Abstract
Background:
Human immunodeficiency virus (HIV) is a public health challenge facing both developing and developed nations. Although injecting drug use is even the main route of HIV transmission in Iran, sexual route is rising gradually. Vulnerable women have been considered as important bridging population for driving HIV epidemics. To increase the access to vulnerable women, in 2007, 5 pilot centers were established in risky areas to deliver comprehensive services to women who themselves or their spouses are engaged in drug use, risky sexual behavior or have history of imprisonment. Management of Sexually Transmitted Infection, psychological counseling and harm reduction are provided by female staff. The aim of this study was to report the activities conducting in 2008.
Methods:
Registered information was used to assess the demographic characteristic, HIV/ AIDS related risk factors and services delivered to clients.
Results:
Till March 2008, 442 clients have been admitted. Most of them (36.2%) had 25–34 years old. 14.3% were illiterate and 31% were totally jobless. The most prevalent risk factors were risky sexual behavior (27.1%) and non-injecting drug use (23.2%). Injecting drug use was detected in 11.3% of attendees. Dividing clients according to marital status, risky sexual behavior was the main risk factor in unmarried (40.2%) and divorced (26.9%) but in married and widow ones, non-injecting drug use was the most (25.8% and 36.5% respectively). Harm reduction (40.5%) and counseling (36.6%) were the most delivered services.
Conclusion:
Since vulnerable women play a critical role to spread HIV-epidemic to general population, increasing centers provide more access to this population.
Keywords: HIV, AIDS, High risk behavior, Women, Iran
Introduction
Epidemics of HIV/ AIDS in Middle East and North Africa region are mainly concentrated in IDUs, men who have sex with men, sex workers and their clients. In some countries, high levels of HIV infection have been identified in networks of drug users (1).
Iran is situated in this region. After the first HIV case detection in 1986, Iran has faced a concentrated HIV epidemic among IDUs since 2000s. The response of the government has focused on this diagnosed high risk populations, mostly young male drug users. By June 2011, based on data collected from provincial levels, a total of 23125 HIV-positive cases have been identified in Iran. Among those, the most common mode of transmission (69.8%) is the shared use of needles among IDUs. Sexual contact and mother-to-child transmission have been diagnosed in 10% and 0.8% respectively. Comparing to cumulative HIV/AIDS cases, newly detected ones in 2010 were attributed to injecting drug use (66.4%), sexual contact (21.1%) and mother-to-child transmission (2.5%). The figures show that although the route of HIV transmission in the majority of newly diagnosed cases remains through injecting drug use, the role of sexual transmission has increased over the time (from 4.2% of newly diagnosed HIV cases in 2001 to 21.1% in 2010). In the same time, the proportion of women has increased gradually in all registered cases from 4.69% in 2001 to 8.5 % in 2010 (2).
The high level of HIV infection among IDUs is also a great concern because of the possibility of transmission through the infected IDUs to their sexual partners (3–5).
A study in Tehran showed that many IDUs in the sample have had multiple sex partners and condom use has not been well adopted, as about half of sexually active male IDUs reported never having used a condom in their lifetime (6).
Women are more vulnerable to HIV infection in many ways like biological susceptibility to HIV (7), less access to employment and education specially in developing countries, generally lower levels of literacy and incomes and some other reasons. Discrimination between sexes also exists, and community pays more attention to men than to women (8). On the other hand, some barriers may restrict women and cause less access to HIV care and affordable medical services (9).
The high risk behaviour of female sex workers, female drug users, and wives/partners of male drug users have therefore necessarily become an important focus of current concern to minimize the epidemic spreading to the general population (10, 11). So based on these evidences, it was realized that a comprehensive services needed to be established to ensure that vulnerable women, as a key bridging group for the transmission of HIV between IDUs and general population, have access to appropriate prevention and care services.
