Abstract
Background
For the past 30 years, opioids have been used to treat chronic nonmalignant pain. This study tests the following hypotheses: (1) there is no strong evidence-based foundation for the conclusion that long-term opioid treatment of chronic nonmalignant pain is effective; and (2) the main problem associated with the safety of such treatment – assessment of the risk of addiction – has been neglected.
Methods
Scientometric analysis of the articles representing clinical research in this area was performed to assess (1) the quality of presented evidence (type of study); and (2) the duration of the treatment phase. The sufficiency of representation of addiction was assessed by counting the number of articles that represent (1) editorials; (2) articles in the top specialty journals; and (3) articles with titles clearly indicating that the addiction-related safety is involved (topic-in-title articles).
Results
Not a single randomized controlled trial with opioid treatment lasting >3 months was found. All studies with a duration of opioid treatment ≥6 months (n = 16) were conducted without a proper control group. Such studies cannot provide the consistent good-quality evidence necessary for a strong clinical recommendation. There were profound differences in the number of addiction articles related specifically to chronic nonmalignant pain patients and to opioid addiction in general. An inadequate number of chronic pain-related publications were observed with all three types of counted articles: editorials, articles in the top specialty journals, and topic-in-title articles.
Conclusion
There is no strong evidence-based foundation for the conclusion that long-term opioid treatment of chronic nonmalignant pain is effective. The above identified signs indicating neglect of addiction associated with the opioid treatment of chronic nonmalignant pain were present.
Keywords: addiction, chronic pain, neuropathic pain, opioids, overdose death, quality of evidence, treatment efficacy
Introduction
Only relatively recently in the history of medicine, was there a need to demonstrate quality of evidence and strength of recommendations to validate treatment effectiveness.1–3 Such support has been provided for various treatments of acute pain with opioids.4 Opiates have been used for treatment of acute and persistent pain for centuries, before the current standards of evidence quality became the norm. Compared to this, the treatment of chronic nonmalignant pain with opioids is a relatively new development. For the period 1983–2012, PubMed has more than 2,000 articles on the opioid treatment of chronic nonmalignant pain, but almost no articles on this topic before then. In regards to the Bonica pain clinic treatment practices from 1960–1980, Loeser wrote that
“it did not enter our minds that there could be a significant number of chronic pain patients who were successfully managed with opioids, because if there were any, we almost never saw them.”5
This explains the almost complete absence of publications on the opioid treatment of chronic pain before 1983. The value of opioids in the treatment of chronic pain attributable to cancer was well recognized before the 1980s. As far as nonmalignant chronic pain is concerned, several initial publications were collected and summarized in the mid-1980s.12 The use of opioids for chronic pain management was introduced when the new standards of evidence-based medicine were already in the final stages of their establishment. Despite this, the opioid treatment of chronic pain came into practice without convincing proof of effectiveness. Since then, doubts about the effectiveness and safety of long-term treatment of chronic nonmalignant pain with opioids have been expressed in several reviews.6–9
The goal of the present study was to test the following hypotheses: (1) there is no strong evidence-based foundation for the conclusion that long-term opioid treatment of chronic nonmalignant pain is effective; and (2) the risk of addiction – the main problem associated with the safety of such treatment – has been neglected. The available information pertinent to these hypotheses was analyzed using scientometric approaches.
Methods
The articles were collected mainly using the National Library of Medicine’s PubMed website (http://www.ncbi.nlm.nih.gov/PubMed). Articles published in English over the 30-year period of 1983–2012 were included. Keywords related to chronic pain (“chronic pain” OR “neuropathic pain”) were added to the terms related to opioids (“opioids” OR “narcotic analgesics” OR “morphine”). In addition, cancer pain and terminal illness were excluded from the search by placing in the search box the following: NOT (“cancer pain” OR “terminal illness”). Boolean operations were used, in which the following variables were selected: keywords, years of publications, and type of publications. In addition to the electronic search of articles, related publications were also searched manually in the reference lists of reports and reviews.
Efficacy hypothesis
Articles found in the searches were reviewed to make sure that they fit the definition of chronic pain. Articles with titles that lacked certain indication of pain duration, such as “persistent,” “persisting,” or “long-term” were checked and included in the database only if the duration of pain was ≥3 months. Criteria for excluding articles were: (1) inclusions of cases with malignant pain; (2) inclusions of treatments combining opioids with local anesthetics or antidepressants; (3) duration of treatment of 1 day (or <24 hours); and (4) having fewer than ten patients.4 To assess the quality of evidence for the efficacy for the treatment, the following factors were taken into consideration: the type of the study (randomized controlled trial [RCT] or not), the duration of opioid treatment (≥6 months or not), and the study conclusion on the treatment efficacy.
