Abstract
Dyslipidemia and its consequences are emerging as epidemics with deleterious consequences on cardiovascular (CV) health. The beneficial effects of omega-3-fatty acids on cardiac and extra cardiac organs have been extensively studied in the last two decades, and continue to show great promise in the primary and secondary prevention of cardiovascular diseases (CVDs). Omega-3-fatty acid supplementation has been proven to have beneficial action on lipid profile, cytokine cascade, oxidant-anti-oxidant balance, parasympathetic and sympathetic tone and nitric oxide synthesis. This review summarizes the current knowledge on the basis of its cardiac and non-cardiac benefits, present results from clinical trials and the recommendations for its use in cardiac diseases and dyslipidemias.
Keywords: Docosahexaenoic acid, eicosapentaenoic acid, omega-3-fatty acids
INTRODUCTION
Dyslipidemia and its metabolic consequences are emerging as epidemics with their deleterious consequences on cardiovascular (CV) health. The beneficial effects of omega 3 fatty acids (Eicosapentaenoic acid and Docosahexaenoic acid) over cardiac and extra cardiac organs havebeen extensivelystudied in thepast two decades, and continue to show great promise in the primary and secondary prevention of CV diseases.
Omega 3 fatty acid supplementation has been proven to have beneficial action on lipid profile, cytokine cascade, oxidant-anti-oxidant balance, parasympathetic and sympathetic tone, and vasodilator Prostaglandin I2 and Nitric Oxide synthesis.
This review summarizes the clinical manifestations of pathogenic adiposity and dyslipidemia on adverse CV outcomes and the role of omega 3 fatty acids in mitigating them. It also aims to cover some of the key epidemiological trials on omega 3 fatty acids that explain its possible mechanism towards causing CV benefits. The dietary recommendations and the therapeutic dosages of fish oils are also discussed.
OMEGA 3 FATTY ACIDS
Omega 3 fatty acids belong to the long chain polyunsaturated fatty acids (FA). The omega 3 fatty acids concerned primarily with CV health are the marine derived Eicosapentaenoic acid (EPA) and Docosahexaenoic acid (DHA) [Figure 1]. Their main sources are fish oils and seafood, but they are actually obtained from the marine microorganisms that are transmitted through the marine food chain. Fish with high omega 3 fatty acid concentrations include fatty fish like albacore, tuna, sardines, salmon, mackerel, and herring. The plant derived omega 3 fatty acid consists of Linolenic acid that can be converted to EPA and DHA. Its role in cardioprotection is less clear than that of DHA and EPA.
Figure 1.
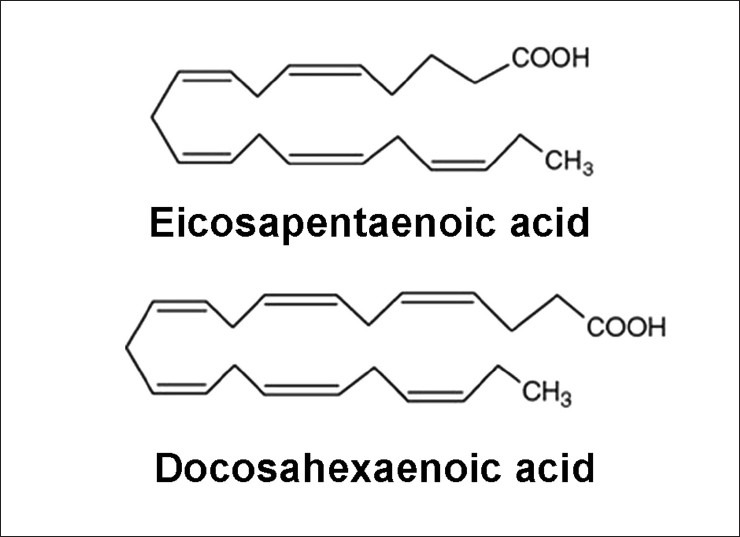
Structure of eicosapentaenoicacid (EPA) and docosahexaenoic acid (DHA)
In addition to dietary sources of omega 3 fatty acids, the capsular form is also available. Prescription omega- 3-acid ethyl esters (P-OM3) is a Food and Drug Administration (FDA) approved prescription formulation of omega 3 fatty acids, to be used as a lipid lowering agent.[1]
LIPID ALTERATIONS IN CV DISEASE
Lipoproteinsare particles in plasma which are made up of lipids and proteins. They serve to transport varying types and amounts of lipids in the circulation, including Triglycerides (TG), that are derived from dietary consumption, intestinal secretion and hepatic production.[2] Low density lipoprotein (LDL), that contains 70% of total plasma cholesterol, is considered the main culprit behind inflammatory processes and early plaque formation, that later ruptures to cause Myocardial infarction (MI) and stroke.[3] High density lipoprotein (HDL) or the good lipoprotein carries only 20% of total plasma cholesterol. These are central mediators of reverse cholesterol transport i.e., transport of cholesterol from peripheral tissues back to the liver where it is excreted via the bile.
A raised TG level is also commonly associated with low HDL and increased levels of small dense LDL, which is regarded atherogenic. Patients with high TG (≥500 mg/dl) are at high risk for developing pancreatitis, caused by the chylomicrons and their remnants that impair pancreatic capillary blood flow causing ischemia induced disruption in acinar structure, along with necrosis, oedema and inflammation characteristic of pancreatitis.
