Abstract
Although several evidence-based guidelines for managing diabetes are available, few, if any, focus on the psychosocial aspects of this challenging condition. It is increasingly evident that psychosocial treatment is integral to a holistic approach of managing diabetes; it forms the key to realizing appropriate biomedical outcomes. Dearth of attention is as much due to lack of awareness as due to lack of guidelines. This lacuna results in diversity among the standards of clinical practice, which, in India, is also due to the size and complexity of psychosocial care itself. This article aims to highlight evidence- and experience-based Indian guidelines for the psychosocial management of diabetes. A systemic literature was conducted for peer-reviewed studies and publications covering psychosocial aspects in diabetes. Recommendations are classified into three domains: General, psychological and social, and graded by the weight they should have in clinical practice and by the degree of support from the literature. Ninety-four recommendations of varying strength are made to help professionals identify the psychosocial interventions needed to support patients and their families and explore their role in devising support strategies. They also aid in developing core skills needed for effective diabetes management. These recommendations provide practical guidelines to fulfill unmet needs in diabetes management, and help achieve a qualitative improvement in the way physicians manage patients. The guidelines, while maintaining an India-specific character, have global relevance, which is bound to grow as the diabetes pandemic throws up new challenges.
Keywords: Diabetes, India, management, psychosocial, recommendations
INTRODUCTION
As India moves from a high prevalence of acute to chronic disease, type 2 diabetes mellitus (T2DM) is becoming a major health concern. Diabetes has been known in India since ancient times and finds mention in the well-referenced samhita texts, Charaka Samhita and Susruta Samhita. Together with Atharva Veda, they are among the oldest texts to describe and classify diabetes.[1] The Susruta Samhita treats diabetes in great detail and lists numerous symptoms that are included in the classical symptomology of diabetes, viz. excess urination, “sweet” urine, weight loss, impotence, and ulcers. Even the differences between hereditary, early-manifesting “thin” diabetes and later-onset, food-related “fat” diabetes was identified, which evidently correspond to modern types 1 and 2. Both Charaka Samhita and Susruta Samhita recognize unbalanced nutrition and lack of sufficient physical activity as probable causes of diabetes, and recommend dietary control and regular exercise for managing diabetes (in addition to treatment options from the ayurvedic pharmacopeia).[1]
Since the introduction of insulin for management of diabetes in 1922 by Dr. Frederick Banting, several important breakthroughs have been seen in diabetes management strategies.[2] (Nonetheless, successful diabetes management has remained elusive even with a wide variety of therapeutic options now accessible to clinical practitioners.[3]) Certainly, a purely pharmacological approach to successfully contain and, perhaps, even reverse the effects of diabetes, is insufficient; factors beyond the pale of pharmacological interventions, which dwell upon the holistic approach of supporting the patient psychologically, socially, and emotionally through the treatment process must be given due consideration.
The importance of emotional issues in diabetes was first noted over 300 years ago in 1674 by Thomas Willis, who claimed that diabetes was caused by “extreme sorrow.”[4] It has been emphasized that there is more to diabetes than just glucose control, and emotions play an important role in diabetes.[5] The emotional and psychological needs of people living with diabetes are complex. Indian diabetes patients have one of the lowest levels of psychological well-being on the World Health Organization-5 (WHO-5) Well-being Index, which is similar to the global trends. Indian patients also showed a significantly higher perception of burden of social and personal distress associated with diabetes.[3] These not only impact the patients’ ability to adhere to therapy but also their psychosocial well-being.
Acknowledging that psychosocial factors play an important role in diabetes therapy, several national and international stakeholders have included guidelines seeking to incorporate psychosocial management of diabetes as a part of standard clinical practice. The American Association of Clinical Endocrinologists (AACE) not only makes specific mention of psychosocial impact in evaluating therapeutic options but also gives independent recommendations for the treatment of comorbidities like depression, inclusion of team care and counseling. The AACE recommends using cultural and faith-based aspects of therapy during counseling.[6] The Scottish Intercollegiate Guidelines Network (SIGN)[7] for the management of diabetes also introduced psychosocial management in 2010. Similar trends are seen in many national guidelines in Europe and in the American Diabetes Association (ADA).[3,8]
Similarly, the global guideline for type 2 diabetes by the International Diabetes Federation (IDF) devotes an entire chapter to recommend standards of minimal, routine and comprehensive care for psychological management. The IDF clinical guidelines task force states in its rationale that “psychosocial factors are relevant to nearly all aspects of diabetes management.” In its recommendations for psychosocial care, the IDF recommends the inclusion of a mental health specialist in the multidisciplinary team for diabetes and indicates the need for counseling the person with diabetes in the context of on-going diabetes education and care. Particularly important is the recognition that signs of cognitive, emotional, behavioral and social problems, which may be complicating self-care, be considered a part of minimal care required for diabetes patients.[9] The International Society for Paediatric and Adolescent Diabetes (ISPAD) guideline also devotes a chapter on psychological care of children and adolescents with diabetes. The ISPAD Consensus Guidelines 2000 stated that “psychosocial factors are the most important influences affecting the care and management of diabetes,” and went on to make the following three general recommendations:[10]
Social workers and psychologists should be part of the interdisciplinary health care team.
Overt psychological problems in young persons or family members should receive support from the diabetes care team and expert attention from mental health professionals.
The diabetes care team should receive training in the recognition, identification and provision of information and counseling on psychosocial problems related to diabetes.
Despite the availability of international guidelines and multiple treatment options globally, the management of diabetes in clinical practice remains sub-par.[11] The available guidelines in most cases do not have cross-cultural applications and contribute little to the local understanding of diabetes. In the Indian context, less than one-third of the doctors reported using clinical guidelines in their practice. The biggest hindrances to the use of these guidelines locally are poor knowledge and the non-applicability of western guidelines in the Indian context.[12] The linguistic, social, cultural, economic, and ethnic heterogeneity of the Indian population and the enormous scale of the diabetes epidemic in India suggest the development of India-specific guidelines for psychosocial management, forged specifically for our sociocultural context. Both in terms of variety and in terms of the scale of challenges, the Indian diabetes landscape is unique and warrants the creation of country-specific guidelines, sensitive to our needs and limitations and based on our sociocultural strengths and resources.
PSYCHOSOCIAL FACTORS INFLUENCING DIABETES MANAGEMENT IN INDIA
Psychosocial factors are important modulators of the success of treatment and long-term prognosis of diabetes. At the same time, optimal diabetes management is associated with considerable physical, social, and psychological well-being. As the diabetes patient is at the core of executing the care process in diabetes, the outcomes of the care process and its effect on long-term prognosis depend on the social, cultural, familial and professional context that informs the patients’ psychosocial condition.[13] There is growing awareness of the importance of these factors both among providers and among patients. At the first Oxford International Diabetes Summit (2002), virtually all (98%) the participants representing medicine, politics, nursing and patient groups called for psychosocial aspects of diabetes to be included in national guidelines.[14]
Nonetheless, the number of patients receiving psychosocial care as a part of their therapy is not commensurate with its impact. It has been shown that as many as 41% of the patients had poor psychological well-being. These psychological problems were recognized by providers as affecting patients’ diabetes self-care. However, despite this, only about 10% of these patients received psychological care.[14] Additionally, there is a paucity of accurate, usable data to understand the exact impact of psychosocial factors on care, as studies investigating the relationships among psychological and social variables and diabetes outcomes are generally cross-sectional in nature, rather than longitudinal, and often fail to report pre-diagnosis baseline data.[13] In India, many of the psychosocial problems differ considerably from those encountered in the western society.[15] Some of the prominent factors that impact diabetes management, in the Indian context, by modifying acceptance of modern health care, include economic and cultural factors and traditional medicine, which are discussed below.[16]
Economic factors
In India, with about 25% of the population living under poverty and 41.6% of the population living under 1.25$ a day, cost of a therapeutic option/economic burden diabetes has a major impact on diabetes care. The direct medical cost to identify one subject with glucose intolerance is INR 5278.[17] The cost of insulin amounts to 350.00 USD (16,000 Indian Rupees) per year, while medication for non-insulin-requiring patients costs about 70.00 USD per year.[18] Out-of-pocket payments for hospital treatment for diabetes claim 17% of the annual household expenditure in poor households, a majority of whom finance the expense through borrowing.[19] Poor households can spend up to 25% of their annual household income on diabetes care.[9]
Cultural and religious factors
Health behaviors are guided by continuous interactions of intrapersonal factors with the cultural environment.[20] Endemic cultural practices and attitudes that hamper appropriate health-related behavior make diabetes management in India challenging. The low rate of literacy contributes to poor diabetes care. Lower levels of literacy in the country are associated with lower awareness of diabetes and its complications,[21] and are reported to be significantly associated with higher glycated hemoglobin (HbA1c) levels.[22] It has also been suggested that specific myths about diabetes management can modulate the success of diabetes management.[9] Another example where cultural practices impact diabetes management is the relative difference in diabetes control of both genders. It has been reported that there is significantly lesser awareness of diabetes and poorer rates of compliance to therapy among housewives. Unfortunately, in one study it was reported that all the patients who were non-complaint due to financial constraints were women. This is despite the fact that women are known to have a higher rate of prevalence compared with men.[23]
Traditional and alternative medicine
India has a wide range of alternative healthcare systems, which are patronized by the general population. A considerable number of patients (14%) still utilize the indigenous forms of medicine and one-third prefers non-allopathic medical systems for treatment. The reasons given for preferring traditional medicines were safety (31%), cost (30%), effectiveness (25%) and availability (11%).[24] Furthermore, contribution of ancient Indian medicine to patient-centered care (PCC), as evidence by the Quadruple of Atreya, has been highlighted earlier.[25] However, critics often point to the lack of acceptance of PCC in traditional, oriented culture, which follows a system of eminence and age-based hierarchy. On the other hand, there have been calls for testing the safety of traditional therapies,[26] in light of questions on their safety, due to incidents of death as a result of administration of folk remedies for diabetes.[27]
Given the scale of challenges that are bound to present themselves as the Indian diabetes management scenario evolves, it behooves a country taking India's growth trajectory to gear up to face these challenges head-on. As noted earlier, the western guidelines have limited applicability in everyday clinical practice in India, but might serve as valuable guides to help frame our own national guidelines. India has a linguistically, culturally, religion-wise and socioeconomically heterogeneous population. Furthermore, it is a developing country and the limited resources severely restrict the availability of resources for diabetes care.[9] At the same time, its strong sociocultural ethos can be utilized to manage diabetes more efficiently at the individual, family, and community level. Given these challenges and strengths, our objective is to frame a clinical practice guideline (CPG) for the psychosocial management of diabetes, sensitive to and appropriate for, the Indian context. We hope that these guidelines will find acceptance across the world.
METHODOLOGY
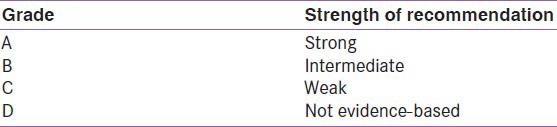
The recommendations have been developed in response to the need for national guidelines for psychosocial management of diabetes in India. The target is all diabetes care professionals in India. The current recommendation has been developed in accordance to the AACE protocol for CPG production [Table 1].[6] Recommendations are assigned evidence level (EL) ratings on the basis of the quality of supporting evidence, all of which have also been rated for strength [Table 2]. A thorough search of the literature pertaining to each of the classes of recommendations is presented, which are pertinent to the Indian clinical context of diabetes. A total of 94 recommendations are made. The guidelines have been written by a core group of 11 authors and reviewed by a committee of six multidisciplinary experts from India. It has been refereed by a South Asian panel of 10 reviewers.
Table 1.
Evidence rating according to American association of clinical endocrinologists protocol 2010[6]
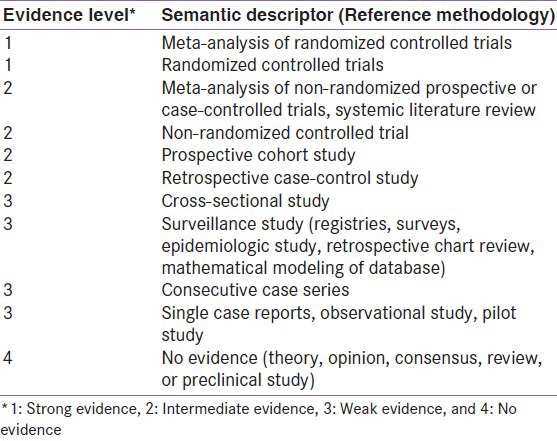
Table 2.
Recommendation grading according to the American association of clinical endocrinologists protocol 2010[6]
The recommendations incorporate the subjectivity of a complex clinical scenario with the objectivity of evidence-based medicine. As individual patient circumstances and psychosocial environments differ, the ultimate clinical management should be based on what is in the best interest of the individual patient and what is appropriate for the local scenario, involving shared decision making by patient and clinician.
