Abstract
Background: Eating breakfast is believed to promote a healthy body weight. Yet, few studies have examined the contribution of energy balance–related behavioral factors to this relation in minority youth.
Objective: We assessed the associations between breakfast consumption and dietary intake, physical activity (PA), and adiposity before and after accounting for energy intake and PA in minority girls.
Design: Cross-sectional data were obtained on body mass index (BMI), percentage body fat (measured by BodPod), dietary intake (measured with 3-d dietary records), and PA (measured with 7-d accelerometry) from 87 Latina and African American girls 8–17 y of age (75% Latina, 80% overweight). Dietary records were used to categorize girls as more frequent breakfast eaters (MF; 2 or 3 of 3 d; n = 57) or less frequent breakfast eaters (LF; 0 or 1 of 3 d; n = 30). Chi-square tests, ANCOVA, and multiple regression analyses were conducted. Mediation was assessed with a Sobel test.
Results: Compared with the MF group, the LF group spent 30% less time (12.6 min/d) in moderate-to-vigorous-intensity PA (MVPA; P = 0.004) and had a higher percentage body fat (P = 0.029). MVPA accounted for 25% (95% CI: −8.8%, 58.1%; P = 0.139) of the relation between breakfast consumption and percentage body fat. We were unable to show that energy intake or MVPA was a significant mediator of the relation between breakfast consumption and adiposity in this sample.
Conclusions: Evidence suggests that among predominantly overweight minority girls, MVPA, but not energy intake, was associated with both breakfast consumption and adiposity; however, a lack of power reduced our ability to detect a significant mediation effect. Other unobserved variables likely contribute to this relation.
INTRODUCTION
The 2009–2010 prevalence rates of pediatric obesity in the United States indicate that 18.2% of children and adolescents 6–19 y of age were obese and 33.2% were overweight (1). Hispanic and non-Hispanic black youth are disproportionately affected, with prevalence rates of overweight and obesity of 41.2% and 41.8%, respectively, compared with non-Hispanic white youth of the same age group (29.0%) (1). Accordingly, 10–19-y-old ethnic minority youth, including Hispanics and African Americans, have the highest rates of type 2 diabetes in the United States (2). In response to these alarming statistics, a major focus of national public health efforts has been to gain a better understanding of the genetic, environmental, and behavioral factors related to pediatric obesity, particularly in minority populations.
Substantial evidence indicates that breakfast skipping is associated with adiposity in youth. In cross-sectional studies, increased frequency of breakfast skipping has been associated with a higher BMI (3–8) and greater visceral adiposity in adolescents (9). Prospective findings have been less consistent, with some (6, 10–14) but not all (3, 15, 16) observational studies showing that breakfast skipping promotes weight gain. Paradoxically, the average daily calorie intake among breakfast consumers generally exceeds that of breakfast skippers by 200–400 kcal/d (7, 8, 14). These findings suggest that the influence of breakfast consumption on weight regulation occurs through energy expenditure rather than restricted consumption. In fact, the effect of eating frequency on measures of adult adiposity has been shown to be confounded by physical activity (PA)5 energy expenditure and physical fitness (17). Yet, experimental studies of meal frequency and size on energy balance do not show significant differences in total daily energy expenditure related to meal skipping or gorging compared with snacking (18, 19). The lack of consistency in the literature indicates the need to better understand the energy balance–related factors associated with breakfast consumption and adiposity in youth.
Understanding how breakfast consumption is related to body weight, BMI, or percentage body fat in high-risk populations will provide useful information for developing behavioral interventions for obesity prevention. Therefore, the purpose of our study was to examine the relations between breakfast consumption, measures of adiposity, and typical dietary intake and PA in a sample of Latina and African American girls. Using a mediation framework, we also explored the contributing role that dietary intake and PA plays in the association between breakfast consumption and adiposity. We hypothesized that girls who consumed breakfast less frequently would have higher measures of adiposity and that this association would be explained, in part, by greater reported energy intake or lower levels of PA.
SUBJECTS AND METHODS
Participants
Participants were from 3 linked pediatric obesity studies that share a set of common methods and measures: Insulin Resistance and Declining Physical Activity Levels in African American and Latina Girls (recruitment approval date, 19 June 2006), Strength and Nutrition Outcomes for Latino Adolescents (NCT00697580), and Strength Training and Nutrition Development for African American Youth (NCT01441323). Participants in Strength Training and Nutrition Development for African American Youth were 8–11 y of age, and participants in Strength and Nutrition Outcomes for Latino Adolescents and Strength Training and Nutrition Development for African American Youth participants were 14–17 y of age.