Assman et al., identified that reduction in the LDL-C levels couldlower the incidence of coronary heart disease (CHD) by up to one-third. HDL was also identified as a major factor with low levels associated with increased risk of CHD.[4]
Elevated TG may result from increased synthesis or decreased catabolism of one or more of the lipoprotein classes or from a combination of enhanced synthesis and suppressed catabolism. The two most common genetic disorders causing hypertriglyceridemia are familial combined hyperlipidemia (FCHL) and familial hypertriglyceridemia (FHTG), with their prevalence being between 1 and 3%. In FCHL, the dyslipidemia results due to apolipoprotein defects causing overproduction of TG, very low density lipoproteins (VLDL), VLDL remnants, Intermediate density lipoproteins (IDL) and LDL. In FHTG, due to LPL inhibition, the patient can develop a more severe hypertriglyceridemia along with raised chylomicron and VLDL levels.
Among the exogenous causes of hypertriglyceridemia, LPL deficiency, defect in Apo C-III and dysbetalipoproteinemia constitute the important disorders. Dysbetalipoproteinemia is an unusual disorder with hypertriglyceridemia characterized by xanthomas, cardiovascular diseases (CVDs), and glucose intolerance in adulthood. Little data is available on the effect of omega 3 fish oils in this disorder.
BENEFITS OF OMEGA 3 FATTY ACIDS
Lipid lowering effects of omega 3 fattyacids
Omega 3 fatty acids primarily reduce TG levels in patients of dyslipidemia. Following mechanisms have been proposed by clinical studies, by which omega 3 fatty acids reduce hepatic VLDL-TG synthesis and secretion, and enhance TG clearance from circulating VLDL particles.[5]
EPA and DHA enhance the LPL activity that accelerates metabolism ofVLDL and chylomicrons.[6]
Omega 3 fatty acids cause increased degradation of apo B - 100 and the beta oxidation of existing hepatic FA and further decrease the substrate for TG synthesis.
The increased delivery of omega 3 fatty acidsto the liver may impair hepatic lipogenesisbyinhibiting theenzymatic conversion of acetyl co -A into FFA.[7]
Omega 3 fatty acids can cause impairment of TG synthesis by the inhibition of the enzyme Phosphatidicacid phosphatase/Phosphohydrolase (PAP) that catalyses conversion of Phosphatidic acidinto Diacyl glycerol(DAG) and Diacylglycerolacyl transferase(DGAT), an enzyme that catalyses the final step in the synthesis of TG.
Lipid lowering effects of combination therapy by P-OM3 and statins
The concurrent use of statins and P-OM3 in patients with mixed hyperlipidemia improves the lipid profile to a greater extent than statin therapy alone.[8]
Combination therapy of P-OM3 and statins has been shown to bring about significant improvement in the non-HDL-C and other lipid parameters in patients who had raised levels of the same before initiation of treatment.[9]
P-OM3 treatment for hypertriglyceridemia may cause elevation in the LDL-C levels due to increased conversion of VLDL particles to LDL particles. Co administration of statins may help in mitigating the rise in LDL-C levels by inhibiting cholesterol production and inducing LDL receptor activity.[8]
Comparison of mechanism of action of omega-3 fatty acids and fibric acid derivatives
Fibric acid derivatives are PPAR-α agonists that induce LPL gene, thus suppressing apolipoprotein C111 and thereby causing reduction in TG levels. In hypercholesterolemic patients with TG elevations more than 700 mg/dl, treatment with fibrates may lead to an increase in the LDL-C levels upto 50%, due to increased LPL activity. Hence a combination therapy with statins is preferred.
Omega-3 fatty acids reduce the CV risks as do the fibrates. Even with increased LDL-C, Omega-3 fatty acids reduce the total cholesterol carried by atherogenic lipoproteins, as reflected by decrease in non-HDL-C levels (total cholesterol - HDL-C). The National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) recognizes low HDL-C (<40 mg/dL) and elevated TG (≥150 mg/dL) as markers of increased CVD risk.[10]
Thus the complementary mechanisms of action by these two lipid lowering drugs (statins and omega-3 fatty acids) is a safe and effective way to improve lipid levels and CVprognosis, beyond the benefits provided by statin therapy alone.
Cardiac benefits
Recent studies provide compelling evidence regarding the beneficial effects of omega 3 fatty acids in reducing risk of cardiac death.[11] Omega 3 fatty acids may improve cardiac function by their anti-triglyceridemic, antihypertensive, hemostatic, antiarrhythmic[12,13,14,15,16] and anti-atherogenic effects. They may also confer CV benefits through enrichment of membrane phospholipids,[17] vasodilation, antithrombotic potential[18] and anti-inflammatory endothelial effects.[19] Some of these mechanisms may be mediated by the effects of omega 3 fatty acids on gene transcription.[20,21] Hypertriglyceridemia is a risk factor for atherosclerotic coronary heart disease. Omega-3 fatty acids reduce the synthesis and secretion of very-low-density lipoprotein (VLDL) particles, and increase TG removal from VLDL and chylomicron particles through the up-regulation of enzymes, such as lipoprotein lipase.[1]
Chronic imbalance of the autonomic nervous system, with increase in sympathetic and/or decrease in parasympathetic tone, increases the risk of major CV events and dysrhythmias.[22,23] There is a possible interaction between EPA/DHA supplementation and the increase in cerebral acetylcholine levels that may enhance the parasympathetic tone and increase heart rate variability, an important protective factor that reduces malignant ventricular arrhythmias and sudden cardiac death (SCD) in survivors of MI[24,25] Omega 3 fatty acids were also shown to slower atrial ventricular conduction and substantially lower the likelihood of having a prolonged QT interval. Some studies have shown significant anti-arrhythmic effect in patients of atrial fibrillation who consumed fish oils, however, further studies are still needed on their anti-arrhythmic potential.[23,26] Polyunsaturated FAs suppress congestive heart failure-induced atrial structural remodeling and atrial fibrillation (AF) promotion but do not affect atrial tachycardia-induced electrical remodeling. The beneficial effects of polyunsaturated FAs on structural remodeling, possibly related to prevention of mitogen-activated protein kinase activation, may contribute to their clinical anti-AF potential.[27] In aggregate, these studies suggest that omega 3 fatty acids have benefits in improving autonomic function.