RECOMMENDATIONS ON PSYCHOSOCIAL ASSESSMENT AND MANAGEMENT
While the current guidelines are intended as a comprehensive picture of psychosocial management in clinical practice, to make their application and utility more topical, they have been grouped based on their utility in different clinical contexts. This arrangement lends itself to contextualizing the recommendations in a given clinical scenario more accurately, while still remaining a part of the larger picture, to present a flavor of the guiding principles of psychosocial management. Current recommendations have been broadly presented in three clinical domains [Table 3]:
Table 3.
Recommendations for psychosocial management of diabetes in India
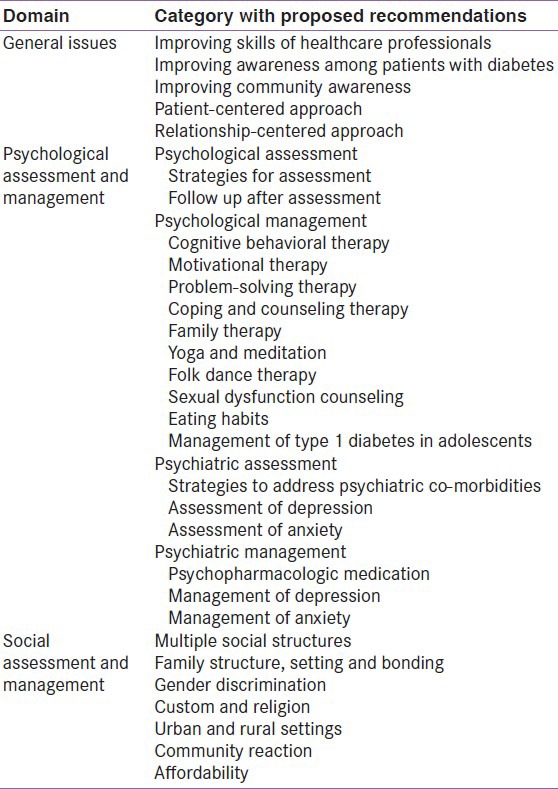
General issues
Psychological assessment and management
Social assessment and management.
GENERAL ISSUES
Improving awareness/skills of healthcare professionals
Recommendation 1: Healthcare professionals should receive at least informal and, preferably, formal training in psychological interventions involving coping and counseling for improved patient satisfaction and therapeutic outcomes[28] (Grade A; EL 1).
Recommendation 2: Healthcare professionals must be made aware of the bio-psychosocial model of managing diabetes and obtain basic grounding in psychosocial aspects of diabetes[15] (Grade A; EL 3).
-
Recommendation 3: Ability of health professionals to counsel patients with diabetes must be enhanced by receiving training in specific courses associated with teaching and counseling techniques, such as “Effective Patient Teaching and Problem Solving”[29] SWOT analysis[30] and CARES[31] (Grade A; EL 3).
- SWOT analysis[32,33,34]: SWOT (strength, weaknesses, opportunities, threats) analysis is an effective tool for personal growth and development. This tool aids doctors in evaluating patient's current strengths and weaknesses and decide the best strategy which can be utilized for patient's development as it will provide information about future threats which can be taken care off with insight into available opportunities for a win–win situation for both doctor and patient.
Recommendation 4: Healthcare professionals should adopt approaches like WATER that involve patients actively, ensure provider-patient bonding and improve therapeutic outcomes[31] (Grade A; EL 4).
Improving awareness among patients
Recommendation 5: In patients with low health literacy and numeracy, diabetes education may be facilitated using interactive modules such as diabetes literacy and numeracy education toolkit[35] (Grade A; EL 1).
-
Recommendation 6: Self-awareness tools such as “Johari Window” is recommended in patients with diabetes to enhance his/her knowledge about oneself that aid in better handling of one's emotional and personal issues, which will further boost one's self-esteem[36] (Grade A; EL 4).
- Johari window[36,37]: Johari window model developed by Joseph Luft and Harry Ingham is an effective tool for self-awareness to handle one's emotions and personal issues. This tool helps in enhancing patient's knowledge about oneself and thus exploring facts about who he/she is as an individual by following 360° feedback approach and sharing information with others. The expansion of open arena by the patient will make him/her confident and comfortable which will further boost one's self esteem.
Recommendation 7: There is a need to create interactive modules for India, where most patients present with low health literacy/numeracy (Grade A; EL 4).
Improving community awareness
Patient-centered approach
PCC is now an accepted part of medical practice today. Initially proposed in psychology as client-centered care, this term was popularized by bodies such as the Picker Institute and Institute of Medicine, through popular publications.[40,41] Recent guidelines on the management of diabetes have further reinforced the need for patient-centeredness, using the term “patient-centered approach” in their nomenclature,[42] which is defined as an approach to “providing care that is respectful of and responsive to individual patient preferences, needs and values and ensuring that patient values guide all clinical decisions.”[43] This approach customizes seeking and accepting the patient's ideas, seeking and giving recognition and encouragement, treatment recognition and decision making in response to the individual patient's perspective. Patient-centered approach has a beneficial impact on improving the health status of type 2 diabetes in terms of biological (glycemic control) and behavioral indicators (eating and exercise, compliance, symptoms of diabetes).[44] Experts also accept the need for, and importance of, therapeutic patient education through patient-centered approach in diabetes management.[45]
Recommendation 10: Patients should be encouraged to participate in patient empowerment programs that result in improved psychosocial self-efficacy and attitudes[46] (Grade A; EL 1).
Recommendation 11: Physicians are recommended to practice patient-centered professionalism, which encompasses competence, accessibility, respect, empathy, and honesty, best described by CARES[47] (Grade A; EL 4).
Recommendation 12: Physicians should explore the social situation, attitudes, beliefs and worries related to diabetes and self-care. Physicians are responsible for assessing the well-being and psychological status of the patient using questionnaires or validated measures[15] (Grade B; EL 2).
-
Recommendation 13: In communicating with a patient, physician should adopt a whole-person approach, and discuss outcomes and clinical implications if necessary[48] (Grade B; EL 3).
-
Five attributes of diabetes care professionals: CARES[47]
- C = Confident competence
- A = Authentic accessibility
- R = Reciprocal respect
- E = Expressive empathy
- S = Straightforward simplicity
-
Relationship-centered approach
Relationship-centered approach is a framework that recognizes the nature and quality of relationship between patient and provider, which needs to be given due importance.[49] It involves extending the principles of a patient-centered approach to encompass other participants in the medical system. Successful management of disease requires a development goal and is facilitated by stronger physician–patient relationships, where communication is a core tool.
Recommendation 14: Open communication between patient and physician must be encouraged for treatment that is logical, acceptable and feasible to both[50] (Grade A; EL 4).
Recommendation 15: Health professionals should aim for greater integration with patients based on cultural, social, cognitive and linguistic comprehension, and must be responsive to cognitive, motivational and emotional barriers in the provider–patient relationship[51] (Grade B; EL 4).
PSYCHOLOGICAL ASSESSMENT AND MANAGEMENT
Although many people with diabetes cope well and live normal, healthy lives with diabetes, several studies, including diabetes attitudes and the wishes and needs (DAWN) study, emphasized that psychological support is under-resourced and inadequate in both adults and children with diabetes, resulting in poor quality of life and reduced general well-being.[3] It is important to establish ways to achieve emotional well-being as part of diabetes management and to include psychological assessment and treatment into routine care rather than wait for the identification of a specific problem or deterioration in psychological status.[52] Furthermore, improved access to health care professionals trained in identifying patients’ needs for providing counseling and psychosocial support is needed for effective management of diabetes.[53] Psychological interventions that use the therapeutic alliance between patient and therapist are understood in emotional, cognitive, and behavioral context.[54] It is known that addressing psychological needs has a positive effect on diabetes outcomes in terms of reduced glycosylated hemoglobin[55] as well as co-morbid depression and systolic blood pressure.[56]
Evidence-based guidelines for psychosocial care in adults with diabetes have been included in the Canadian Diabetes Association,[57] SIGN,[7] National Institute of Health and Clinical Excellence (NICE),[58] Institute for Clinical Systems Improvement,[59] German Diabetes Association[60] and, for the first time in 2005, in the ADA standards of care,[8] indicating the importance of psychological interventions in different problem areas.
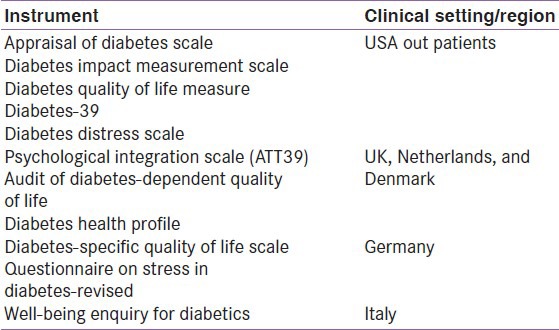
Psychological assessment
The considerable impact that diabetes and its treatment can have on quality of life is, perhaps, that this disease has spurred a large number of attempts to develop patient-assessed health outcome measures specific to diabetes. Several reliable instruments useful in assessing psychosocial adjustment to diabetes have been included in various evidence-based guidelines for psychosocial care, such as Well-being Questionnaire (WHO-5)[61] (in SIGN, ADA, IDF-2005; Patient Health Questionnaire-9 (PHQ-9)[62] by SIGN, German Diabetic Association; Problem Areas in Diabetes (PAID) Scale[63] by NICE and ADA guidelines. Studies reported several other diabetes-specific psychological screening instruments with good evidence of reliability and validity, which are currently being implemented [Table 4].[64]
Table 4.
Populations in which the instruments were evaluated[64]
Recommendation 16: When psychosocial problems are identified, healthcare professionals should explain the link between these and poorer diabetes control. They should advise patients where best to obtain further help, and facilitate this if appropriate[65,66] (Grade A; EL 1).
Recommendation 17: Assessment of the patient's psychological and social situation must be part of the diabetes management using reliable, validated tools that include instruments and questionnaires[53] (Grade A; EL 1).
Recommendation 18: From the Indian perspective, consider Self-perception of Health Questionnaire,[54] WHO-5, PAID and other diabetes-specific questionnaires available in local languages as suitable tools[15,46] (Grade B; EL 2).
Psychological management
In medical and mental health settings, psychological treatments are routinely used to improve outcomes, e.g., to reduce psychological distress and improve adherence. The need for effective, well-evaluated psychosocial interventions to help people to deal with the routine stress of diabetes (diabetes distress) has been widely noted in the literature.[67] Especially now that treatment regimens are becoming more and more intensive, comprehensive behavioral changes are required. Additional psychosocial support is called for to help people to make these changes and to preserve and sustain their efforts with the goal of optimizing both glycemic control and quality of life.[54]
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT), also called “Socratic Dialogue,” is an approach that helps patients recognize the power of “self-talk” (what they say to themselves) and enhances emotion-focused coping skills in dealing with emotional distress. CBT has gained much prominence as psychotherapy for depression and other problems.[68,69] In CBT, individuals are educated and trained on changing habitual patterns of responding to challenges or problems. It uses measurement tools designed to determine the individual's perception (cognition) and understanding of diabetes and its self-management (behavioral changes). Thus, the cognitions and behaviors are intertwined and the cognitions are changed the same way one would change other behaviors, through identifying alternatives.
CBT is recommended as a primary psychological intervention for looking at “negative behaviors” and “dysfunctional thoughts” among people with diabetes by the NICE, SIGN, ADA and IDF guidelines.[70] Studies have shown that CBT is either similar or more effective than medication in the treatment of psychological problems, including depression, anxiety, and stress.[71,72] Several reviews concluded that cognitive behavioral interventions have beneficial effects on mood and metabolic control with improvements in course and outcome.[73,74] It has been suggested that integrating CBT with the current practice of diabetes management would be ideal for the future.[75] As evident from a randomized controlled trial, CBT was shown to improve glycemic control in patients with diabetes when combined with patient education.[76]
The questions used in CBT are termed the five W's: What, where, when, why, and whom, and the model used is termed FIND: Frequency, intensity, number of times and duration of the individual's problem. However, implementing CBT requires a fair amount of experience and skill, which demand substantial clinical training with backgrounds in counseling, nursing, psychiatry, psychology, or social work. Discussing patient's behavior, resistance, rituals and consequences aligned with interpersonal problems can further increase the healthcare professional's understanding of the patient's perspective.[77]
Recommendation 19: CBT should be recommended either alone or in combination with other strategies to diabetes patients with co-morbid psychiatric disorders or to improve glycemic control and emotional well-being[78,79] (Grade A; EL 1).
Recommendation 20: Healthcare professionals should receive formal training in CBT[28] (Grade A; EL 1).
Recommendation 21: A simple method that can be followed in the Indian context is the Karnal Model for counseling[80] (Grade A; EL 1).
