Abstract
The authors examined the relations among intimate partner violence (IPV), maternal depressive symptoms, and maternal harsh intrusive parenting. Using a cross-lagged, autoregressive path model, they sought to clarify the directionality of the relations among these 3 variables over the first 2 years of the child’s life. The results indicated that, in this diverse sample of families living in predominantly low-income rural communities (N = 705), higher levels of early IPV were associated with increases in maternal depressive symptoms, which in turn were associated with increases in maternal harsh intrusive parenting behaviors. These findings suggest that interventions aimed at improving the parenting of women exposed to domestic violence may want to simultaneously target IPV and depressive symptomatology.
Keywords: depression, intimate partner violence, parenting
Parenting practices have long been acknowledged as a potent predictor of child functioning. Higher levels of harsh, controlling parenting behaviors and lower levels of sensitive, supportive parenting have consistently been associated with less ideal outcomes for children of all ages (Cox & Harter, 2003). Parenting during early childhood has been shown to be particularly important for children’s functioning, with significant implications for children’s later development (Maccoby, 2000; Verhoeven, Junger, Van Aken, Deković, & Van Aken, 2007), yet early childhood is a particularly challenging time for parents to interact with their children sensitively. The transition to parenthood can be a stressful time for parents because it places new demands on the couple and requires reorganization of the family system in order to accommodate the new child (Cox, Paley, Burchinal, & Payne, 1999; Maccoby). As the child approaches toddlerhood, increases in child negative affectivity also contribute to parenting stress in that it increases and broadens the types of demands placed on parents at this time (Keenan & Wakschlag, 2000; Verhoeven et al.). Taken together, these stressors make the first 2 years of the child’s life a particularly challenging time for parents to not use negative and controlling tactics with their children, yet it is an especially important time for them to not do so. Although parenting behaviors tend to remain stable over time (Dallaire & Weinraub, 2005), they are not a fixed quality but instead have been shown to be affected by a number of contextual factors, including family dynamics (Cummings & Davies, 2010) and the mother’s well-being (Cummings & Davies, 1994; Golding, 1999; Teti, Gelfand, & Pompa, 1990). Given the integral role that parenting plays in child development, it is important to examine factors that may place parenting at risk.
Theoretical Background
Considerable research has been devoted to the impact of intimate partner violence (IPV) on parenting practices. Being in a physically violent relationship has been associated with more harsh, controlling, and aggressive parenting behaviors (DeVoe & Smith, 2002; Holden & Ritchie, 1991; Levendosky & Graham-Bermann, 2001; Straus & Gelles, 1990). Although some research supports the idea that mothers exposed to IPV overcompensate by being more sensitive to and supportive of their children (e.g., Letourneau, Fedick, & Willms, 2007; Levendosky, Huth-Bocks, Shapiro, & Semel, 2003), there is growing evidence that IPV negatively affects parenting behaviors, particularly in the context of maternal depressive symptoms (Levendosky & Graham-Bermann; Levendosky et al., 2003). For example, Levendosky et al. (2003) found that intimate partner physical violence was associated with negative parenting, but only for depressed mothers. Although there is mounting evidence that IPV exerts its influence on parenting via its impact on maternal well-being (Campbell, 2002; Levendosky & Graham-Bermann), some research suggests that the relations among these three variables are bidirectional (Davila, Bradbury, Cohan, & Tochluk, 1997). Although it is clear from clinicians and researchers that IPV, maternal depressive symptoms, and maternal parenting behaviors are related to one another, less is known about the directionality of these relations, largely because of a dearth of longitudinal research in which bidirectional relations have been investigated. The goal of the current study was to address this gap by investigating the nature of the relationship among these three constructs over time.
Intimate Partner Violence
IPV has been associated with a variety of negative outcomes for children (Kitzmann, Gaylord, Holt, & Kenny, 2003; Wolfe, Crooks, Lee, McIntyre-Smith, & Jaffe, 2003). Although there likely is a direct link between IPV and child outcomes (Cummings & Davies, 2010), the effect of IPV on children can also be explained by disturbances in parent–child relationships, as evidenced by increases in parental negativity (DeVoe & Smith, 2002; Levendosky & Graham-Bermann, 2001; Straus & Gelles, 1990) and difficulties forming secure parent–child attachments (Goodman & Gotlib, 2002). Stress and anger produced during conflict among spouses is described as spilling over into the parent–child relationship, resulting in relationships characterized by more harsh, controlling maternal parenting behaviors and higher rates of child-directed aggression (Cox, Paley, & Harter, 2001; Slep & O’Leary, 2005), in addition to an increased likelihood of corporal punishment (Straus & Kantor, 1995). Consistent with this idea, recent work suggests that there is a substantial co-occurrence of partner maltreatment and child abuse (Jouriles, McDonald, Slep, Heyman, & Garrido, 2008; Knickerbocker, Heyman, Slep, Jouriles, & McDonald, 2007), such that an estimated 45% to 70% of children living in physically violent homes are also being physically abused by a parent (Holt, Buckley, & Whelen, 2008). Similarly, Levendosky, Leahy, Bogat, Davidson, and von Eye (2006) found that higher levels of IPV were associated with less ideal observed parenting behaviors, which they captured using a latent variable that included measures of maternal intrusiveness and hostility.
Maternal Depressive Symptoms
Substantial empirical attention has been paid to the impact of maternal depressive symptoms on children’s development. Depressed mothers are more likely to be harsh, controlling, and negative when interacting with their children (Lovejoy, Graczyk, O’Hare, & Neuman, 2000), in addition to being more emotionally insensitive and unsupportive, withdrawn, and aggressive (Burke, 2003). For example, Lyons-Ruth and colleagues (2000) reported (using data from a representative sample of children under age 3) that for every additional depressive symptom a mother endorsed, the odds of her feeling annoyed, yelling at, or spanking her young child increased by 31% to 38%. Similarly, Cohn, Campbell, Matias, and Hopkins (1990), using a sample of 46 depressed and nondepressed mother–infant dyads, found that depressed mothers showed increased negative affect and less contingent responsiveness when interacting with their children. Young children may be at particular risk for the negative impact of maternal depressive symptoms in that disturbances in early relationships may result in children not acquiring foundational skills, the lack of which can have lasting consequences for children’s development (DeVoe & Smith, 2002). In a meta-analysis looking at the impact of depressive symptoms on positive, engaging, and negative parenting behaviors, Lovejoy and colleagues (2000) found that maternal depressive symptoms were most strongly associated with negative dimensions of maternal parenting; thus, harsh intrusive parenting was the focus of the current study.
As alluded to above, maternal psychopathology is one proposed mechanism through which IPV may influence parenting behaviors (Huang, Wang, & Warrener, 2010; Levendosky & Graham-Bermann, 2001), such that the stress of intense conflict among parents negatively impacts maternal depressive symptoms, which in turn impact maternal parenting behaviors. Several authors have found support for this notion, including Levendosky and Graham-Bermann, whose work suggests that depressive symptoms mediate the relationship between IPV and multiple dimensions of parenting.
