SUMMARY
What is known and Objective
Cancer chemotherapy-associated cognitive impairments (termed ‘chemo-fog’ or ‘chemo-brain’), particularly in memory, have been self-reported or identified in cancer survivors previously treated with chemotherapy. While a variety of deficits have been detected, a consistent theme is a detriment in visuospatial working memory. The parietal cortex, a major site of storage of such memory, is implicated in chemotherapy-induced damage. However, if the findings of two recent publications are combined, the (pre)frontal cortex might be an equally viable target. Two recent studies, one postulating a mechanism for ‘top-down control’ of working memory capacity and another visualizing chemotherapy-induced alterations in brain activation during working memory processing, are reviewed and integrated.
Comment
A computational model and the proposal that the prefrontal cortex plays a role in working memory via top-down control of parietal working memory capacity is consistent with a recent demonstration of decreased frontal hyperactivation following chemotherapy.
What is new and Conclusion
Chemotherapy-associated impairment of visuospatial working memory might include the (pre)frontal cortex In addition to the parietal cortex. This provides new opportunity for basic science and clinical investigation.
Keywords: Chemobrain, Chemofog, Control model, Frontal cortex, Working memory
WHAT IS KNOWN AND OBJECTIVE
A chemotherapy-associated cognitive impairment (1) has been reported since at least the early 1980s (2). Patient-volunteered and clinical identification of cognitive changes after high-dose adjuvant therapy for breast cancer prompted a systematic evaluation that resulted in the assessment that “… the risk of cognitive impairment is substantially increased for patients who receive high-dose chemotherapy when compared with patients in the control group and when compared with the patients in the standard-dose chemotherapy group” (3). The terms ‘chemo brain’ and ‘chemo fog’ were applied to the nonspecific, primarily memory-related, cognitive impairments (4); the term ‘chemotherapy-induced cognitive impairment’ was introduced to suggest a causal link; and the term ‘chemotherapy-associated cognitive impairment’ (CACI) takes a more middle position.
Although there are exceptions (e.g., see (5)), one of the most often identified cognitive domains reported to be impaired in CACI is memory (see review by Raffa et al. (4) and more recent studies (e.g., (6); (7-9)), including visuospatial working memory (vsWM) — the ability to retain and manipulate information during brief tasks. This type of memory is distinct from short-term memory, which is associated primarily with the hippocampus. In vsWM, there is co-activation of neural activity in the intraparietal sulcus (IPS) in the posterior parietal cortex and with the dorsolateral prefrontal cortex (dlPFC) (10-13). The extent of participation of the dlPFC to the storage, as opposed to some important, but separate, function of vsWM, such as enhancement of attention or filtering out distractions (14), has been a matter of some debate (15); (16); (17); (18). The generally prevailing current view is that the IPS is the main storage site of vsWM and that the dlPFC might provide neural ‘top-down control’ on the IPS (10, 19-21).
Edin et al. (22) have proposed that a major role of the dlPFC in vsWM is to boost the memory capacity of the IPS. They formulated this hypothesis in a computational model that incorporates both the IPS and dlPFC in vsWM storage. Using physiologically-realistic parameter values, the model suggests that the normal balance of excitatory and inhibitory neuronal activity within the IPS network (intrinsic input) limits vsWM capacity. However, the model predicts that at high cognitive loads excitatory activation of the IPS from the dlPFC (extrinsic input) counteracts capacity-limiting intrinsic inhibition. This results in functional boosting of IPS memory capacity, and hence of vsWM.
If the model is correct that extrinsic input from activation of the dlPFC enhances vsWM (22), then anything that significantly impairs dlPFC activation should impair IPS memory storage capacity and be manifested clinically as an impaired vsWM such as seen in CACI. A report that breast cancer chemotherapy negatively impacts frontal lobe activation has recently been published (23). The results of Edin et al. (22) and McDonald et al. (23) are here summarized and it is postulated that chemotherapeutic agents might transiently or permanently inhibit normal dlPFC top-down enhancement of memory storage capacity in the IPS and result in impaired vsWM.
