Abstract
Health literacy (HL) affects adult asthma management, yet less is known about how parent HL affects child asthma care.
Objective
To examine associations between parent HL and measures related to child asthma.
Methods
Parents of 499 school-age urban children with persistent asthma in Rochester, New York completed home interviews. Measures: The Rapid Estimate of Adult Literacy in Medicine for parent HL; NHLBI criteria for asthma severity, and validated measures of asthma knowledge, beliefs, and experiences. Analyses: Bivariate and multivariate analyses of associations between parent HL measures related to child asthma.
Results
Response rate: 72%, mean child age: 7.0 years. Thirty-two percent had a Hispanic parent; 88% had public insurance. Thirty-three percent had a parent with limited HL. Low parent HL was independently associated with greater parent worry parent perception of greater asthma burden, and lower parent-reported quality of life. Measures of health care use (e.g., emergency care, preventive medicines) were not associated with parent HL.
Conclusions
Parents with limited HL worried more and perceived greater overall burden from the child’s asthma, even though reported health care use did not vary.
Practice Implications
Improved parent understanding and provider-parent communication about child asthma could reduce parent-perceived asthma burden, alleviate parent worry, and improve parent quality of life.
Keywords: Health Literacy, asthma, asthma care, child health, child asthma, health behavior, health beliefs, provider-patient communication, pediatric care, medical care, REALM, poverty, low-income, PACQOL, asthma burden, urban children
1. Introduction
Health literacy (HL) is “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [1]. Inadequate health literacy limits individuals’ abilities to access and pay for medical care; understand health care advice; weigh the risks and benefits of health decisions; follow recommendations for treatment; use medicines safely and correctly; and understand rights and responsibilities in health care [1]. Approximately half of US and Canadian adults have literacy problems that could interfere with their health and medical care [2].
Limited HL interferes with adults’ understanding, participation in treatment decisions, and self-management of asthma [3]. In addition, HL level can predict adults’ ability to acquire new asthma self-management skills such as symptom awareness and management and medication use [4]. There is less conclusive evidence to link parent or caregiver HL with child health care [5].
Studies of children can involve parents or ‘caregivers’ or both. We use each of these terms in the way they were used in the works we cite. Thus, when we refer to others’ work, we use the terms ‘caregiver’ or “caregivers and parents’, consistent with the terms used by the authors. When describing the current project, we use the term ‘parent’.
Low maternal literacy has been linked with poorer birth outcomes, and maternal literacy has been associated with health knowledge, behavior, and use of pediatric care [6]. Links between caregiver or parent HL and child health care have been found in small studies of children who have diabetes [7] or asthma [8], yet a study of parent HL and more general child health care over a one-year period did not find similar links [6]. Limited caregiver HL can also interfere with correct dosing and use of medicines in children [9]. A study conducted in 13 countries examined associations between parent education and child respiratory health found no links between parent literacy and prevalence of physician-diagnosed asthma among children, yet did find independent associations between parent education and overall child health [10].
Child asthma is prevalent in both developed and developing nations [], and is one of the most common chronic illnesses among adults and children in North America [3,]. There are racial and socioeconomic disparities in asthma prevalence and morbidity that disproportionately affect low-income, urban, minority children [11]. Measures of adult HL demonstrate similar racial and socioeconomic disparities [1], with a disproportionate prevalence of HL problems among low-income [13] and minority adults [14]. It is therefore important to examine parent HL and child asthma care where these disparities are likely to intersect: among low-income urban schoolchildren.
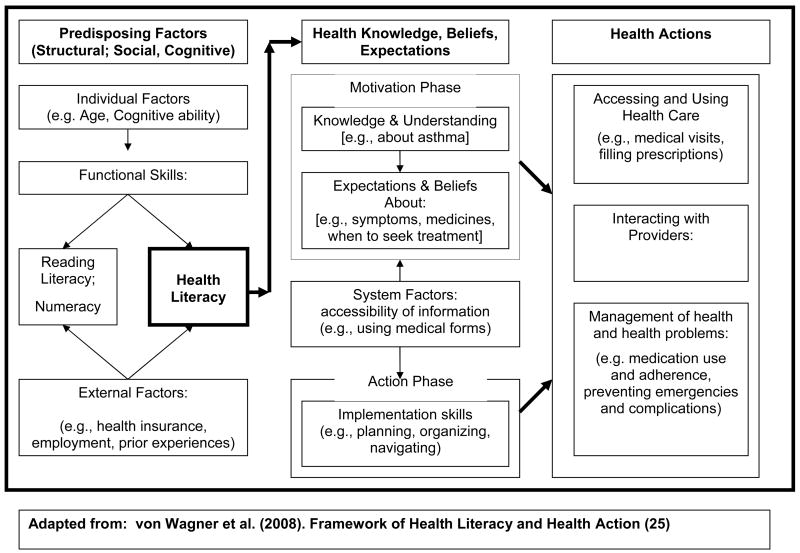
1.1 Conceptual Framework (Figure One)
Figure One.
Conceptual Framework: The Role of Parent Health Literacy for Child Asthma
We utilized the framework of health literacy and health action developed by von Wagner and colleagues [15]. This framework examines determinants of health actions in three domains, categorized by Paasche-Orlow and Wolf as: 1) systems access and use, 2) provider-patient interface, and 3) disease management [16].