-
Recommendation 22: Healthcare professionals should have at least eight sessions with the patient during the therapy[76] (Grade C; EL 3).
- Karnal model[31,80]: The Karnal model relies on the cognitive behavioral therapy approach, which follows the “antecedents’ lead to behavior’ leads to consequences” (ABC) framework which will be effective only if a complete history of the patient is considered. The model represents an easy, simple and acceptable method of counseling applicable to various psychological disorders and can be used in all health care situations, including similar resource-challenged settings with social constraints.
Motivational therapy
Motivational enhancement therapy is a brief counseling method for enhancing motivation to change problematic health behaviors by exploring and resolving ambivalence. Although it has successfully been used in the field of addictions, it lacks sufficient evidence for effectiveness in improving diabetes control.[78] It is more patient-centered and empowering than traditional care.[81] The therapy has been recommended by IDF, ADA and SIGN for improving the psychological well-being in patients with diabetes.
This therapy involves a patient-centered counseling through motivational interviewing (MI), and has been shown to enhance glucose control in specific patient groups (older obese women with non-insulin-dependent DM).[82] MI appears to be a promising approach for adolescents as well, with initial studies showing improved glycemic control.[83,84] A recent multi-center randomized trial demonstrated that MI with adolescents improved long-term glycemic control and quality of life.[85] A modified version of MI, known as “WATER,” involves a checklist designed for healthcare professionals to change the patient's attitude toward problematic behaviors and improve diabetes care-related behaviors.[86]
Recommendation 23: Physicians should receive formal training in interventions involving MI, like WATER[86] (Grade A; EL 3).
Recommendation 24: Patients should be motivated to initiate or intensify insulin using motivational approaches, such as analogy building, which reduce clinical inertia as well as patient resistance related to insulin usage[31,86] (Grade A; EL 4).
Recommendation 25: Long-term motivational therapy with suitable follow-up is recommended in combination with CBT for improvement in HbA1c levels in poorly controlled type 1 diabetes mellitus (T1DM) adults[87] (Grade B; EL 1).
Problem-solving therapy
Problem-solving is a learned behavior involving strategies for problem resolution. In this, the individual is required to select, apply and evaluate the effectiveness of a chosen strategy.[88] It is a prerequisite for decision making to help reinforce healthy behaviors on a daily basis and involves problem specification, goal and barrier identification and application of skills, and knowledge and experiential learning.[89]
Several tools are available to assess the problem-solving approach, such as the Diabetes Self-Management Assessment Report Tool (D-SMART®),[90] Diabetes problem-solving inventory,[91] Assessment of primary care resources and supports for chronic disease self-management tool, to facilitate assessment and improvement of support for patient self-management.[92]
Recommendation 26: Therapy should be individualized, and is recommended in children/adolescents for improvement in behaviors and adherence and in adults for dietary behavior[93] (Grade A; EL 1).
-
Recommendation 27: Problem-based approach should be used in conjunction with diabetes self-management education, patient empowerment and life-long management programs to improve diabetes-related outcomes and quality of life[94] (Grade A; EL 1).
-
Modified version of MI: WATER approach[86]
-
W = Welcome warmlyBody LanguageThe OPD encounter
-
A = Ask and assessIdentifying and using cuesInternal, external, laboratoryHierarchy of questioningThe insulin encounter
-
T = Tell truthfullyMid-sentence analysisVerbal/non-verbal cuesAnalogy building
-
E = Explain with empathyExamples/Experience-sharingDemonstrationCoping skills training
-
R = Reassure and returnProchaska's theory of motivationMinimizing discomfort of changeWorking the environment (Eco-sensitivity)
-
-
Coping and counseling therapy
The basic idea of a coping strategy is that it should ease stress, provide comfort or enhance one's mood in a difficult situation and have a constructive, lasting impact on the mind and body. Coping is a complex process that can be defined as “constantly changing cognitive and behavioral efforts to manage specific external and/or internal demands that are appraised as taxing or exceeding the resources of the person.”[95] Tools like Ways of Coping Questionnaire are available to assess parents in coping with their child's insulin-dependent diabetes.[96]
Recommendation 28: Group-based counseling programs in conjunction with psychological counseling, CBT and behavioral family systems therapy-diabetes (BFST-D) are recommended to reduce diabetes-related stress as well as achieve glycemic control in problematic diabetics[5] (Grade A; EL 1).
Recommendation 29: It is recommended that healthcare professionals should receive formal training in psychological interventions involving coping and counseling for improved patient satisfaction and therapeutic outcomes[28] (Grade A; EL 1).
Recommendation 30: Greater social support, patient empowerment and supporting coping skills must be considered among women with diabetes for better psychosocial adjustment to illness[46,97] (Grade A; EL 2).
Recommendation 31: Family physicians should encourage patients with diabetes to integrate positive coping skills and de-learn negative coping mechanisms such as rumination (excessive thinking about the disease), catastrophizing (assuming undue negative impact to the disease), self-blame (blaming oneself for the illness) and other-blame (blaming others for one's condition) in their daily life[98] (Grade A; EL 2).
Recommendation 32: Therapy to improve resilience resources and coping strategies of patients is recommended in patients finding difficulty in adjustment with treatment and lifestyle modification[99] (Grade B; EL 3).
Family therapy
Several studies have shown the link between high levels of non-diabetes-specific family factors, such as conflict, stress and family cohesion, with poorer glycemic control and adherence.[100] Family therapy helps to reduce diabetic-related conflict between family members and reduces the impact of stress and mental health disorders associated with diabetes, particularly in children and adolescents.[101] An intervention based on family-focused teamwork increased family involvement without causing family conflict or adversely affecting youth quality of life, and helped prevent worsening of glycemic control.[102]
Recommendation 33: BFST-D in combination with educational support is recommended in reducing family conflict and improving treatment adherence in patients with diabetes with poor glycemic control and improving overall family communication and problem-solving skills[15,103] (Grade A; EL 1).
Recommendation 34: Family therapy should be recommended in children to allow for a better balance between parental and self-care of the child[104,105] (Grade A; EL 4).
Recommendation 35: Physicians should explore the role of family support and family functioning in implementing family-oriented programs for individuals with diabetes[15] (Grade B; EL 3).
Yoga and meditation
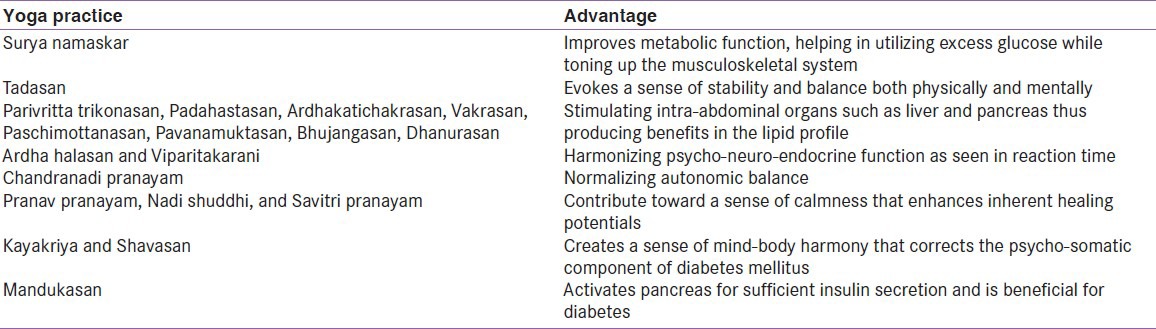
Lifestyle modification through yoga produces consistent physiological changes and can make an appreciable contribution to primary prevention as well as management of diabetes. Yoga has been studied for controlling the symptoms and complications of diabetes. A comprehensive yogic breathing program has been shown to improve the physical, psychological, and social domains and total quality of life in people with diabetes taking oral hypoglycemic drugs (OADs),[106] and is recommended as an effective complementary or integrative therapy program for diabetes management.[107,108] Table 5 summarizes the important yoga practices and their advantages.
Table 5.
Benefits of yoga practices on management of diabetes[108]
Recommendation 36: Yoga is recommended as it can improve well-being, reduce weight and improve sleep in individuals with diabetes[109,110] (Grade A; EL 4).
Recommendation 37: Comprehensive yogic breathing can be prescribed to improve the quality of life in patients with diabetes[106] (Grade B; EL 1).
Recommendation 38: Patients with pre-existing complications such as cardiovascular and other comorbidities are recommended to practice yoga regularly for the better management of diabetes[111] (Grade B; EL 1).
Recommendation 39: Physicians should use stress management educational programs like yoga to improve the subjective well-being scores of people with diabetes and to contribute to the primary prevention as well as management of diabetes[112] (Grade C; EL 3).
Folk dance therapy
Dance/movement therapy is a popular form of physical activity that deals with individual's physical, emotional, cognitive and social integration. A total body movement such as dance enhances the functions of other body systems, such as circulatory, respiratory, skeletal and muscular systems, and is known to increase neurotransmitter and endorphins in the brain, which create a state of well-being. Today, dance/movement therapy is a well-recognized form of complementary therapy used in hospitals for special settings associated with physical and psychological problems.[107]
Recommendation 40: Dancing twice a week for 8-12 weeks is recommended for diabetes patients for improved outcomes of HbA1c, weight, body fat and blood pressure[113] (Grade B; EL 2).
Recommendation 41: Group activities such as round dances, where singing, dancing, and socializing are to be embedded in the Diabetes Prevention Program under a community-based participatory research approach, can improve outcomes in patients with diabetes[114] (Grade C; EL 3).
Sexual dysfunction counseling
Chronic medical conditions, particularly diabetes, are frequently associated with sexual difficulties and problems, which are often underreported and underdiagnosed. Furthermore, patients and physicians may feel uncomfortable while discussing such issues. They may feel that sexual problems are not important enough to be mentioned in the context of disease, resulting in poor glycemic control. The situation gets worse with the presence of a comorbidity such as depression. Patients should be encouraged to talk about their sexual problems with the therapist or physician, as both biomedical and psychosocial factors have to be explored. Therapeutic interventions should include basic counseling, biomedical treatment of atrophy and lubrication difficulties, as well as treatment of comorbidities and/or sex therapy.
Recommendation 42: Physicians should be trained to evaluate sexual problems in both genders in order to facilitate recognition and possible treatment[80,115] (Grade A; EL 3).
Recommendation 43: Diabetic hypertensive/neuropathic patients should be evaluated for sexual dysfunction and appropriate therapy should be considered[116] (Grade A; EL 3).
Recommendation 44: Therapeutic interventions should include basic psychological counseling, biomedical treatment as well as treatment of comorbidities and/or sex therapy[117] (Grade A; EL 3).
Eating habits
Diet adherence and managing wrong eating habits are crucial in the management of diabetes. Eating disorders are frequently seen in patients with T1DM, especially children and adolescents who also skip insulin as a form of weight control. This leads to an earlier than expected onset of diabetes-related microvascular complications, particularly retinopathy.[118] There is also evidence that adolescents with diabetes, especially girls, have a higher incidence of eating disorders, and that eating disorders are associated with poor glycemic control.[119,120,121] A dietary regimen adherence in diabetes mellitus (DRADMS) questionnaire was developed to obtain a measure of the T2DM patients’ problems in preventing adherence to the regimen.[122]
Recommendation 45: Management of eating disorders requires a multidisciplinary team: Endocrinologist/diabetologist, nurse educator, nutritionist, psychologist and, frequently, psychiatrist[118] (Grade B; EL 4).
Recommendation 46: While treating T1DM patients with eating disorders, physicians should consider including diabetes treatment, nutritional management, and psychological therapy[118] (Grade B; EL 4).
Recommendation 47: For T2DM patients with non-adherence to diet, closer scrutiny, use of DRADMS questionnaire and psychosocial counseling are recommended[122] (Grade B; EL 2).
Recommendation 48: Policy decision about built environment and accessibility of fast foods must be incorporated in residential areas and near educational institutions[123,124] (Grade B; EL 4).
Management of type 1 diabetes in adolescents
Management of T1DM in adolescents and children is an important psychological aspect that requires utmost care, particularly in the adolescent age group. It is at this period of life when the child desires freedom and independence, and this produces barriers in achieving a good glycemic control. The ISPAD Consensus Guidelines 2000, which stated that “Psychosocial factors are the most important influences affecting the care and management of diabetes,” also emphasized the importance of psychological care of children and adolescents with diabetes.[10] In a 10-year prospective study from diagnosis of type 1 diabetes, it was found that adolescents were at high risk for various psychiatric disorders.[125,126] Furthermore, there is also evidence that adolescents with diabetes have a higher incidence of eating disorders and are associated with poor glycemic control and early onset of diabetes-related complications.[118,119,120,121]
For adolescents with T1DM family communication, conflict resolution and problem-solving skills are critical elements for the effective management of diabetes. Family communication helps to reduce diabetic-related conflict between family members and reduces the impact of stress and mental health disorders associated with diabetes in children and adolescents.[101] Other therapies like MI and behavioral family systems therapy appear to be promising approaches for adolescents for improved glycemic control.[83,84] A recent multi-center randomized trial demonstrated that MI with adolescents improved long-term glycemic control and quality of life.[85]
Recommendation 49: Therapies such as problem solving and MI should be individualized in children/adolescents with diabetes for enhancement in behaviors, adherence to medication and change in dietary patterns for improved glycemic control[85,88] (Grade A; EL 1).