The current study used cross-sectional data from the baseline measures of each of the 3 studies. Details of the study methods were published previously (20–23). Briefly, participants were recruited through medical clinics, churches, community centers, local schools, and advertisements in Los Angeles County, CA. Participants were excluded if they were using a medication; had a diagnosis of a condition known to influence body composition, fat distribution, or insulin/glucose metabolism; or had a diagnosis of diabetes based on fasting plasma glucose (≥126 mg/dL) at the time of entry into the study. Before any testing procedures were initiated, written informed consent and assent were obtained from all parents and children, respectively. Although 187 girls completed a baseline visit, clinical data (n = 29), 3 d of complete dietary records (n = 31), or accelerometry data (n = 40) were missing, which resulted in a final sample size of 87. The study protocols were standardized across the 3 studies and were individually approved by the Institutional Review Board at the University of Southern California Health Sciences Campus.
Measures
Anthropometric measures
Study participants arrived in the afternoon at the University of Southern California Clinical Trials Unit after a minimum of a 3-h fast. Weight and height were measured 3 times to the nearest 0.1 kg and 0.1 cm, respectively, with a beam medical scale and a wall-mounted stadiometer used by trained medical professionals. BMI z scores were computed. Determination of age- and sex-specific BMI percentiles was based on established CDC normative curves (24, 25). Participants with a BMI percentile ≥85% were categorized as overweight. Body composition (percentage body fat and percentage lean tissue) was measured by air plethysmography (BodPod; Life Measurements Instruments). Pubertal Tanner stage was assessed by a licensed pediatric health care provider (26).
Accelerometric measures
Objective assessments of PA were obtained by using a GT1M accelerometer (Actigraph). This uniaxial accelerometer measures acceleration in the vertical plane and has been shown to be a valid and reliable measure of PA for children and adolescents (27, 28). All participants were instructed to wear the device on the right hip under clothing (attached to an adjustable belt), except during water-based activities or when sleeping. Accelerometer data were downloaded and processed by using a modification of the SAS program developed for use with NHANES PA monitor data (http://riskfactor.cancer.gov/tools/nhanes_pam). The raw data were processed to calculate the minutes of wear and nonwear time (defined as ≥60 min of 1 to 100 counts with exceptions for up to 3 min of values >100 or 0 counts).
In keeping with prior research (29, 30), we defined a valid day of wear as ≥10 h of wear time, and only participants with ≥4 valid days of data were included in these analyses. Accelerometer data were collected in 15-s epochs and aggregated into 1-min epochs across the studies. The raw counts were categorized by intensity level (moderate intensity: 4 metabolic equivalent tasks; vigorous intensity: 7 metabolic equivalent tasks) by using age-adjusted thresholds developed by the Freedson group (31). Time spent in these activity intensities was summed and averaged across all valid days to create the mean minutes per day spent in moderate-to-vigorous intensity PA (MVPA).
Dietary intake
Typical energy intake (in kcal/d) and diet composition were estimated from dietary records collected over 2 weekdays and 1 weekend day. Dietary intake and accelerometry data were collected during the same period, but not necessarily on the same days. At the clinic visit, participants were given 3-d dietary records to complete at home before the next study visit and a 10-min lesson on how to complete the dietary records and estimate portion sizes. Measuring cups, spoons, and rulers were supplied to all participants to aid in accurate reporting. The completed dietary records were reviewed and clarified with each participant by trained research staff when they were collected.
Nutrition data were analyzed by using the Nutrition Data System for Research software (version 2008; Nutrition Coordinating Center at the University of Minnesota, Minneapolis, MN). Dietary data were carefully screened for plausibility through a multistep process. Participants’ comments were reviewed and clarified by trained project staff. All of the collected dietary data were used in the current analysis.
Breakfast consumption
Breakfast was defined as any food or beverage consumed between 0500 and 1000 with a combined total energy of ≥100 kcal (15, 32). Breakfast consumption was recorded as occurring 0, 1, 2, or 3 out of 3 d. Participants were divided into 2 breakfast-consumption categories based on the sample median (2 d, or 67% of the time). Girls who consumed breakfast less frequently (LF; n = 30) had eaten breakfast on 0 or 1 of the 3 d. Girls who consumed breakfast more frequently (MF; n = 57) had eaten breakfast on 2 or 3 of the 3 d.