Recent studies suggest that inflammatory mediators such as tumor necrosis factor-α (TNF-α) and interleukins (ILs) seem to be involved in CHD. TNF-αreleased early in the course of acute MI can decrease myocardial contractility in a dose dependent fashion.[28] Omega 3 fatty acids have been shown to inhibit the production of ILs, like IL-6, and TNF-α, both in vitro and in vivo.[29,30,31]
The potential benefits of omega 3 fatty acids are being found in the prevention and treatment of heart failure (HF) by improving its structure and function.[32,33,34,35] EPA and DHA favorably affect cardiac remodeling by the ligand activation of Peroxisome proliferatoractivator receptor-gamma (PPAR-γ) that up-regulates adiponectin (the cardio-protective adipokine), along with the suppression of inflammatory cytokines.[36,37]
Non-cardiacbenefits
There is evidence of the efficacy of omega 3 fatty acidsin the treatment of numerous non-cardiac conditions. The action of EHA and DPA on the parasympathetic tone along with the direct inhibitory effect on TNF-α, IL-1 and IL-2 synthesis may also explain their beneficial action in various inflammatory conditionssuch as ulcerative colitis, Crohn's disease, Rheumatoid arthritis,[38,39,40] systemic lupus erythematosus, septicemia, septic shock and cancer,[41,42] which are associated with excess production of TNF-α. However, these benefits are yet to be proven and further studies are warranted.
When administered to obese patients, EPA has been found to increase the levels of adiponectin, which can reduce inflammation and improve insulin sensitivity[37] in addition to the potential beneficial HF effects discussed earlier.
Effect on hemostatic system
In patients of hypertriglyceridemia, there is increased risk for thrombosis due to enhanced production of plasminogen activator inhibitor-1 that increases factor 7. Omega 3 fatty acids have been found to mitigate this process, thus reducing the chance of thrombosis.
The action of omega 3 fatty acids on membrane phospholipids and cyclooxygenase-lipoxygenase enzyme complex cause reduction in platelet activity. Thus, omega 3 fatty acids may have antiplatelet activity through potential pleotropism.[43]
Endothelial prolife ration and function
Several epidemiologic and animal studies have shown evidence of benefit of omega 3 fatty acids in significantly lowering the levels of atherosclerosis[44] mediated by its anti-inflammatory properties and inhibition of endothelial activation.[45,46] This may be brought about by the action ofEPA and DHA, thatreducesthe adhesion and migration of monocytes and influence the processes involving leukocyte-endothelial cell interactions[45,46]
Vascular smooth muscle cell proliferation plays an important role in the pathogenesis of atherosclerosis and re-stenosis. EPA and DHAhave been found to have a role in inhibition of this smooth muscle cell proliferation.[47]
Another suggested mechanism for the cardioprotective action of EPA is by their action on endothelial cells by correcting imbalance between the endothelium derived factors, as has been demonstrated in animal models.[48]
Benefit in genetic disorders of hypertriglyceridemia
Omega 3 fatty acids may benefit patients of FCHL and FHTG by the enhancement of the LPL activity, thereby reducing the VLDL production and reducing the markedly elevated TG by upto 50%.
Treatment with omega 3 fatty acids in conditions of exogenous hypertriglyceridemia is doubtful, as in them, LPL is either deficient or is ineffective due to defect in Apo/C11.
The benefits of Omega 3 fatty acids have been summarized in Figure 2.
Figure 2.
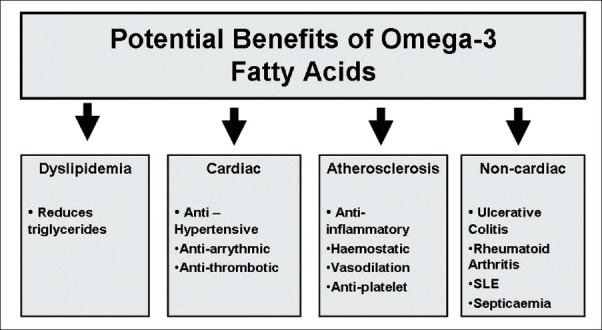
Cardiac and non-cardiac benefits of omega-3-fatty acids
CLINICAL TRIALS ON OMEGA 3 FATTY ACIDS
The most compelling evidence for CV benefits ofomega 3 fatty acidscomes fromthenumerous prospective and retrospective trials conducted worldwide, which, despite sometimes conflicting results, hasshown that a sufficient intake of omega-3 fatty acids can have a positive role in primary and secondary prevention of CVDs.[49]
It is evident that moderate fish oil consumption decreases the risk of major CV events, such as MI, SCD, CHD, AF, and most recently, death in patients with HF.[49,50,51]
The association of fish consumption with reduced risk from all-cause ischemic heart disease and stroke mortality was found in an ecological study byHe etal.[52] Although the first Diet and Re-infarction Trial (DART) hypothesized that omega 3 fatty acids might protect the myocardium against the adverse sequel of acute ischemic stress, it sequel gave conflicting outcomes.[53] Studies have reported that chronic intake of fish or fish oil was associated with a reduction in repeat infarction after MI[54,55] as well as reduction in infarct size as estimated by the frequency of Q wave infarcts and by peak creatine kinase and lactate dehydrogenaseactivities after MI.[54] The most cited, largest, prospective randomized controlled trial (RCT) with P-OM3 is the GruppoItaliano per lo Studio dellaSopravivenzanell’ Infarto Mio CardicoPrevenzione study (GISSI-prevention study)[56] in which 11,324 patients with preexisting CHD on conventional cardiac pharmacotherapy were randomized to either 300 mg of vitamin E, 850 mg of Omega 3 fatty acid ethyl esters (as EPA and DHA), both or neither. After three and a half years of follow-up, the group who were given the Omega/3 fatty acid alone experienced a 15% reduction in the primary end point of death, non-fatal MI and non-fatal stroke. There was 20% reduction in all-cause mortality and a 45% reduction in sudden death, compared with the control group. Vitamin E provided no additional benefit. TG decreased by 4% and LDL cholesterol levels increased by 2.5% after 6 months in the Omega 3 fatty acidtreatment groups compared with controls.
