investigation on how to foster the maturation of the newly formed β-cells to function is of vital therapeutic importance.
Supplementary Material
ACKNOWLEDGMENTS
This research was performed with the support of the nPOD, a collaborative type 1 diabetes research project sponsored by the JDRF. Organ procurement organizations partnering with nPOD to provide research resources are listed at www.jdrfnpod.org/our-partners.php.
The work was supported by National Institute of Diabetes and Digestive and Kidney Diseases grants DK-059579, DK-061539, and DK-077967; the Larry L. Hillblom Foundation; and the Peter and Valerie Kompaniez Foundation.
No potential conflicts of interest relevant to this article were reported.
A.E.B. and M.C.-T. independently evaluated the morphometric analysis of the pancreas. M.C.-T. and M.A. supervised procurement of the pancreata by the nPOD program and the immunostaining procedures in Florida and participated in interpretation of the data. P.C.B. and T.G. supervised the immunostaining procedures in Los Angeles and participated in interpretation of the data. D.W.D. performed pathologic evaluation of pancreas sections. A.E.B., M.A., and P.C.B. contributed to writing the manuscript and preparation of the figures. P.C.B. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors acknowledge Irina Kusmartseva (University of Florida) for the gross images, Rosibel Hernandez and Johanna Park (University of California, Los Angeles) for technical assistance, and Bonnie Lui (University of California, Los Angeles) for editorial assistance.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db12-1686/-/DC1.
See accompanying commentary, p. 2178.
REFERENCES
- 1.Klöppel G, Löhr M, Habich K, Oberholzer M, Heitz PU. Islet pathology and the pathogenesis of type 1 and type 2 diabetes mellitus revisited. Surv Synth Pathol Res 1985;4:110–125 [DOI] [PubMed] [Google Scholar]
- 2.Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 2003;52:102–110 [DOI] [PubMed] [Google Scholar]
- 3.Rahier J, Guiot Y, Goebbels RM, Sempoux C, Henquin JC. Pancreatic beta-cell mass in European subjects with type 2 diabetes. Diabetes Obes Metab 2008;10(Suppl. 4):32–42 [DOI] [PubMed] [Google Scholar]
- 4.Xu G, Stoffers DA, Habener JF, Bonner-Weir S. Exendin-4 stimulates both beta-cell replication and neogenesis, resulting in increased beta-cell mass and improved glucose tolerance in diabetic rats. Diabetes 1999;48:2270–2276 [DOI] [PubMed] [Google Scholar]
- 5.Matveyenko AV, Dry S, Cox HI, et al. Beneficial endocrine but adverse exocrine effects of sitagliptin in the human islet amyloid polypeptide transgenic rat model of type 2 diabetes: interactions with metformin. Diabetes 2009;58:1604–1615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zulewski H, Abraham EJ, Gerlach MJ, et al. Multipotential nestin-positive stem cells isolated from adult pancreatic islets differentiate ex vivo into pancreatic endocrine, exocrine, and hepatic phenotypes. Diabetes 2001;50:521–533 [DOI] [PubMed] [Google Scholar]
- 7.Tourrel C, Bailbé D, Meile MJ, Kergoat M, Portha B. Glucagon-like peptide-1 and exendin-4 stimulate beta-cell neogenesis in streptozotocin-treated newborn rats resulting in persistently improved glucose homeostasis at adult age. Diabetes 2001;50:1562–1570 [DOI] [PubMed] [Google Scholar]
- 8.Tschen SI, Dhawan S, Gurlo T, Bhushan A. Age-dependent decline in beta-cell proliferation restricts the capacity of beta-cell regeneration in mice. Diabetes 2009;58:1312–1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tschen SI, Georgia S, Dhawan S, Bhushan A. Skp2 is required for incretin hormone-mediated β-cell proliferation. Mol Endocrinol 2011;25:2134–2143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parnaud G, Bosco D, Berney T, et al. Proliferation of sorted human and rat beta cells. Diabetologia 2008;51:91–100 [DOI] [PubMed] [Google Scholar]
- 11.Elashoff M, Matveyenko AV, Gier B, Elashoff R, Butler PC. Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology 2011;141:150–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gier B, Matveyenko AV, Kirakossian D, Dawson D, Dry SM, Butler PC. Chronic GLP-1 receptor activation by exendin-4 induces expansion of pancreatic duct glands in rats and accelerates formation of dysplastic lesions and chronic pancreatitis in the Kras(G12D) mouse model. Diabetes 2012;61:1250–1262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell-Thompson M, Wasserfall C, Kaddis J, et al. Network for Pancreatic Organ Donors with Diabetes (nPOD): developing a tissue biobank for type 1 diabetes. Diabetes Metab Res Rev 2012;28:608–617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campbell-Thompson ML, Heiple T, Montgomery E, Zhang L, Schneider L. Staining protocols for human pancreatic islets. J Vis Exp 2012;(63):e4068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hruban RH, Takaori K, Klimstra DS, et al. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol 2004;28:977–987 [DOI] [PubMed] [Google Scholar]