Statistical analysis
Independent t tests and chi-square tests were used to compare demographic characteristics between the MF and LF groups. The main analyses were conducted by using a single-mediator model (see online supplemental material for a description of mediation analysis under “Supplemental data” in the online issue) (33). Before mediation analyses were conducted, significant relations between the predictor (eg, breakfast consumption frequency: LF and MF), the potential mediators (eg, PA and energy intake), and the outcome (eg, adiposity) were assessed through ANCOVA that included age, race, and BMI percentile as covariates. BMI was included only when measures of adiposity were not the outcome variables. Mediation parameters required to assess our hypothesized mediation effects were estimated for variables that showed associations with breakfast consumption and adiposity via covariate-adjusted multiple linear regression analyses. The magnitude of an observed mediation effect and the 95% 95% CI were estimated as the explained proportion of the total effect (34). A Sobel test was conducted to assess the significance of a mediation effect (35, 36).
All outcome variables were normally distributed, with the exception of vigorous-intensity PA and MVPA, which were square root transformed. For ease of interpretation, untransformed means are presented in the tables. Unadjusted and adjusted group means with 95% CIs and P values are presented. Estimates of effect size (η2) are provided in the text for significant ANCOVA test results. All analyses were conducted by using SPSS Statistics 17.0. Significance was set at P < 0.05.
RESULTS
The analytic sample (n = 87) consisted of Latina (75%) and African American girls with a mean (±SD) of 12.1 (± 3.1) y of age. Half of the sample was in Tanner stages I and II (53%), and most were classified as overweight (80%). Thirty-five percent of the sample (n = 30) was categorized as LF. No significant differences in age, Tanner stage, or BMI category distribution were found between breakfast groups (P > 0.05 for each comparison; data not shown). In addition, there were no unadjusted or adjusted group mean differences in total daily energy intake, macronutrient composition (dietary fat, carbohydrate, and protein), total fiber intake, or total sugar intake (Table 1).
TABLE 1.
Mean daily dietary intakes of Latina and African American girls 8–17 y of age, by less frequent or more frequent breakfast consumption1
| Unadjusted model |
Adjusted model2 |
|||||
| Intake | Less frequent | More frequent | P | Less frequent | More frequent | P |
| Total energy (kcal) | 1751 (1550, 1952) | 1737 (1591, 1883) | 0.911 | 1772 (1569, 1975) | 1726 (1579, 1872) | 0.714 |
| Dietary fat (% of energy) | 32.4 (30.3, 34.6) | 31.9 (30.4, 33.5) | 0.684 | 32.8 (30.8, 34.8) | 31.7 (30.3, 33.2) | 0.394 |
| Carbohydrate (% of energy) | 52.9 (50.5, 55.4) | 53.2 (51.4, 55.0) | 0.883 | 52.7 (50.2, 55.1) | 53.3 (51.5, 55.1) | 0.674 |
| Protein (% of energy) | 15.1 (13.8, 16.4) | 15.6 (14.6, 16.5) | 0.591 | 14.9 (13.7, 16.2) | 15.7 (14.7, 16.6) | 0.368 |
| Total fiber (g/1000 kcal) | 8.4 (7.4, 9.4) | 8.3 (7.6, 9.1) | 0.911 | 8.2 (7.2, 9.3) | 8.4 (7.7, 9.2) | 0.781 |
| Total sugar (g/1000 kcal) | 50.5 (42.6, 58.5) | 51.7 (45.9, 57.5) | 0.813 | 52.8 (46.4, 59.2) | 50.5 (45.9, 55.1) | 0.567 |
Values are means; 95% confidence limits in parentheses. Less frequent breakfast consumption was defined as eating breakfast 0 or 1 d of the 3 d (n = 30 girls). More frequent breakfast consumption was defined as eating breakfast 2 or 3 of the 3 d (n = 57 girls).
Adjusted for age, race, and BMI percentile. Group differences were tested by using ANCOVA.
Significant unadjusted group mean differences in accelerometer-measured moderate-intensity PA (P = 0.003, η2 = 0.098) and MVPA (P = 0.002, η2 = 0.106) were observed, which remained significant after age, race, and BMI percentile were included as covariates [P = 0.007 (η2 = 0.081) and P = 0.004 (η2 = 0.094), respectively] (Table 2). On average, the LF group spent 30% less time in MVPA (∼12.6 min/d) than did the MF group.
TABLE 2.