Materials and Methods
In 2006, a sex rapid assessment and response was carried out to answer some questions about high risk sexual behavior and its determinants in Iran. According to its valuable findings, in 2007–08, after advocating all decision and policy makers including religious leaders and governors, 5 “Counseling and Harm Reduction centers” for vulnerable women were established in risky areas in 4 provinces as a pilot phase. Vulnerable women were defined as women with high risk sexual behavior, drug use and history of imprisonment. Presence of these risk factors in women’s spouses were also put them in our target group. HIV/AIDS related education, Harm Reduction including needle and syringe program, condom distribution, psychological and mental counseling, STI management, Methadone Maintenance Therapy (MMT) and referral system to” voluntary counseling & testing centers” and other health facilities were given by female staff.
This study wants to determine demographic characteristics and main risky behaviors among clients and to show the role of these centers to provide more access to services for vulnerable women. We reviewed the registered data in 5 pilot centers establishing in 2007–08. The assessed variables were Age, Marital status, Education, Occupation, high risk behaviors and services distributing to clients. High risk behaviors contained injecting and non injecting drug use, risky sexual behavior and history of imprisonment in women or in their spouses.
Data were presented as percentages for categorical variables. Analyses were carried out using SPSS version 15.0.
Results
Generally, 442 people had been admitted in these centers until March 2008. Baseline characteristics of clients have been summarized in Table 1. Among 5 age groups, the most prevalent age was 25–34 years (36.2%) and 35–44 years (34.8%). The study showed that 45.2% of clients were living with their spouses although totally 83% of clients had history of marriage. Divorced women contributed 26% of recorded files.
Table 1:
Descriptive statistics of clients in specific centers for vulnerable women
| Number Total:442 | Percent (%) | |||
|---|---|---|---|---|
| Age (year) | < 15 | 2 | 0.5 | |
| 15–24 | 91 | 20.6 | ||
| 25– 34 | 160 | 36.2 | ||
| 35– 44 | 154 | 34.8 | ||
| ≥ 45 | 35 | 7.9 | ||
| Marital Status | Unmarried | 75 | 17 | |
| Married | Living with spouses | 200 | 45.2 | |
| Divorced | 115 | 26 | ||
| Widow | 52 | 11.8 | ||
| Education | Illiterate | 63 | 14.3 | |
| Low educated | 322 | 72.9 | ||
| Literate | Diploma | 43 | 9.7 | |
| High educated | 14 | 3.2 | ||
| Occupation | Jobless | 137 | 31 | |
| House wife | 180 | 40.7 | ||
| Employed | 125 | 28.3 |
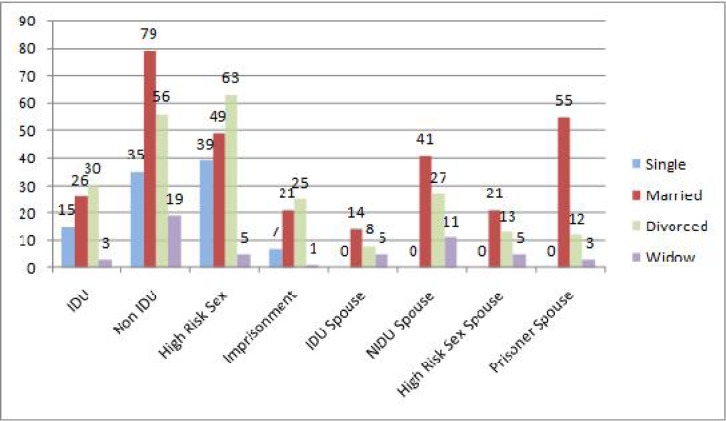
Fourteen percent of clients were illiterate and 12.9 % have diploma or university education. In all, 28.3% had job and 31% were totally jobless. The most risky behaviors were high risk sexual contact (27.1%) and non injecting drug use (23.2%); we detected that 11.6% of clients were IDUs. In general, 20% of risk factors among vulnerable women were related to their spouses. Distribution of risk factors according to marital status was shown in Fig. 1.