Addiction hypothesis
The following signs were used to determine whether attention to the addiction-related safety of long-term opioid treatment was insufficient: the number of journal editorials on this topic, the number of articles in the top specialty journals, and the number of journal articles with titles clearly stating that the addiction-related safety of the treatment is involved. The editorials (articles solicited by an editorial board to provide an editorial perspective on an article published in a journal) on several topics associated with the safety of long-term opioid treatment of chronic pain were selected in the following way: keywords related to chronic pain (“chronic pain” OR “neuropathic pain”) and opioids (“opioids” OR “narcotic analgesics” OR “morphine”) were combined with keywords associated with addiction (“addiction” OR “dependence” OR “abuse” OR “misuse”) or with overdose death (“death” OR “mortality” OR “fatality”). The article type was selected by using the PubMed filtering tool “Editorial.”
To quantitatively evaluate the presentation of the above topics in leading medical journals, the 20 top journals were selected with the approach used previously.10 The journal selection was based on two factors: (1) the rank of a journal sorted by the impact factor, as indicated by Journal Citation Report for 2011 (http://science.thomsonreuter.com) and (2) the journal specialty area. They included biomedical journals in general (ten journals), pharmacology (six journals), and psychiatry or neurology (four journals). The impact factor was used for the selection of journals in each specialty area category separately. The following journals were included: Addiction, The American Journal of Psychiatry, Annals of Internal Medicine, Annals of Neurology, Archives of General Psychiatry, BMJ, The Journal of Clinical Investigation, The Journal of Pharmacology and Experimental Therapeutics, JAMA: The Journal of the American Medical Association, Lancet, The New England Journal of Medicine, Nature Medicine, Nature Neuroscience, Nature Reviews Drug Discovery, Nature Reviews Neuroscience, Nature, Pharmacological Reviews, Proceedings of the National Academy of Science of the United States of America, Science (New York, NY, USA), and Trends in Pharmacological Sciences. All types of articles were used for this index.
To select articles with titles clearly indicating that they are devoted to specific topics (topic-in-title articles), the indicator “(Title)” was added to the selected terms placed into PubMed search boxes. All types of articles were used for this index also.
Results
Efficacy hypothesis
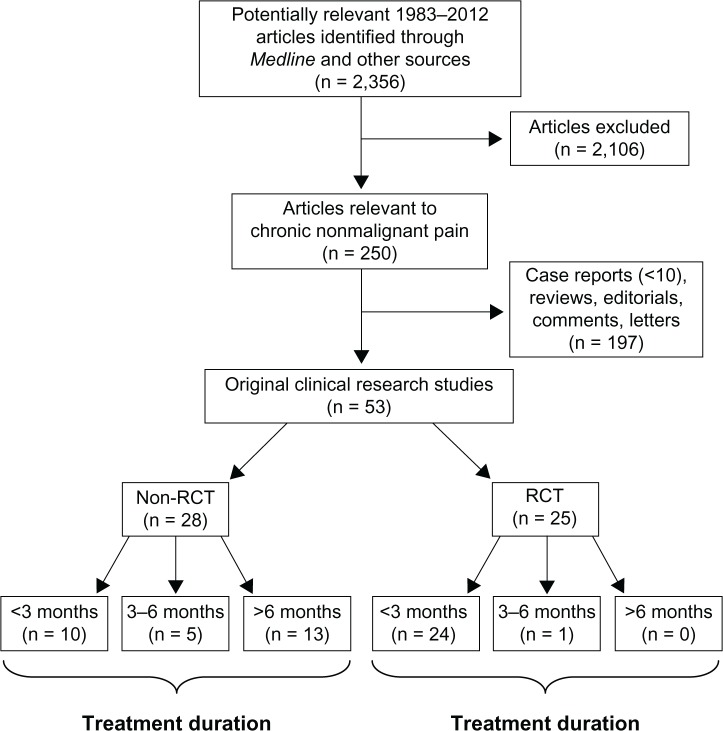
The electronic and manual search of the literature identified 2,356 articles. The results of this initial search were reviewed and reduced to 250 articles; see flowchart (Figure 1) and Supplementary material. Fifty-three articles were original clinical research articles on the opioid treatment of chronic nonmalignant pain (Table 1).11–63 Analysis of these publications revealed that 25 are reports of RCT studies, the rest are studies that lack a proper control group.64 Most of the RCT studies had a treatment duration of ≤1 month. Only one study is in the “≥3 months category” (90 days).58 The other randomized investigation with long treatment duration (16 weeks) was an open study.65 Table 2 presents 16 studies in which the duration of opioid treatment was ≥6 months, none of which is an RCT. Thus, there is not a single study that both fits the high quality of evidence category and has a long-term opioid treatment (duration of treatment ≥6 months). Systematic reviews on the opioid treatment of chronic nonmalignant pain have come to the same conclusion regarding long-term efficacy of the treatment, ie, there is insufficient evidence to make a definite conclusion (Table 3).6–9
Figure 1.
Flow chart of screened, excluded, and included articles on chronic nonmalignant pain from 1983–2012.
Abbreviation: RCT, randomized controlled trial.
Table 1.