Harris et al.[57] have reviewedtrials that evaluated the risk of CHD events as a function of in vivo levels ofomega 3 purified unsaturated fatty acids (PUFA) and showed that reduction in major CV events correlated inversely with the tissue levels of EPA, and even more sowith DHA.
In the Japan EPA Lipid Intervention Study (JELIS) trial,[50] patientswith hypercholesterolemiawere randomized to statin alone or statin and highly purified EPA 1,800 mg/day. Both treatments lowered LDL-cholesterol by the same amount, yet the combination of EPA plus statin produced a greater reduction in major coronary events, suggesting a mechanism independent of lipid lowering.
However, it should be noted that there areother studies thathave not shown significant benefits of omega 3 fatty acids. For example, a trial by Burr et al.[58] suggested that patients with angina treated with fish oil capsules seem to have a higher risk ofSCD (sudden cardiac death) than untreated control subjects. Risk of cardiac death was found higher among subjects advised to take oily fish than among those not so advised; the adjusted hazard ratio was 1.26 (95% confidence interval 1.00, 1.58; P = 0.047), and even greater for SCD (1.54; 95% CI 1.06, 2.23; P = 0.025). The excess risk was largely located among the subgroup given fish oil capsules. The OMEGAtrial to test the effect of highly purified omega-3 fatty acids on top of modern therapy after MI also showed no benefit of EPA/DHA on any of the primary or secondary end points.[59]
ADVERSE EXPERIENCES ASSOCIATED WITH OMEGA 3 FATTY ACIDS
Some epidemiological studies have raised concern about the adverse effects oftoxic contaminants such as methyl mercury, an environmental contaminant found in certain fish (not in fish oil) that may diminish the health benefits of omega 3 fatty acids.[60] Farm raised salmon and rainbow trout are consideredbetter sources of omega 3 fatty acidsthan their wild counterparts as they contain the same amount of mercury levels and as much or more Omega 3 fatty acids.[61] However, the purification process while manufacturing encapsulated fish oils (like P-OM3) reduce the environmental toxins.[62] P-OM3 carries a pregnancy category C labeling that states that there are no adequate and well controlledstudies regarding its safety in pregnant women.
Another potential danger of omega 3 fatty acids suggested by some reportsis the risk of bleeding due to impairment of platelet aggregation and increased bleeding time.[63] However, several studies have shown no clinically significant increased bleeding with high doses of Omega-3 fatty acids, even when taken with other antiplatelet medications.[64,65]
Studies have reported that Omega 3 fatty acids causea transient increase in glucose levels but no increase infructosamine or Glycosylated hemoglobin.[66]
The use of fish oil capsule therapy involves rancidity related to fish oil instability and susceptibility to oxidation resulting innausea, gastrointestinal upset and ‘fishy burp’. This may impair patient compliance. These can be prevented by its consumption at bed time or with meals, using enteric coated products or keeping fish oil capsules in freezer.
Despite the above potential adverse experiences suggested by various trials, the benefits of Omega 3 fatty acids out weighits perils.
DOSAGE
The American Heart Association (AHA) recommends fish/seafood consumption or fish oil supplementation as a therapeutic strategy to decrease cardiac dysrhythmias, reduce sudden death, decrease the rate of atherosclerosis and to slightly lower the blood pressure.[1]
Omega 3 fatty acid supplements can be taken at any time in full or divided doses with no fear of drug interactions with any other ongoing medications. Depending on the fish oil product available, the correct dosage for TG lowering, primary or secondary prevention can be calculated by adding up the amount of DHA and DPA per capsule anddividing this number into the targeted daily doses.
For primary prevention in those without any CV risks, the target DHA and EPA consumption level is at least 500 mg/d. This can be achieved through two servings of a cold-water seafish, such as salmon, per week.[67] For secondary prevention, the AHA has endorsed the use of Omega 3 fatty acids with the target level 1 gm/day in patients with CHD.[68] Based on the GISSI-HF study results, these recommendations, similar to CHD, should also be extended to patients with HF (e.g., approximately 800-1,000 mg of combined EPA/DHA daily).[51,69] In patients with hypertriglyceridemia, 3-4 gm/d of DHA and EPA is recommended[70,1,71] which lowers the TG levels by 20-50%, and also achieve antiplatelet and anti-inflammatory effects.[72]
Combination therapy of Omega 3 fatty acids with baseline statin therapy further lowers TG by another - upto 29%.[8] Hence, it is effective in improving CV prognosis in patients with hypertriglyceridemia (200-499 mg/dl). The recommendations of Omega 3 fatty acid intake has been summarized in Figure 3.
Figure 3.