COMMENT
Model of top(dlPFC)-down(IPS) control
The simulation model used by Edin et al. (22) was based on a cortical network model of synaptic connections and network dynamics underlying vsWM that was previously developed (24). The model included the dlPFc and the IPS. Within the IPS, a neural network was modeled as 1,024 excitatory and 256 inhibitory cells (‘E cells’ and ‘I cells’, respectively) and incorporated operational features such as neuronal synapses of excitatory and inhibitory neurotransmitters, including AMPA (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid), NMDA (N-methyl-D-aspartate), and GABA (γ-amino-butyric acid). Based on the findings from a multiple-electrode cross-correlation analysis of vsMN in monkey prefrontal cortex (25), adjacent and nearby cells were given a relatively stronger influence (interaction) and distant cells a relatively weaker influence. The corresponding relevant excitatory and inhibitory neurotransmitters were used: E cell → E cell (AMPA & NMDA); E cell → I cell (AMPA & NMDA); I cell → E cell (GABA); and I cell → I cell (GABA). Details are available (22, 24, 25). The model was adapted to vsWM and an equation was derived relating mneumonic firing rate, r, to vsWM load, Λ, which in condensed form is (22)
| (1) |
where f is the neuronal input-output function relating rates to synaptic input; G+ and G− are the connection strength between neurons coding for the same (stimulatory, G+) and different (inhibitory, G−) stimuli; and IX is external input. Note that as mneumonic load increases, inhibitory input (G−) to the network increases until at some load the capacity is exceeded — which is consistent with what is known about vsWM. From equation [1], it is possible to find a ‘capacity equation’ (22)
| (2) |
where H(IX) is the effective connection strength at capacity. It was straightforward then to derive an upper limit (UL) for capacity (cap) as (22)
| (3) |
where ω is the size of a neural population that codes for one item relative to the entire network. The model matches with experimentally measured capacity and suggests that inhibition can be a major mechanism limiting vsWM capacity of the IPS (to 2 – 7 items).
Chemotherapy-induced altered brain activation during vsWM
The early electrophysiological and neuroimaging studies related to CACI were previously reviewed (1). Two of the studies are especially relevant to the present topic. One study (26) found that 60 year-old monozygotic twin sisters with minimal differences in their standardized neuropsychological tests differed significantly with respect to cognitive complaints (chemotherapy-treated sister >> cancer-free sister). fMRI revealed much broader activation in WM circuitry in parietal and frontal regions of the chemotherapy-treated twin than in the cancer-free twin. In the other study (27), it was concluded that greater recruitment of frontal cortex is involved when chemotherapy-treated patients perform a functional memory task.
The recent publication of McDonald et al. (23) provides fMRI evidence of the alterations in brain region activation during WM processing. This was a prospective longitudinal study of women diagnosed with noninvasive (stage 0) or non-metastatic invasive breast cancer (stages I to IIIA) (mean ages 50.5 – 52.9 years) and healthy controls. The patients were divided into those, designated CTx+, that were treated with standard-dose chemotherapy regimens (doxorubicin/cyclophosphamide/paclitaxel, N = 11; docetaxel/doxorubicin/cyclophosphamide, N = 2; or doxorubicin/cyclophosphamide, N = 3) and those, designated CTx−, that did not receive chemotherapy. All participants underwent fMRI scanning during a WM task (see (23) for details) at baseline (after surgery, but prior to chemotherapy), 1 month after chemotherapy, and 1 year later (or at yoked intervals for CTx− and controls). At baseline, the patients had “… significantly increased frontal and parietal activation compared with controls”. A month after initiation of chemotherapy or anti-estrogen regimens, “hyperactivation” in frontal lobe regions decreased compared to controls. The activation returned to approximately baseline levels in some frontal lobe regions, but remained low in others. There were no significant between-group differences in psychosocial factors such as mood, anxiety, or fatigue.