Mean daily physical activity of Latina and African American girls 8–17 y of age, by less frequent or more frequent breakfast consumption1
| Unadjusted model |
Adjusted model2 |
|||||
| Less frequent | More frequent | P | Less frequent | More frequent | P | |
| Physical activity intensity (min/d) | ||||||
| Moderate | 28.2 (22.2, 34.2) | 39.7 (35.4, 44.1) | 0.003 | 29.0 (23.1, 35.0) | 39.3 (35.0, 43.6) | 0.007 |
| Vigorous | 1.4 (−0.4, 3.2) | 2.4 (1.1, 3.7) | 0.117 | 1.8 (0, 3.6) | 2.2 (1.0, 3.5) | 0.289 |
| Moderate to vigorous | 29.6 (22.5, 36.7) | 42.2 (37.0, 47.3) | 0.002 | 30.8 (23.8, 37.8) | 41.6 (36.5, 46.6) | 0.004 |
Values are means; 95% confidence limits in parentheses. Less frequent breakfast consumption was defined as eating breakfast 0 or 1 d of the 3 d (n = 30 girls). More frequent breakfast consumption was defined as eating breakfast 2 or 3 of the 3 d (n = 57 girls).
Adjusted for age, race, and BMI percentile. Group differences were tested by using ANCOVA.
Unadjusted analyses indicated that the LF group had a higher mean percentage body fat (P = 0.013, η2 = 0.069) than did the MF group, which remained significant after the inclusion of age and race as covariates (P = 0.029, η2 = 0.053) (Table 3). The additional inclusion of total energy intake as a covariate did not attenuate the association between breakfast consumption and percentage body fat (P = 0.026, η2 = 0.055). However, in a separate model, the inclusion of MVPA as a covariate rendered this association nonsignificant. Overweight, mean BMI z score, and mean BMI percentile did not differ significantly between the LF and MF groups (Table 3).
TABLE 3.
Measures of adiposity in Latina and African American girls 8–17 y of age, by less frequent or more frequent breakfast consumption1
| Unadjusted model |
Adjusted model2 |
Adjusted means3 |
Adjusted means4 |
|||||||||
| Measure | Less frequent | More frequent | P | Less frequent | More frequent | P | Less frequent | More frequent | P | Less frequent | More frequent | P |
| Overweight | 90.0% | 75.4% | 0.103 | |||||||||
| BMI z score | 1.8 (1.6, 2.1) | 1.4 (1.3, 0.7) | 0.083 | 1.8 (1.5, 2.1) | 1.6 (1.4, 1.8) | 0.157 | 1.8 (1.5, 2.1) | 1.6 (1.4, 1.7) | 0.149 | 1.8 (1.5, 2.0) | 1.6 (1.4, 1.8) | 0.298 |
| BMI percentile | 92.5 (86.6, 98.3) | 87.9 (83.6, 92.1) | 0.207 | 91.4 (86.0, 96.7) | 88.4 (84.6, 92.3) | 0.381 | 91.4 (86.0, 96.8) | 88.4 (84.5, 92.3) | 0.375 | 90.7 (85.2, 96.3) | 88.8 (84.8, 92.7) | 0.632 |
| Body fat (%) | 37.2 (33.5, 41.0) | 31.3 (28.6, 34.1) | 0.013 | 36.1 (33.1, 39.1) | 31.9 (29.7, 34.1) | 0.029 | 36.2 (33.1, 39.2) | 31.9 (29.7, 34.1) | 0.026 | 35.4 (32.3, 38.5) | 32.3 (30.1, 34.5) | 0.112 |
Values are means; 95% confidence limits in parentheses. Less frequent breakfast consumption was defined as eating breakfast 0 or 1 d of the 3 d (n = 30 girls). More frequent breakfast consumption was defined as eating breakfast 2 or 3 d of the 3 d (n = 57 girls).
Adjusted for age and race.
Adjusted for age, race, and total energy intake (in kcal).
Adjusted for age, race, and moderate-to-vigorous-intensity physical activity. Group differences were tested by using chi-square independence tests (proportions of overweight) and ANCOVA.
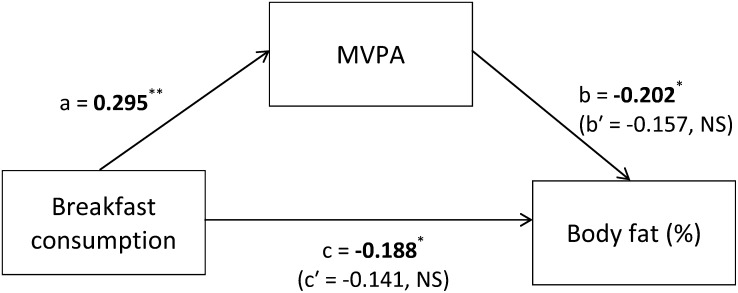
The significant interrelations between breakfast consumption, MVPA, and body fat, which were important to establish mediation, were reexamined through a series of multiple regression models (Figure 1). A significant association was found between breakfast consumption and percentage body fat after control for age and race (β = −0.188, P = 0.029) as previously described in the statistically equivalent ANCOVA. Additional age- and race-adjusted regression analyses showed significant associations between breakfast consumption and MVPA (β = 0.295, P = 0.004) and MVPA and percentage body fat (β = −0.202, P = 0.024). In the mediation analysis, MVPA explained 25% (95% CI: −8.8%, 58.1%) of the relation between breakfast consumption and percentage body fat, which resulted in an attenuated association between the 2 variables (β = −0.141, P = 0.112); however, the mediation effect was not significant (Sobel test: P = 0.139). The nonsignificant mediation effect can be explained, in part, by the nonsignificant association between MVPA and percentage body fat after adjustment for breakfast consumption (β = −0.157, P = 0.090). A mediation effect for energy intake was similarly not observed (−2.0%; 95% CI: −14.7%, 10.8%; P = 0.757).