Parents with limited HL may lack the context – comprised of von Wagner’s predisposing structural and sociocognitive determinants -- to manage and understand new information. In turn, this lack of context could affect parents: 1) knowledge, beliefs and expectations about the child’s asthma (motivational factors); 2) understanding of available services and information (health system factors); and 3) behavior specific to the child’s asthma (implementation and action factors) [15]. We therefore examined cross-sectional associations between parent HL and selected structural and sociocognitive determinants of health action and selected health actions and outcomes related to the child’s asthma.
1.2. Objectives and Hypotheses
Our objectives were to: 1) measure health literacy among parents of low-income urban children who have significant asthma, and 2) examine associations between parent HL and child asthma care. We hypothesized that children of parents with limited HL would have: 1) less use of preventive medications, 2) greater use of acute care (emergency or inpatient), 3) greater unmet need for care, and greater asthma morbidity compared to parents with adequate HL. We also hypothesized that parents with limited HL would: 1) rate the child’s health less favorably, 2) report more worry and concern about the child’s asthma, and 3) report poorer overall parent quality of life.
2. Methods
2.1 Setting
Our setting was the Rochester City School District (RCSD) in the City of Rochester, New York. Rochester is a medium-sized city where over 40% of children live in poverty (11th highest in the United States) --more than double the rate for all of New York State []. The Rochester City School district serves approximately 37,000 pupils K-12 and 2,300 pre-K students. Most students are from minority and low-income families, and 88% receive free or reduced-price lunches, which require an income below 130% (free) or between 130–185% (reduced) of the Federal Poverty Level (FPL) [].
2.2 Sample and Data Collection
Our sample frame included children who began the school year in RCSD elementary schools in the fall of 2006, 2007, and 2008. We performed sampling via health forms that are completed by parents at the beginning of each school year. We contacted parents of children who were reported to have asthma, performed symptom screening for asthma severity, and invited parents of children who had persistent asthma to participate in an asthma program. A total of 530 children were enrolled. We excluded 15 children for whom parent health literacy data were missing and 16 children whose parent conducted the interview in Spanish (the REALM is an English-only tool and not predictive of Spanish-language communication).
Our subjects were 499 children, ages 3–10 years (mean age 7 years), who had persistent asthma per criteria of the National Heart Lung and Blood Institute (NHLBI) [17]. Data were collected via school health forms, telephone screening interview, and in-person interviews during home visits. The University of Rochester Institutional Review Board approved the study protocol, and informed consent was obtained from all caregivers as well as assent from children 7 years of age and older. We conducted cross-sectional analyses of baseline data that were collected prior to initiation of the asthma program.
2.3. Measures
Our independent measures included parent: health literacy, employment status, race and ethnicity. We measured race [White, Black, Alaska Native/Pacific Islander, Asian, Other] and ethnicity [Hispanic or non-Hispanic] consistent with Federal requirements]. We used the Rapid Estimate of Adult Literacy in Medicine (REALM) to measure parent health literacy. The REALM is a 66-item word recognition and pronunciation scale that takes approximately 2–3 minutes to complete [18]. Consistent with prior research, we considered a reading level below 9th grade as limited HL [8].
Additional independent measures included child health insurance (private, public, none) and age (in years). We used sampling methods and income proxies instead of measuring income directly. We made this choice for several reasons. Our primary motive was to preserve trust with participants in our community-based trial. Although data for the current study come from baseline assessments, participation in the full project involves several lengthy in-home visits and a lifestyle intervention, both of which require high levels of trust. Because direct questions about income can threaten this level of trust, we asked about health insurance and employment as income proxies rather than asking about income itself. These proxy measures can be multicollinear with income itself and thus cannot be used together in multivariate models – and for this health-care focused study, insurance coverage can be a more direct factor in the relationship between income and asthma outcomes. The sample frame is documented to be predominantly low income (poverty level in Rochester and meal subsidy levels within RCSD).
Our dependent measures of child asthma care and experiences included parent report of: number of symptom-free days over two weeks []; use of any urgent care in the past year; any unmet health care need in the past year (meaning that parent had to delay or not get health care for the child when parent felt care was needed; or delay or not get prescription medicines for the child when parent felt they were needed); parent experiences with reading or filling out medical forms [], parent perception of the child’s overall health (excellent/good or fair/poor), parent perception of asthma control, and degree of parent worry about the child’s health. We measured parent-reported quality of life using Juniper’s Paediatric Asthma Caregiver’s Quality of Life Questionnaire (PACQLQ) [19]. The PACQLQ is a standard instrument used to assess the quality of life of caretakers of children with asthma, and provides a quantitative score that reflects answers to questions about the burden of caring for a child with asthma. The survey consists of thirteen items with questions about impairment related to their child’s asthma during the past week. The instrument addresses two domains; emotional function (9 items) and activity limitation (4 items). Items are scored on a 7-point Likert scale, and means are calculated within each domain. Higher scores represent better quality of life. Differences of 0.5 or greater are accepted as clinically important [20]
We also examined several dependent measures of parent perception of the child’s asthma and asthma care. We utilized six previously-validated subscales that ask respondents to agree or disagree, on a 5-point Likert scale, with statements related to the child’s asthma [21,22].