Recommendation 50: BFST-D in combination with educational support is recommended for adolescents with diabetes, which helps in refining problem-solving skills for reducing family conflict and improving treatment adherence in order to achieve better glycemic control[103] (Grade A; EL 1).
Recommendation 51: Problem-focused coping strategies and behavioral coping skills are recommended in adolescents with T1DM for better metabolic control, psychosocial adjustment and treatment adherence[127] (Grade A; EL 3).
Recommendation 52: Adolescents with difficulty in achieving treatment goals or with recurrent diabetes ketoacidosis should be screened for psychiatric disorders[128] (Grade B; EL 1).
PSYCHIATRIC ASSESSMENT
The impact of mental illness on diabetes patients has become a major concern for overall health, as they are at least twice as common in them compared with the general population. A study reported that at least 30% of the diabetes patients had anxiety disorders, while 8.5-32.5% had depression.[129] There is growing evidence, particularly from North America, that young people with diabetes appear to have a greater incidence of psychiatric disorders.[125,126,130] In a 10-year prospective study from diagnosis of type 1 diabetes, adolescents were at high risk for various psychiatric diagnoses; females were more likely than males to receive a diagnosis, and half of those with a history of poor glycemic control had a psychiatric diagnosis.[126] Diabetes and psychiatric disorders share a bidirectional association, both influencing each other in multiple ways. The severity of one disorder often contributes to the pathogenesis of the other resulting in comorbidity. For instance, diabetes in individuals results in emergence of psychiatric disorder or psychiatric disorders like depression can not only act as a significant risk factor in the development of diabetes but also interferes with the management of diabetes by influencing treatment adherence. Furthermore, impaired glucose tolerance and diabetes could merge as a side-effect of the medications used in the treatment of psychiatric disorders.[131] Psychiatric comorbidity with diabetes is associated with impaired quality of life, increased cost of care, poor treatment adherence and poor glycemic control.
Strategies to address psychiatric comorbidities
Recommendation 53: Training of general practitioners and physicians in the identification and management of psychiatric comorbidities in rural and urban areas is recommended[38] (Grade C; EL 4).
Depression
Diabetes and depression appear to have a consistent bidirectional relationship, with depression often preceding the development of T2DM in adults.[132] Depression and diabetes may be related through either biological or behavioral pathways. Biological pathways include hormonal abnormalities, alterations in glucose transport function and increased immuno-inflammatory activation.[133] While negative health behaviors associated with depression, such as inactivity, poor diet, smoking and non-adherence to treatment, recommendations and self-care may be important explanatory behavior factors that may impact diabetes and its complications.
Assessment of depression
Recommendation 54: A careful assessment of depression in diabetes should include the use of a structured clinical interview (Grade A; EL 4).
Recommendation 55: Self-reported measures such as the Beck Depression Inventory,[134] Centers for Epidemiologic Studies Depression Scale,[135] PHQ-9,[136] Hamilton Rating Scale for Depression and Hospital Anxiety and Depression Scale (HADS) are to be considered to assess depression in patients with diabetes.[137] The Geriatric Depression Scale is used to screen for depressive symptoms in older individuals. Validated diabetes-specific psychological instruments are also available that can be used in diabetes management[15,46] (Grade A; EL 1).
Recommendation 56: Recognizing and providing treatment for subclinical presentations of depression are recommended[52,138] (Grade B; EL 3).
Recommendation 57: Differentiating symptoms of depression that are directly associated with diabetes from those that may be more independent of diabetes is recommended based on the International Statistical Classification of Diseases and Related Health Conditions-10 of the WHO and Diagnostic and Statistical Manual of Mental Disorders-IV of the American Psychiatric Association[131] (Grade C; EL 2).
Anxiety
Diabetes-related stress, including feeling overwhelmed by diabetes and its care, feeling discouraged with the treatment plan and feeling fearful of the future, may contribute to the symptoms of anxiety. The stress of dealing with diabetes may impact patients’ psychosocial functioning and quality of life, which may also increase the risk for developing anxiety symptoms.[139] Diabetes patients may experience short-term, episodic stress related to self-care activities or more long-term, chronic stress related to living with a chronic illness, which may eventually develop into anxiety symptoms or a chronic anxiety disorder.[13]
Assessment of anxiety
Recommendation 58: Proper identification and diagnosis of anxiety is recommended to distinguish diabetes-related physical symptoms from an anxiety disorder[140] (Grade B; EL 4).
Recommendation 59: Screening tools such as the HADS[141] and the Generalized Anxiety Disorder-7 Scale,[142] PHQ and Symptom Checklist-90 are to be considered (Grade B; EL 1).
Recommendation 60: Physicians should consider standardized scales facilitating diabetes-focused assessment that include the Diabetes Distress Scale,[143] Diabetes Quality of Life Questionnaire,[144] hypoglycemia fear survey[145] and Diabetes Fear of Injection and Self-Testing Questionnaire[146] (Grade A; EL 1).
PSYCHIATRIC MANAGEMENT
Psychopharmacologic medication
Psychotropic medications, helpful in reducing the psychological symptoms in individuals with emotional health problems, are most effective when used in conjunction with other approaches such as CBT, Problem-Solving Therapy, etc., A number of medications have been shown to effectively treat a variety of emotional health problems[147] of varying intensity.[148] Nonetheless, psychotherapy and pharmacotherapy do not show strong differences in effect sizes and, hence, the option of using psychopharmacologic agents in therapy must be made after due consideration of all the factors of patient well-being and empowerment.[148]
Recommendation 61: Choice of pharmacotherapy should give due consideration to criteria such as contraindications, treatment access or patient preferences, and must be used as a complement to psychotherapy[39,149] (Grade A; EL 1).
Recommendation 62: Physicians should be aware of the possible metabolic adverse effects of psychotropic medications[39] (Grade A; EL 4).
Management of depression
Recommendation 63: Psychotropics such as antidepressants (Phenylzine), antipsychotics (Haloperidol, Ziprasidone, and Aripiprazole) and mood stabilizers (Topiramate) associated with a low risk of impaired glycemic control are recommended to manage depression with diabetes[131] (Grade A; EL 4).
Recommendation 64: Tricyclic antidepressants, selective serotonin reuptake inhibitors, norepinephrine reuptake inhibitors and serotonin modulators are to be avoided as they have been shown to be associated with increased risk of diabetes following intermittent and continued long-term use[150] (Grade A; EL 1).
Recommendation 65: Non-pharmacological interventions such as CBT and interpersonal therapy can be used either alone or in combination with pharmacotherapy[72,131] (Grade A; EL 4).
Recommendation 66: Psychiatrists should be sensitized to understand the multifaceted interactions between diabetes and psychiatric disorders for improved therapeutic outcomes[131] (Grade A; EL 4).
Management of anxiety
Recommendation 67: Psychological interventions focused on self-care, such as group education programs including coping skills, behavioral-cognitive skills, relaxation techniques, problem-solving skills, mindfulness-based stress management and family therapy, are to be considered[139,151] (Grade B; EL 3).
Recommendation 68: Behavioral intervention can be included as an adjunct to routine medical care in the management of young people with T1DM[152] (Grade B; EL 1).
Electroconvulsive therapy in diabetes
The literature on the effect of electroconvulsive therapy (ECT) on DM remains controversial, with evidence of both amelioration and worsening of hyperglycemia.[153] Reports of ECT leading to dangerous hyperglycemia in a previously non-diabetic patient suggested the possibility of an unmasking or exacerbation of diabetic pathology during a course of ECT.[154] But, another more recent study included 19 patients with insulin-requiring T2DM undergoing ECT, none of whom were on oral hypoglycemic drugs. There was no statistically significant difference in the average daily insulin requirements or acute glycemic control associated with ECT, suggesting that ECT in insulin-requiring type 2 diabetes patients is safe and efficacious.[155]
Recommendation 69: ECT is suggested to be safe and efficacious for T2DM patients requiring insulin in some literature, although caution must be practiced before prescribing it[155] (Grade C; EL 3).
SOCIAL ASSESSMENT AND MANAGEMENT
Social factors currently play a small role in the treatment plan for diabetes. Nonetheless, social factors have an important role in the acceptance, adherence to treatment and overall outcome of diabetes management. Studies have found the importance of social (economic class, financial expenditure, regional disparities, family structure, affordability to medical care, educational profile) and cultural factors (ethnicity, customs, food habits, fasting conditions, community beliefs) in the prevalence and management of diabetes care.
In resource-limited countries like India, diverse social, cultural as well as religious economic, psychological, regional, educational, and familial factors have consequences on the clinical progression, treatment and outcome of any disease management.[46] Thus, we need to lay emphasis on working on the environment (eco-sensitivity) and medical anthropology for the better management of diabetes. Further, taking into consideration the perceptions of patients’ for different therapeutic agents from different social structures, ethnopharmacy also plays an important role. The socioeconomic status of households/individuals in urban as well as in rural areas in India can be assessed from the scale developed by Tiwari et al. 2005[156] and updated in 2012.[157] The scale can play a key role in the development of evidence-based guidelines based on the indication and efficacy of care practices directed at social issues, which is much needed for health care professionals engaged in diabetes care.
Social structure
The influence of social class or socioeconomic status on the incidence and management of diabetes is observed globally as well as in India. In India, cultural diversity and deep-rooted social structures have great implications on the clinical course, treatment and ultimate outcome of any disease. Prevalence of diabetes is reportedly higher in the highest socioeconomic groups, and decreases with decreasing socioeconomic status in India.[158] However, populations with diabetes from the lower social class and no health insurance were found to be at the greatest risk of not receiving preventive care[159] in the USA or admission to hospital for diabetes care[160] in the UK. While diabetes was once considered a disease of affluence, in the last decade, its prevalence rates in the middle and lower income groups have shown a trend toward convergence.[161] Families with higher average family income and education profile are known to spend more on diabetes care.[162]
Recommendation 70: Because socioeconomic status and health insurance play an important role in access to diabetes care, physicians are recommended to assess the socioeconomic class of the patient for better disease management[159] (Grade B; EL 2).
Recommendation 71: Physicians must be sensitive to the income and education profile of patients while choosing therapeutic options, to promote greater adherence to therapy and to improve outcome[162] (Grade B; EL 4).
Family structure
Several studies from India have demonstrated the importance of family structure in the management of diabetes. In India, it is reported that cost-effective focus for overall diabetes care can be placed on the nuclear family as a unit,[39] which occupies 60% of the total household units[163] with mean size of 4.8 persons per house, (rural areas – 4.9 persons, urban areas – 4.6 persons). Other aspects in diabetes management and involving family risk factors associated with the same are[5] low marital satisfaction; high criticalness, hostility, conflict; poor problem-solving skills; low family coherence; low closeness/cohesion; low family organization; lack of congruence in diabetes beliefs and expectations. For adolescents with T1DM, family communication, conflict resolution and problem-solving skills are critical elements for the effective family management of diabetes. Moreover, social bonds, especially family bonds, are known to influence outcomes of diabetes management, which holds the key to avoiding negative progression of the disease.[164] The practical and emotional strains arising out of this affect diabetes management and family beliefs and emotion management and help manage this impact by improving patient morale. However, unresolved family conflicts about diabetes are associated with more depressive symptoms and lower quality of life.
Recommendation 72: Physicians should encourage patients to seek support from family members, based on individual family structures, overcome barriers in adherence to treatment and promote patterns of behavior, which may make diabetes management easier[165] (Grade A; EL 2).
Recommendation 73: In weight loss programs, healthcare providers should recommend the collaboration of a spouse to actively work together to reach a common goal[166] (Grade A; EL 2).
Recommendation 74: Diabetes management should be made more flexible and convenient in a familial context to reinforce the patient's personal sense of health, emotional well-being and ability to maintain diabetes care[164] (Grade C; EL 4).