Fig. 1:
Distribution of risk factors according to marital status in “Counseling and Harm Reduction Centers for vulnerable Women”
Regarding marital status, high risk sexual behavior was the most risk factor in unmarried women (40.2%) and divorced ones (26.9%) but in widows and women living with their spouses, non injecting drug use had the highest prevalence (corresponding values were 36.5% and 25.8% respectively). Data showed that the most values of high risk sexual behavior, history of imprisonment and Injecting Drug use were seen in divorced women (40.4%, 46.3% and 40.5% respectively) but non injecting drug use, were mainly detected in women living with spouses (41.8%).
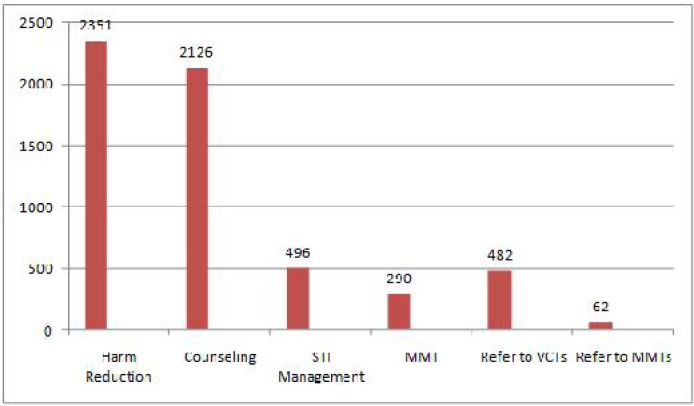
More than half of IDUs (55.2%) were unemployed while there was no important difference in the prevalence of high risk sexual behavior among employed (36.5%) and unemployed women (32.3%). Figure 2 shows the provided services to clients.
Fig. 2:
Delivered Services to clients in “Counseling and Harm Reduction Centers for vulnerable Women”
Totally, 5805 services had been offered to clients. Harm reduction was the most number (40.5%) and STI management contributed just 8.5% of services. Table 2 is related to delivered services providing to women by their risk factors. In all, the greatest part of counseling (44.6%) and Harm Reduction (58.1%) were delivered to women with high risk sexual behavior and IDUs respectively. In general, around one third of distributed services was counseling and 71.2% of high risk sexually women profited by it.
Table 2:
Delivered services to clients disaggregated by risk factors
| Harm Reduction | STI Management | Counseling | Refer to VCTs | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| No. | (%) | No. | (%) | No | (%) | No. | (%) | |
| IDU Spouses | 509 | (21.70) | 21 | (4.20) | 52 | (2.40) | 21 | (4.40) |
| Prisoner Spouses | 51 | (2.20) | 57 | (11.50) | 154 | (7.20) | 66 | (13.70) |
| High Risk Sex Spouses | 10 | (0.40) | 19 | (3.80) | 394 | (18.50) | 333 | (6.80) |
| NIDU *Spouses | 52 | (2.20) | 55 | (11.10) | 149 | (7.00) | 55 | (11.40) |
| IDUs | 1366 | (58.10) | 51 | (10.30) | 130 | (6.10) | 61 | (12.70) |
| NIDUs | 201 | (8.50) | 142 | (28.60) | 245 | (11.50) | 120 | (24.90) |
| High Risk Sex | 134 | (5.70) | 123 | (24.80) | 948 | (44.60) | 83 | (17.20) |
| History of Imprisonment | 28 | (1.20) | 28 | (5.60) | 54 | (2.50) | 43 | (8.90) |
NIDU: Non Injecting Drug Users
Discussion
Some studies have shown increasing pattern of HIV prevalence in women) 12–14). In 2009, according to UNAIDS information, the majority of detected HIV infections among females over 13 years were attributed to heterosexual contact for all age groups. The recorded statistics of HIV positive cases in Iran have shown increasing patterns in the proportion of women. On the other hand the HIV infections attributed to heterosexual contact is also increasing. The activities reducing stigma and discrimination may be considered as a reason for these trends.
According to” Modeling of New HIV Infections Based on exposure Groups in Iran”, we also predicted that the major route of direct and indirect transmission of HIV infection is unsafe injection (IDUs and their sexual partners) and sexual contact takes the second rank (15).