WHAT IS NEW AND CONCLUSION
‘Chemotherapy-associated cognitive impairment’ describes a panorama of usually mild to moderate transient or persistent deficit in attention, concentration, language skill, or executive function (such as multitasking and ability to organize information) following treatment with chemotherapeutic agents (for overviews, see Raffa et al. (4) and Raffa & Tallarida (1)). Some of the earliest and most common descriptors included in lists of patient self-reports or provider/family observations are terms such as ‘visuo-spatial’ (e.g., (28, 29)), ‘visuo-motor’ (e.g., (30)), or ‘visual memory’ (e.g., (31)). Each of these contributes to impairments in visuospatial working memory. An effect on the visual system might also be involved ((1)). Other types of memory are also impacted, such as short-term memory; for example, 5-fluorouracil (5-FU) (32), methotrexate (33), and cyclophosphamide (34) have deleterious effects on hippocampal cells.
WM capacity, the maximum number of items that can be transiently stored in WM, is an important component in general cognitive abilities and the IPS is generally believed to be a major site of storage of vsWM in humans (19-21, 35-37). Edin et al. (22) have proposed a mechanistic model for top-down control by the dlPFC of vsWM capacity. Their model accurately accounts for known features and limitations in human vsWM. An intriguing finding is that excitatory inputs from the dlPFC onto IPS neuronal networks counteract capacity-limiting inhibitory interactions between stored memories within the IPS and allow higher vsWM capacity. fMRI data from the study support the idea that enhanced functional coupling between dlPFC and IPS during high vsWM load boosts performance.
So it seems that excitatory PFC input can boost IPS capacity, particularly when IPS capacity is stressed. It would seem, then, that if the reverse happened, that is, if a functional coupling between dlPFC and IPS was disrupted, there would be a relative decrease in vsWM capacity.
Direct evidence for this hypothesis appears to have been provided by the recent neuroimaging (fMRI) study published by McDonald et al. (23) as described above. In the study, chemotherapeutic regimens altered activation within typical WM circuitry and the authors suggested a “… greater vulnerability of frontal regions to treatment effects, particularly chemotherapy”. Of particular note were the findings that: the patients had abnormally high frontal lobe activation at baseline, frontal activation was reduced at one month (M1) after chemotherapy, and there was partial return to baseline at one year (Y1) after therapy:
The abnormally high baseline activation in frontal regions suggests that the patients were compensating for reduced parietal storage capacity with increased excitatory input from the frontal cortex. This is consistent with previous findings of a greater recruitment of frontal cortical tissue when chemotherapy-treated patients are asked to perform a memory task (27). In this situation, it appears that functional performance compensation mirrors dlPFC top-down compensation.
That frontal activation was decreased at M1, rather than the same or increased over baseline in an effort to compensate for the increased load, suggests that damage in this region contributes to CACI decrement in WM.
The partial return of activation to baseline at Y1 corresponds to the self-reports and clinical observations of partial recovery of functional vsWM with time.
Conclusion
A mechanism for dorsolateral prefrontal cortex (dlPFC) → intraparietal sulcus (IPS) top-down control of visuospatial working memory (vsWM) has been proposed by Edin et al. (22). According to the model, inhibitory influences on IPS vsWM capacity, particularly under high load conditions, is counteracted by excitatory input from the dlPFC. The present communication supposes that the opposite might also be true: interruption of the top-down control might contribute to vsWM deficits described in chemotherapy-associated cognitive impairment (CACI). This supposition is supported by a very recent publication by McDonald et al. (23), which found common chemotherapeutic treatment regimens decrease activation of frontal brain regions involved in the vsWM network circuitry. The seemingly reasonable conclusion is that at least some symptoms of CACI, particularly those involving vsWM, result from deleterious effects on frontal brain regions and resultant diminution of top-down dlPFC → IPS enhancement of vsWM capacity. This construct might provide additional insight into the neural substrates of CACI and suggest novel treatment strategies. Since the major neurotransmitters and receptors associated with this network are related to GABA and glutamate (NMDA, AMPA), there might be a possible role for GABAergic and/or glutamatergic agents for prophylaxis or management of CACI.