It is important to emphasize that the linkages among IPV, maternal depressive symptoms, and maternal parenting behaviors may not be unidirectional but rather part of dynamic bidirectional relationships that change over time. For example, in addition to the rich literature that links IPV and depressive symptoms both concurrently and over time (Golding, 1999; Morewitz, 2004; Zlotnick, Johnson, & Kohn, 2006; Zlotnick, Kohn, Peterson, & Pearlstein, 1998), there also is evidence that depressive symptoms may contribute to conflict among couples (Beach, Sandeen, & O’Leary, 1990; Burke, 2003; Campbell, 2002). Similarly, just as depressive symptoms may influence parenting, the burden of caring for young children may be a risk factor for developing maternal depressive symptoms (Lyons-Ruth, Wolfe, & Lyubchik, 2000). Alternatively, individuals with depressive symptoms may be easier targets of intimate partner physical victimization. In support of this idea, Lehrer, Buka, Gortmaker, and Shrier (2006), using a sample of 1,659 adolescent girls, found that a 1-point increase in baseline depressive symptoms was associated with a 3% increase in the odds of subsequent exposure to both mild and moderate to severe IPV. In addition, just as IPV may negatively influence maternal parenting behaviors, arguments over harsh parenting practices may contribute to future IPV (Slep & O’Leary, 2001). As these examples illustrate, although these variables are known correlates of one another, the nature of their relationship, as well as the way in which they influence one another over time, is not entirely understood. Largely because of limited longitudinal research on their associations, in addition to a lack of studies that consider each of these bidirectional associations simultaneously in order to better understand their relative influence on one another, there remains relative ambiguity regarding the direction of their effect on one another.
IPV as a Control Parameter
Acknowledgment of the bidirectional nature of the relationships among IPV, maternal depressive symptoms, and maternal parenting behaviors, however, is not meant to imply that all of these relationships exert the same influence on one another at all stages in development. Instead, it seems likely that “control parameters” exist (see Thelen & Smith, 1998) such that at a particular point in a child’s development one of these variables in the family system may exert more influence on the others, and functioning in one domain may be exerting a larger influence on functioning in the others, thereby creating a cascading effect (Cox, Mills-Koonce, Propper, & Gariepy, 2010). Several studies point to IPV as the control parameter in the current study, including a number of studies that suggest that marital discord is a precursor of maternal depression (Beach et al., 1990; Proulx, Helms, & Buehler, 2007). For example, in their meta-analysis of 93 studies of marital quality and personal well-being, Proulx et al. found that the strength of the association between marital quality and well-being was stronger when marital quality was used to predict well-being, as opposed to when well-being was used to predict marital quality. Also supporting the idea of IPV as a control parameter, Campbell, Kub, Belknap, and Templin (1997), in their longitudinal study of battered women, found that women who were no longer in their physically violent relationship at the 2.5-year follow-up showed decreases in the number of depressive symptoms they endorsed, whereas the depressive symptoms of the women who remained in their violent relationships remained stable over time. Also lending legitimacy to this expected direction of influence is Margolin, Gordis, and Oliver’s (2004) finding that prior marital aggression placed families at increased risk for subsequent hostility spilling over from the marital relationship into the parent–child relationship.
Taken together, these findings suggest that, although there likely are bidirectional associations among IPV, maternal depressive symptoms, and maternal parenting behaviors, it seems probable that IPV is a control parameter in that it may be more likely to induce depressive symptoms in mothers (than vice versa), and these depressive symptoms in turn may influence negative maternal parenting behaviors.
The Current Study
As can be seen in the previous sections, there is relative ambiguity about the directionality of the relations among IPV, maternal depressive symptoms, and maternal harsh intrusive parenting behaviors. Although there is some suggestion that IPV exerts its influence on maternal parenting behaviors through its impact on maternal depressive symptoms, few studies to date have looked at the relations among these variables over time (see Zlotnick et al., 2006, and Choi & Marks, 2008, for notable exceptions), and even fewer have considered the possibility of bidirectional relationships. Given the potentially devastating effect that each of these factors can have on the development of a young child, it is important to better understand their interdependence so as to identify the best area for intervention. Given that younger children are more likely to be exposed to IPV than older children (Fantuzzo, Boruch, Beriama, Atkins, & Marcus, 1997), and that parenting during the first years of life is particularly important for children’s long-term functioning (Cox & Harter, 2003), it seems particularly important to investigate these relations over the first 2 years of the child’s life. Despite strong linkages between IPV and poor outcomes for both mothers and children (e.g., Golding, 1999; Sturge-Apple, Davies, Cicchetti, & Manning, 2010), there has been a relative lack of research devoted to the impact of IPV on the mothering of very young children, especially in community samples. The large population-based community sample of families living in rural communities used in the current study, therefore, offered a unique opportunity to investigate the impact of intimate partner physical violence on maternal parenting behaviors and psychological well-being.
Guided by family systems theory (Cox & Paley, 1997, 2003), which emphasizes the importance of considering the dynamic interplay between the multiple relationships in the family, the goal of the current study was to determine the nature of the relationships among IPV, maternal depressive symptoms, and maternal harsh intrusive parenting over the first 2 years of a child’s life. According to family systems theory, each family relationship (e.g., the parent–child relationship) is embedded in a network of other family relationships (e.g., the marital relationship), and a better understanding of the functioning and development of any given system within the family can be gained by considering the interdependence of these relationships and their mutual influence over time. In the current study, this theory would posit that one can obtain a more comprehensive understanding of the relations among IPV, maternal depressive symptoms, and maternal harsh intrusive parenting behaviors by simultaneously considering the dynamic, bidirectional relations among the various relationships and individual levels.
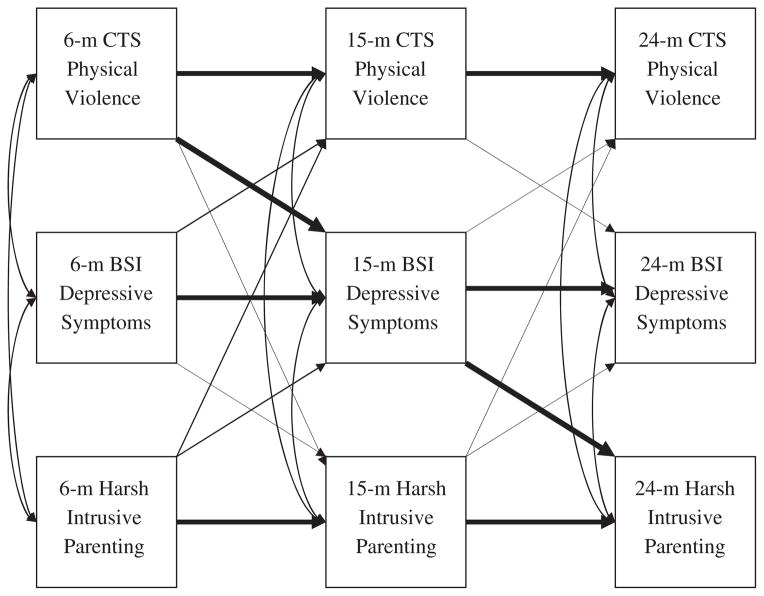
Using data from an ethnically and economically diverse population-based sample of families living in rural communities, we sought to test the longitudinal relations among these variables in an understudied population. Two competing processes were tested: (a) one in which there would be bidirectional relations among IPV, maternal depressive symptoms, and maternal harsh intrusive parenting, and (b) one in which IPV would emerge as a control parameter. We hypothesized that IPV would be the control parameter at this time in the child’s life, such that the effect of IPV would place parenting at risk through its influence on maternal depressive symptomatology; that is, we hypothesized that maternal depressive symptoms would fully mediate the relationship between IPV and maternal harsh intrusive parenting behaviors. In order to simultaneously test these two processes, a nonrecursive path model in which all theoretically plausible cross-lagged paths between the focal variables was estimated. See Figure 1 for a visual depiction of the conceptual model. If, during model estimation, only the boldface paths depicted in this figure were to emerge as statistically significant, the data would support the hypothesis that IPV is a control parameter. If, in addition to the boldface paths, any of the non-boldface paths were to emerge as statistically significant, the data would support the existence of bidirectional relations among the variables.
Figure 1.