FIGURE 1.
Mediation model of the effect of MVPA on the association between breakfast consumption and percentage body fat. Values in boldface type represent standardized, age- and race-adjusted associations between breakfast consumption and MVPA (total effect, a), MVPA and percentage body fat (total effect, b), and breakfast consumption and percentage body fat (total effect, c). Values in parentheses represent standardized age- and race-adjusted associations between breakfast consumption and percentage body fat with control for the hypothesized mediator, MVPA (direct effect, c′), and between MVPA and percentage body fat with control for breakfast consumption (direct effect, b′). The indirect or mediation effect (ab′) was −0.046 and nonsignificant as assessed with the Sobel test: t = −1.48; 95% CI: −2.48, −0.12; P = 0.139. *P < 0.05, **P < 0.01. MVPA, moderate-to-vigorous-intensity physical activity.
DISCUSSION
Using a mediation framework, we examined the relation between breakfast consumption and measures of adiposity to assess the contributing role of typical dietary intake and PA in a sample of Latina and African American girls. We found that eating breakfast less frequently was associated with higher percentage body fat and with spending nearly 30% less time in MVPA but not with energy intake or macronutrient composition in this population. However, we were unable to detect a 25% mediation effect of MVPA on the relation between breakfast consumption and percentage body fat with our limited sample size (P = 0.139). Collectively, these findings suggest that frequency of breakfast consumption is associated with adiposity and MVPA in this population. MVPA may partially mediate the relation between breakfast consumption and adiposity; however, on the basis of the observed magnitude of the effect, it is likely that other unobserved variables, such as socioeconomic factors (37), further explain this relation.
We did not detect an association between average daily energy intake or macronutrient composition and typical breakfast consumption. Our hypothesis was based on a review of the literature on breakfast habits of youth (8) and recent findings from a similarly aged nationally representative sample that suggested that breakfast skippers consume 200–400 kcal/d more than non–breakfast skippers (7). One explanation for our null finding could be that, compared with other studies, our study sample had a greater proportion of overweight girls and lacked variation between groups. Sex could similarly moderate this association. Alternatively, differences in our definition and categorization of breakfast consumption frequency compared with other studies, or possible dietary recall biases (eg, underreporting), might have masked a significant finding in our study. Therefore, we cannot definitively conclude from this study that dietary intake does not contribute to the association between breakfast frequency and adiposity.
As hypothesized, we observed an association between breakfast consumption and MVPA. The MF group spent ∼13 more minutes a day (or 30%) in MVPA than did the LF group. Similar in magnitude to the current findings, a large cross-sectional study of 1860 Pakistani children (5–12 y of age) also demonstrated an inverse association between breakfast skipping and MVPA >2 d/wk (self-reported; OR ratio: 0.63; 95% CI: 0.45, 0.89) (38). A study of 877 British adolescents (14 y of age) found that, among girls, eating breakfast infrequently was associated with lower levels of total PA (accelerometry measured), but only during the morning (39). The mechanisms that link breakfast consumption with PA have yet to be explored; however, studies of the effect of breakfast consumption on cognitive function related to perceived alertness, energy (40, 41), and fatigue (40, 42, 43) or the clustering patterns of these energy balance–related behaviors (44–46) could help to inform future research.