The first and second scales include five questions each that measure parent beliefs about asthma medicines [22]. One scale represents perceived need for asthma medicines (e.g., “My child’s life would be impossible without their controller medicines”, “These controller medicines protect my child from becoming worse”. The other represents parent concerns about asthma medicines (e.g., “My child’s controller medicines are a mystery to me”, “Having to take these controller medicines disrupts my child’s life”). Higher scores represent greater need or concern.
The third scale, illness representation includes six items that assess parent knowledge of asthma symptoms (e.g., “Asthma cannot be controlled”, “Asthma symptoms are unpredictable”, “It’s hard to figure out how bad an asthma attack is”). Higher scores represent greater knowledge [21].
The fourth, treatment expectations, includes seven items that capture the degree of parent optimism or pessimism about the child’s asthma treatment (e.g., “I expect that my child can fully participate in gym and normal physical activity”, “I believe that my child can be symptom-free most of the time”, “I worry that something terrible will happen to my child if I am not there”). Higher scores represent more positive expectations [21].
The fifth scale includes ten items that describe parent perception of interactions with providers regarding the child’s asthma (e.g., “The doctor(s) who treat my child for asthma may understand asthma in general, but they don’t understand how asthma affects my child”, “I’m involved as much as I want to be in making decisions about when to give what medications”, “I worry about bothering my child’s doctor when I have questions or worries”). Higher scores represent greater worry or concern [21].
The sixth scale uses four items to measure parent beliefs about when to seek care for the child’s asthma (e.g., “If my child had asthma symptoms more than 2 times per week, I would contact my child’s health care provider”, “If my child was limited in gym or physical activity, I would call my child’s health care provider”). Higher scores indicate greater inclination to seek care [21].
Responses for each scale were added to produce a numeric score for each scale. These scores were then analyzed by calculating and comparing means.
2.4. Analyses
We performed bivariate analyses (chi-square and t-test) to identify associations between parent HL and our dependent measures. We then performed multivariate logistic and linear regression analyses to identify independent associations between parent HL and key child asthma outcomes. Dependent variables that were significant in bivariate analyses at a level of < 0.10 were included in multivariate analyses. All statistical tests were two-tailed. We used SPSS version 15.0 for all analyses [23].
3. Results
Our response rate was 72%. Table 1 shows demographic characteristics of the sample by parent HL. Overall, 85% of children had public insurance – mostly Medicaid -- which requires income at or below 100% FPL. Overall, for 33 percent of children, the respondent parent had limited HL, whereas for 67 percent of children, the respondent parent had adequate HL. We found significant differences by parent HL in type of child health insurance, parent race/ethnicity, and parent employment status: limited HL was more prevalent among publicly-insured children whose parents were non-white, Latino or not employed.
Table One.
Demographic Characteristics by Parent Health Literacy
| Overall n (%) |
Adequate HL n (%) |
Low HL n (%) |
P-value | |
|---|---|---|---|---|
| Parent Health Literacy (HL) | 499 (100) | 335 (67) | 164 (33) | |
| Child has Public Insurance1 | 425 (87.4) | 278 (85.3) | 147 (91.9) | .042 |
| Parent Race is: Black | 316 (63.3) | 225 (67.2) | 91 (55.5) | |
| White | 62 (12.4) | 49 (14.6) | 13 (7.9) | |
| Mixed/Other | 121 (24.2) | 61 (18.2) | 60 (36.6) | <.001 |
| Parent is: Hispanic | 109 (21.9) | 57 (17.0) | 52 (31.9) | <.001 |
| Parent is: Employed | 314 (65.8) | 237 (72.7) | 78 (51.0) | <.001 |
Includes Medicaid and State Children’s Health Insurance Program (SCHIP)
Table 2 shows associations between parent HL and morbidity or perceived burden of asthma on the child and the parent. Parents with limited HL were more likely to: perceive their child’s health as fair or poor (versus excellent, very good or good); and report that they worry “very much more” than other parents do about their child’s health. Parents with low HL had worse scores for: asthma knowledge (illness representation), treatment expectations, and interactions with providers, and had higher scores for perceived need for asthma medicines. However, there were no differences by parent HL in parent: concerns about medicines, beliefs about when to seek asthma care, perception of whether the child’s asthma was under good control, or number of symptom-free days.
Table Two.
Parent Health Literacy and Child Asthma Burden
| Overall n (%) |
Adequate HL n (%) |
Low HL n (%) |
P-value | |
|---|---|---|---|---|
| Parent Health Literacy (HL) | 499 (100) | 335 (67) | 164 (33) | |
| Child’s Health is Fair or Poor | 122 (24.4) | 58 (17.3) | 64 (39.0) | <.001 |
| Worry More than Other Parents | 242 (48.7) | 143 (42.8) | 99 (60.7) | <.001 |
| Asthma Not Under Good Control | 400 (80.2) | 276 (82.4) | 124 (75.6) | .094 |
| Number of Symptom-Free Days | ||||
| Mean | 8.02 | 8.02 | 8.01 | |
| (SD) | (4.83) | (4.76) | (4.98) | .990 |
| Parent Quality of Life* | ||||
| Mean | 5.34 | 5.41 | 5.18 | |
| (SD) | (1.24) | (1.17) | (1.36) | .061 |
Juniper Parent Quality of Life Scale [34]
Table 3 shows associations between parent HL and child health care use and experiences. Parents with limited HL were more likely to need help with medical forms and information, but did not differ from parents with adequate HL in their use of preventive asthma medicines or urgent care for the child, and did not report significant differences in unmet need for health care or prescriptions for the child.