Our study showed that 11.3% of clients in these pilot centers were IDUs and in 2.6% of women, injecting drug use was detected in their spouses. Besides, risky sexual behavior was seen in 27.1% of women and it could be possible that their partners were IDUs in some sexual contacts; Regarding the IDU’s risky sexual behavior, it seems the establishment of these centers can be a good opportunity to increase access to these high risk groups.
As we revealed, the most clients were in 25–34 years and the most risky sexual behaviors were seen in this group. Data was in line with the other study which was conducted among vulnerable women in Zanjan in 2008. The study showed the average age of 28.4±7.9 (16). In 2006 general population and Housing census, near 57% of women aged more than 10 were living with their spouses. In our study we recognized that most clients (45.2%) were comprised of women who were living with their spouses. This could be affected by either more married than single women in urban society or indicate that these women have less stigma to go health centers. Although the proportion of divorce in urban women over 10 years is around 0.9%, 11.8% of our clients were divorced (17). Regarding the most prevalent of risky sexual behavior (40.4%), injecting drug use (40.5%) and prison history (46.3%) in this group, it is clear that health providers should be trained to detect and counsel them properly.
Women have less access to employment and education in developing countries. Lack of education and economic security impresses many women, whose literacy levels are generally lower than men (9). In this study we detected 14.3% illiteracy among vulnerable women. A population-based household survey in 5 cities and 5 villages in Iran showed that the level of health literacy as the scale of capacity to get, development, and comprehend basic health information is low particularly in women. 17% of study population was illiterate and educational level was the most important determinant of health literacy (18). In our study the largest proportion of illiteracy was seen in 35–44 years old and the least value was in less than 25. These figures are in line with the decreasing pattern of illiteracy among women in Iran. It was shown that female literacy rate doubled in both rural and urban areas from 1976 to 1986. By 1996, the literacy rate for all women over than six years old was 74% and 62% in urban and rural women respectively. Female enrollment at the elementary and middle-school levels reached to 100% in 1996 (19). According to the 2008 UNAIDS global figures, only 38% of young women have correct, comprehensive knowledge of HIV/AIDS. Since HIV/AIDS is related to literacy, by its reasonable level, we should seize the opportunity to increase the knowledge of HIV/AIDS in vulnerable women.
Poverty increases vulnerability to HIV/AIDS (20–21) and HIV burden is focused in the poorest areas of some countries. The chance of multiple partnerships for women is related to negative economic shocks (22).
Based on National Statistical Centre of Iran, the unemployment rate in the fourth quarter of 2006 was 12.1%. In our study, 71.7% of clients had no definite source of income. These socioeconomic conditions are often distinguished as a primary cause for women’s involvement in sex work and unprotected sex accordingly (23, 24). Increasing access to services for women by dropping financial barriers in access to services was recommended. It can be done in health care setting through special programs which can provide economic opportunities for women (e.g. skills training) (9). In these regards, these pilot centres were established to increase the access of women to different services providing there.
As we showed the most risk factors among vulnerable women were high risk sexual behavior (27.1%). The other prevalent risky behavior was non injecting drug use which usually is either a cause or an effect of sex work. Some studies revealed the strong link between female criminal activity and female drug involvement (25, 26).
Although in this study, we could not measure the overlaps between these two risk factors, a study in Tehran has shown that 85.3% of Vulnerable women in the study had experiences of drug use and 68.8% of participants were addicted to drugs at the time of research (27).
Regarding services providing to clients, harm reduction had the most frequent. Although STI management is one of the most important objectives and the risk of HIV transmission increases in presence of STIs, just 8.5% of services were attributed to STI management. We must consider that attention to other activities and requests for them should not affect on STI evaluation and treatment. Personnel should be trained and sensitized on role of proper STI management in both HIV and STI control programs (28–30).
Generally, it seems that based on available data, in line with the main objective of establishing these centers, which is more access to vulnerable women; these centres could find the target group correctly and provide them with bases of different services in this regard. Service providers should be trained to do more effectively. It is clear that besides increasing these centers and strengthening them on how to have more access to high risk population, we might partly overcome the third wave of HIV which threatens our community. One of the most important issues in increasing access to this hard to reach group is to provide Stigma free services.