Consistent with other research (9), we found that girls who ate breakfast less frequently had a greater percentage body fat; however, we were unable to detect a statistically significant mediation effect of MVPA on this association despite significant separate associations of MVPA with breakfast consumption and percentage body fat (5). Support of this hypothesis would have been consistent with the results of a longitudinal study of 2361 adolescent girls (12). Albertson et al (12) showed that both energy intake and PA, both measured by 3-d dietary records, mediated the association between breakfast eating and BMI over time, but the magnitude and significance of the mediation effects were not tested. Furthermore, at the end of the 10-y study, among the girls who had a high BMI at baseline, those who ate breakfast more frequently had a lower BMI than did those who ate breakfast less frequently. Inconsistencies in the findings between the study by Albertson et al (12) and our study could have be a result of the cross-sectional compared with longitudinal nature of the studies or sample demographics or PA measurement methods; however, it was more likely that we lacked the power to detect the modest 25% mediation effect given the wide CI (95% CI: −8.8%, 58.1%). Post hoc power analyses indicated that 133 participants would be required to detect a mediation effect of this magnitude with 80% power. Although we were unable to detect significant effects of dietary intake or PA on the association between breakfast consumption and percentage body fat in this population, most of the evidence supports the promotion of breakfast consumption for weight control, particularly among overweight youth. Additional studies using a mediation framework on the contribution of energy balance–related or socioeconomic, cultural, or psychological factors to the link between breakfast consumption and adiposity is warranted.
To our knowledge, this was the first study to explore the association of breakfast frequency with energy intake, PA, and measures of adiposity in a minority sample of girls at high risk of obesity. The use of accelerometers removed some of the biases associated with self-reported measures, such as recall and social desirability, although some issues of measurement error remain. Similarly, our method for assessing breakfast was relatively objective. We obtained 3-d dietary records of dietary intake and applied a predetermined definition of breakfast to assess the frequency of breakfast eating during the record period. In addition, our sample had a large proportion of overweight girls, which allowed us to test previously observed associations from samples with large variations in body size in a more homogeneous population of high-risk minority girls.
Despite the many strengths of the current study, it also had limitations. The generalizability of the findings is limited to Latinas and African American girls 8–11 and 13–17 y of age. The relatively small sample size precluded the inclusion of more categories of breakfast frequency and reduced the power to detect a mediation effect of MVPA, which could explain some of the discrepancies in our findings compared with those of other researchers. Last, because of the cross-sectional design of our study, we were unable to make conclusions about causal effect that breakfast eating might have on energy intake, PA, or weight change. Furthermore, without temporally ordered variables and no independent associations of breakfast consumption and MVPA with percentage body fat observed in the mediation analysis, it is difficult to conclude from this cross-sectional study that MVPA, rather than breakfast consumption, is the true mediator. Future research will be needed to replicate these findings in larger longitudinal and intervention studies.
The findings of this study contribute to the evidence suggesting that eating breakfast more frequently is associated with higher levels of PA and lower levels of adiposity among minority girls. We estimate that 25% of the association between breakfast consumption and percentage body fat was explained by MVPA in a population of predominantly overweight Latina and African American girls; however, a lack of power reduced our ability to detect a significant mediation effect. Although these results do not conclusively show a statistically significant contribution of MVPA (or dietary intake) to the link between breakfast consumption and adiposity, public health messages should continue to encourage regular breakfast consumption as a method to promote healthy lifestyles and lower levels of adiposity.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—SMS, CKW, and ES: contributed to the analysis and interpretation of the data and the writing and revisions of the manuscript; ES, JND, STN-R, BRB, Y-WH, and DS-M: contributed to the interpretation of the data and the writing and revisions of the manuscript; and MJW, MIG, and DS-M: contributed to the design of the experiment, analysis of the data, and revisions of the manuscript. None of the authors had any conflicts of interest to report.