Table Three.
Parent Health Literacy and Experiences with Asthma Care
| Overall n (%) |
Adequate HL n (%) |
Low HL n (%) |
P-value | |
|---|---|---|---|---|
| Parent Health Literacy (HL) | 499 (100) | 335 (67) | 164 (33) | |
| Medical Forms: | ||||
| Need Help to Read Forms | 191 (38.3) | 106 (31.6) | 85 (51.8) | <.001 |
| Not Confident Filling Forms | 127 (25.5) | 60 (17.9) | 67 (40.9) | <.001 |
| Used Any Preventive Medicines | 341 (68.3) | 224 (66.9) | 117 (71.3) | .357 |
| Used Any Urgent Care (Emergency or Inpatient) | 205 (41.1) | 138 (41.2) | 67 (40.9) | >.999 |
| Any Unmet Need (Health Care or Prescriptions) | 105 (21.0) | 74 (22.1) | 31 (18.9) | .483 |
| Illness Representation | ||||
| Mean | 3.20 | 2.84 | ||
| (SD) | (062) | (0.76) | <.001 | |
| Treatment Expectations | ||||
| Mean | 3.06 | 2.83 | ||
| (SD) | (0.64) | (0.62) | <.001 | |
| Interactions with Provider | ||||
| Mean | 4.14 | 3.85 | ||
| (SD) | (0.52) | (0.50) | <.001 | |
| Parent Beliefs (??) | ||||
| Mean | 3.83 | 3.90 | ||
| (SD) | (0.86) | (0.84) | 0.353 | |
| BMQ* Need for Medicines | ||||
| Mean | 16.56 | 18.15 | ||
| (SD) | (3.86) | (3.89) | <.001 | |
| BMQ* Concerns | ||||
| Mean | 14.17 | 14.80 | ||
| (SD) | (3.70) | (4.11) | .084 | |
BMQ denotes Beliefs About Medicines Questionnaire [37]
Table 4 shows the unadjusted and adjusted odds ratios for associations between parent HL and key measures regarding child asthma. Bivariate associations remained significant after adjusting for socio-demographic characteristics of the child and the parent. Among parents with limited HL, the odds of reporting the child’s health as fair or poor were nearly four times greater, and the odds of reporting more worry than other parents were more than two times greater, compared with children whose parents had adequate HL. In adjusted models, low HL was stronger than other covariates in predicting: greater perceived need for asthma medicines, less knowledge about asthma, lower expectations about asthma treatment, and perception of worse interactions with providers about the child’s asthma.
Table Four.
Regression Results: Role of Limited Parent Health Literacy on Key Asthma-Related Outcomes
| Unadjusted | Adjusted* | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | P-value | |
| Logistic Regression: | ||||||
| Child’s Overall Health Fair/Poor Parent HL Limited Parent HL Adequate (Referent) |
3.06 | 2.0–4.7 | <.001 | 3.96 1.0 |
2.4–6.4 | <.001 |
| Worry More than Other Parents Parent HL Limited Parent HL Adequate (Referent) |
2.07 | 1.4–3.0 | <.001 | 1.85 1.0 |
1.2–2.8 | .004 |
| Help to Read Medical Forms Parent HL Limited Parent HL Adequate (Referent) |
2.32 | 1.6–3.4 | <.001 | 2.03 1.0 |
1.3–3.1 | .001 |
| Not Confident Filling Out Forms Parent HL Limited Parent HL Adequate (Referent) |
3.17 | 2.1–4.8 | <.001 | 2.53 1.0 |
1.6–4.0 | <.001 |
| Linear Regression: | ||||||
| Unadjusted | Adjusted | |||||
| Std. β | 95% CI | Std. β | 95% CI | |||
| Parent Quality of Life (PACQOL) Parent HL Limited Parent HL Adequate (Referent) |
−0.09 | −0.47 to −0.001 | .084 | −0.097 | −0.51 to−0.004 | 0.47 |
| Illness Representation Parent HL Limited Parent HL Adequate (Referent) |
−0.25 | −0.5 to −0.2 | <.001 | −0.22 | −0.4 to −0.8 -.80 |
<.001 |
| Treatment Expectation (Lower) Parent HL Limited Parent HL Adequate (Referent) |
−0.16 | −0.3 to −0.1 | <.001 | −0.15 | −0.3 to −0.7 | .002 |
| Physician Interactions (Worse) Parent HL Limited Parent HL Adequate (Referent) |
−0.26 | −0.4 to −0.2 | <.001 | −0.20 | −0.3 to −0.1 | <.001 |
| BMQ** Necessity (Greater Need) Parent HL Limited Parent HL Adequate (Referent) |
0.19 | 0.9 to 2.3 | <.001 | 0.15 | 0.4 to 2.0 | .003 |
| BMQ** Concerns Parent HL Limited Parent HL Adequate (Referent) |
0.77 | −0.09 to 1.35 | .08 | 0.69 | −0.21 to 1.35 | .153 |
Covariates:
Child: Health Insurance
Parent: Employment, Ethnicity, Race, Health Literacy
Std denotes standardized β
BMQ denotes Beliefs About Medicines Questionnaire [37]
4. Discussion and Conclusion
4.1 Discussion
In this cohort of children who are predominantly low-income, urban, and have persistent asthma, we found that even though health care use (e.g., preventive medicines, urgent care, intent to seek care) did not differ by parent HL, many asthma-related beliefs and experiences did differ. Parents with limited HL perceived their children as sicker, perceived greater asthma burden, reported poorer interactions with their child’s provider, worried more about their child’s health, and reported lower quality of life than did parents with adequate HL.