There were several potential limitations in our study. Since these centers were newly established without any similar experience in the region, there were not registered data as much as we reported (because of not using unique reporting forms at time of the study). Developing the first national protocol has been finished in 2010 and it will be revised based on field experiences. A complementary study is recommended to renew this information and make us able to compare the findings. Knowledge and HIV related behaviors, heterogeneity among vulnerable women in terms of their behaviors and some important questions can be mentioned in future studies.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc) have been completely observed by the authors.
Acknowledgments
We express our appreciation to the focal points of HIV/ AIDS program in provincial level for collecting information and Health care providers in those centers who kindly delivered services to clients. The authors declare that there is no conflict of interest.
References
- 1.UNAIDS report on the Global AIDS Epidemic 2010. Available from: www.unaids.org/globalreport/documents/2010.
- 2.Ministry of Health and Medical Education HIV/AIDS Statistics in Iran 2011.
- 3.Panda S, Kumar MS, Lokabiraman S, Jayashree K, Satagopan MC, Solomon S, et al. Risk factors for HIV infection in injection drug users and evidence for onward transmission of HIV to their sexual partners in Chennai, India. J Acquir Immune Defic Syndr. 2005;39(1):9–15. doi: 10.1097/01.qai.0000160713.94203.9b. [DOI] [PubMed] [Google Scholar]
- 4.Gyarmathy VA, Neaigus A. Marginalized and socially integrated groups of IDUs in Hungary: potential bridges of HIV infection. J Urban Health. 2005;82(3 suppl 4):101–12. doi: 10.1093/jurban/jti112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strathdee SA. Sexual HIV transmission in the context of injection drug use: implications for interventions. Int J Drug Policy. 2003;14:79–81. [Google Scholar]
- 6.Zamani S, Kihara M, Gouya MM, Vazirian M, et al. High Prevalence of HIV Infection Associated With Incarceration Among Community-Based Injecting Drug Users in Tehran, Iran. J Acquir Immune Defic Syndr. 2006;42:342–46. doi: 10.1097/01.qai.0000219785.81163.67. [DOI] [PubMed] [Google Scholar]
- 7.Turmen T. Gender and HIV/AIDS. International Journal of Gynecology & Obstetrics. 2003;82:411–18. doi: 10.1016/s0020-7292(03)00202-9. [DOI] [PubMed] [Google Scholar]
- 8.Pourreza A, Batebi A, Moussavi P. A Survey about Knowledge and Attitudes of People towards Violence against Women in Community/ Family Settings. Iranian J Publ Health. 2004;33(2):33–37. [Google Scholar]
- 9.Anonymous 2011. World Health Organization (WHO): Gender inequalities and HIV. Available from: www.who.int/gender/hiv_aids.
- 10.McClelland GM, Teplin LA, Abram KM, Jacobs N. HIV and AIDS Risk Behaviors Among Female Jail Detainees: Implications for Public Health Policy. Am J Publ Health. 2002;92(5):818–25. doi: 10.2105/ajph.92.5.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spittal PM, Craib KJP, Wood E, Laliberte N, Li K, Tyndall MW, et al. Risk factors for elevated HIV incidence rates among female injection drug users in Vancouver. CMAJ. 2002;166(7):894–99. [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenberg PS, Biggar RJ, Goedert JJ, Gail MH. Trends in HIV Incidence Among Young Adults in the United States. JAMA. 1998;279(23):1894–1899. doi: 10.1001/jama.279.23.1894. [DOI] [PubMed] [Google Scholar]
- 13.Asamoah Odei E, Garcia Calleja JM, Boerma JT. HIV prevalence and trends in sub-Saharan Africa: no decline and large subregional differences. Lancet. 2004;364(9428):35–40. doi: 10.1016/S0140-6736(04)16587-2. [DOI] [PubMed] [Google Scholar]
- 14.Taha TE, Dallabetta GA, Hoover DR, Chiphangwi JD, Mtimavalye LA, Liomba GN, et al. Trends of HIV-1 and sexually transmitted diseases among pregnant and postpartum women in urban Malawi. AIDS. 1998;12(2):197–203. doi: 10.1097/00002030-199802000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Haghdoost AA, Nasirian M. Modeling of New HIV Infections Based on exposure Groups in Iran. 1st ed. Medical University of Kerman, Fanoos Inc; Kerman: 2011. [Google Scholar]
- 16.Tavasoli S, Shoghli AR. High risk behavior among vulnerable women in Zanjan (Doctoral Thesis) Zanjan University of Medical Sciences; Iran: 2008. [Google Scholar]
- 17.Anonymous Statistical Center Of Iran. General population and Housing census. 2006. Available from: www.amar.org.ir.