Gender discrimination
Gender discrimination toward healthcare, including diabetes, is observed all over the world. In India, higher outpatient attendance for T1DM is recorded for men than for women (<30 years age). Interestingly, half of these young women who are at a marriageable age often lose their follow-up to clinic due to perceived social stigma, often leading them to medical consequences, including diabetic ketoacidosis.[167] The reasons for the same are mainly disbeliefs as “will she be able to cope with the house work, can she have a normal baby, she will require more care and so on.” Women show poorer compliance to therapy due to greater economic dependence on family members.[23] Differences in functional limitations between adults with and without diabetes are more evident in women than they are in men, due to their strong association with biological and behavioral factors.[97]
Diabetes is often perceived as a costly disorder in India; parents usually get their daughters married without disclosing that she has diabetes, which has eventually lead to very grave consequences. Another aspect of gender discrimination in diabetes care comes from the role of parents in the management of children with T1DM, where mothers often share a disproportionate burden of diabetes care in the child. If fathers do not share in the responsibility, they feel out of touch with the complexities of management. Therefore, care should be taken to ensure distribution of responsibility between the parents.[168] Affirmative action is required on the part of diabetes care professionals to ensure that women are not discriminated against as far as diabetes care is concerned.
Recommendation 75: Inclusion of interventions that increase women's perceived self-confidence and social support for positive health outcomes is recommended[169] (Grade B; EL 3).
Recommendation 76: Social support and self-confidence of women with type 2 diabetes in determining their individualized goals and strategies must be assessed[170] (Grade C; EL 4).
Recommendation 77: Diabetes health care professionals treating young women who are at a marriageable age with diabetes should engage in educating parents, the girl to be married and the prospective groom and his parents about the management of the disorder and provide confidence and reassurance that she can lead a normal life if taken care of properly with respect to medication and regular checkup (Grade A; EL 4).
Custom/religion
Cultural differences in the form of language, educational backgrounds, religion, health attributions, beliefs and practices toward illness must be acknowledged and considered by healthcare providers for treatment decisions and to determine how to obtain this information from patients,[171] especially in people with a South Asian origin.[172] Because of the vast diversity of cultural and religious health attributions, beliefs and practices, it is important to prioritize such factors in diabetes care and education.[171] In chronic conditions like diabetes, religious or spiritual beliefs become increasingly important; firstly, because they provide the social and emotional support and, secondly, because they aid in coping with the stress of the disease. Hindus observe fasting and go to strenuous pilgrimage like Amarnathji as part of their religious traditions during various times of the year. Jains may not eat from dusk to dawn, irrespective of the duration of this period. Buddhists observe the 3-month-long Buddhist lent during the rainy season.
People with diabetes are recommended to follow the physician's advice in observing fasts or going to pilgrimages to avoid any glycemic emergencies.[173] Similarly, worldwide, Muslims fast during the month of Ramadan. People with diabetes, who wish to fast, have been stratified based on the severity of disease, and specific rules and recommendations have been issued.[174] People with diabetes who are categorized in the “observe fasting” group are further advised to follow the recommended strategies to ensure safety before, during and after the month of Ramadan.
Recommendation 78: “Culturally competent assessment tool” can be used to test the cultural competency of healthcare delivery interventions[175] (Grade B; EL 1).
Recommendation 79: Indian physicians, who often have to manage a multilingual, multi-ethnic population, should be sensitized to the importance of cultural and religious health attributes, beliefs and practices (Grade A; EL 4).
Recommendation 80: Physicians should recommend pilgrims to undergo pre-pilgrimage health clearance and educate them about hypoglycemia, need of caloric intake, compliance with medications or insulin, glucose monitoring, carrying their medical records and importance of protective wear[173] (Grade A; EL 3).
Recommendation 81: Those who are medically fit to fast need education about the importance of balanced diet, moderate physical exercise, adherence to advised medications, self-monitoring of glycemia, early recognition of dangerous situations and necessary remedial measures[165] (Grade B; EL 4).
Recommendation 82: Ramadan-focused patient education should focus on pre-Ramadan evaluation, risk stratification and generous religious exemptions available for deserving individuals[176] (Grade B; EL 4).
Recommendation 83: Physicians should educate patients on the availability of modern insulin analogues for diabetes care during Ramadan for better control and therapeutic outcome[176] (Grade A; EL 4).
Recommendation 84: Religious and cultural leaders should be requested and encouraged to speak positively about modern diabetes care[177] (Grade A; EL 4).
Recommendation 85: Physicians should be trained to enquire about the role of religion and spirituality in patient's life using standardized screening questions[178] (Grade C; EL 4).
Recommendation 86: Physicians should pose questions about religion and spirituality that are framed specifically in the context of patients’ coping and self-managing with diabetes that are comfortable for both the patient and the clinician[178] (Grade C; EL 4).
Recommendation 87: Physicians should provide information, training and skill-building activities to sensitive patient's cultural context and disseminate diabetes education[179] (Grade D; EL 3).
Recommendation 88: A culturally competent perspective should be the key for treatment of diabetes in people with diverse cultural and religious backgrounds[171] (Grade D; EL 4).
Recommendation 89: Important diagnostic and racial differences in religious participation and the supports required for enhanced quality of life for persons with serious mental illness and diabetes at religious participations may be considered[180] (Grade D; EL 4).
Urban/rural settings
The prevalence of diabetes has increased in the urban and rural areas of India, with an urban-rural split of 2:1 or 3:1 sustained through the last two to three decades.[181] Lifestyle factors and family history play synergistic roles in increasing the risk of diabetes in the urban population,[182] which is consistent with the rise in burden of overweight and obesity.[183] Awareness about diabetes and management are also lower in the rural population.[184]
Because the demography of India is predominantly rural, even with a lower rate of prevalence, the rural population in India can be expected to constitute a larger proportion of the diabetes population. Unfortunately, lack of access to early diagnosis of disease, quality healthcare, and healthcare infrastructure is impeding healthcare standards in rural India. Affirmative action is required on the part of diabetes care professionals to ensure that no section of society is discriminated against as far as diabetes care is concerned.
Recommendation 90: While treating the rural population with diabetes, physicians should assess people at risk of psychosocial problems and provide counseling on self-care and psychosocial management[65] (Grade A; EL 4).
Community reaction
Job discrimination and social isolation are common fears about the expected community reaction to a person living with diabetes. In India, families with young female diabetes patients fear ill-treatment at school or college, reduced future marriage prospects, isolation in social relations, etc., as a result of disclosure of their diabetic status.[167]
Recommendation 91: An understanding of factors that influence patients’ decisions to maintain confidentiality about diabetes within their social networks is needed for using community-based interventions to improve diabetes self-management in ethnic minority patients[185] (Grade A; EL 3).
Affordability
Economic affordability in the context of diabetes depends on the share of annual house hold expenditure spent on diabetes care. In India, out-of-pocket payments form a large share of house hold expenditure and result in a financial strain on the household. According to the World Health Statistics, 2012, currently, India has less than half the global average of physician per 10,000 patients and healthcare expenditure (as a % Gross Domestic Product). A larger share of this expenditure comes from the private sector through the out-of-pocket expenses recovered from patients.
Recommendation 92: Physicians should discuss the cost of medication with the patients, considering the economic status of the patient[19] (Grade B; EL 4).
Recommendation 93: Physicians should encourage households with individuals involved in diabetes care to seek health insurance[19] (Grade C; EL 4).
Recommendation 94: For diabetes care in a resource-poor population, physicians should recommend primary prevention through promotion of healthy lifestyles and risk reduction as the most cost-effective intervention (Grade D; EL 4).
CONCLUSIONS
The current guideline on psychosocial aspects of diabetes encapsulates global evidence and experience, while maintaining a uniquely Indian flavor. Publications from a wide range of sources have been considered while designing the recommendations, and represent a vast cross-section of opinions. This guideline bridges a crucial gap in diabetes management and hopes to address the scale and variety of challenges in the psychosocial management of diabetes in India. It should encourage all stakeholders in diabetes care to create and devote adequate time and resources to ensure optimal psychosocial management of people with diabetes.
ACKNOWLEDGMENTS
The authors thank Jeevan Scientific Technology Limited, Hyderabad, for providing writing assistance in the development of this manuscript.
The authors thank members of the South Asian Referee Panel: Dr. Fatema Jawad, Pakistan; Dr. Syed Abbas Raza, Pakistan; Dr. Aisha Sheikh, Pakistan; Dr. Kishwar Azad, Bangladesh; Dr. Fauzia Mohsin, Bangladesh; Dr. Bedowra Zabeen, Bangladesh; Dr. Noel Somasundaram, Sri Lanka; Dr. Prasad Katulanda, Sri Lanka; Dr. Jyoti Bhattarai, Nepal; and Dr. Dina Shrestha, Nepal, for their valuable comments.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Weaver LJ, Narayan KM. Reconsidering the history of type 2 diabetes in India: Emerging or re-emerging disease? Natl Med J India. 2008;21:288–91. [PubMed] [Google Scholar]
- 2.Shah SN, Joshi SR, Parmar DV. History of insulin. J Assoc Physicians India. 1997;Suuple 1:S4–9. [PubMed] [Google Scholar]
- 3.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: Results of the cross-national Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005;22:1379–85. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 4.Ford DE, Biton V, Rubin RR, Peyrot M. Was Willis right? Thoughts on the interaction of depression and diabetes. Diabetes Metab Res Rev. 2002;18:173–5. doi: 10.1002/dmrr.292. [DOI] [PubMed] [Google Scholar]
- 5.Fisher EB, Thorpe CT, Devellis BM, Devellis RF. Healthy coping, negative emotions, and diabetes management: A systematic review and appraisal. Diabetes Educ. 2007;33:1080–103. doi: 10.1177/0145721707309808. [DOI] [PubMed] [Google Scholar]
- 6.Handelsman Y, Mechanick JI, Blonde L, Grunberger G, Bloomgarden ZT, Bray GA, et al. American association of clinical endocrinologists medical guidelines for clinical practice for developing a diabetes mellitus comprehensive care plan. Endocr Pract. 2011;17:1–53. doi: 10.4158/ep.17.s2.1. [DOI] [PubMed] [Google Scholar]
- 7.Scottish intercollegiate guidelines network. Sign 55. Management of diabetes, 2001. [Last accessed 2012 Sep 25]. Available from: http://www.sign.ac.uk .
- 8.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2005;28:S4. [PubMed] [Google Scholar]
- 9.IDF global guidelines for type 2 diabetes, 2005. [Last accessed 2012 Sep 25]. Available from: http://www.idf.org/webdata/docs/IDF%20GGT2D.pdf .
- 10.ISPAD. Consensus guidelines for the management of type 1 diabetes mellitus in children and adolescents, 2000. [Last accessed 2013 Apr 22]. Available from: http://www.diabetesguidelines.com/health/dkw/pro/guidelines/ispad/ispad/asp .