Our results differ from those of DeWalt and Pignone, who found that limited parent HL was associated with worse asthma care and outcomes [8]. However this is likely explained by differences in the range of asthma severity in the two studies. DeWalt and Pignone included children with a broad range of severity, from mild to severe, whereas our study included only children with persistent asthma.
Effective asthma management requires accurate symptom recognition, skills in equipment and medication use, adherence to medication regimens, and understanding of when to seek different types of care. However, studies have demonstrated inadequate asthma management, which contributes to preventable morbidity [24,25]. This is particularly true for low income and minority children [26,27]. Asthma education can improve asthma care among adults. A number of studies have demonstrated that adults with limited HL can learn new skills for managing their own asthma [28]; however, skills acquisition is not always linked to improved asthma outcomes. In one intervention with parents of children with asthma, inhaler technique showed minimal improvement, and parents’ use of child asthma medicines remained poor even after intervention [29]. Evidence from a study of adherence in young children with asthma found variable and disappointing degrees of adherence even when use was monitored with a Smartinhaler within a research study [30]. Children in a school-based asthma management program showed paradoxical effects; although participants improved self-management behavior, missed fewer days of school and improved academic performance relative to the comparison group, their health status did not improve [31]. Factors other than health literacy can influence perception, management, and experiences of parents and children with asthma. Although health literacy is both measurable and to some degree mutable, it is also strongly associated with socioeconomic status, education level, and other psychosocial factors that remain unmeasured. Factors including family structure [32], homelessness [33], and cultural background [34] and even provider perception of patients [35] are important contextual or even focal factors in ‘health literacy’ interventions.
Scientific and financial support are both increasing for ‘health literacy’ interventions, and these efforts are important. It is essential – with all interventions – to consider the context within which ‘health literacy’ is operationalized. As described in sections 4.1.1–4.1.3, von Wagner’s domains of motivation (knowledge), attitudes (health beliefs), health systems (information and communication), and volition (task-specific skills) provide a model for multi-focal interventions to address health literacy in the context of other psychosocial factors and collectively mediate parent worry and concern.
4.1.1 Motivational Factors: Parent knowledge, beliefs and expectations about child asthma
In our sample, all children had persistent asthma, yet parents with limited HL perceived a greater burden from the child’s asthma. They had less knowledge, had lower expectations about what treatment could accomplish, reported poorer interactions with the child’s asthma care providers, had problems with basic medical paperwork, and felt their children were sicker. Consequently, they worried more about the child’s health. Our results are consistent with those of Moon and colleagues, who found that parents with limited literacy skills are more likely to rate their child’s health unfavorably relative to parents whose literacy skills are adequate [36].
Parent beliefs and expectations about asthma management are also shaped by ethnic and cultural factors that could affect health literacy. Smeeton et al examined parental attitudes toward asthma management among ethnic minorities in London, and found ethnicity-related differences in: beliefs about risks and benefits of asthma medicines; use of preventive versus rescue medicines; perceptions of and expectations about the child’s asthma; and perception of stigma associated with a diagnosis of asthma [34].
Cognitive factors themselves can influence management of child asthma – both by parents and by children themselves. One study in Egypt found that child knowledge, perceptions, locus of control, and self-efficacy most strongly affected child self-management of asthma, whereas the strongest predictors of parent management of child asthma were: socioeconomic status, asthma knowledge, and health beliefs [37].
4.1.2 Health System Factors: understanding and accessibility of available services and information
Although parents with low HL perceived greater asthma burden and greater need for asthma medicines, there were no HL-related differences in perceptions of when to seek care or actual use of care. It is possible that the important difference here lies in parents’ understanding of available services and information. Parents who struggle to read health materials may not understand their child’s condition or treatment. Whether their children are actually sicker or parents just perceive them to be, these parents could feel lost in the system. As a consequence, although they report more problems and concerns related to the child’s asthma, their beliefs about when to seek care may not differ proportionate to their different experiences with child asthma.
Yoos and colleagues examined the alignment of parent versus provider representation of child asthma to elucidate the effects of concordance and discordance on child asthma care. They found that parents with low levels of education were less able to represent the child’s asthma in ways that providers expected, and therefore recommended that providers elucidate and incorporate parent beliefs into communication about the child’s asthma and treatment plan [38]. Such steps could improve parent understanding of information about the child’s asthma as well as services available to address and help manage it.