Visual Depiction of the Conceptual Model.
Note: The boldface arrows indicate that we hypothesized that these paths would be significant, whereas the non-boldface arrows indicate paths that were estimated but were not hypothesized to be significant. Double-headed arrows indicate correlations that were estimated between within-time variables. m = month; CTS = Conflict Tactics Scale – Couple Form R; BSI = Brief Symptom Inventory.
Past research has identified a number of correlates of IPV, maternal depressive symptoms, and maternal parenting behaviors, including family income (Falconier & Epstein, 2011; Teti et al., 1990), race (Caetano, Vaeth, & Ramisetty-Mikler, 2008; Callahan & Wolinsky, 1994; Murry, Smith, & Hill, 2001), and maternal perceptions of social support (Stice, Ragan, & Randall, 2004; Teti et al.). To rule out the possibility that these variables are exclusively responsible for the relationships tested, we incorporated these three variables, in addition to the data collection site, as covariates in our investigation.
Method
Participants
The participants in this study constituted a subsample of The Family Life Project, an ongoing longitudinal study of 1,292 families living in six predominantly low-income, non-metropolitan counties in eastern North Carolina and central Pennsylvania (see http://projects.fpg.unc.edu/~flp/). Between September 15, 2003, and September 14, 2004, families were recruited in local hospitals shortly after the birth of the target child. A sample representative of the six counties was recruited with African American and low-income families oversampled. See Burchinal, Vernon-Feagans, Cox, and The Family Life Project Investigators (2008), for additional information about the recruitment and sampling procedures. Our subsample consisted of families in which both biological parents lived in the home with the target child when he or she was 6 months old and who remained living in the home until the child was 24 month old (N = 705). Of these children, 367 (52.1%) were male, 176 (25%) were African American, and 541 (72.6%) of the parents were married at the 6-month timepoint. The mean household income-to-needs ratio was 2.35 (range: 0–13.40). Our subsample was less racially diverse, more economically advantaged, and included more married couples than the complete sample. Mothers with transient or nonresidential partners were not included in these analyses because we believed that violence in these types of relationships would differentially affect mothers’ depressive symptoms and parenting behaviors, compared to violence occurring in more stable, coresidential relationships (Kouros, Papp, & Cummings, 2008).
Procedure
Data used in these analyses came from a series of home visits, when the target child was 6, 15, and 24 months old. At each of these timepoints, two research assistants visited children and their families in their homes, where they administered interviews and questionnaires to the parents and videotaped parent–child interactions for later coding. To minimize the possibility that respondents would be intimidated or somehow coerced by their partner’s presence, respondents completed questionnaires via a laptop computer while seated in a quiet space away from the other household members. During this time, their partner completed videotaped interactions with the target child while the research assistants ensured that the respondent remained undisturbed. These procedures are consistent with those used by similar studies in which both parents were present during data collection (e.g., Barnett, Deng, Mills-Koonce, Willoughby, & Cox, 2008; Towe-Goodman, Stifter, Coccia, & Cox, 2011).
At each visit, all participants were given a document that listed county-specific resources, including domestic violence and other counseling services, and were instructed that these resources were available to them or anyone they knew. All study procedures were approved by the University of North Carolina at Chapel Hill’s institutional review board.
Measures
Intimate partner violence
IPV was assessed using the Conflict Tactics Scale–Couple Form R (CTS-R; Straus & Gelles, 1990), a 19-item self-report measure completed by the mothers when their child was 6, 15, and 24 months old. Respondents were asked to rate, on a 7-point Likert-type scale (on which 0 = never, 1 = once, 2 = twice, 3 = 3–5 times, 4 = 6–10 times, 5 = 11–20 times, and 6 = more than 20), how often in the past 12 months they had engaged in specific behaviors. They were also asked to rate how often in the past 12 months their partner had engaged in each behavior. Scores on the 9-item Physical Violence subscale of this measure (which captures incidences of physical aggression and violence) from each of the three timepoints were used in this study. An example item reads “[How often in the past 12 months have you/your partner] kicked, bit, or hit him/her/you with a fist?” Sixty-three percent of mothers in our subsample did not report any physical violence. This figure is consistent with those found by the National Family Violence Survey, which reported that 10% to 12% of couples experienced at least one instance of IPV in the previous year, and 28% to 30% of U.S. couples have experienced some domestic violence during the course of their marriage (Straus & Gelles). When we looked at CTS-R scores over time, the majority of physically violent couples in our sample were classified as dual perpetrators (approximately 70% of the physically violent families), a prevalence rate that is consistent with previous work with community samples, which suggests that physical violence in community samples is more commonly mutual (Archer, 2000; Caetano et al., 2008). In an effort to more accurately capture the experience of most of our mothers, maternal reports of their own IPV and their report of their partners’ IPV were summed to create a total score that represents the total amount of physical violence experienced by the mother. Cronbach’s alphas for the 18 item total scores were .84, .87, and .88 for the 6-, 15-, and 24-month timepoints, respectively.
The CTS-R was also administered to fathers who participated in each of the visits; however, a number of residential fathers were either unable or unwilling to participate in the visits. Specifically, 87 of the 705 fathers did not participate in any of the three visits. None, however, who participated in the visit refused to complete the CTS-R. Although fathers who did not participate were more likely to be African American, of lower income, and to have attained a lower level of education than those who did participate, participation in the visit was not related to mothers’ reports of his or her physical violence. Unfortunately, we do not have detailed information about why fathers did not participate in the visit (anecdotal evidence suggests that difficulty rearranging paternal and maternal work schedules in order to complete the visit played a role); however, we have found no reason to believe that this nonresponse was related to IPV in particular. Because we believe that paternal responses were not missing at random, we could not use a missing-data technique if we also included fathers’ reports. Because maternal and paternal reports were moderately correlated (rs = .45, .36, and .38 for the 6-, 15-, and 24-month time-points, respectively), only the maternal report was used in the analyses presented below in order to maximize the number of families included in the analyses. To strengthen our confidence in our findings, however, all analyses were repeated using paternal report of IPV to test whether findings were the same regardless of reporter.
Maternal depressive symptoms
To assess their depressive symptoms, mothers completed the Brief Symptom Inventory (Derogatis, 2000), a 23-item self-report questionnaire of psychological distress. Respondents are asked to rate on a 5-point Likert-type scale (on which 0 = not at all and 4 = extremely) how distressed they were by each symptom over the past 7 days. The measure’s 6-item Depression subscale was used in the current study. An example item reads “[How much were you distressed by] feeling hopeless about the future?” Cronbach’s alphas for the 6-, 15-, and 24-month timepoints were .81, .84, and .86, respectively.