- 16.Saisho Y, Manesso E, Butler AE, et al. Ongoing beta-cell turnover in adult nonhuman primates is not adaptively increased in streptozotocin-induced diabetes. Diabetes 2011;60:848–856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soltani SM, O’Brien TD, Loganathan G, et al. Severely fibrotic pancreases from young patients with chronic pancreatitis: evidence for a ductal origin of islet neogenesis. Acta Diabetol 2011 Jul 20 [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Henquin JC, Rahier J. Pancreatic alpha cell mass in European subjects with type 2 diabetes. Diabetologia 2011;54:1720–1725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoon KH, Ko SH, Cho JH, et al. Selective beta-cell loss and alpha-cell expansion in patients with type 2 diabetes mellitus in Korea. J Clin Endocrinol Metab 2003;88:2300–2308 [DOI] [PubMed] [Google Scholar]
- 20.Stefan Y, Orci L, Malaisse-Lagae F, Perrelet A, Patel Y, Unger RH. Quantitation of endocrine cell content in the pancreas of nondiabetic and diabetic humans. Diabetes 1982;31:694–700 [DOI] [PubMed] [Google Scholar]
- 21.Herman GA, Bergman A, Stevens C, et al. Effect of single oral doses of sitagliptin, a dipeptidyl peptidase-4 inhibitor, on incretin and plasma glucose levels after an oral glucose tolerance test in patients with type 2 diabetes. J Clin Endocrinol Metab 2006;91:4612–4619 [DOI] [PubMed] [Google Scholar]
- 22.Sakaki M, Sano T, Hirokawa M, Takahashi M, Kiyoku H. Immunohistochemical study of endocrine cells in ductal adenocarcinoma of the pancreas. Virchows Arch 2002;441:249–255 [DOI] [PubMed] [Google Scholar]
- 23.Gelling RW, Du XQ, Dichmann DS, et al. Lower blood glucose, hyperglucagonemia, and pancreatic alpha cell hyperplasia in glucagon receptor knockout mice. Proc Natl Acad Sci U S A 2003;100:1438–1443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu R, Dhall D, Nissen NN, Zhou C, Ren SG. Pancreatic neuroendocrine tumors in glucagon receptor-deficient mice. PLoS ONE 2011;6:e23397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou C, Dhall D, Nissen NN, Chen CR, Yu R. Homozygous P86S mutation of the human glucagon receptor is associated with hyperglucagonemia, alpha cell hyperplasia, and islet cell tumor. Pancreas 2009;38:941–946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Henopp T, Anlauf M, Schmitt A, et al. Glucagon cell adenomatosis: a newly recognized disease of the endocrine pancreas. J Clin Endocrinol Metab 2009;94:213–217 [DOI] [PubMed] [Google Scholar]
- 27.Takeda Y, Fujita Y, Honjo J, et al. Reduction of both beta cell death and alpha cell proliferation by dipeptidyl peptidase-4 inhibition in a streptozotocin-induced model of diabetes in mice. Diabetologia 2012;55:404–412 [DOI] [PubMed] [Google Scholar]
- 28.Bramswig NC, Everett LJ, Schug J, et al. Epigenomic plasticity enables human pancreatic α to β cell reprogramming. J Clin Invest 2013;123:1275–1284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams-Herman D, Johnson J, Teng R, et al. Efficacy and safety of sitagliptin and metformin as initial combination therapy and as monotherapy over 2 years in patients with type 2 diabetes. Diabetes Obes Metab 2010;12:442–451 [DOI] [PubMed] [Google Scholar]
- 30.Bunck MC, Cornér A, Eliasson B, et al. Effects of exenatide on measures of β-cell function after 3 years in metformin-treated patients with type 2 diabetes. Diabetes Care 2011;34:2041–2047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Retnakaran R, Zinman B. Short-term intensified insulin treatment in type 2 diabetes: long-term effects on β-cell function. Diabetes Obes Metab 2012;14(Suppl. 3):161–166 [DOI] [PubMed] [Google Scholar]
- 32.Xiang AH, Peters RK, Kjos SL, et al. Effect of pioglitazone on pancreatic beta-cell function and diabetes risk in Hispanic women with prior gestational diabetes. Diabetes 2006;55:517–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meier JJ, Köhler CU, Alkhatib B, et al. Beta-cell development and turnover during prenatal life in humans. Eur J Endocrinol 2010;162:559–568 [DOI] [PubMed] [Google Scholar]
- 34.Thorel F, Népote V, Avril I, et al. Conversion of adult pancreatic alpha-cells to beta-cells after extreme beta-cell loss. Nature 2010;464:1149–1154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dhawan S, Georgia S, Tschen SI, Fan G, Bhushan A. Pancreatic β cell identity is maintained by DNA methylation-mediated repression of Arx. Dev Cell 2011;20:419–429 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.