4.1.3. Implementation and Action Factors: parent behavior specific to child asthma
To successfully manage a child’s asthma, parents must take action both within and outside the health system. Most behavior within the health system involves communication – yet parents who have HL problems may be less able to effectively give or receive communication about the child’s asthma. Our results demonstrated lower reported provider interaction scores among parents with low HL. It is possible that parents who struggle to fill out forms at medical visits may be unable to convey important details about their child’s asthma, limiting providers’ opportunities to respond. In turn, providers may alter their communication with parents based on perceptions of caregiver literacy; prior research has documented a degree of discordance between caregiver HL and provider perception of caregiver HL [35]. The authors suggest that providers could overestimate caregiver HL and under-explain asthma symptoms or treatment regimens, assuming that information is understood; or they could underestimate caregiver HL and censor or withhold more complex information or action plans [35].
This misalignment of information exchange can affect child asthma management and outcomes. Prior research has documented associations between asthma control and provider teaching about asthma. Halterman et. al. found that children whose asthma control was sub-optimal were significantly less likely to have received from a physician an asthma action plan or instruction in correct use of metered-dose inhalers (MDI’s) [25]. Warman et. al. found that lower education level was negatively associated with receipt of an asthma action plan [39]. In fact, parents in clinical settings reported that teaching about acute care and MDI use was more likely to occur than was teaching about preventive management [40]. With regard to this study, it is important to consider the potential role of parent HL on their perception, recall, and representation of what they were taught.
Basic stressors and challenges can interfere with the higher-order concerns, resources, skills, and action of parents regarding child asthma. Health literacy is one of many factors rather than a singular determinant of parent management of child asthma.
4.1.4 Limitations
We studied an urban, low-income, largely minority sample of children that experiences known high prevalence of childhood asthma and greater likelihood of limited parent health literacy. Results for parent HL and associations with asthma care could differ in other samples and settings.
Our sample had limited variation in asthma severity. Health literacy may show associations with asthma severity and service use outcomes in samples with greater variation in asthma from mild to severe. However our sample of children with persistent asthma allowed us to isolate the associations between parent HL and the key outcomes of parent worry and concern about the asthmatic child in a population with similar levels of severity.
We used parent report of asthma morbidity and did not obtain physiologic measures of asthma severity, such as spirometric measurements. However, the National Heart, Lung, and Blood Institute criteria for defining asthma severity depend primarily on parent report of symptoms and, therefore, these data are consistent with that standard.
Our study is cross-sectional, and therefore cannot examine causal pathways or draw causal inferences. Further research is needed to determine which pathways are involved in parent perception of and worry about their child’s health.
4.2. Conclusion
Despite equivalent asthma severity and equivalent use of medical care and medicines, parents with limited HL had less knowledge and lower expectations, and experienced a greater burden of confusion, communication, and worry. They also rated the child’s health less favorably, and reported lower overall quality of life.
4.3 Practice Implications
It is possible that interventions for parents or caregivers with limited HL could enhance their understanding, expectations, communication about and skills for management of child asthma. Enhanced knowledge and skills could contribute to greater parent confidence and self-efficacy, in turn minimizing the perceived burden of child asthma on parents worry, concern, and quality of life. Longitudinal research is needed to examine pathways for effects of parent HL on child asthma care and outcomes, to assess the importance of health literacy relative to and within the context of multiple factors in health care management and use, and to test interventions which utilize those pathways to address parent concerns and improve child asthma care.
Acknowledgments
This work was supported by funding from the National Heart, Lung, and Blood Institute [5R01-HL079954] (Role – support for data collection and analyses for the full School Based Asthma Therapy (SBAT) trial and support of time for authors Halterman and Conn); the Halcyon Hill Foundation (Role – support for data collection, and partial support of time for authors Halterman and Conn); the Centers for Disease Control and Prevention, Office of the Director [1K01- DP001125] (Role – support of time for author Shone); and the Robert Wood Johnson Generalist Physician Faculty Scholars Program (Role – support of time for authors Halterman and Sanders)
We gratefully acknowledge Ms. Telva Hernandez and Mr. Reynaldo Tejon for assistance with data coding and analyses; Ms. Maria Fagnano for validation of results; and the entire Asthma Study Team for data collection.
Footnotes
This work represents opinions of the authors and does not reflect perspectives of any of the funders. The funders had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
The authors do not have any potential or actual conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Laura P. Shone, University of Rochester School of Medicine, 601 Elmwood Avenue, Department of Pediatrics, Box 777, Rochester, NY USA 14642, TEL: 585.273.4084, FAX: 585.756.4132, Laura_Shone@URMC.Rochester.edu
Kelly M. Conn, Department of Pediatrics, University of Rochester School of Medicine, USA
Lee Sanders, Department of Pediatrics, University of Miami, USA.