Maternal parenting behaviors
Maternal parenting behaviors were assessed during parent–child interactions at each home visit. When the children were 6 and 15 months old, mothers and children were presented with a standard set of toys and asked to complete a free play activity. Mothers were instructed to interact with their children as they typically would if given some free time during the day. When the children were 24 months old, the same mother–child dyads completed a puzzle task, in which they were presented with three developmentally appropriate puzzles of increasing difficulty. Parents were told that this was a task for the child to complete but that they could provide any assistance they deemed necessary. All interactions lasted 10 minutes and were videotaped for later coding by an ethnically diverse team of coders who were blind to other information about the families. Using seven global rating scales (Cox & Crnic, 2002: sensitivity/responsiveness, detachment/disengagement, intrusiveness, stimulation of cognitive development, positive regard, negative regard, and animation) adapted from those used by the National Institute for Child Health and Human Development Study of Early Child Care (National Institute for Child Health and Human Development Early Child Care Research Network, 1999), coders rated parenting behaviors on a 5-point scale (on which 1 = not at all characteristic and 5 = very characteristic). Informed by an exploratory factor analysis with an oblique rotation (i.e., promax), the individual subscales were composited to obtain overall sensitive parenting and harsh intrusive parenting scores; only the harsh intrusive maternal parenting composite (the mean of intrusiveness and negative regard) was used in these analyses. Parents given a score of 5 on the intrusiveness subscale consistently displayed behaviors that showed a lack of respect for the child as an individual. These mothers frequently interfered with the child’s needs, desires, and interests, and they denied almost all of their attempts at autonomy, often persisting with their own desires or agenda despite strong child defensive behavior (e.g., crying, withdrawing, verbalizing that they would like her to stop). Example behaviors include physically manipulating the child’s hands or body, denying the child the opportunity to select the toys/pieces to use or the opportunity to try to interact with the toys or complete the task themselves, and verbally directing the child at a pace and in a context that was not appropriate to the child’s cues. The negative regard subscale captured the amount of negative and hostile maternal behaviors that were directed toward the target child during the activity. Example behaviors include expressing disapproval through irritated or harsh comments and/or vocal tone, tense facial muscles or posture meant to communicate a threat or disapproval, threatening or punishing the child without explanation, or calling the child unflattering names. In our sample, parents assigned a 5 on this subscale typically displayed harsh, disapproving comments and behaviors consistently throughout the task in addition to exhibiting more severe forms of hostility, such as threatening or striking the child. Interrater reliabilities, assessed using intraclass correlations across each pair of coders, were .80, .79, and .86 for the 6-, 15-, and 24-month timepoints. At each timepoint, coders underwent training until acceptable reliability (intraclass correlation >.80) was achieved and maintained for each coder on every scale. Once acceptable reliability was established, coders began coding in pairs while continuing to code at least 20% of their weekly cases with a criterion coder. Reliability was based on the independent scores of coders. Each coding pair met biweekly to reconcile scoring discrepancies; the final consensus scores were used in all analyses.
Control Variables
Demographic variables
At each visit, mothers reported information on a variety of household demographic variables, including the total household income from all possible sources, the number of individuals living in the home, and the race of the target child. Income-to-needs ratios were calculated at each assessment timepoint by dividing the total household income from all possible sources by the federally determined poverty threshold for the number of people living in the household for that year. Income-to-needs ratios above 1.0 indicate that a family is able to provide for basic needs, whereas values below 1.0 indicate that they are not. Income-to-needs ratios at the different timepoints were highly correlated (rs ranged from .71 to .81 in our subsample); thus, only the 6-month income-to-needs ratio was used in the current analyses. These demographic variables, in addition to the data collection site (North Carolina vs. Pennsylvania), were used as control variables in all analyses.
Maternal perceptions of social support
When the children were 6 and 24 months old, maternal perception of social support was assessed using the 16-item modified version of the Questionnaire on Social Support (Crnic, Greenberg, Ragzin, Robinson, & Basham, 1983), which asks mothers about their satisfaction with the quality of their community involvement, friendships, family, and intimate relationships. Mothers were asked to rate, on a 5-point Likert-type scale (on which 1 = very dissatisfied and 5 = very satisfied), how satisfied they were with their current situation. An example item reads, “If you were to become upset or angry, would you have someone to talk honestly to, who is not involved? How satisfied are you with this situation?” We used the mean of the Community Involvement, Friendships, Family, and Intimate Relationships subscales from the 6-and 24-month timepoints as covariates in the current analyses. Cronbach’s alphas for this 15-item composite score for our sample were .82 and .79 for the 6- and 24-month timepoints, respectively. Unfortunately, the Questionnaire on Social Support was not administered to mothers at the 15-month timepoint. Because maternal perceptions of social support showed moderate stability from 6 to 24 months (r = .46, p < .01), we used the 6-month assessment of social support as a covariate for both the 6-and 15-month timepoints, whereas we used the 24-month assessment of social support as a covariate for the 24-month variables.
Analytic Strategy
We used a cross-lagged autoregressive path model to test our research question. The model was estimated with the Mplus 6.0 software package (Muthén & Muthén, 2010), using the robust maximum likelihood estimator. This estimator accommodates nonnormal data by adjusting standard errors using the Huber–White sandwich estimator. All results presented are fully standardized. Full information maximum likelihood was used as the missing-data technique (Arbuckle, 1996). Model fit was examined using a number of fit indices, including the comparative fit index (CFI; Bentler, 1990), the Tucker–Lewis index (TLI; Tucker & Lewis, 1973), and the root-mean-square error of approximation (RMSEA; Browne & Cudeck, 1993). CFI and TLI values above .90 and RMSEA values below .05 indicate adequate model fit.
To examine the nature of the relations among IPV, maternal depressive symptoms, and maternal harsh intrusive parenting, a number of paths were estimated between study variables. First, autoregressive paths were estimated between the different timepoints of IPV, maternal depressive symptoms, and maternal parenting behaviors; that is, the 24-month assessment of each construct was regressed onto the 15-month assessment of that construct, and the 15-month assessment of each construct was regressed onto the 6-month assessment of that construct (e.g., 24-month maternal parenting was regressed onto 15-month maternal parenting, and 15-month maternal parenting was regressed onto 6-month maternal parenting). These paths account for the stability in each of these constructs over time. Second, within-time variables were correlated (e.g., 6-month depressive symptoms were correlated with both 6-month IPV and 6-month maternal harsh intrusive parenting behaviors, and 6-month IPV was correlated with maternal harsh intrusive parenting) in order to account for the interdependence of the three variables at each of the timepoints. Next, cross-lagged paths were placed among variables such that all 6-month variables were used to predict all 15-month variables, and all 15-month variables were used to predict all 24-month variables. Last, paths were estimated between the control variables and each of the nine focal variables. Nonsignificant paths from the control variables to the focal variables were removed from the final model in order to preserve model parsimony.
Results
The means, standard deviations, and bivariate correlations among all study variables are shown in Table 1. Associations among variables were largely as expected, such that intimate partner physical violence was positively associated with both maternal depressive symptoms and maternal harsh intrusive parenting. Depressive symptoms were also associated with more maternal harsh intrusive parenting behaviors. IPV, maternal depressive symptoms, and maternal harsh intrusive parenting all showed stability over time, as evidenced by significant positive correlations among the three assessments of each construct. Consistent with previous literature, the families’ income-to-needs ratios were significantly correlated with IPV, maternal depressive symptoms, and maternal harsh intrusive parenting, such that higher income was associated with less IPV, fewer depressive symptoms, and less maternal harsh intrusive parenting. Child’s race was significantly correlated with both IPV and maternal harsh intrusive parenting (such that African American mothers tended to be exposed to more IPV and tended to be rated as higher on maternal harsh intrusive parenting), but it was not consistently related to maternal depressive symptoms scores. Maternal perception of social support was negatively associated with IPV and maternal depressive symptoms and initial levels of harsh intrusive parenting behaviors.
Table 1.