- 11.Venkataraman K, Kannan AT, Mohan V. Challenges in diabetes management with particular reference to India. Int J Diabetes Dev Ctries. 2009;29:103–9. doi: 10.4103/0973-3930.54286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hasan H, Zodpey S, Saraf A. Diabetologist's perspective on practice of evidence based diabetes management in India. Diabetes Res Clin Pract. 2012;95:189–93. doi: 10.1016/j.diabres.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 13.Petrak F, Herpertz S, Albus C, Hirsch A, Kulzer B, Kruse J. Psychosocial factors and diabetes mellitus: Evidence-based treatment guidelines. Curr Diabetes Rev. 2005;1:255–70. doi: 10.2174/157339905774574329. [DOI] [PubMed] [Google Scholar]
- 14.Young EE, Unachukwu CN. Psychosocial aspects of diabetes mellitus. Afr J Diabetes Med. 2012;20:5–7. [Google Scholar]
- 15.Sridhar GR, Madhu K. Psychosocial and cultural issues in diabetes mellitus. Curr Sci. 2002;83:1556–64. [Google Scholar]
- 16.Sridhar GR. Containing the diabetes epidemic. Natl Med J India. 2003;16:57–60. [PubMed] [Google Scholar]
- 17.Ramachandran A, Ramachandran S, Snehalatha C, Augustine C, Murugesan N, Viswanathan V, et al. Increasing expenditure on health care incurred by diabetic subjects in a developing country: A study from India. Diabetes Care. 2007;30:252–6. doi: 10.2337/dc06-0144. [DOI] [PubMed] [Google Scholar]
- 18.Ramachandran A. Socio-economic burden of diabetes in India. J Assoc Physicians India. 2007;55:9–12. [PubMed] [Google Scholar]
- 19.Rao KD, Bhatnagar A, Murphy A. Socio-economic inequalities in the financing of cardiovascular and diabetes inpatient treatment in India. Indian J Med Res. 2011;133:57–63. [PMC free article] [PubMed] [Google Scholar]
- 20.Samuel-Hodge CD, Headen SW, Skelly AH, Ingram AF, Keyserling TC, Jackson EJ, et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: Spirituality, the multi-caregiver role, and other social context factors. Diabetes Care. 2000;23:928–33. doi: 10.2337/diacare.23.7.928. [DOI] [PubMed] [Google Scholar]
- 21.Mehrotra R, Bajaj S, Kumar D, Singh KJ. Influence of education and occupation on knowledge about diabetes control. Natl Med J India. 2000;13:293–6. [PubMed] [Google Scholar]
- 22.Nagpal J, Bhartia A. Quality of diabetes care in the middle- and high-income group populace: The Delhi Diabetes Community (DEDICOM) survey. Diabetes Care. 2006;29:2341–8. doi: 10.2337/dc06-0783. [DOI] [PubMed] [Google Scholar]
- 23.Lahiri SK, Haldar D, Chowdhury SP, Sarkar GN, Bhadury S, Datta UK. Junctures to the therapeutic goal of diabetes mellitus: Experience in a tertiary care hospital of Kolkata. J Midlife Health. 2011;2:31–6. doi: 10.4103/0976-7800.83271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh P, Yadav RJ, Pandey A. Utilization of indigenous systems of medicine and homoeopathy in India. Indian J Med Res. 2005;122:137–42. [PubMed] [Google Scholar]
- 25.Kalra S, Kalra B, Agrawal N. Therapeutic patient education: Lessons from Ayurveda: The quadruple of Atreya. Internet J Geriatr Gerontol. 2010;5:10. [Google Scholar]
- 26.Gogtay NJ, Bhatt HA, Dalvi SS, Kshirsagar NA. The use and safety of non-allopathic Indian medicines. Drug Saf. 2002;25:1005–19. doi: 10.2165/00002018-200225140-00003. [DOI] [PubMed] [Google Scholar]
- 27.Indian Council of Medical Research Task Force. Assessment of effects on health due to consumption of bitter bottle gourd (Lagenaria siceraria) juice. Indian J Med Res. 2012;135:49–55. doi: 10.4103/0971-5916.93424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kinmonth AL, Woodcock A, Griffin S, Spiegal N, Campbell MJ. Randomised controlled trial of patient centred care of diabetes in general practice: Impact on current wellbeing and future disease risk. The diabetes care from diagnosis research team. BMJ. 1998;317:1202–8. doi: 10.1136/bmj.317.7167.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.King EB, Schlundt DG, Pichert JW, Kinzer CK, Backer BA. Improving the skills of health professionals in engaging patients in diabetes-related problem solving. J Contin Educ Health Prof. 2002;22:94–102. doi: 10.1002/chp.1340220205. [DOI] [PubMed] [Google Scholar]
- 30.David , Fred R. 4th ed. New York: Macmillan Publishing Company; 1993. Strategic Management. [Google Scholar]
- 31.Kalra S, Kalra B, Batra P. Patient motivation for insulin/injectable therapy: The karnal model. Int J Clin Cases Investig. 2010;1:11–5. [Google Scholar]
- 32.Personal SWOT Analysis. Mind Tools Ltd. 2007-2011. [Last accessed 2013 Apr 22]. Available from: http://www.mindtools.com/pages/article/newTMC_05_1.htm. http://www.mindtools.com/pages/article/worksheets/SWOTAnalysisWorksheet.pdf .
- 33.Mike Dobson and Rachel Coombes. Work Experience Module. Unit 1. Making Sense of Learning through Self-awareness. [Last accessed 2013 Apr 22]. pp. 10–15. Available form: http://www.exeter.ac.uk/fch/work-experience/handbook.pdf .
- 34.SWOT Analysis: Strengths, Weaknesses, Opportunities, and Threats. Renault, Val. Community Assessment, Agenda Setting, and Choice of Broad Strategies. University of Kansas. n.d. English. 2012. [Last accessed 2013 Apr 22]. Available form: http://eclkc.ohs.acf.hhs.gov/hslc/tta-system/operations/mgmtadmin/planning/planning/2SWOTAnalysisS.htm .
- 35.Cavanaugh K, Wallston KA, Gebretsadik T, Shintani A, Huizinga MM, Davis D, et al. Addressing literacy and numeracy to improve diabetes care: Two randomized controlled trials. Diabetes Care. 2009;32:2149–55. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Whelton, Cameron . 7th Ed. New Jersey: Pearson publication; 2007. Developing management skills. [Google Scholar]
- 37.Discover your weaknesses and growth areas with johari window model. [Last accessed 2013 Apr 22]. Available from: http://www.managing-change.net/johari-window-model.html .
- 38.Gautam S. Fourth revolution in psychiatry-Addressing comorbidity with chronic physical disorders. Indian J Psychiatry. 2010;52:213–9. doi: 10.4103/0019-5545.70973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sridhar GR. Psychiatric co-morbidity and diabetes. Indian J Med Res. 2007;125:311–20. [PubMed] [Google Scholar]
- 40.Gerteis M, Edgman-Levitan S, Daley J, Delbanco TL. San Francisco: Calif Jossey-Bass; 1993. Through the Patient's Eyes: Understanding and Promoting Patient-Centered Care. [Google Scholar]
- 41.Picker Principles of Patient Centered Care; Principles of patientcentered care. [Last accessed 2013 Apr 22]. Available form: http://cgp.pickerinstitute.org/?page_id=1319 .
- 42.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycaemia in type 2 diabetes: A patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2012;55:1577–96. doi: 10.1007/s00125-012-2534-0. [DOI] [PubMed] [Google Scholar]
- 43.Washington, DC: National Academies Press; 2001. Committee on Quality of Health-Care in America, Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. [Google Scholar]
- 44.Prueksaritanond S, Tubtimtes S, Asavanich K, Tiewtranon V. Type 2 diabetic patient-centered care. J Med Assoc Thai. 2004;87:345–52. [PubMed] [Google Scholar]
- 45.Kalra S, Baruah M, Ganapathy M, Ganie A, Sahay R, Unnikrishnan A. Patient centred approach to diabetes management: The dawn philosophy. Internet J Fam Pract. 2010;8:10. [Google Scholar]
- 46.Sridhar GR, Madhu K, Veena S, Madhavi RP, Sangeetha B, Rani AS. Living with diabetes: Indian experience. Diab Met Syndr Clin Res Rev. 2007;1:181–7. [Google Scholar]
- 47.Kalra S, Kalra B. A good diabetes counselor ‘Cares’: Soft skills in diabetes counseling. Internet J Health. 2010:11. [Google Scholar]
- 48.Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C, et al. Preferences of patients for patient centred approach to consultation in primary care: Observational study. BMJ. 2001;322:468–72. doi: 10.1136/bmj.322.7284.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Beach MC, Inui T Relationship-Centered Care Research Network. Relationship-centered care. A constructive reframing. J Gen Intern Med. 2006;21:S3–8. doi: 10.1111/j.1525-1497.2006.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Snoek FJ. Barriers to good glycaemic control: The patient's perspective. Int J Obes Relat Metab Disord. 2000;24:S12–20. doi: 10.1038/sj.ijo.0801421. [DOI] [PubMed] [Google Scholar]
- 51.Torres HC, Rozemberg B, Amaral MA, Bodstein RC. Perceptions of primary healthcare professionals towards their role in type 2 diabetes mellitus patient education in Brazil. BMC Public Health. 2010;10:583. doi: 10.1186/1471-2458-10-583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sridhar GR. Dealing with depression in metabolic disorders. Depression in medically-ill patients. In: Desai NG, editor. ECAB Clinical Update: Psychiatry. New Delhi: Elsevier; 2012. pp. 20–36. [Google Scholar]
- 53.American Diabetes Association. Standards of medical care in diabetes – 2012. Diabetes Care. 2012;35:S11–63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Winkley K, Ismail K, Landau S, Eisler I. Psychological interventions to improve glycaemic control in patients with type 1 diabetes: Systematic review and meta-analysis of randomised controlled trials. BMJ. 2006;333:65. doi: 10.1136/bmj.38874.652569.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Alam R, Sturt J, Lall R, Winkley K. An updated meta-analysis to assess the effectiveness of psychological interventions delivered by psychological specialists and generalist clinicians on glycaemic control and on psychological status. Patient Educ Couns. 2009;75:25–36. doi: 10.1016/j.pec.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 56.Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611–20. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian diabetes association 2003 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2003;27(2):S50–2. [Google Scholar]
- 58.London: NICE; 2007. NICE-Depression: Management of depression in primary and secondary care. [Google Scholar]
- 59.Institute for Clinical Systems Improvement (Bloomington, MN, USA) Management of type 2 diabetes mellitus, 2004. [Last accessed 2012 Sep 25]. Available from: http://www.icsi.org/knowledge .
- 60.Herpertz S, Petrak F, Albus C, Hirsch A, Kruse J, Kulzer B. Psychosoziales und diabetes mellitus. In: Deutsche Diabetes Gesellschaft (DDG) und Deutsches Kollegium Psychosomatische Medizin (DKPM), editors. Evidenzbasierte Diabetes-Leitlinie DDG. Diabetes Stoffwechsel. 2003;12:35–58. [Google Scholar]
- 61.Bradley C. The well-being questionnaire. In: Bradley C, editor. Handbook of Psychology and Diabetes. Switzerland: Hardwood Acad; 1994. pp. 89–109. [Google Scholar]
- 62.Daly EJ, Trivedi MH, Raskin P, Grannemann BG. Screening for depression in a diabetic outpatient population. Int J Psychiatry Clin Pract. 2007;11:268–72. doi: 10.1080/13651500701245981. [DOI] [PubMed] [Google Scholar]
- 63.Welch GW, Jacobson AM, Polonsky WH. The Problem Areas in Diabetes Scale. An evaluation of its clinical utility. Diabetes Care. 1997;20:760–6. doi: 10.2337/diacare.20.5.760. [DOI] [PubMed] [Google Scholar]
- 64.Garratt AM, Schmidt L, Fitzpatrick R. Patient-assessed health outcome measures for diabetes: A structured review. Diabet Med. 2002;19:1–11. doi: 10.1046/j.1464-5491.2002.00650.x. [DOI] [PubMed] [Google Scholar]
- 65.Bhaskara M, Manja P, Zeljko M. Organization of diabetes healthcare in Indian rural areas. Diabetologia Croatica. 2002;31:161–71. [Google Scholar]
- 66.Rao PR, Shobhana R, Lavanya A, Padma C, Vijay V, Ramachandran A. Development of a reliable and valid psychosocial measure of self-perception of health in type 2 diabetes. J Assoc Physicians India. 2005;53:689–92. [PubMed] [Google Scholar]
- 67.Delamater AM, Jacobson AM, Anderson B, Cox D, Fisher L, Lustman P, et al. Psychosocial therapies in diabetes: Report of the Psychosocial Therapies Working Group. Diabetes Care. 2001;24:1286–92. doi: 10.2337/diacare.24.7.1286. [DOI] [PubMed] [Google Scholar]
- 68.Beck AT, Steer RA, Garbin MG. Psychometric properties of the beck depression inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 69.Richter P, Werner J, Heerlein A, Kraus A, Sauer H. On the validity of the Beck Depression Inventory. A review. Psychopathology. 1998;31:160–8. doi: 10.1159/000066239. [DOI] [PubMed] [Google Scholar]
- 70.Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. 2006;74:658–70. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- 71.Dobson KS, Hollon SD, Dimidjian S, Schmaling KB, Kohlenberg RJ, Gallop RJ, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the prevention of relapse and recurrence in major depression. J Consult Clin Psychol. 2008;76:468–77. doi: 10.1037/0022-006X.76.3.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lustman PJ, Clouse RE. Treatment of depression in diabetes: Impact on mood and medical outcome. J Psychosom Res. 2002;53:917–24. doi: 10.1016/s0022-3999(02)00416-6. [DOI] [PubMed] [Google Scholar]
- 73.Snoek FJ, Skinner TC. Psychological counselling in problematic diabetes: Does it help? Diabet Med. 2002;19:265–73. doi: 10.1046/j.1464-5491.2002.00678.x. [DOI] [PubMed] [Google Scholar]
- 74.Lustman PJ, Freedland KE, Griffith LS, Clouse RE. Predicting response to cognitive behavior therapy of depression in type 2 diabetes. Gen Hosp Psychiatry. 1998;20:302–6. doi: 10.1016/s0163-8343(98)00039-5. [DOI] [PubMed] [Google Scholar]
- 75.Westbrook D, Kennerley H, Kirk J. London: Sage Publications Ltd; 2008. An Introduction to Cognitive Behaviour Therapy: Skills and Application. [Google Scholar]
- 76.Janice T. The use of cognitive behavioral therapy in diabetes care: A review and case study. J Diabetes Nurs. 2010;14:86–92. [Google Scholar]
- 77.Grant A, Townend M, Mills J, Cockx A. London: Sage Publications Ltd; 2008. Assessment and Case Formulation in Cognitive Behavioural Therapy. [Google Scholar]
- 78.Ismail K, Maissi E, Thomas S, Chalder T, Schmidt U, Bartlett J, et al. A randomised controlled trial of cognitive behaviour therapy and motivational interviewing for people with Type 1 diabetes mellitus with persistent sub-optimal glycaemic control: A Diabetes and Psychological Therapies (ADaPT) study. (iii-iv).Health Technol Assess. 2010;14:1–101. doi: 10.3310/hta14220. [DOI] [PubMed] [Google Scholar]
- 79.Madhu K, Sridhar GR. Stress management in diabetes mellitus. Int J Diabetes Dev Ctries. 2005;25:7–11. [Google Scholar]
- 80.Kalra S. Counselling in male sexual dysfunction: The karnal model. Internet J Fam Pract. 2010:9. [Google Scholar]
- 81.Dellasega C, Añel-Tiangco RM, Gabbay RA. How patients with type 2 diabetes mellitus respond to motivational interviewing. Diabetes Res Clin Pract. 2012;95:37–41. doi: 10.1016/j.diabres.2011.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Smith DE, Heckemeyer CM, Kratt PP, Mason DA. Motivational interviewing to improve adherence to a behavioral weight-control program for older obese women with NIDDM. A pilot study. Diabetes Care. 1997;20:52–4. doi: 10.2337/diacare.20.1.52. [DOI] [PubMed] [Google Scholar]
- 83.Viner RM, Christie D, Taylor V, Hey S. Motivational/solution-focused intervention improves HbA1c in adolescents with Type 1 diabetes: A pilot study. Diabet Med. 2003;20:739–42. doi: 10.1046/j.1464-5491.2003.00995.x. [DOI] [PubMed] [Google Scholar]
- 84.Channon S, Smith VJ, Gregory JW. A pilot study of motivational interviewing in adolescents with diabetes. Arch Dis Child. 2003;88:680–3. doi: 10.1136/adc.88.8.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Channon SJ, Huws-Thomas MV, Rollnick S, Hood K, Cannings-John RL, Rogers C, et al. A multicenter randomized controlled trial of motivational interviewing in teenagers with diabetes. Diabetes Care. 2007;30:1390–5. doi: 10.2337/dc06-2260. [DOI] [PubMed] [Google Scholar]
- 86.Kalra S, Kalra B, Sharma A, Sirka M. Motivational interviewing: The water approach. Endocr J. 2010;57:S391. [Google Scholar]
- 87.Rubak S, Sandbæk A, Lauritzen T, Borch-Johnsen K, Christensen B. Effect of “motivational interviewing” on quality of care measures in screen detected type 2 diabetes patients: A one-year follow-up of an RCT, addition Denmark. Scand J Prim Health Care. 2011;29:92–8. doi: 10.3109/02813432.2011.554271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hill-Briggs F. The Art and Science of Diabetes Self-Management Education: A Desk Reference for Healthcare Professionals. Chicago: American Association of Diabetes Educators; 2006. Problem-solving; pp. 731–59. [Google Scholar]
- 89.Bonnet C, Gagnayre R, d’Ivernois JF. Learning difficulties of diabetic patients: A survey of educators. Patient Educ Couns. 1998;35:139–47. doi: 10.1016/s0738-3991(98)00051-2. [DOI] [PubMed] [Google Scholar]
- 90.Charron-Prochownik D, Zgibor JC, Peyrot M, Peeples M, McWilliams J, Koshinsky J, et al. The Diabetes Self-management Assessment Report Tool (D-SMART): Process evaluation and patient satisfaction. Diabetes Educ. 2007;33:833–8. doi: 10.1177/0145721707307613. [DOI] [PubMed] [Google Scholar]
- 91.Glasgow RE, Toobert DJ, Barrera M, Jr, Strycker LA. Assessment of problem-solving: A key to successful diabetes self-management. J Behav Med. 2004;27:477–90. doi: 10.1023/b:jobm.0000047611.81027.71. [DOI] [PubMed] [Google Scholar]
- 92. [Last accessed 2012 Sep 25]. Available from: http://www.dawnstudy.com/summit2008/downloads/22_Brownson.pdf .