Fig 1.
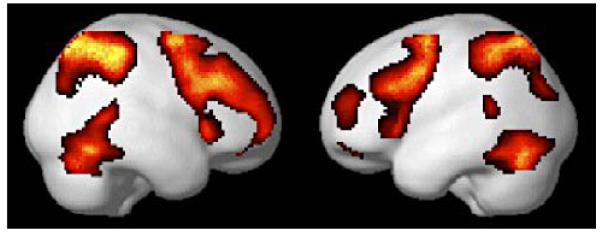
An example of activation of human fronto-parietal networks (visualized by fMRI scan) during working memory tasks. From Habel et al. (13) with permission.
ACKNOWLEDGEMENTS
The author thanks Michael Jacobs, Pharm.D. (Temple University School of Pharmacy) for bringing chemo-fog/brain to his attention. Partial salary recovery was provided by NIH CA129092.
Footnotes
CONFLICT OF INTEREST STATEMENT The author declares that there are no conflicts of interest.
REFERENCES
- 1.Raffa RB, Tallarida RJ. Chemo Fog: Cancer Chemotherapy-Related Cognitive Impairment. Vol. 678. New York, N.Y; Landes Bioscience / Springer: 2010. [PubMed] [Google Scholar]
- 2.Silberfarb PM, Philibert D, Levine PM. Psychosocial aspects of neoplastic disease: II. Affective and cognitive effects of chemotherapy in cancer patients. Am J Psychiatry. 1980;137:597–601. doi: 10.1176/ajp.137.5.597. [DOI] [PubMed] [Google Scholar]
- 3.Ganz PA. Cognitive dysfunction following adjuvant treatment of breast cancer: a new dose-limiting toxic effect? Journal of the National Cancer Institute. 1998;90:182–183. doi: 10.1093/jnci/90.3.182. [DOI] [PubMed] [Google Scholar]
- 4.Raffa RB, Duong PV, Finney J, et al. Is ‘chemo-fog’/‘chemo-brain’ caused by cancer chemotherapy? Journal of Clinival Pharmacy and Therapeutics. 2006;31:129–138. doi: 10.1111/j.1365-2710.2006.00726.x. [DOI] [PubMed] [Google Scholar]
- 5.O’Neil S, Ji L, Buranahirun C, et al. Neurocognitive outcomes in pediatric and adolescent patients with central nervous system germinoma treated with a strategy of chemotherapy followed by reduced-dose and volume irradiation. Pediatric Blood Cancer. 2011;57:669–673. doi: 10.1002/pbc.23146. [DOI] [PubMed] [Google Scholar]
- 6.Ashford J, Schoffstall C, Reddick WE, et al. Attention and working memory abilities in children treated for acute lymphoblastic leukemia. Cancer. 2010;116:4638–4645. doi: 10.1002/cncr.25343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mabbott DJ, Monsalves E, Spiegler BJ, et al. Longitudinal evaluation of neurocognitive function after treatment for central nervous system germ cell tumors in childhood. Cancer. 2011;117:5402–5411. doi: 10.1002/cncr.26127. [DOI] [PubMed] [Google Scholar]
- 8.Yamada TH, Denburg NL, Beglinger LJ, Schultz SK. Neuropsychological outcomes of older breast cancer survivors: cognitive features ten or more years after chemotherapy. Journal of Neuropsychiatry and Clinical Neuroscience. 2010;22:48–54. doi: 10.1176/appi.neuropsych.22.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robinson KE, Livesay KL, Campbell LK, et al. Working memory in survivors of childhood acute lymphocytic leukemia: functional neuroimaging analyses. Pediatric Blood Cancer. 2010;54:585–590. doi: 10.1002/pbc.22362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldman-Rakic PS. Cellular basis of working memory. Neuron. 1995;14:477–485. doi: 10.1016/0896-6273(95)90304-6. [DOI] [PubMed] [Google Scholar]
- 11.Gnadt JW, Andersen RA. Memory related motor planning activity in posterior parietal cortex of macaque. Experimental Brain Research. 1988;70:216–220. doi: 10.1007/BF00271862. [DOI] [PubMed] [Google Scholar]