Descriptive Statistics and Bivariate Correlations Among Dependent and Independent Variables (N = 705)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. 6-m physical violence | — | ||||||||||||
| 2. 15-m physical violence | .68** | — | |||||||||||
| 3. 24-m physical violence | .49** | .47** | — | ||||||||||
| 4. 6-m depressive symptoms | .22** | .20** | .13** | — | |||||||||
| 5. 15-m depressive symptoms | .35** | .41** | .23** | .51** | — | ||||||||
| 6. 24-m depressive symptoms | .21** | .24** | .16** | .37** | .41** | — | |||||||
| 7. 6-m harsh intrusive parenting | .17** | .12** | .18** | .09* | .13** | .10* | — | ||||||
| 8. 15-m harsh intrusive parenting | .11** | .11** | .08* | .08* | .09* | .04 | .37** | — | |||||
| 9. 24-m harsh intrusive parenting | .23** | .20** | .15** | .10* | .22** | .16** | .32** | .46** | — | ||||
| 10. Income-to-needs ratio | −.16** | −.16** | −.16** | −.15** | −.15** | −.16** | −.22** | −.23** | −.27** | — | |||
| 11. Child’s racea | .21** | .20** | .24** | .00 | .10** | −.01 | .27** | .24** | .27** | −.24** | — | ||
| 12. 6-m perceived social support | −.18** | −.10* | −.21** | −.36** | −.31** | −.24** | −.08* | −.02 | −.04 | .07 | −.02 | — | |
| 13. 24-m perceived social support | −.12* | −.11** | −.12** | −.22** | −.16** | −.28** | −.03 | .12 | −.01 | .05 | .02 | .46** | — |
| M | 0.22 | 0.18 | 0.17 | 1.86 | 2.16 | 1.99 | 2.23 | 2.13 | 2.20 | 2.36 | — | 3.33 | 3.29 |
| SD | 0.55 | 0.59 | 0.58 | 0.77 | 0.78 | 0.69 | 0.67 | 0.79 | 0.76 | 1.02 | — | 0.55 | 0.50 |
Note: m = month.
0 = White 1 = African American.
p < .05.
p < .01.
IPV Model
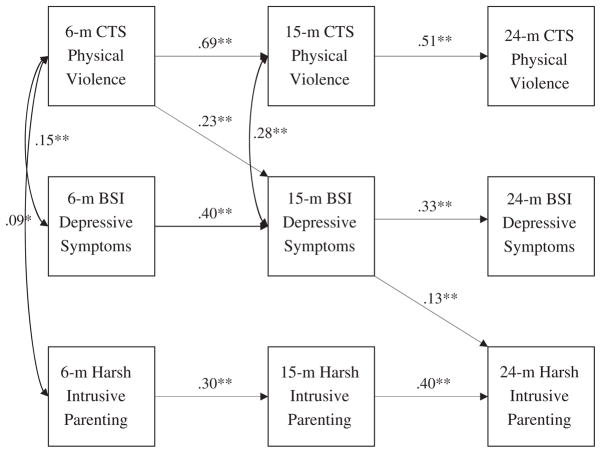
The following paths from the control variables to the nine focal variables were significant and thus were retained in the final model. The family’s income-to-need ratio was negatively associated with harsh intrusive parenting at the 6-month (β = −.16, p < .01), 15-month (β = −.12, p < .01), and 24-month (β = −.14, p < .01) assessments; with maternal depressive symptoms at the 6-month (β = −.13, p < .01) and 24-month (β = .40, p < .01) assessments; and with IPV at the 6-month (β = −.10, p < .01) and 24-month (β = −.06, p < .01) assessments. Child race (0 = White, 1 = African American) was positively associated with harsh intrusive parenting behaviors at the 6-month (β = .13, p < .01), 15-month (β = .16, p < .01), and 24-month (β = .07, p < .05) assessments, in addition to intimate partner physical violence at the 6-month (β = .22, p < .01) and 24-month (β = .14, p < .05) assessments. Maternal perceptions of social support were associated with IPV at the 6-month (β = −.18, p < .01) assessment, maternal depressive symptoms at the 6-month (β = −.37, p < .01), 15-month (β = −.13, p < .01), and 24-month (β = −.14, p < .01) assessments; and maternal harsh intrusive parenting behaviors at the 6-month (β = −.13, p < .01) assessment. Last, the data collection site was significantly associated with IPV at the 6-month (β = .07, p < .01) assessment, maternal depressive symptoms at the 6-month (β = .10, p < .01) and 24-month (β = .12, p < .01) assessments, and maternal harsh intrusive parenting behaviors at the 6-month assessment (β = −.13, p < .01). The final model fit was adequate, χ2 (33, N = 705) = 85.76, p = .00, CFI = .95, TLI = .90, RMSEA = .04. As can be seen in Figure 2 (in which only significant paths are depicted), even after accounting for the stability of each construct over time and the correlation among constructs at each wave (and controlling for the family’s income-to-needs ratio, the child’s race, maternal perceptions of social support, and the data collection site), higher levels of reported IPV when the child was 6 months old were associated with increases in maternal depressive symptoms when the child was 15 months old (β = .23, p < .01), which in turn were associated with increases in maternal harsh intrusive parenting at the 24-month assessment (β = .13, p < .01); that is, it appears that the impact of early IPV on later maternal parenting behaviors is indirect, operating through increased maternal depressive symptoms. This indirect path (from 6-month IPV, through 15-month maternal depressive symptoms, to 24-month maternal harsh intrusive parenting) was statistically significant (β = .04, p < .01).
Figure 2.
Final Model Relating Intimate Partner Physical Violence, Maternal Depressive Symptoms, and Maternal Harsh Intrusive Parenting.
Note: χ2(33, N = 705) = 85.76, p = .00, comparative fit index (CFI) = .95, Tucker – Lewis Index (TLI) = .90, root-mean-square error of approximation (RMSEA) = .04. CTS Physical Violence = Physical Violence subscale of the Conflict Tactics Scale – Couple Form R; BSI Depressive Symptoms = Depression Subscale of the Brief Symptom Inventory; Harsh intrusive Parenting = harsh intrusive composite score from the parent – child interaction; m = month. All paths depicted are standardized and significant. When this model was rerun with paternal CTS Violence scores instead, all depicted paths remained significant and similar in magnitude, χ 2(28, N = 223) = 36.75, p = .00, CFI = .98, TLI = .95, RMSEA = .04. *p < .05. **p < .01.
To strengthen our confidence in the presented results (because of concerns related to the common reporter bias), we also estimated a model using paternal report of IPV instead of maternal report. Because fathers’ data were not missing at random (as discussed in the Method section), we were unable to use a missing-data technique when estimating this model. Although this resulted in a small subsample of families, this model fit the data well, χ2(28, n = 223) = 36.75, p = .12, CFI = .98, TLI = .95, RMSEA = .04. All paths depicted in Figure 2 remained significant and stayed very similar in magnitude, suggesting that our finding of a link between IPV and maternal depressive symptoms likely is not exclusively due to the fact that mothers reported on both IPV and their depressive symptoms.
Discussion
Using a sample of coresiding, biological parents living in rural communities, in the current study we sought to investigate the nature of the relations among intimate partner physical violence, maternal depressive symptoms, and maternal harsh intrusive parenting behaviors during the first 2 years of a child’s life. The results indicate that, after taking into account the stability in each construct over time, their intercorrelation at a given time, and the potentially transactional nature of these variables over time, higher levels of IPV when the children were 6 months old were associated with increases in maternal depressive symptoms when the children were 15 months old, which were in turn associated with increases in maternal harsh intrusive parenting when the children were 24 months old. These results are consistent with our hypothesis that IPV would be the control parameter at this time in development; that is, in this population-based sample of families living in rural communities, IPV appears to be linked with increases in maternal depressive symptoms, thereby creating a cascade effect that places parenting at risk. This finding suggests that efforts aimed at alleviating the depressive symptoms of mothers of young children should also consider the climate of their romantic relationship, because treatment that does not consider the overarching influence of this control parameter may not be as effective as treatment that does take into account the presence of IPV.