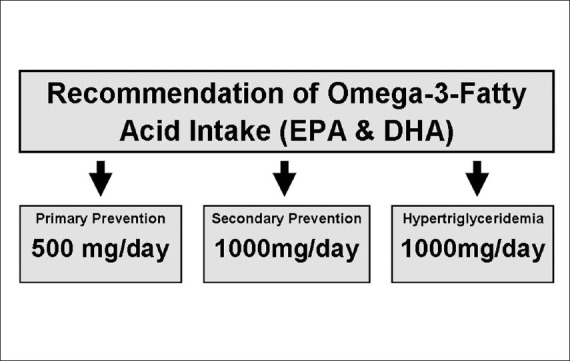
Dosing of omega-3-fatty acids in various disorders
CONCLUSION
In view of the potential benefits of Omega 3 fatty acids on CV health, a dietary approach to increasing Omega 3 fatty acid intake is preferable. For patients with CHD, consultation with their physician is needed to consider Omega 3 fatty acid supplements for CHD risk reduction. Further studies are needed to determine optimal dosing and the relative ratio of DHA and EPA that provides maximal cardioprotection in those at risk of CV disease as well as in the treatment of atherosclerotic, arrhythmic, and primary myocardial disorders.[73]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Bays HE, Tighe AP, Sadovsky R, Davidson MH. Prescription omega-3 fatty acids and their lipid effects: Physiologic mechanisms of action and clinical implications. Expert Rev Cardiovasc Ther. 2008;6:391–409. doi: 10.1586/14779072.6.3.391. [DOI] [PubMed] [Google Scholar]
- 2.Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ. Lipids, sterols and their metabolites. In: Shils ME, Shike M, Ross AC, editors. Modern Nutrition in Health and Disease. 10th ed. Philadelphia: Lippincott Williams and Wilkins; 2007. pp. 99–103. [Google Scholar]
- 3.W van Lammeren G, L Moll F, Borst GJ, de Kleijn DP, PM de Vries JP, Pasterkamp G. Atherosclerotic plaque biomarkers: Beyond the horizon of the vulnerable plaque. Curr Cardiol Rev. 2011;7:22–7. doi: 10.2174/157340311795677680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Assmann G, Gotto AM., Jr HDL cholesterol and protective factors in atherosclerosis. Circulation. 2004;109:III8–14. doi: 10.1161/01.CIR.0000131512.50667.46. [DOI] [PubMed] [Google Scholar]
- 5.Harris WS, Miller M, Tighe AP, Davidson MH, Schaefer EJ. Omega-3 fatty acids and coronary heart disease risk: Clinical and mechanistic perspectives. Atherosclerosis. 2008;197:12–24. doi: 10.1016/j.atherosclerosis.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Weitz D, Weintraub H, Fisher E, Schwartzbard AZ. Fish oil for the treatment of cardiovascular disease. Cardiol Rev. 2010;18:258–63. doi: 10.1097/CRD.0b013e3181ea0de0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris WS, Bulchandani D. Why do omega-3 fatty acids lower serum triglycerides? Curr Opin Lipidol. 2006;17:387–93. doi: 10.1097/01.mol.0000236363.63840.16. [DOI] [PubMed] [Google Scholar]
- 8.Davidson MH, Stein EA, Bays HE, Maki KC, Doyle RT, Shalwitz RA, et al. Efficacy and tolerability of adding prescription omega-3 fatty acids 4 g/d to simvastatin 40 mg/d in hypertriglyceridemic patients: An 8-week, randomized, double-blind, placebo-controlled study. Clin Ther. 2007;29:1354–67. doi: 10.1016/j.clinthera.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 9.Bays HE, McKenney J, Maki KC, Doyle RT, Carter RN, Stein E. Effects of prescription omega-3-acid ethyl esters on non-high-density lipoprotein cholesterol when co-administered with escalating doses of atorvastatin. Mayo Clin Proc. 2010;85:122–8. doi: 10.4065/mcp.2009.0397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farnier M. Update on the clinical utility of fenofibrate in mixed dyslipidemias: Mechanisms of action and rational prescribing. Vasc Health Risk Manag. 2008;4:991–1000. doi: 10.2147/vhrm.s3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mozaffarian D, Wu JH. Omega-3 fatty acids and cardiovascular disease: Effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol. 2011;58:2047–67. doi: 10.1016/j.jacc.2011.06.063. [DOI] [PubMed] [Google Scholar]
- 12.deLeiris J, de Lorgeril M, Boucher F. Fish oil and heart health. J Cardiovasc Pharmacol. 2009;54:378–384. doi: 10.1097/FJC.0b013e3181af6c56. [DOI] [PubMed] [Google Scholar]
- 13.Saremi A, Arora R. The utility of omega-3 fatty acids in cardiovascular disease. Am J Ther. 2009;16:421–36. doi: 10.1097/MJT.0b013e3180a5f0bb. [DOI] [PubMed] [Google Scholar]
- 14.vonSchacky C. Omega-3 fatty acids: Antiarrhythmic, proarrhythmic or both? Curr Opin Clin Nutr Metab Care. 2008;11:94–9. doi: 10.1097/MCO.0b013e3282f44bdf. [DOI] [PubMed] [Google Scholar]
- 15.Kromhout D, Yasuda S, Geleijnse JM, Shimokawa H. Fish oil and omega-3 fatty acids in cardiovascular disease: Do they really work? Eur Heart J. 2012;33:436–43. doi: 10.1093/eurheartj/ehr362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Minno MN, Tremoli E, Tufano A, Russolillo A, Lupoli R, Di Minno G. Exploring newer cardioprotective strategies: ω-3 fatty acids in perspective. Thromb Haemost. 2010;104:664–80. doi: 10.1160/TH10-01-0008. [DOI] [PubMed] [Google Scholar]