Footnotes
Abbreviations used: LF, less frequent; MF, more frequent; MVPA, moderate-to-vigorous-intensity physical activity; PA, physical activity.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA 2012;307:483–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dabelea D, Bell RA, D'Agostino RB, Jr, Imperatore G, Johansen JM, Linder B, Liu LL, Loots B, Marcovina S, et al. Incidence of diabetes in youth in the United States. JAMA 2007;297:2716–24. [DOI] [PubMed] [Google Scholar]
- 3.Barton BA, Eldridge AL, Thompson D, Affenito SG, Striegel-Moore RH, Franko DL, Albertson AM, Crockett SJ. The relationship of breakfast and cereal consumption to nutrient intake and body mass index: the National Heart, Lung, and Blood Institute Growth and Health Study. J Am Diet Assoc 2005;105:1383–9. [DOI] [PubMed] [Google Scholar]
- 4.Dubois L, Girard M, Potvin Kent M, Farmer A, Tatone-Tokuda F. Breakfast skipping is associated with differences in meal patterns, macronutrient intakes and overweight among pre-school children. Public Health Nutr 2009;12:19–28. [DOI] [PubMed] [Google Scholar]
- 5.Roseman MG, Yeung WK, Nickelsen J. Examination of weight status and dietary behaviors of middle school students in Kentucky. J Am Diet Assoc 2007;107:1139–45. [DOI] [PubMed] [Google Scholar]
- 6.Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics 2008;121:e638–45. [DOI] [PubMed] [Google Scholar]
- 7.Deshmukh-Taskar PR, Nicklas TA, O'Neil CE, Keast DR, Radcliffe JD, Cho S. The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999-2006. J Am Diet Assoc 2010;110:869–78. [DOI] [PubMed] [Google Scholar]
- 8.Rampersaud GC, Pereira MA, Girard BL, Adams J, Metzl JD. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc 2005;105:743–60. [DOI] [PubMed] [Google Scholar]
- 9.Alexander KE, Ventura EE, Spruijt-Metz D, Weigensberg MJ, Goran MI, Davis JN. Association of breakfast skipping with visceral fat and insulin indices in overweight Latino youth. Obesity (Silver Spring) 2009;17:1528–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haines J, Neumark-Sztainer D, Wall M, Story M. Personal, behavioral, and environmental risk and protective factors for adolescent overweight. Obesity (Silver Spring) 2007;15:2748–60. [DOI] [PubMed] [Google Scholar]
- 11.Tin SPP, Ho SY, Mak KH, Wan KL, Lam TH. Breakfast skipping and change in body mass index in young children. Int J Obes (Lond) 2011;35:899–906. [DOI] [PubMed] [Google Scholar]
- 12.Albertson AM, Franko DL, Thompson D, Eldridge AL, Holschuh N, Affenito SG, Bauserman R, Striegel-Moore RH. Longitudinal patterns of breakfast eating in black and white adolescent girls. Obesity (Silver Spring) 2007;15:2282–92. [DOI] [PubMed] [Google Scholar]
- 13.Niemeier HM, Raynor HA, Lloyd-Richardson EE, Rogers ML, Wing RR. Fast food consumption and breakfast skipping: predictors of weight gain from adolescence to adulthood in a nationally representative sample. J Adolesc Health 2006;39:842–9. [DOI] [PubMed] [Google Scholar]
- 14.Berkey CS, Rockett H, Gillman M, Field A, Colditz G. Longitudinal study of skipping breakfast and weight change in adolescents. Int J Obes Relat Metab Disord 2003;27:1258–66. [DOI] [PubMed] [Google Scholar]
- 15.Affenito SG, Thompson DR, Barton BA, Franko DL, Daniels SR, Obarzanek E, Schreiber GB, Striegel-Moore RH. Breakfast consumption by African-American and white adolescent girls correlates positively with calcium and fiber intake and negatively with body mass index. J Am Diet Assoc 2005;105:938–45. [DOI] [PubMed] [Google Scholar]
- 16.Elgar FJ, Roberts C, Moore L, Tudor-Smith C. Sedentary behaviour, physical activity and weight problems in adolescents in Wales. Public Health 2005;119:518–24. [DOI] [PubMed] [Google Scholar]
- 17.Duval K, Strychar I, Cyr MJ, Prud'homme D, Rabasa-Lhoret R, Doucet E. Physical activity is a confounding factor of the relation between eating frequency and body composition. Am J Clin Nutr 2008;88:1200–5. [DOI] [PubMed] [Google Scholar]
- 18.Bellisle F, McDevitt R, Prentice AM. Meal frequency and energy balance. Br J Nutr 1997;77(suppl 1):S57–70.. [DOI] [PubMed] [Google Scholar]
- 19.Taylor MA, Garrow JS. Compared with nibbling, neither gorging nor a morning fast affect short-term energy balance in obese patients in a chamber calorimeter. Int J Obes Relat Metab Disord 2001;25:519–28. [DOI] [PubMed] [Google Scholar]
- 20.Davis JN, Kelly LA, Lane CJ, Ventura EE, Byrd-Williams CE, Alexandar KA, Azen SP, Chou CP, Spruijt-Metz D, Weigensberg MJ, et al. Randomized control trial to improve adiposity and insulin resistance in overweight Latino adolescents. Obesity (Silver Spring) 2009;17:1542–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ventura E, Davis J, Byrd-Williams C, Alexander K, McClain A, Lane CJ, Spruijt-Metz D, Weigensberg M, Goran M. Reduction in risk factors for type 2 diabetes mellitus in response to a low-sugar, high-fiber dietary intervention in overweight Latino adolescents. Arch Pediatr Adolesc Med 2009;163:320–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA 2010;303:242–9. [DOI] [PubMed] [Google Scholar]