Our results did not provide any support for bidirectional associations among the three focal variables during the first 2 years of the children’s life; that is, although we estimated all theoretically plausible paths (i.e., all of those depicted in Figure 1) and allowed for the possibility of bidirectional associations, only the paths depicted in Figure 2 were statistically significant, supporting the idea of a control parameter. These findings are consistent with past research concluding that the primary direction of this effect is from IPV to depressive symptoms (e.g., Beach et al., 1990; Proulx et al., 2007); however, given that different control parameters gain salience at different points in development (Cox et al., 2010), it is possible that the relations among these variables will change over time. Examination of these relations at different points in development may therefore be important to undertake, because they may yield different results.
Past research suggests several potential explanations for these findings. For example, it has been suggested that IPV may lead to increased risk of depressive symptoms by discouraging the individual from seeking support for his or her spouse (Choi & Marks, 2008) and by limiting available spousal support (Beach et al., 1990), which in turn may deplete parental coping resources and increase parental stress. This proposition is supported by researchers who have found longitudinal associations between IPV and parenting stress (e.g., Holden & Ritchie, 1991), as well as those who have found that depression mediates the linkage between IPV and parenting stress (Renner, 2009). In a complementary line of research, the stress process framework (Pearlin, Menaghan, Lieberman, & Mullan, 1981) posits that strains in key social roles, including the spousal role, can cause stress that typically manifests in mental health difficulties, including depressive symptoms. This increase in depressive symptoms, it would follow, may affect harsh maternal parenting behaviors; that is, the negative, angry, and coercive behaviors often associated with depressive symptoms may carry over into a mother’s interactions with her child, and the withdrawn, listless, depressive mood often experienced by these same mothers may deplete their ability to respond sensitively to the child and may contribute to self-doubt or less self-efficacious beliefs about their abilities as a parent (Cohn et al., 1990; Lyons-Ruth et al., 2000; Rutter, 1990; Teti & Gelfand, 1991).
This study adds to the extant literature in a number of ways. Using data from a large, ethnically and economically diverse population-based sample, we were able to expand our understanding of the interrelationships among three potentially deleterious influences on child development. Because the existing data on these variables have largely been cross-sectional (Proulx et al., 2007; Zlotnick et al., 2006), the current study’s multiple assessment points over the first 2 years of the children’s life, in addition to its analytic strategy (which allowed us to rule out alternative explanations or characterizations of the direction of these effects), provide some insight into how these relationships operate in an understudied community sample.
Despite its contributions, this study also has a number of limitations. These findings generalize only to coresidential biological parents living in rural communities. Future research should examine these relationships among non-residential partners and among partners whose relationships dissolve over time. Also, despite the strengths of the cross-lagged autoregressive path model (including its ability to determine the directionality of the effect), this is not a causal model. Although a significant path coefficient in this context indicates that the exogenous variable predicts the endogenous variable, the extent to which one can infer causality depends on the study’s design. Given that we did not manipulate any of our study variables, this remains correlational research and should be treated as such. The fact that we summed mothers’ reports of their and their partners’ physical violence was additionally limiting in that we did not make a distinction between mothers who were victims of domestic violence, those who committed violent acts against their partners, and those who were involved in mutually violent relationships. Making this distinction in our sample, however, proved to be quite difficult, because of the large number of families in which mothers reported that both they and their partners had committed violent acts. Past research has suggested that these different types of violence have different causes and consequences for both mothers and children (Johnson, 2008); however, given that less than 10% of our families in which IPV occurred reported that the father was the sole perpetrator of violence (n = 30, a figure consistent with Johnson’s report of IPV in community samples), we were unable to make this distinction in the current study. Given the fact that mothers are affected by the overall climate of their romantic relationship, we felt that this compositing was appropriate for testing our research question. Future research, however, should explore the possibility that the perpetrator’s identity may moderate the aforementioned relationships.
Additionally limiting is the fact that our study did not incorporate a measure of the severity of the IPV experienced by the mother; instead, we relied on the frequency of physically violent acts perpetrated by either partner in the past year. Although post hoc analyses did not suggest that these relationships varied for mothers who reported more severe violent acts (e.g., being choked, beaten up, threatened with a knife or gun) than those reporting less severe violent acts, the role of the severity of the IPV should be explored in future studies.
The magnitude of the parameter estimates produced in this model also requires some discussion. Although the path coefficients are modest in magnitude, coefficients around this size are common when using this type of model. Likely an artifact of the great stability in each construct over time (in that a large amount of the variability in the next timepoint is already explained by the previous timepoint, thereby not leaving much unique variance to be explained by other factors), significant effects of this magnitude are often still considered meaningful. Please see Cui, Donnellan, and Conger (2007) for a more thorough discussion of the importance of small effect sizes produced by a similar autoregressive path model.
Perhaps the most striking limitation of this study is the fact that mothers reported both on IPV and on their depressive symptoms, and thus there may be a common reporter bias. Although mothers may inaccurately or unintentionally underreport instances of violence (Jouriles, McDonald, Norwood, & Ezell, 2001), violence is not a dimension of conflict that can be induced in a laboratory setting. Although not without flaw, the CTS has been shown to have good predictive power compared with other methods of assessing violence (see Kitzmann et al., 2003, for a discussion), and thus it seemed a good option for our purposes. Additionally concerning is the fact that mothers may have reported on their experiences of IPV when their partner was present in the home. Although mothers completed the CTS-R using a laptop computer while seated away from the other household members, they may not have felt comfortable truthfully reporting on physical violence while their partner was present. As mentioned in the Results section, in order to strengthen our confidence in the presented results we estimated all models a second time using paternal report of IPV instead of maternal report. The fact that our findings remain largely the same when using fathers’ and mothers’ reports of IPV, in addition to the fact that maternal and paternal reports were significantly correlated in our sample, strengthens our confidence in the accuracy of our measurement.
Conclusions and Implications
The current study adds to the literature by examining the longitudinal relations among IPV, maternal depressive symptoms, and maternal harsh intrusive parenting behaviors over the first 2 years of a child’s life. The results of this study suggest that the impact of intimate partner physical violence on later maternal harsh intrusive parenting behaviors operates through its impact on intermediary maternal depressive symptoms. These findings suggest that clinicians and agencies who serve individuals living in physically violent homes may want to simultaneously assess and target IPV, maternal depressive symptoms, and child-directed aggression. These findings also underscore the importance of simultaneously considering multiple relationships within the family, in addition to the connections between different forms of family aggression, in order to better treat and understand the influence of intimate partner physical violence on maternal parenting and psychological functioning.
Acknowledgments
The Family Life Project Key Investigators include Lynne Vernon-Feagans, Martha Cox, Clancy Blair, Peg Burchinal, Linda Burton, Keith Crnic, Nan Crouter, Patricia Garrett-Peters, Doug Granger, Mark Greenberg, Stephanie Lanza, Adele Miccio, Roger Mills-Koonce, Deborah Skinner, Cynthia Stifter, Lorraine Taylor, Emily Werner, and Mike Willoughby. This research was supported by a grant from the National Institute of Child Health and Human Development (PO1-HD-39667), with cofunding from the National Institute on Drug Abuse.