- 17.Harris WS. Omega-3 fatty acids and cardiovascular disease: A case for omega-3 index as a new risk factor. Pharmacol Res. 2007;55:217–23. doi: 10.1016/j.phrs.2007.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Din JN, Harding SA, Valerio CJ, Sarma J, Lyall K, Riemersma RA, et al. Dietary intervention with oil rich fish reduces platelet-monocyte aggregation in man. Atherosclerosis. 2008;197:290–6. doi: 10.1016/j.atherosclerosis.2007.04.047. [DOI] [PubMed] [Google Scholar]
- 19.Pauwels EK, Kostkiewicz M. Fatty acid facts, Part III: Cardiovascular disease, or, a fish diet is not fishy. Drug News Perspect. 2008;21:552–61. doi: 10.1358/dnp.2008.21.10.1314058. [DOI] [PubMed] [Google Scholar]
- 20.Calder PC. Omega-3 fatty acids and inflammatory processes. Nutrients. 2010;2:355–74. doi: 10.3390/nu2030355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Calder PC. Fatty acids and inflammation: The cutting edge between food and pharma. Eur J Pharmacol. 2011;668:S50–8. doi: 10.1016/j.ejphar.2011.05.085. [DOI] [PubMed] [Google Scholar]
- 22.Lee JH, O’Keefe JH, Lavie CJ, Marchioli R, Harris WS. Omega-3 fatty acids for cardioprotection. Mayo Clin Proc. 2008;83:324–32. doi: 10.4065/83.3.324. [DOI] [PubMed] [Google Scholar]
- 23.Anand RG, Alkadri M, Lavie CJ, Milani RV. The role of fish oil in arrhythmia prevention. J Cardiopulm Rehabil Prev. 2008;28:92–8. doi: 10.1097/01.HCR.0000314202.09676.f0. [DOI] [PubMed] [Google Scholar]
- 24.Papazafiropoulou AK, Kardara MS, Pappas SI. Pleiotropic effects of omega-3 fatty acids. Recent Pat Endocr Metab Immune Drug Discov. 2012;6:40–6. doi: 10.2174/187221412799015254. [DOI] [PubMed] [Google Scholar]
- 25.O’Keefe JH, Jr, Abuissa H, Sastre A, Steinhaus DM, Harris WS. Effects of omega-3 fatty acids on resting heart rate, heart rate recovery after exercise, and heart rate variability in men with healed myocardial infarctions and depressed ejection fractions. Am J Cardiol. 2006;97:1127–30. doi: 10.1016/j.amjcard.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 26.Gronroos NN, Alonso A. Diet and risk of atrial fibrillation-epidemiologic and clinical evidence - Circ J. 2010;74:2029–38. doi: 10.1253/circj.cj-10-0820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sakabe M, Shiroshita-Takeshita A, Maguy A, Dumesnil C, Nigham A, Leung TK, et al. Arrhythmia/electrophysiology-omega 3 polyunsaturated fatty acids prevent atrial fibrillation associated with heart failure but not atrial tachycardia remodelling. Circulation. 2007;116:2101–9. doi: 10.1161/CIRCULATIONAHA.107.704759. [DOI] [PubMed] [Google Scholar]
- 28.Xiong J, Xue FS, Yuan YJ, Wang Q, Liao X, Wang WL. Cholinergic anti-inflammatory pathway: A possible approach to protect against myocardial ischemia reperfusion injury. Chin Med J (Engl) 2010;123:2720–6. [PubMed] [Google Scholar]
- 29.Gottrand F. Long-chain polyunsaturated fatty acids influence the immune system of infants. J Nutr. 2008;138:1807S–1812S. doi: 10.1093/jn/138.9.1807S. [DOI] [PubMed] [Google Scholar]
- 30.Kiecolt-Glaser JK, Belury MA, Andridge R, Malarkey WB, Hwang BS, Glaser R. Omega-3 supplementation lowers inflammation in healthy middle-aged and older adults: A randomized controlled trial. Brain Behav Immun. 2012;26:988–95. doi: 10.1016/j.bbi.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Han YY, Lai SL, Ko WJ, Chou CH, Lai HS. Effects of fish oil on inflammatory modulation in surgical intensive care unit patients. Nutr Clin Pract. 2012;27:91–8. doi: 10.1177/0884533611429796. [DOI] [PubMed] [Google Scholar]
- 32.Shibata R, Sato K, Pimentel DR, Takemura Y, Kihara S, Ohashi K, et al. Adiponectin protects against myocardial ischemia-reperfusion injury through AMPK- and COX-2-dependent mechanisms. Nat Med. 2005;11:1096–103. doi: 10.1038/nm1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ouchi N, Walsh K. Adiponectin as an anti-inflammatory factor. Clin Chim Acta. 2007;380:24–30. doi: 10.1016/j.cca.2007.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamagishi K, Nettleton JA, Folsom AR ARIC Study Investigators. Plasma fatty acid composition and incident heart failure in middle-aged adults: The Atherosclerosis Risk in Communities (ARIC) Study. Am Heart J. 2008;156:965–74. doi: 10.1016/j.ahj.2008.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamagishi K, Iso H, Date C, Fukui M, Wakai K, Kikuchi S, et al. Fish, omega-3 polyunsaturated fatty acids, and mortality from cardiovascular diseases in a nationwide community-based cohort of Japanese men and women the JACC (Japan Collaborative Cohort Study for Evaluation of Cancer Risk) Study. J Am Coll Cardiol. 2008;52:988–96. doi: 10.1016/j.jacc.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 36.Neschen S, Morino K, Rossbacher JC, Pongratz RL, Cline GW, Sono S, et al. Fish oil regulates adiponectin secretion by a peroxisome proliferator-activated receptor-gamma-dependent mechanism in mice. Diabetes. 2006;55:924–8. doi: 10.2337/diabetes.55.04.06.db05-0985. [DOI] [PubMed] [Google Scholar]