- 12.Funahashi S, Bruce CJ, Goldman-Rakic PS. Mnemonic coding of visual space in the monkey’s dorsolateral prefrontal cortex. Journal of Neurophysiology. 1989;61:331–349. doi: 10.1152/jn.1989.61.2.331. [DOI] [PubMed] [Google Scholar]
- 13.Habel U, Koch K, Pauly K, et al. The influence of olfactory-induced negative emotion on verbal working memory: individual differences in neurobehavioral findings. Brain Research. 2007;1152:158–170. doi: 10.1016/j.brainres.2007.03.048. [DOI] [PubMed] [Google Scholar]
- 14.McNab F, Klingberg T. Prefrontal cortex and basal ganglia control access to working memory. Nature Neuroscience. 2008;11:103–107. doi: 10.1038/nn2024. [DOI] [PubMed] [Google Scholar]
- 15.Benchenane K, Tiesinga PH, Battaglia FP. Oscillations in the prefrontal cortex: a gateway to memory and attention. Current Opinion in Neurobiology. 2011;21:475–485. doi: 10.1016/j.conb.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Grossberg S. Towards a unified theory of neocortex: laminar cortical circuits for vision and cognition. Progress in Brain Research. 2007;165:79–104. doi: 10.1016/S0079-6123(06)65006-1. [DOI] [PubMed] [Google Scholar]
- 17.Matzel LD, Kolata S. Selective attention, working memory, and animal intelligence. Neuroscience and Biobehavioral Reviews. 2010;34:23–30. doi: 10.1016/j.neubiorev.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruchkin DS, Grafman J, Cameron K, Berndt RS. Working memory retention systems: a state of activated long-term memory. Behavioral Brain Science. 2003;26:709–728. doi: 10.1017/s0140525x03000165. discussion 728-777. [DOI] [PubMed] [Google Scholar]
- 19.Curtis CE, D’Esposito M. Persistent activity in the prefrontal cortex during working memory. Trends in Cognitive Science. 2003;7:415–423. doi: 10.1016/s1364-6613(03)00197-9. [DOI] [PubMed] [Google Scholar]
- 20.Linden DE. The working memory networks of the human brain. Neuroscientist. 2007;13:257–267. doi: 10.1177/1073858406298480. [DOI] [PubMed] [Google Scholar]
- 21.Linden DE, Bittner RA, Muckli L, et al. Cortical capacity constraints for visual working memory: dissociation of fMRI load effects in a fronto-parietal network. Neuroimage. 2003;20:1518–1530. doi: 10.1016/j.neuroimage.2003.07.021. [DOI] [PubMed] [Google Scholar]
- 22.Edin F, Klingberg T, Johansson P, McNab F, Tegner J, Compte A. Mechanism for top-down control of working memory capacity. Procedings of the National Academy of Sciences USA. 2009;106:6802–6807. doi: 10.1073/pnas.0901894106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McDonald BC, Conroy SK, Ahles TA, West JD, Saykin AJ. Alterations in brain activation during working memory processing associated with breast cancer and treatment: a prospective functional magnetic resonance imaging study. Journal of Clinical Oncology. 2012;30:2500–2508. doi: 10.1200/JCO.2011.38.5674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Compte A, Brunel N, Goldman-Rakic PS, Wang XJ. Synaptic mechanisms and network dynamics underlying spatial working memory in a cortical network model. Cerebral Cortex. 2000;10:910–923. doi: 10.1093/cercor/10.9.910. [DOI] [PubMed] [Google Scholar]