References
- Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling. Mahwah, NJ: Erlbaum; 1996. pp. 243–277. [Google Scholar]
- Archer J. Sex differences in aggression between heterosexual partners: A meta-analytic review. Psychological Bulletin. 2000;126:651–680. doi: 10.1037/0033-2909.126.5.651. [DOI] [PubMed] [Google Scholar]
- Barnett MA, Deng M, Mills-Koonce W, Willoughby M, Cox M. Interdependence of parenting of mothers and fathers of infants. Journal of Family Psychology. 2008;22:561–573. doi: 10.1037/0893-3200.22.3.561. [DOI] [PubMed] [Google Scholar]
- Beach SRH, Sandeen E, O’Leary KD. Depressive symptoms in marriage. New York: Guilford Press; 1990. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Burchinal M, Vernon-Feagans L, Cox M The Family Life Project Investigators . Cumulative social risk, parenting, and infant development in rural low-income communities. Parenting. 2008;8:41–69. doi: 10.1080/15295190701830672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L. The impact of maternal depressive symptoms on familial relationships. International Review of Psychiatry. 2003;15:243–255. doi: 10.1080/0954026031000136866. [DOI] [PubMed] [Google Scholar]
- Caetano R, Vaeth PAC, Ramisetty-Mikler S. Intimate partner violence victim and perpetrator characteristics among couples in the United States. Journal of Family Violence. 2008;23:507–518. doi: 10.1007/s10896-008-9178-3. [DOI] [Google Scholar]
- Callahan CM, Wolinsky FD. The effect of gender and race on the measurement properties of the CES–D in older adults. Medical Care. 1994;32:341–356. doi: 10.1097/00005650-199404000-00003. [DOI] [PubMed] [Google Scholar]
- Campbell JC. Health consequences of intimate partner violence. The Lancet. 2002;359:1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Kub J, Belknap RA, Templin T. Predictors of depression in battered women. Violence Against Women. 1997;3:271–293. doi: 10.1177/1077801297003003004. [DOI] [Google Scholar]
- Choi H, Marks NF. Marital conflict, depressive symptoms, and functional impairment. Journal of Marriage and Family. 2008;70:377–390. doi: 10.1111/j.1741-3737.2008.00488.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn JF, Campbell SB, Matias R, Hopkins J. Face-to-face interactions of postpartum depressed and nondepressed mother–infant pairs at 2 months. Developmental Psychology. 1990;26:15–23. doi: 10.1037/0012-1649.26.1.15. [DOI] [Google Scholar]
- Cox MJ, Crnic K. Unpublished manuscript. University of North Carolina; Chapel Hill: 2002. Qualitative ratings for parent–child interaction at 3–12 months of age. [Google Scholar]
- Cox MJ, Harter KSM. Parent–child relationships. In: Bornstein MH, Davidson L, Keyes CLM, Moore KA, editors. Well-being: Positive development across the life course. Mahwah, NJ: Erlbaum; 2003. pp. 191–204. [Google Scholar]
- Cox MJ, Mills-Koonce WR, Propper CB, Gariepy J-L. Systems theory and cascades in developmental psychopathology. Development and Psychopathology. 2010;22:497–506. doi: 10.1017/S0954579410000234. [DOI] [PubMed] [Google Scholar]
- Cox MJ, Paley B. Families as systems. Annual Review of Psychology. 1997;48:243–267. doi: 10.1146/annurev.psych.48.1.243. [DOI] [PubMed] [Google Scholar]
- Cox MJ, Paley B. Understanding families as systems. Current Directions in Psychological Science. 2003;12:193–196. doi: 10.1111/1467-8721.01259. [DOI] [Google Scholar]
- Cox MJ, Paley B, Burchinal M, Payne CC. Marital perceptions and interactions across the transition to parenthood. Journal of Marriage and the Family. 1999;61:611–625. doi: 10.2307/353564. [DOI] [Google Scholar]
- Cox MJ, Paley B, Harter K. Intimate partner conflict and parent–child relationships. In: Grych J, Fincham F, editors. Child development and intimate partner conflict. New York: Cambridge University Press; 2001. pp. 249–272. [Google Scholar]
- Crnic K, Greenberg M, Ragzin A, Robinson N, Basham N. Effects of stress and social supports in mothers in premature and full term infants. Child Development. 1983;54:209–217. doi: 10.2307/1129878. [DOI] [PubMed] [Google Scholar]
- Cui M, Donnellan MB, Conger RD. Reciprocal influences between parents’ marital problems and adolescent internalizing and externalizing behavior. Developmental Psychology. 2007;43:1544–1552. doi: 10.1037/0012-1649.43.6.1544. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Maternal depressive symptoms and child development. Journal of Child Psychology and Psychiatry. 1994;35:73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Marital conflict and children: An emotional security perspective. New York: Guilford Press; 2010. [Google Scholar]
- Dallaire DH, Weinraub M. The stability of parenting behaviors over the first 6 years of life. Early Childhood Research Quarterly. 2005;20:201–219. doi: 10.1016/j.ecresq.2005.04.008. [DOI] [Google Scholar]
- Davila J, Bradbury TN, Cohan CL, Tochluk S. Marital functioning and depressive symptoms: Evidence for a stress generation model. Journal of Personality and Social Psychology. 1997;73:849–861. doi: 10.1037/0022-3514.73.4.849. [DOI] [PubMed] [Google Scholar]
- Derogatis L. Brief Symptom Inventory. Vol. 18. Minneapolis, MN: NCS Pearson; 2000. [Google Scholar]
- DeVoe ER, Smith EL. The impact of domestic violence in urban preschool children: Battered mothers’ perspectives. Journal of Interpersonal Violence. 2002;17:1075–1101. doi: 10.1177/088626002236661. [DOI] [Google Scholar]
- Falconier MK, Epstein NB. Couples experiencing financial strain: What we know and what we can do. Family Relations. 2011;60:303–317. doi: 10.1111/j.1741-3729.2011.00650.x. [DOI] [Google Scholar]
- Fantuzzo J, Boruch R, Beriama A, Atkins M, Marcus S. Domestic violence and children: Prevalence and risk in five major cities. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:116–122. doi: 10.1097/00004583-199701000-00025. [DOI] [PubMed] [Google Scholar]
- Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence. 1999;14:99–132. doi: 10.1023/A:1022079418229. [DOI] [Google Scholar]
- Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- Holden GW, Ritchie KL. Linking extreme marital discord, child rearing, and child behavior problems: Evidence from battered women. Child Development. 1991;62:311–327. doi: 10.1111/j.1467-8624.1991.tb01533.x. [DOI] [PubMed] [Google Scholar]
- Holt S, Buckley H, Whelan S. The impact of exposure to domestic violence on children and young people: A review of the literature. Child Abuse & Neglect. 2008;32:797–810. doi: 10.1016/j.chiabu.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Huang C-C, Wang L-R, Warrener C. Effects of domestic violence on behavior problems in preschool-aged children: Do maternal mental health and parenting mediate the effects? Children and Youth Services Review. 2010;30:1317–1323. doi: 10.1016/j.childyouth.2010.04.024. [DOI] [Google Scholar]
- Johnson MP. A typology of domestic violence: Intimate terrorism, violent resistance, and situational couple violence. Boston: Northeastern University Press; 2008. [Google Scholar]
- Jouriles EN, McDonald R, Norwood WD, Ezell E. Issues and controversies in documenting the prevalence of children’s exposure to domestic violence. In: Graham-Bermann SA, Edleson JL, editors. Domestic violence in the lives of children: The future of research, intervention, and social policy. Washington, DC: American Psychological Association; 2001. pp. 12–34. [Google Scholar]
- Jouriles EN, McDonald R, Slep AMS, Heyman RE, Garrido E. Child abuse in the context of domestic violence: Prevalence, explanation, and practice implications. Violence and Victims. 2008;23:221–235. doi: 10.1891/0886-6708.23.2.221. [DOI] [PubMed] [Google Scholar]