- 23.Shahabi A, Bernstein L, Azen SP, McClain AD, Belcher B, Hsu YW, Nguyen-Rodriguez ST, Spruijt-Metz D. Recruitment and retention of African American and Latino preadolescent females into a longitudinal biobehavioral study. Ethn Dis 2011;21:91–8. [PMC free article] [PubMed] [Google Scholar]
- 24.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. CDC growth charts: United States. Adv Data 2000;Jun 8:1–27. [PubMed] [Google Scholar]
- 25.Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, Grummer-Strawn LM, Curtin LR, Roche AF, Johnson CL. Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics 2002;109:45–60. [DOI] [PubMed] [Google Scholar]
- 26.Tanner JM. Growth and maturation during adolescence. Nutr Rev 1981;39:43–55. [DOI] [PubMed] [Google Scholar]
- 27.Puyau MR, Adolph AL, Vohra FA, Zakeri I, Butte NF. Prediction of activity energy expenditure using accelerometers in children. Med Sci Sports Exerc 2004;36:1625–31. [PubMed] [Google Scholar]
- 28.Trost SG, Ward DS, Moorehead SM, Watson PD, Riner W, Burke JR. Validity of the computer science and applications (CSA) activity monitor in children. Med Sci Sports Exerc 1998;30:629–33. [DOI] [PubMed] [Google Scholar]
- 29.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008;40:181–8. [DOI] [PubMed] [Google Scholar]
- 30.Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol 2008;167:875–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trost SG, Pate RR, Sallis JF, Freedson PS, Taylor WC, Dowda M, Sirard J. Age and gender differences in objectively measured physical activity in youth. Med Sci Sports Exerc 2002;34:350–5. [DOI] [PubMed] [Google Scholar]
- 32.Siega-Riz AM, Popkin BM, Carson T. Trends in breakfast consumption for children in the United States from 1965-1991. Am J Clin Nutr 1998;67:748S–56S. [DOI] [PubMed] [Google Scholar]
- 33.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–82. [DOI] [PubMed] [Google Scholar]
- 34.Mackinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behav Res 1995;30:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation modeling. : Leinhardt S, ed. Sociological methodology 1982. Washington, DC: Jossey-Bass, 1982:290–312. [Google Scholar]
- 36.Sobel ME. Some new results on indirect effects and their standard errors in covariance structure models. : Tuma N, ed. Sociological methodology 1986. Washington, DC: American Sociological Association, 1986:159–86. [Google Scholar]
- 37.Magnusson MB, Sjoberg A, Kjellgren KI, Lissner L. Childhood obesity and prevention in different socio-economic contexts. Prev Med 2011;53:402–7. [DOI] [PubMed] [Google Scholar]
- 38.Mushtaq MU, Gull S, Mushtaq K, Shahid U, Shad MA, Akram J. Dietary behaviors, physical activity and sedentary lifestyle associated with overweight and obesity, and their socio-demographic correlates, among Pakistani primary school children. Int J Behav Nutr Phys Act 2011;8:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corder K, van Sluijs EM, Steele RM, Stephen AM, Dunn V, Bamber D, Goodyer I, Griffin SJ, Ekelund U. Breakfast consumption and physical activity in British adolescents. Br J Nutr 2011;105:316–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cooper SB, Bandelow S, Nevill ME. Breakfast consumption and cognitive function in adolescent schoolchildren. Physiol Behav 2011;103:431–9. [DOI] [PubMed] [Google Scholar]
- 41.Kral TV, Heo M, Whiteford LM, Faith MS. Effects on cognitive performance of eating compared with omitting breakfast in elementary schoolchildren. J Dev Behav Pediatr 2012;33:9–16. [DOI] [PubMed] [Google Scholar]
- 42.Tanaka M, Mizuno K, Fukuda S, Shigihara Y, Watanabe Y. Relationships between dietary habits and the prevalence of fatigue in medical students. Nutrition 2008;24:985–9. [DOI] [PubMed] [Google Scholar]
- 43.Sweeney NM, Tucker J, Reynosa B, Glaser D. Reducing hunger-associated symptoms: the midmorning nutrition break. J Sch Nurs 2006;22:32–9. [DOI] [PubMed] [Google Scholar]
- 44.Hoyland A, Dye L, Lawton CL. A systematic review of the effect of breakfast on the cognitive performance of children and adolescents. Nutr Res Rev 2009;22:220–43. [DOI] [PubMed] [Google Scholar]
- 45.Ottevaere C, Huybrechts I, Benser J, De Bourdeaudhuij I, Cuenca-Garcia M, Dallongeville J, Zaccaria M, Gottrand F, Kersting M, Rey-Lopez JP, et al. Clustering patterns of physical activity, sedentary and dietary behavior among European adolescents: the HELENA study. BMC Public Health 2011;11:328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kremers SPJ, De Bruijn GJ, Schaalma H, Brug J. Clustering of energy balance-related behaviours and their intrapersonal determinants. Psychol Health 2004;19:595–606. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.