- 25.Constantinidis C, Franowicz MN, Goldman-Rakic PS. Coding specificity in cortical microcircuits: a multiple-electrode analysis of primate prefrontal cortex. Journal of Neuroscience. 2001;21:3646–3655. doi: 10.1523/JNEUROSCI.21-10-03646.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferguson RJ, McDonald BC, Saykin AJ, Ahles TA. Brain structure and function differences in monozygotic twins: possible effects of breast cancer chemotherapy. Journal of Clinical Oncology. 2007;25:3866–3870. doi: 10.1200/JCO.2007.10.8639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silverman DH, Dy CJ, Castellon SA, et al. Altered frontocortical, cerebellar, and basal ganglia activity in adjuvant-treated breast cancer survivors 5-10 years after chemotherapy. Breast Cancer Research and Treatment. 2007;103:303–311. doi: 10.1007/s10549-006-9380-z. [DOI] [PubMed] [Google Scholar]
- 28.Brezden CB, Phillips KA, Abdolell M, Bunston T, Tannock IF. Cognitive function in breast cancer patients receiving adjuvant chemotherapy. Journal of Clinical Oncology. 2000;18:2695–2701. doi: 10.1200/JCO.2000.18.14.2695. [DOI] [PubMed] [Google Scholar]
- 29.Wieneke MH, Dienst ER. Neuropsychological assessment of cognitive functioning following chemotherapy for breast cancer. Psycho-Oncology. 1995;4:61–66. [Google Scholar]
- 30.Schagen SB, van Dam FS, Muller MJ, Boogerd W, Lindeboom J, Bruning PF. Cognitive deficits after postoperative adjuvant chemotherapy for breast carcinoma. Cancer. 1999;85:640–650. doi: 10.1002/(sici)1097-0142(19990201)85:3<640::aid-cncr14>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 31.van Dam FS, Schagen SB, Muller MJ, et al. Impairment of cognitive function in women receiving adjuvant treatment for high-risk breast cancer: high-dose versus standard-dose chemotherapy. Journal of the National Cancer Institute. 1998;90:210–218. doi: 10.1093/jnci/90.3.210. [DOI] [PubMed] [Google Scholar]
- 32.Mustafa S, Walker A, Bennett G, Wigmore PM. 5-Fluorouracil chemotherapy affects spatial working memory and newborn neurons in the adult rat hippocampus. European Journal of Neuroscience. 2008;28:323–330. doi: 10.1111/j.1460-9568.2008.06325.x. [DOI] [PubMed] [Google Scholar]
- 33.Lyons L, ElBeltagy M, Umka J, et al. Fluoxetine reverses the memory impairment and reduction in proliferation and survival of hippocampal cells caused by methotrexate chemotherapy. Psychopharmacology (Berlin) 2011;215:105–115. doi: 10.1007/s00213-010-2122-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lyons L, Elbeltagy M, Bennett G, Wigmore P. The effects of cyclophosphamide on hippocampal cell proliferation and spatial working memory in rat. PLoS One. 2011;6:e21445. doi: 10.1371/journal.pone.0021445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Todd JJ, Marois R. Capacity limit of visual short-term memory in human posterior parietal cortex. Nature. 2004;428:751–754. doi: 10.1038/nature02466. [DOI] [PubMed] [Google Scholar]
- 36.Vogel EK, Machizawa MG. Neural activity predicts individual differences in visual working memory capacity. Nature. 2004;428:748–751. doi: 10.1038/nature02447. [DOI] [PubMed] [Google Scholar]
- 37.Xu Y, Chun MM. Dissociable neural mechanisms supporting visual short-term memory for objects. Nature. 2006;440:91–95. doi: 10.1038/nature04262. [DOI] [PubMed] [Google Scholar]