- Keenan K, Wakschlag LS. More than the terrible twos: The nature and severity of behavior problems in clinic-referred preschool children. Journal of Abnormal Child Psychology. 2000;28:33–46. doi: 10.1023/A:1005118000977. [DOI] [PubMed] [Google Scholar]
- Kitzmann KM, Gaylord NK, Holt AR, Kenny ED. Child witnesses to domestic violence: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2003;71:339–352. doi: 10.1037/0022-006X.71.2.339. [DOI] [PubMed] [Google Scholar]
- Knickerbocker L, Heyman RE, Slep AMS, Jouriles EN, McDonald R. Co-occurrence of child and partner maltreatment. European Psychologist. 2007;12:36–44. doi: 10.1027/1016-9040.12.1.36. [DOI] [Google Scholar]
- Kouros CD, Papp LM, Cummings E. Interrelations and moderators of longitudinal links between marital satisfaction and depressive symptoms among couples in established relationships. Journal of Family Psychology. 2008;22:667–677. doi: 10.1037/0893-3200.22.5.667. [DOI] [PubMed] [Google Scholar]
- Lehrer J, Buka S, Gortmaker S, Shrier LA. Depressive symptomology as a predictor of exposure to IPV among US female adolescents and young adults. Archives of Pediatric and Adolescent Medicine. 2006;160:270–276. doi: 10.1001/archpedi.160.3.270. [DOI] [PubMed] [Google Scholar]
- Letourneau NL, Fedick CB, Willms JD. Mothering and domestic violence: A longitudinal analysis. Journal of Family Violence. 2007;22:649–659. doi: 10.1007/s10896-007-9099-6. [DOI] [Google Scholar]
- Levendosky AA, Graham-Bermann SA. Parenting in battered women: The effects of domestic violence on women and children. Journal of Family Violence. 2001;16:171–192. doi: 10.1023/A:1011111003373. [DOI] [Google Scholar]
- Levendosky AA, Huth-Bocks AC, Shapiro DL, Semel MA. The impact of domestic violence on the maternal–child relationship and preschool-age children’s functioning. Journal of Family Psychology. 2003;17:275–287. doi: 10.1037/0893-3200.17.3.275. [DOI] [PubMed] [Google Scholar]
- Levendosky AA, Leahy KL, Bogat G, Davidson WS, von Eye A. Domestic violence, maternal parenting, maternal mental health, and infant externalizing behavior. Journal of Family Psychology. 2006;20:544–552. doi: 10.1037/0893-3200.20.4.544. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/S0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Wolfe R, Lyubchik A. Depressive symptoms and the parenting of young children: Making the case for early preventive mental health services. Harvard Review of Psychiatry. 2000;8:148–153. doi: 10.1093/hrp/8.3.148. [DOI] [PubMed] [Google Scholar]
- Maccoby EE. Parenting and its effects on children: On reading and misreading behavior genetics. Annual Review of Psychology. 2000;51:1–29. doi: 10.1146/annurev.psych.51.1.1. [DOI] [PubMed] [Google Scholar]
- Margolin G, Gordis EB, Oliver PH. Links between marital and parent-child interactions: Moderating role of husband-to-wife aggression. Development and Psychopathology. 2004;16:753–771. doi: 10.1017/S0954579404004766. [DOI] [PubMed] [Google Scholar]
- Morewitz SJ. Domestic violence and maternal and child health. New York: Kluwer Academic/Plenum Press; 2004. [Google Scholar]
- Murry VM, Smith EP, Hill NE. Race, ethnicity and culture in studies of families in context. Journal of Marriage and Family. 2001;63:911–914. doi: 10.1111/j.1741-3737.2001.00911.x. [DOI] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles: Author; 2010. [Google Scholar]
- National Institute for Child Health, Human Development Early Child Care Research Network. Child care and mother–child interaction in the first 3 years of life. Developmental Psychology. 1999;35:1399–1413. doi: 10.1037/0012-1649.35.6.1399. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Proulx CM, Helms HM, Buehler C. Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family. 2007;69:576–593. doi: 10.1111/j.17413737.2007.00393.x. [DOI] [Google Scholar]
- Renner LM. Intimate partner violence victimization and parenting stress: Assessing the mediating role of depressive symptoms. Violence Against Women. 2009;15:1380–1401. doi: 10.1177/1077801209346712. [DOI] [PubMed] [Google Scholar]
- Rutter M. Some focus and process considerations regarding effects of parental depression on children. Developmental Psychology. 1990;26:60–67. doi: 10.1037/h0092669. [DOI] [Google Scholar]
- Slep AMS, O’Leary SG. Examining partner and child abuse: Are we ready for a more integrated approach to family violence? Clinical Child and Family Psychology Review. 2001;4:87–107. doi: 10.1023/A:1011319213874. [DOI] [PubMed] [Google Scholar]
- Slep AMS, O’Leary SG. Parent and partner violence in families with young children: Rates, patterns, and connections. Journal of Consulting and Clinical Psychology. 2005;73:435–444. doi: 10.1037/0022-006X.73.3.435. [DOI] [PubMed] [Google Scholar]
- Stice E, Ragam J, Randall P. Prospective relations between social support and depression: Differential direction of effects for parent and peer support? Journal of Abnormal Psychology. 2004;113:155–159. doi: 10.1037/0021-843X.113.1.155. [DOI] [PubMed] [Google Scholar]
- Straus MA, Gelles RJ. Physical violence in American families: Risk factors and adaptations to violence in 8,145 families. New Brunswick, NJ: Transaction; 1990. [Google Scholar]
- Straus M, Kantor GK. Corporal punishment of adolescents by parents: A risk factor in the epidemiology of depression, child abuse, and wife beating. Adolescence. 1995;29:543–561. [PubMed] [Google Scholar]
- Sturge-Apple M, Davies PT, Cicchetti D, Manning LG. Mothers’ parenting practices as explanatory mechanisms in associations between interparental violence and child adjustment. Partner Abuse. 2010;1:45–60. doi: 10.1891/1946U82116560.1.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teti DM, Gelfand DM. Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Development. 1991;62:918–929. doi: 10.1111/j.1467-8624.1991.tb01580.x. [DOI] [PubMed] [Google Scholar]
- Teti DM, Gelfand DM, Pompa J. Depressed mothers’ behavioral competence with their infants: Demographic and psychosocial correlates. Development and Psychopathology. 1990;2:259–270. doi: 10.1017/S0954579400000766. [DOI] [Google Scholar]
- Thelen E, Smith LB. Dynamic systems theories. In: Damon W, Lerner RM, editors. Handbook of child psychology: Vol. 1. Theoretical models of human development. New York: Wiley; 1998. pp. 595–625. [Google Scholar]
- Towe-Goodman NR, Stifter CA, Coccia MA, Cox MJ. Interparental aggression, attention skills, and early childhood behavior problems. Development and Psychopathology. 2011;23:563–576. doi: 10.1017/S0954579411000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. doi: 10.1007/BF02291170. [DOI] [Google Scholar]
- Verhoeven M, Junger M, Van Aken C, Deković M, Van Aken MAG. Parenting during toddlerhood: Contributions of parental, contextual, and child characteristics. Journal of Family Issues. 2007;28:1663–1691. doi: 10.1177/0192513X07302098. [DOI] [Google Scholar]
- Wolfe DA, Crooks CV, Lee V, McIntyre-Smith A, Jaffe PG. The effects of children’s exposure to domestic violence: A meta-analysis and critique. Clinical Child and Family Psychology Review. 2003;6:171–187. doi: 10.1023/A:1024910416164. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Johnson DM, Kohn R. Intimate partner violence and long-term psychosocial functioning in a national sample of American women. Journal of Interpersonal Violence. 2006;21:262–275. doi: 10.1177/0886260505282564. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Kohn R, Peterson J, Pearlstein T. Partner physical victimization in a national sample of American families: Relationship to psychological functioning, psychosocial factors, and gender. Journal of Interpersonal Violence. 1998;13:156–166. doi: 10.1177/088626098013001009. [DOI] [Google Scholar]