Jill S. Halterman, Department of Pediatrics, University of Rochester School of Medicine, USA
References
- 1.Nielsen-Bohlman LT, Panzer AM, Hamlin B, Kindig DA. Committee on Health Literacy, Board on Neuroscience and Behavioral Health. Washington, DCL: National Academies Press; 2004. Institution of Medicine. Health literacy: a prescription to end confusion. [PubMed] [Google Scholar]
- 2.Paasche-Orlow MK, Parker RM, Gazmarian JA, Neilsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 20:175–84. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poureslami IM, Rootmen I, Balka E, Devarakonda R, Hatch J, FitzGerald M. A systematic review of asthma and health literacy: a cultural-ethnic perspective in Canada. Medscape General Medicine. 2007;9:40. [PMC free article] [PubMed] [Google Scholar]
- 4.Mancuso CA, Rincon M. Impact of health literacy on longitudinal asthma outcomes. Journal of General Internal Medicine. 2006;21:813–7. doi: 10.1111/j.1525-1497.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yin HS, Forbis SG, Dreyer BD. Health literacy and pediatric health. Curr Probl Pediatr Adolesc Health Care. 2007 Aug;37:258–86. doi: 10.1016/j.cppeds.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Sanders L, Zacur G. Parent health literacy: a predictor of child healthcare utilization. E-PAS (Pediatri Acad Soc) 2003;53:1517. [Google Scholar]
- 7.Ross LA, Frier BM, Kelnar CJ, Deary IJ. Child and parental mental ability and glycaemic control in children with Type I diabetes. Diabet Med. 2001 May;18:364–9. doi: 10.1046/j.1464-5491.2001.00468.x. [DOI] [PubMed] [Google Scholar]
- 8.DeWalt DA, Dilling MH, Rosenthal MS, Pignone MP. Low parent literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007 Jan-Feb;7:25–31. doi: 10.1016/j.ambp.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yin HS, Dreyer BP, Foltin G, van Schaick L, Mendelsohn AL. Association of low caregiver health literacy with reported use of nonstandardized dosing instruments and lack of knowledge of weight-based dosing. Ambul Pediatr. 2007 Jul;7:292–8. doi: 10.1016/j.ambp.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Gehring U, Pattenden S, Slachtova H, Antova T, Braun-Fahrlander C, Fabianova E, Fletcher T, Galassi C, Hoek G, Kuzmin SV, Luttmann-Gibson H, Moshammer H, Rudnai P, Zlotkowska R, Heinrich J. Parental education and children’s respiratory and allergic symptoms in the Pollution and the Young (PATY) study. Eur Respir J. 2006 Jan;27:95–107. doi: 10.1183/09031936.06.00017205. [DOI] [PubMed] [Google Scholar]
- 11.McDaniel M, Paxson C, Waldfogel J. Racial disparities in childhood asthma in the United States: evidence from the National Health Interview Survey, 1997–2003. Pediatrics. 2006;117:868–77. doi: 10.1542/peds.2005-1721. [DOI] [PubMed] [Google Scholar]
- 12.Schaafsma ES, Raynor T, de Jonmg-van TW. Accessing medication information by ethnic minorities: barriers and possible solutions. Pharm World Sci. 2003;25:185–90. doi: 10.1023/a:1025812716177. [DOI] [PubMed] [Google Scholar]
- 13.Weiss BD, Reed RL, Kligman EW. Literacy skills and communication methods of low-income older persons. Pat Educ Counseling. 1995;25:109–19. doi: 10.1016/0738-3991(95)00710-h. [DOI] [PubMed] [Google Scholar]
- 14.Georges CA, Bolton LB, Bennett C. Functional health literacy: An issue in African-American and other ethnic and racial communities. J Nat Black Nurses Association. 2004;15(1) [PubMed] [Google Scholar]
- 15.von Wagner C, Steptoe A, Wolf MS, Wardle J. Health literacy and health actions: a review and a framework from health psychology. Health Educ Behav Online First. 2008 Aug 26; doi: 10.1177/1090198108322819. doi: 1177/1090198108322819. [DOI] [PubMed] [Google Scholar]
- 16.Paasche-Orlowe MK, Wolf MS. The causal pathways linking health literacy to health outcomes. American Journal of Health Behavior. 2007;31(Suppl 1):s19–s26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 17.National Asthma Education and Prevention Program (NAEPP) US Department of Health and Human Services National Institutes of Health publication 02-5075. Bethesda, MD: US Department of Health and Human Services; 2002. Expert Panel Report II: Guidelines for the Diagnosis and management of Asthma: Update on Selected Topics 2002. [Google Scholar]
- 18.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, Crouch MA. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–5. [PubMed] [Google Scholar]
- 19.Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in the parents of children with asthma. Quality of Life Research. 1996;5:27–34. doi: 10.1007/BF00435966. [DOI] [PubMed] [Google Scholar]
- 20.American Thoracic Society Quality of Life Resource. Instrument description for the Pediatric Asthma Caregiver’s Quality of Life Questionnaire (PACQLQ) [Accessed on December 18, 2008]. Available at: http://www.atsqol.org/sections/instruments/pt/pages/pacqlq.html.