- 37.Itoh M, Suganami T, Satoh N, Tanimoto-Koyama K, Yuan X, Tanaka M, et al. Increased adiponectin secretion by highly purified eicosapentaenoic acid in rodent models of obesity and human obese subjects. Arterioscler Thromb Vasc Biol. 2007;27:1918–25. doi: 10.1161/ATVBAHA.106.136853. [DOI] [PubMed] [Google Scholar]
- 38.Papadia C, Coruzzi A, Montana C, Di Mario F, Franzè A, Forbes A. Omega-3 fatty acids in the maintenance of ulcerative colitis. JRSM Short Rep. 2010;1:15. doi: 10.1258/shorts.2010.010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wiese DM, Lashner BA, Lerner E, DeMichele SJ, Seidner DL. The effects of an oral supplement enriched with fish oil, prebiotics, and antioxidants on nutrition status in Crohn's disease patients. Nutr Clin Pract. 2011;26:463–73. doi: 10.1177/0884533611413778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Caughey GE, James MJ, Proudman SM, Cleland LG. Fish oil supplementation increases the cyclooxygenase inhibitory activity of paracetamol in rheumatoid arthritis patients. Complement Ther Med. 2010;18:171–4. doi: 10.1016/j.ctim.2010.05.032. [DOI] [PubMed] [Google Scholar]
- 41.Manson JE, Bassuk SS, Lee IM, Cook NR, Albert MA, Gordon D, et al. The VITamin D and OmegA-3 TriaL (VITAL): Rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemp Clin Trials. 2012;33:159–71. doi: 10.1016/j.cct.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Terry PD, Terry JB, Rohan TE. Long-chain (n-3) fatty acid intake and risk of cancers of the breast and the prostate: Recent epidemiological studies, biological mechanisms, and directions for future research. J Nutr. 2004;134:3412S–3420S. doi: 10.1093/jn/134.12.3412S. [DOI] [PubMed] [Google Scholar]
- 43.Serebruany VL, Miller M, Pokov AN, Lynch D, Jensen JK, Hallén J, et al. Early impact of prescription Omega-3 fatty acids on platelet biomarkers in patients with coronary artery disease and hypertriglyceridemia. Cardiology. 2011;118:187–94. doi: 10.1159/000329300. [DOI] [PubMed] [Google Scholar]
- 44.Sekikawa A, Curb JD, Ueshima H, El-Saed A, Kadowaki T, Abbott RD, et al. Marine-derived n-3 fatty acids and atherosclerosis in Japanese, Japanese-American, and white men: A cross-sectional study. J Am Coll Cardiol. 2008;52:417–24. doi: 10.1016/j.jacc.2008.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Singh TU, Kathirvel K, Choudhury S, Garg SK, Mishra SK. Eicosapentaenoic acid-induced endothelium-dependent and -independent relaxation of sheep pulmonary artery. Eur J Pharmacol. 2010;636:108–13. doi: 10.1016/j.ejphar.2010.02.041. [DOI] [PubMed] [Google Scholar]
- 46.Nowak JZ. [Anti-inflammatory pro-resolving derivatives of omega-3 and omega-6 polyunsaturated fatty acids] Postepy Hig Med Dosw (Online) 2010;64:115–32. [PubMed] [Google Scholar]
- 47.Sudheendran S, Chang CC, Deckelbaum RJ. N-3 vs. saturated fatty acids: Effects on the arterial wall. Prostaglandins Leukot Essent Fatty Acids. 2010;82:205–9. doi: 10.1016/j.plefa.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Matsumoto T, Nakayama N, Ishida K, Kobayashi T, Kamata K. Eicosapentaenoic acid improves imbalance between vasodilator and vasoconstrictor actions of endothelium-derived factors in mesenteric arteries from rats at chronic stage of type 2 diabetes. J Pharmacol Exp Ther. 2009;329:324–34. doi: 10.1124/jpet.108.148718. [DOI] [PubMed] [Google Scholar]
- 49.Bausano G. [Heart failure and mortality: Polyunsaturated fatty acids and the relevance of evidence] Recenti Prog Med. 2011;102:33–42. [PubMed] [Google Scholar]
- 50.Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): A randomised open-label, blinded endpoint analysis. Lancet. 2007;369:1090–8. doi: 10.1016/S0140-6736(07)60527-3. [DOI] [PubMed] [Google Scholar]
- 51.Investigators. Gissi HF, Tavazzi L, Maggioni AP, Marchioli R, Barlera S, Franzosi MG, et al. Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure (the GISSI-HF trial): A randomised, double-blind, placebo-controlled trial. Lancet. 2008;372:1223–30. doi: 10.1016/S0140-6736(08)61239-8. [DOI] [PubMed] [Google Scholar]
- 52.He K, Song Y, Daviglus ML, Liu K, Van Horn L, Dyer AR, et al. Accumulated evidence on fish consumption and coronary heart disease mortality: A meta-analysis of cohort studies. Circulation. 2004;109:2705–11. doi: 10.1161/01.CIR.0000132503.19410.6B. [DOI] [PubMed] [Google Scholar]
- 53.Burr ML. Secondary prevention of CHD in UK men: The Diet and Reinfarction Trial and its sequel. Proc Nutr Soc. 2007;66:9–15. doi: 10.1017/S0029665107005241. [DOI] [PubMed] [Google Scholar]
- 54.Landmark K, Abdelnoor M, Kilhovd B, Dørum HP. Eating fish may reduce infarct size and the occurrence of Q wave infarcts. Eur J Clin Nutr. 1998;52:40–4. doi: 10.1038/sj.ejcn.1600510. [DOI] [PubMed] [Google Scholar]