- 93.Hill-Briggs F, Gemmell L. Problem solving in diabetes self-management and control: A systematic review of the literature. Diabetes Educ. 2007;33:1032–50. doi: 10.1177/0145721707308412. [DOI] [PubMed] [Google Scholar]
- 94.Sridhar GR, Madhu K. Stress in the cause and course of diabetes. Int J Diabetes Dev Ctries. 2001;21:112–20. [Google Scholar]
- 95.Lazarus RS, Folkman S. Coping and adaptation. In: Gentry WD, editor. The Handbook of Behavioral Medicine. New York: Guilford; 1984. pp. 282–325. [Google Scholar]
- 96.Azar R, Solomon CR. Coping strategies of parents facing child diabetes mellitus. J Pediatr Nurs. 2001;16:418–28. doi: 10.1053/jpdn.2001.27878. [DOI] [PubMed] [Google Scholar]
- 97.Chiu CJ, Wray LA. Gender differences in functional limitations in adults living with type 2 diabetes: Biobehavioral and psychosocial mediators. Ann Behav Med. 2011;41:71–82. doi: 10.1007/s12160-010-9226-0. [DOI] [PubMed] [Google Scholar]
- 98.Garnefski N, Kraaij V. Cognitive emotion regulation questionnaire: Development of a short 18-item version (CERQ-short) Pers Individ Dif. 2006;41:1045–53. [Google Scholar]
- 99.Yi-Frazier JP, Smith RE, Vitaliano PP, Yi JC, Mai S, Hillman M, et al. A Person-Focused Analysis of Resilience Resources and Coping in Diabetes Patients. Stress Health. 2010;26:51–60. doi: 10.1002/smi.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Viner R, McGrath M, Trudinger P. Family stress and metabolic control in diabetes. Arch Dis Child. 1996;74:418–21. doi: 10.1136/adc.74.5.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chernoff RG, Ireys HT, DeVet KA, Kim YJ. A randomized, controlled trial of a community-based support program for families of children with chronic illness: Pediatric outcomes. Arch Pediatr Adolesc Med. 2002;156:533–9. doi: 10.1001/archpedi.156.6.533. [DOI] [PubMed] [Google Scholar]
- 102.Laffel LM, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr. 2003;142:409–16. doi: 10.1067/mpd.2003.138. [DOI] [PubMed] [Google Scholar]
- 103.Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, et al. Randomized, controlled trial of Behavioral Family Systems Therapy for Diabetes: Maintenance and generalization of effects on parent-adolescent communication. Behav Ther. 2008;39:33–46. doi: 10.1016/j.beth.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 104.Sridhar GR. Gender differences in childhood diabetes. Int J Diabetes Dev Ctries. 1996;16:108–13. [Google Scholar]
- 105.Sridhar GR. Diabetes mellitus in children below the age of five. Indian J Endocrinol Metab. 1997;1:13–5. [Google Scholar]
- 106.Jyotsna VP, Joshi A, Ambekar S, Kumar N, Dhawan A, Sreenivas V. Comprehensive yogic breathing program improves quality of life in patients with diabetes. Indian J Endocrinol Metab. 2012;16:423–8. doi: 10.4103/2230-8210.95692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Unnikrishnan AG, Kalra S, Garg MK. Preventing obesity in India: Weighing the options. Indian J Endocrinol Metab. 2012;16:4–6. doi: 10.4103/2230-8210.91174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Madanmohan, Bhavanani AB, Dayanidy G, Sanjay Z, Basavaraddi IV. Effect of yoga therapy on reaction time, biochemical parameters and wellness score of peri and post-menopausal diabetic patients. Int J Yoga. 2012;5:10–5. doi: 10.4103/0973-6131.91696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kosuri M, Sridhar GR. Yoga practice in diabetes improves physical and psychological outcomes. Metab Syndr Relat Disord. 2009;7:515–7. doi: 10.1089/met.2009.0011. [DOI] [PubMed] [Google Scholar]
- 110.Sahay BK. Role of yoga in diabetes. J Assoc Physicians India. 2007;55:121–6. [PubMed] [Google Scholar]
- 111.Pandey A, Tripathi P, Pandey R, Srivatava R, Goswami S. Alternative therapies useful in the management of diabetes: A systematic review. J Pharm Bioallied Sci. 2011;3:504–12. doi: 10.4103/0975-7406.90103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sharma R, Gupta N, Bijlani RL. Effect of yoga based lifestyle intervention on subjective well-being. Indian J Physiol Pharmacol. 2008;52:123–31. [PubMed] [Google Scholar]
- 113.Murrock CJ, Higgins PA, Killion C. Dance and peer support to improve diabetes outcomes in African American women. Diabetes Educ. 2009;35:995–1003. doi: 10.1177/0145721709343322. [DOI] [PubMed] [Google Scholar]
- 114.Brown BD, Harris KJ, Harris JL, Parker M, Ricci C, Noonan C. Translating the diabetes prevention program for Northern Plains Indian youth through community-based participatory research methods. Diabetes Educ. 2010;36:924–35. doi: 10.1177/0145721710382582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sridhar GR. Contributions of psychosocial and physical factors in diabetes sexual dysfunction. Soc Sci Int. 1992;8:1–4. [Google Scholar]
- 116.Basu A, Ryder RE. New treatment options for erectile dysfunction in patients with diabetes mellitus. Drugs. 2004;64:2667–88. doi: 10.2165/00003495-200464230-00004. [DOI] [PubMed] [Google Scholar]
- 117.Muniyappa R, Norton M, Dunn ME, Banerji MA. Diabetes and female sexual dysfunction: Moving beyond “benign neglect”. Curr Diab Rep. 2005;5:230–6. doi: 10.1007/s11892-005-0014-3. [DOI] [PubMed] [Google Scholar]
- 118.Larrañaga A, Docet MF, García-Mayor RV. Disordered eating behaviors in type 1 diabetic patients. World J Diabetes. 2011;2:189–95. doi: 10.4239/wjd.v2.i11.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Daneman D, Olmsted M, Rydall A, Maharaj S, Rodin G. Eating disorders in young women with type 1 diabetes. Prevalence, problems and prevention. Horm Res. 1998;50:79–86. doi: 10.1159/000053110. [DOI] [PubMed] [Google Scholar]
- 120.Jones JM, Lawson ML, Daneman D, Olmsted MP, Rodin G. Eating disorders in adolescent females with and without type 1 diabetes: Cross sectional study. BMJ. 2000;320:1563–6. [PMC free article] [PubMed] [Google Scholar]
- 121.Neumark-Sztainer D, Patterson J, Mellin A, Ackard DM, Utter J, Story M, et al. Weight control practices and disordered eating behaviors among adolescent females and males with type 1 diabetes: Associations with sociodemographics, weight concerns, familial factors, and metabolic outcomes. Diabetes Care. 2002;25:1289–96. doi: 10.2337/diacare.25.8.1289. [DOI] [PubMed] [Google Scholar]
- 122.Shobhana R, Ramarao P, Shiela P. Psychosocial aspects of dietary non-adherance in diabetes. Int J Diabetes Dev Ctries. 1998;18:75–7. [Google Scholar]
- 123.Sridhar G, Kumar PS, Venkata P, Rao AA, Kishore DV, Madhu K, et al. Built environment factors, psychosocial factors and diabetes mellitus: A South Indian study. Indian J Clin Med. 2010;1:15–22. [Google Scholar]
- 124.Sridhar GR. Eat, drink and live merry? Int J Diabetes Dev Ctries. 2011;31:1–3. [Google Scholar]
- 125.Blanz BJ, Rensch-Riemann BS, Fritz-Sigmund DI, Schmidt MH. IDDM is a risk factor for adolescent psychiatric disorders. Diabetes Care. 1993;16:1579–87. doi: 10.2337/diacare.16.12.1579. [DOI] [PubMed] [Google Scholar]
- 126.Northam EA, Matthews LK, Anderson PJ, Cameron FJ, Werther GA. Psychiatric morbidity and health outcome in Type 1 diabetes – Perspectives from a prospective longitudinal study. Diabet Med. 2005;22:152–7. doi: 10.1111/j.1464-5491.2004.01370.x. [DOI] [PubMed] [Google Scholar]
- 127.Jaser SS, White LE. Coping and resilience in adolescents with type 1 diabetes. Child Care Health Dev. 2011;37:335–42. doi: 10.1111/j.1365-2214.2010.01184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, et al. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 129.Chaudhry R, Mishra P, Mishra J, Parminder S, Mishra BP. Psychiatric morbidity among diabetic patients: A hospital-based study. Ind Psychiatry J. 2010;19:47–9. doi: 10.4103/0972-6748.77637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kovacs M, Goldston D, Obrosky DS, Bonar LK. Psychiatric disorders in youths with IDDM: Rates and risk factors. Diabetes Care. 1997;20:36–44. doi: 10.2337/diacare.20.1.36. [DOI] [PubMed] [Google Scholar]
- 131.Balhara YP. Diabetes and psychiatric disorders. Indian J Endocrinol Metab. 2011;15:274–83. doi: 10.4103/2230-8210.85579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: A meta-analysis. Diabetes Care. 2008;31:2383–90. doi: 10.2337/dc08-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Golden SH. A review of the evidence for a neuroendocrine link between stress, depression and diabetes mellitus. Curr Diabetes Rev. 2007;3:252–9. doi: 10.2174/157339907782330021. [DOI] [PubMed] [Google Scholar]
- 134.Beck AT, Steer RA, Brown GK. SanAntonio, TX: The Psychological Corporation; 1996. Beck Depression Inventory (BDI)-II Manual. [Google Scholar]
- 135.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 136.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kota SK, Jammula S, Kota SK, Meher LK, Modi KD. Necrobiosis lipoidica diabeticorum: A case-based review of literature. Indian J Endocrinol Metab. 2012;16:614–20. doi: 10.4103/2230-8210.98023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Gonzalez JS, Safren SA, Cagliero E, Wexler DJ, Delahanty L, Wittenberg E, et al. Depression, self-care, and medication adherence in type 2 diabetes: Relationships across the full range of symptom severity. Diabetes Care. 2007;30:2222–7. doi: 10.2337/dc07-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Weinger K, Lee J. Psychosocial and psychiatric challenges of diabetes mellitus. Nurs Clin North Am. 2006;41:667–80. doi: 10.1016/j.cnur.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 140.Jacobson AM. The psychological care of patients with insulin-dependent diabetes mellitus. N Engl J Med. 1996;334:1249–53. doi: 10.1056/NEJM199605093341907. [DOI] [PubMed] [Google Scholar]
- 141.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 142.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 143.Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, et al. Assessing psychosocial distress in diabetes: Development of the diabetes distress scale. Diabetes Care. 2005;28:626–31. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- 144.Burroughs TE, Desikan R, Waterman BM, Gilin D, McGill J. Development and validation of the diabetes quality of life brief clinical inventory. Diabetes Spectr. 2004;17:41–9. [Google Scholar]