- 21.Yoos HL, Kitzman H, McMullen A. Barriers to anti-inflammatory medication use in childhood asthma. Ambul Pediatr. 2003;3:181–90. doi: 10.1367/1539-4409(2003)003<0181:btamui>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 22.Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. 1999;14:1–24. [Google Scholar]
- 23.SPSS for Windows, Rel. 15.0. Chicago: SPSS Inc; [Google Scholar]
- 24.Ordonez GA, Phelan PD, Olinsky A, Robertson CF. Preventable factors in hospital admissions for asthma. Arch Dis Child. 1998;78(2):143–7. doi: 10.1136/adc.78.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Halterman JS, Auinger P, Conn KM, Lynch K, Yoos HL, Szilagyi PG. Inadequate therapy and poor symptom control among children with asthma: a multistate sample. Ambul Pediatr. 2007 Mar-Apr;7:153–9. doi: 10.1016/j.ambp.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 26.Crain EF, Kercsmar C, Weiss KB, Mitchell H, Lynn H. Reported difficulties in access to quality care for children with asthma in the inner city. Arch Pediatr Adolesc Med. 1998;152:333–9. doi: 10.1001/archpedi.152.4.333. [DOI] [PubMed] [Google Scholar]
- 27.Eggleston PA, Malveaux FJ, Butz AM, et al. Medications used by children with asthma living in the inner city. Pediatrics. 1998;101(3 Pt 1):349–54. doi: 10.1542/peds.101.3.349. [DOI] [PubMed] [Google Scholar]
- 28.Paasche-Orlow MK, Riekert KA, Bilderback A, Chanmugam A, Hill P, Rand CS, Brancati FL, Krishnan JA. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med 2005. 2005;172:980–6. doi: 10.1164/rccm.200409-1291OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aziz NA, Norzila MZ, Hamid MZ, Noorlaili MT. Skills amongst parents of children with asthma: a pilot interventional study in a primary care setting. Med J Malaysia. 2006 Dec;6:534–9. [PubMed] [Google Scholar]
- 30.Burgess SW, Sly PD, Morawska A, Devadason SG. Assessing adherence and factors associated with adherence in young children with asthma. Respirology. 2008 Jun;13:559–63. doi: 10.1111/j.1440-1843.2008.01292.x. [DOI] [PubMed] [Google Scholar]
- 31.Bartholomew LK, Sockrider M, Abramson SL, Swank PR, Czyzewski DI, Tortolero SR, Markham CM, Fernandez ME, Shegog R, Tyrell S. Partners in school asthma management: evaluation of a self-management program for children with asthma. J Sch Health. 2006 Aug;76:283–90. doi: 10.1111/j.1746-1561.2006.00113.x. [DOI] [PubMed] [Google Scholar]
- 32.Chen AY, Escarce JJ. Family structure and the treatment of childhood asthma. Med Care. 2008 Feb;46:174–84. doi: 10.1097/MLR.0b013e318156ff20. [DOI] [PubMed] [Google Scholar]
- 33.Sleath BL, Jackson E, Thomas KC, Galloway J, Dumain L, Thorpe J, Rollins A, Morrissey J. Literacy and perceived barriers to medication taking among homeless mothers and their children. Am J Health Syst Pharm. 2006 Feb 15;63:346–51. doi: 10.2146/ajhp050070. [DOI] [PubMed] [Google Scholar]
- 34.Smeeton NC, Rona RJ, Gregory J, White P, Morgan M. Parental attitudes towards the management of asthma in ethnic minorities. Arch Dis Child. 2007 Dec;92(12):1082–7. doi: 10.1136/adc.2006.112037. Epub 2007 Feb 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wittich AR, Mangan J, Grad R, Wang W, Gerald LB. Pediatric asthma: caregiver health literacy and the clinician’s perception. Journal of Asthma. 2007 Jan;44:51–5. doi: 10.1080/02770900601125672. [DOI] [PubMed] [Google Scholar]
- 36.Moon RY, Cheng TL, Patel KM, Baumhaft K, Scheidt PC. Parental literacy level and understanding of medical information. Pediatrics. 1998;102:e25. doi: 10.1542/peds.102.2.e25. [DOI] [PubMed] [Google Scholar]
- 37.Ftohy EM, Abdel-Gawwad ES, Kamal MM, El-Bourgy MD, El-Mallawani H. Cognitive predictors of self-management behavior of asthmatic children and their families in Alexandria. J Egypt Public Health Assoc. 1999;74:439–61. [PubMed] [Google Scholar]
- 38.Yoos HL, Kitzman H, Henderson C, McMullen A, Sidora-Arcoleo K, Halterman JS, Anson E. The impact of the parental illness representation on disease management in childhood asthma. Nurs Res. 2007 May-Jun;56:167–74. doi: 10.1097/01.NNR.0000270023.44618.a7. [DOI] [PubMed] [Google Scholar]
- 39.Warman KL, Silver EJ, McCourt MP, Stein REK. How does home management of asthma exacerbations by parents of inner-city children differ from NHLBI guideline recommendations? Pediatrics. 1999;103:422–7. doi: 10.1542/peds.103.2.422. [DOI] [PubMed] [Google Scholar]
- 40.McMullen A, Yoos HL, Anson E, Kitzman H, Halterman JS, Arcoleo KS. Asthma care of children in clinical practice: do parents report receiving appropriate education? Pediatr Nurs. 2007 Jan-Feb;33:37–44. [PubMed] [Google Scholar]