- 55.Benedetto U, Melina G, di Bartolomeo R, Angeloni E, Sansone D, Falaschi G, et al. n-3 polyunsaturated fatty acids after coronary artery bypass grafting. Ann Thorac Surg. 2011;91:1169–75. doi: 10.1016/j.athoracsur.2010.11.068. [DOI] [PubMed] [Google Scholar]
- 56.Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: Results of the GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico. Lancet. 1999;7(354):447–55. [PubMed] [Google Scholar]
- 57.Harris WS, Poston WC, Haddock CK. Tissue n-3 and n-6 fatty acids and risk for coronary heart disease events. Atherosclerosis. 2007;193:1–10. doi: 10.1016/j.atherosclerosis.2007.03.018. [DOI] [PubMed] [Google Scholar]
- 58.Burr ML, Ashfield-Watt PA, Dunstan FD, Fehily AM, Breay P, Ashton T, et al. Lack of benefit of dietary advice to men with angina: Results of a controlled trial. Eur J Clin Nutr. 2003;57:193–200. doi: 10.1038/sj.ejcn.1601539. [DOI] [PubMed] [Google Scholar]
- 59.Rauch B, Schiele R, Schneider S, Diller F, Victor N, Gohlke H, et al. OMEGA, a randomized, placebo-controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction. Circulation. 2010;122:2152–9. doi: 10.1161/CIRCULATIONAHA.110.948562. [DOI] [PubMed] [Google Scholar]
- 60.Smith KM, Barraj LM, Kantor M, Sahyoun NR. Relationship between fish intake, n-3 fatty acids, mercury and risk markers of CHD (National Health and Nutrition Examination Survey 1999-2002) Public Health Nutr. 2009;12:1261–9. doi: 10.1017/S1368980008003844. [DOI] [PubMed] [Google Scholar]
- 61.Foran JA, Hites RA, Carpenter DO, Hamilton MC, Mathews-Amos A, Schwager SJ. A survey of metals in tissues of farmed Atlantic and wild Pacific salmon. Environ Toxicol Chem. 2004;23:2108–10. doi: 10.1897/04-72. [DOI] [PubMed] [Google Scholar]
- 62.Bays HE. Safety considerations with omega-3 fatty acid therapy. Am J Cardiol. 2007;99:35C–43C. doi: 10.1016/j.amjcard.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 63.Vanschoonbeek K, Feijge MA, Paquay M, Rosing J, Saris W, Kluft C, et al. Variable hypocoagulant effect of fish oil intake in humans: Modulation of fibrinogen level and thrombin generation. Arterioscler Thromb Vasc Biol. 2004;24:1734–40. doi: 10.1161/01.ATV.0000137119.28893.0b. [DOI] [PubMed] [Google Scholar]
- 64.Harris WS. Expert opinion: Omega-3 fatty acids and bleeding-cause for concern? Am J Cardiol. 2007;99:44C–46C. doi: 10.1016/j.amjcard.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 65.Watson PD, Joy PS, Nkonde C, Hessen SE, Karalis DG. Comparison of bleeding complications with omega-3 fatty acids+aspirin+clopidogrel–versus–aspirin+clopidogrel in patients with cardiovascular disease. Am J Cardiol. 2009;104:1052–4. doi: 10.1016/j.amjcard.2009.05.055. [DOI] [PubMed] [Google Scholar]
- 66.Bays H, Stein EA. Pharmacotherapy for dyslipidaemia-current therapies and future agents. Expert Opin Pharmacother. 2003;4:1901–38. doi: 10.1517/14656566.4.11.1901. [DOI] [PubMed] [Google Scholar]
- 67.Harris WS, Kris-Etherton PM, Harris KA. Intakes of long-chain omega-3 fatty acid associated with reduced risk for death from coronary heart disease in healthy adults. Curr Atheroscler Rep. 2008;10:503–9. doi: 10.1007/s11883-008-0078-z. [DOI] [PubMed] [Google Scholar]
- 68.Kris-Etherton PM, Harris WS, Appel LJ AHA Nutrition Committee. American Heart Association. Omega-3 fatty acids and cardiovascular disease: New recommendations from the American Heart Association. Arterioscler Thromb Vasc Biol. 2003;23:151–2. doi: 10.1161/01.atv.0000057393.97337.ae. [DOI] [PubMed] [Google Scholar]
- 69.Fonarow GC. Statins and n-3 fatty acid supplementation in heart failure. Lancet. 2008;372:1195–6. doi: 10.1016/S0140-6736(08)61241-6. [DOI] [PubMed] [Google Scholar]
- 70.Bays H. Rationale for prescription omega-3-acid ethyl ester therapy for hypertriglyceridemia: A primer for clinicians. Drugs Today (Barc) 2008;44:205–46. doi: 10.1358/dot.2008.44.3.1166387. [DOI] [PubMed] [Google Scholar]
- 71.Harris WS, Jacobson TA. Omega-3 fatty acids. In: Ballantyne CM, editor. Clinical lipidology: A companion to braunwald's heart disease. Philadelphia, PA: Saunders, an imprint of Elsevier Inc; 2009. pp. 326–38. [Google Scholar]
- 72.Marchioli R, Barzi F, Bomba E, Chieffo C, Di Gregorio D, Di Mascio R, et al. Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: Time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenzanell’Infarto Miocardico (GISSI)-Prevenzione. Circulation. 2002;105:1897–903. doi: 10.1161/01.cir.0000014682.14181.f2. [DOI] [PubMed] [Google Scholar]
- 73.Lavie CJ, Milani RV, Mehra MR, Ventura HO. Omega-3 polyunsaturated fatty acids and cardiovascular diseases. J Am Coll Cardiol. 2009;54:585–94. doi: 10.1016/j.jacc.2009.02.084. [DOI] [PubMed] [Google Scholar]