- 18.Tehrani A, Amirkhani MA, Haghdoost AA, Alavian M, Asgharifard H, Barghamdi M, et al. Health Literacy and the Influencing Factors: A Study in Five Provinces of Iran. Strides in Development of Medical Education. 2007;4(1):1–9. [Google Scholar]
- 19.Aghajanian A, Merhyar AH. Fertility, Contraceptive Use and Family Planning Program Activity in the Islamic Republic of Iran. International Family Planning Perspectives. 1999;25(2):98–102. [Google Scholar]
- 20.Quinn TC, Overbaugh J. HIV/AIDS in Women: An Expanding Epidemic. Science. 2005;308(5728):1582–83. doi: 10.1126/science.1112489. [DOI] [PubMed] [Google Scholar]
- 21.United Nations Publication Population, Development and HIV/AIDS with particular emphasis on poverty: The concise report. 2005. Available from: http://www.un.org/esa/population/publications/concise2005/PopdevHIVAIDS.
- 22.Dinkelman T, Lam D, Leibbrandt M. Household and community income, economic shocks and risky sexual behavior of young adults; evidence from the Cape Area Panel Study 2002 and 2005. AIDS. 2007;21(7):49–56. doi: 10.1097/01.aids.0000300535.05226.a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.UNICEF Poverty drives Kenyan girls into sex work. 2008. Available from: http://www.unicef.org/infobycountry.
- 24.Reed E, Gupta J, Biradavolu M, Devireddy V, Blankenship KM. The Context of Economic Insecurity and Its Relation to Violence and Risk Factors for HIV Among Female Sex Workers in Andhra Pradesh, India. Public Health Rep. 2010;125(4):81–89. doi: 10.1177/00333549101250S412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.James J, Gosho C, Watson Wohl R. The Relationship between Female Criminality and Drug Use. Int J Addict. 1979;14(2):215–229. doi: 10.3109/10826087909060367. [DOI] [PubMed] [Google Scholar]
- 26.Gossop M, Poeis B, Griffiths P, Strang J. Sexual behaviour and its relationship to drug-taking among prostitutes in south London. Addiction. 2006;89(8):961–970. doi: 10.1111/j.1360-0443.1994.tb03356.x. [DOI] [PubMed] [Google Scholar]
- 27.Sherafatipour J. Social and economical characteristics of Street women in Tehran. Social Welfare Quarterly. 2006;6(22):173–196. [Google Scholar]
- 28.Mayaud P, McCormick D. Interventions against sexually transmitted infections (STI) to prevent HIV infection. Br Med Bull. 2001;58(1):129–153. doi: 10.1093/bmb/58.1.129. [DOI] [PubMed] [Google Scholar]
- 29.McClelland RS, Sangaré L, Hassan WM, Lavrys L, Mandaliya K, et al. Infection with Trichomonas vaginalis Increases the Risk of HIV-1 Acquisition. J Infect Dis. 2007;195(5):698–702. doi: 10.1086/511278. [DOI] [PubMed] [Google Scholar]
- 30.Wasserheit JN. Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sexually Transmitted Diseases. 1992;19(2):61–77. [PubMed] [Google Scholar]