- 145.Cox DJ, Irvine A, Gonder-Frederick L, Nowacek G, Butterfield J. Fear of hypoglycemia: Quantification, validation, and utilization. Diabetes Care. 1987;10:617–21. doi: 10.2337/diacare.10.5.617. [DOI] [PubMed] [Google Scholar]
- 146.Snoek FJ, Mollema ED, Heine RJ, Bouter LM, van der Ploeg HM. Development and validation of the diabetes fear of injecting and self-testing questionnaire (D-FISQ): First findings. Diabet Med. 1997;14:871–6. doi: 10.1002/(SICI)1096-9136(199710)14:10<871::AID-DIA457>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 147.Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. U.S. Department of Health and Human Services. [Google Scholar]
- 148.Pinquart M, Duberstein PR, Lyness JM. Treatments for later-life depressive conditions: A meta-analytic comparison of pharmacotherapy and psychotherapy. Am J Psychiatry. 2006;163:1493–501. doi: 10.1176/ajp.2006.163.9.1493. [DOI] [PubMed] [Google Scholar]
- 149.Cuijpers P, Dekker J, Hollon SD, Andersson G. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: A meta-analysis. J Clin Psychiatry. 2009;70:1219–29. doi: 10.4088/JCP.09r05021. [DOI] [PubMed] [Google Scholar]
- 150.Rubin RR, Ma Y, Marrero DG, Peyrot M, Barrett-Connor EL, Kahn SE, et al. Elevated depression symptoms, antidepressant medicine use, and risk of developing diabetes during the diabetes prevention program. Diabetes Care. 2008;31:420–6. doi: 10.2337/dc07-1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Rosenzweig S, Reibel DK, Greeson JM, Edman JS, Jasser SA, McMearty KD, et al. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: A pilot study. Altern Ther Health Med. 2007;13:36–8. [PubMed] [Google Scholar]
- 152.Matam P, Kumaraiah V, Munichoodappa C, Kumar KM, Aravind S. Behavioural intervention in the management of compliance in young type-I diabetics. J Assoc Physicians India. 2000;48:967–71. [PubMed] [Google Scholar]
- 153.Finestone DH, Weiner RD. Effects of ECT on diabetes mellitus. An attempt to account for conflicting data. Acta Psychiatr Scand. 1984;70:321–6. doi: 10.1111/j.1600-0447.1984.tb01216.x. [DOI] [PubMed] [Google Scholar]
- 154.Reddy S, Nobler MS. Dangerous hyperglycemia associated with electroconvulsive therapy. Convuls Ther. 1996;12:99–103. [PubMed] [Google Scholar]
- 155.Netzel PJ, Mueller PS, Rummans TA, Rasmussen KG, Pankratz VS, Lohse CM. Safety, efficacy, and effects on glycemic control of electroconvulsive therapy in insulin-requiring type 2 diabetic patients. J ECT. 2002;18:16–21. doi: 10.1097/00124509-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 156.Tiwari SC, Kumar A, Kumar A. Development and standardization of a scale to measure socio-economic status in urban and rural communities in India. Indian J Med Res. 2005;122:309–14. [PubMed] [Google Scholar]
- 157.Tiwari SC, Kumar A. Updation of the scale to measure socio-economic status in urban and rural communities in India. Indian J Med Res. 2012;135:432–4. [PMC free article] [PubMed] [Google Scholar]
- 158.Safraj S, Anish Ts, Vijayakumar K, Kutty VR, Soman CR. Socioeconomic position and prevalence of self-reported diabetes in rural Kerala, India: Results from the PROLIFE study. Asia Pac J Public Health. 2012;24:480–6. doi: 10.1177/1010539510387822. [DOI] [PubMed] [Google Scholar]
- 159.Oladele CR, Barnett E. Racial/Ethnic and social class differences in preventive care practices among persons with diabetes. BMC Public Health. 2006;6:259. doi: 10.1186/1471-2458-6-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bottle A, Millett C, Xie Y, Saxena S, Wachter RM, Majeed A. Quality of primary care and hospital admissions for diabetes mellitus in England. J Ambul Care Manage. 2008;31:226–38. doi: 10.1097/01.JAC.0000324668.83530.6d. [DOI] [PubMed] [Google Scholar]
- 161.Deepa M, Anjana RM, Manjula D, Narayan KM, Mohan V. Convergence of prevalence rates of diabetes and cardiometabolic risk factors in middle and low income groups in urban India: 10-year follow-up of the Chennai Urban Population Study. J Diabetes Sci Technol. 2011;5:918–27. doi: 10.1177/193229681100500415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kumar A, Nagpal J, Bhartia A. Direct cost of ambulatory care of type 2 diabetes in the middle and high income group populace of Delhi: The DEDICOM survey. J Assoc Physicians India. 2008;56:667–74. [PubMed] [Google Scholar]
- 163.National Family Health Survey (NFHS-3), 2005-06. Vol. 2. Mumbai, India: IIPS; 2007. International Institute for Population Sciences (IIPS) and Macro International. [Google Scholar]
- 164.Chesla CA, Fisher L, Mullan JT, Skaff MM, Gardiner P, Chun K, et al. Family and disease management in African-American patients with type 2 diabetes. Diabetes Care. 2004;27:2850–5. doi: 10.2337/diacare.27.12.2850. [DOI] [PubMed] [Google Scholar]
- 165.Wen LK, Parchman ML, Shepherd MD. Family support and diet barriers among older Hispanic adults with type 2 diabetes. Fam Med. 2004;36:423–30. [PubMed] [Google Scholar]
- 166.Gorin A, Phelan S, Tate D, Sherwood N, Jeffery R, Wing R. Involving support partners in obesity treatment. J Consult Clin Psychol. 2005;73:341–3. doi: 10.1037/0022-006X.73.2.341. [DOI] [PubMed] [Google Scholar]
- 167.Kalra B, Kalra S, Kumar A. Social stigma and discrimination: A care crisis for young women with diabetes in India. Diabetes Voice. 2009;54:37–9. [Google Scholar]
- 168.Sridhar GR. Gender differences in childhood diabetes. Int J Diabetes Dev Ctries. 1996;16:108–13. [Google Scholar]
- 169.Veena S, Madhu K, Sridhar GR. Gender difference in coping with type 2 diabetes mellitus. Int J Diabetes Dev Ctries. 2001;21:97–102. [Google Scholar]
- 170.Whittemore R, D›Eramo Melkus G, Grey M. Metabolic control, self-management and psychosocial adjustment in women with type 2 diabetes. J Clin Nurs. 2005;14:195–203. doi: 10.1111/j.1365-2702.2004.00937.x. [DOI] [PubMed] [Google Scholar]
- 171.Vaughn LM, Jacquez F, Baker RC. Cultural health attributions, beliefs, and practices: Effects on healthcare and medical education. Open Med Educ J. 2009;2:64–74. [Google Scholar]
- 172.Osman A, Curzio J. South Asian cultural concepts in diabetes. (30-2).Nurs Times. 2012;108:28. [PubMed] [Google Scholar]
- 173.Ganie MA, Koul S, Razvi HA, Laway BA, Zargar AH. Hyperglycemic emergencies in Indian patients with diabetes mellitus on pilgrimage to Amarnathji yatra. Indian J Endocrinol Metab. 2012;16:S87–90. doi: 10.4103/2230-8210.94267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Jaleel MA, Raza SA, Fathima FN, Jaleel BN. Ramadan and diabetes: As-Saum (The fasting) Indian J Endocrinol Metab. 2011;15:268–73. doi: 10.4103/2230-8210.85578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Zeh P, Sandhu HK, Cannaby AM, Sturt JA. The impact of culturally competent diabetes care interventions for improving diabetes-related outcomes in ethnic minority groups: A systematic review. Diabet Med. 2012;29:1237–52. doi: 10.1111/j.1464-5491.2012.03701.x. [DOI] [PubMed] [Google Scholar]
- 176.Pathan MF, Sahay RK, Zargar AH, Raza SA, Khan AK, Ganie MA, et al. South Asian Consensus Guideline: Use of insulin in diabetes during Ramadan. Indian J Endocrinol Metab. 2012;16:499–502. doi: 10.4103/2230-8210.97992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Shen H, Edwards H, Courtney M, McDowell J, Wu M. Peer-led diabetes self-management programme for community-dwelling older people in China: Study protocol for a quasi-experimental design. J Adv Nurs. 2012;68:2766–77. doi: 10.1111/j.1365-2648.2012.06059.x. [DOI] [PubMed] [Google Scholar]
- 178.Quinn MT, Cook S, Nash K, Chin MH. Addressing religion and spirituality in African Americans with diabetes. (647-8).Diabetes Educ. 2001;27:643–4. doi: 10.1177/014572170102700505. 655. [DOI] [PubMed] [Google Scholar]
- 179.Gore TN, Williams A, Sanderson B. Recipe for health: Impacting diabetes in African Americans through faith-based edcuation. J Christ Nurs. 2012;29:49–53. doi: 10.1097/cnj.0b013e31823a8a77. [DOI] [PubMed] [Google Scholar]
- 180.Murray-Swank A, Goldberg R, Dickerson F, Medoff D, Wohlheiter K, Dixon L. Correlates of religious service attendance and contact with religious leaders among persons with co-occurring serious mental illness and type 2 diabetes. J Nerv Ment Dis. 2007;195:382–8. doi: 10.1097/01.nmd.0000253801.18367.a5. [DOI] [PubMed] [Google Scholar]
- 181.Menon VU, Kumar KV, Gilchrist A, Sugathan TN, Sundaram KR, Nair V, et al. Prevalence of known and undetected diabetes and associated risk factors in central Kerala – ADEPS. Diabetes Res Clin Pract. 2006;74:289–94. doi: 10.1016/j.diabres.2006.03.025. [DOI] [PubMed] [Google Scholar]
- 182.Mohan V, Shanthirani CS, Deepa R. Glucose intolerance (diabetes and IGT) in a selected South Indian population with special reference to family history, obesity and lifestyle factors – The Chennai Urban Population Study (CUPS 14) J Assoc Physicians India. 2003;51:771–7. [PubMed] [Google Scholar]
- 183.Lau SL, Debarm R, Thomas N, Asha HS, Vasan KS, Alex RG, et al. Healthcare planning in north-east India: A survey on diabetes awareness, risk factors and health attitudes in a rural community. J Assoc Physicians India. 2009;57:305–9. [PubMed] [Google Scholar]
- 184.Ramachandran A, Snehalatha C, Baskar AD, Mary S, Kumar CK, Selvam S, et al. Temporal changes in prevalence of diabetes and impaired glucose tolerance associated with lifestyle transition occurring in the rural population in India. Diabetologia. 2004;47:860–5. doi: 10.1007/s00125-004-1387-6. [DOI] [PubMed] [Google Scholar]
- 185.Kohinor MJ, Stronks K, Haafkens JA. Factors affecting the disclosure of diabetes by ethnic minority patients: A qualitative study among Surinamese in the Netherlands. BMC Public Health. 2011;11:399. doi: 10.1186/1471-2458-11-399. [DOI] [PMC free article] [PubMed] [Google Scholar]