Duration of opioid treatment in studies on chronic nonmalignant pain
| Duration of treatment | Number of studies without a proper control group*,11–38
|
Number of randomized controlled trials39–63
|
||||||
|---|---|---|---|---|---|---|---|---|
| ≤1 m | >1 m–<3 m | ≥3 m | ≥1 y | ≤1 m | >1 m–<3 m | ≥3 m | ≤1 y | |
| Years | ||||||||
| 1983–1992 | 1 | 0 | 0 | 3 | 1 | 0 | 0 | 0 |
| 1993–2002 | 4 | 1 | 2 | 6 | 10 | 2 | 0 | 0 |
| 2003–2012 | 4 | 0 | 3 | 4 | 5 | 6 | 1 | 0 |
| Total | 9 | 1 | 5 | 13 | 16 | 8 | 1 | 0 |
Note:
Studies without a proper control group (see Grimes and Schulz).64
Abbreviations: m, month; y, year.
Table 2.
Studies with the duration of opioid treatment ≥6 months
| Reference | Study design | Diagnosis | Opioid | Route of administration | Number of enrolled patients | Length of treatment |
|---|---|---|---|---|---|---|
| France et al11 | Case series (uncontrolled, retrospective, selected patients) | Back pain | Codeine, oxycodone, hydromorphone | Oral | 16 | 6–22 months |
| Portenoy and Foley12 | Descriptive study (uncontrolled, retrospective, patients selected from two separate studies) | Back pain, postherpetic neuralgia, neuropathic pain | Oxycodone, methadone, levorphanol, codeine | Oral | 38 | 6 months to 10 years |
| Zenz et al13 | Descriptive study (uncontrolled, prospective) | Back pain, neuropathic pain | Sustained-release dihydrocodeine, buprenorphine, sustained-release morphine | Oral | 100 | ≥ 1 year (20 patients) |
| Kanoff15 | Descriptive study (uncontrolled, prospective) | Reflex sympathetic dystrophy, arachnoiditis | Morphine via implanted delivery system | Intrathecal | 15 | 2–44 months |
| Hassenbusch et al16 | Descriptive study (uncontrolled, prospective) | Neuropathic pain | Morphine, sufentanil via implanted delivery system | Intrathecal | 22 | 12–56 months (18 patients) |
| Tutak and Doleys17 | Descriptive study (uncontrolled, prospective) | Back pain | Morphine via implanted delivery system | Intrathecal | 26 | 16–27 months |
| Angel et al19 | Descriptive study (uncontrolled, prospective) | Back pain, neuropathic pain | Morphine via implanted delivery system | Intrathecal | 15 | 3 years(11 patients) |
| Anderson and Burchiel20 | Descriptive study (uncontrolled, prospective) | Neuropathic pain, nociceptive pain | Morphine via implanted delivery system | Intrathecal | 40 | 24 months (20 patients) |
| Harati et al24 | Descriptive study (uncontrolled, prospective) | Diabetic neuropathy | Tramadol | Oral | 117 | 6 months (100 patients) |
| Milligan et al25 | Descriptive study (uncontrolled, prospective) | Neuropathic pain, nociceptive pain | Fentanyl | Transdermal | 532 | 12 months (301 patients) |
| Mironer and Tollison26 | Descriptive study (uncontrolled, prospective) | Back pain, neuropathic pain | Methadone | Intrathecal | 24 | 6 months (9 patients) |
| Anderson et al28 | Uncontrolled study (prospective, randomized to morphine intrathecal infusion or its epidural injection) | Chronic nonmalignant pain | Morphine via implanted delivery system | Intrathecal | 40 | 6 months (27 patients) |
| Allan et al31 | Uncontrolled study (prospective, multicenter, randomized to oral morphine) | Back pain | Fentanyl | Transdermal | 680 | 13 months |
| Chao32 | Descriptive study (uncontrolled, retrospective) | Back pain, neuropathic pain | Sustained-release morphine | Oral | 68 | 12 months |
| Mcllwain and Ahdieh33 | Descriptive study (uncontrolled, prospective, multicenter) | Osteoarthritis | Extended-release oxymorphone | Oral | 153 | 12 months (61 patients) |
| Portenoy et al36 | Uncontrolled registry study | Osteoarthritis, diabetic neuropathy, back pain | Controlled-release oxycodone | Oral | 219 | 1–3 years (14–39 patients) |
Table 3.
Systematic reviews on opioid treatment of chronic pain
| Study | Type of pain | Opioid | Route of administration | Duration of treatment | Conclusion on the treatment efficacy |
|---|---|---|---|---|---|
| Kalso et al6 | Osteoarthritis, diabetic neuropathy, peripheral neuropathic pain, phantom limb pain, postherpetic neuralgia, musculoskeletal pain | Morphine, oxycodone | Oral, transdermal, or intravenous | From 4 days to 8 weeks | The short-term efficacy of opioids was good in both neuropathic and musculoskeletal pain conditions. However, only a minority of patients went on to long-term management with opioids; therefore, open-label follow-up data were too weak to make a definite conclusion. |
| Martell et al7 | Back pain | Morphine, oxycodone, sustained-release morphine, controlled-release oxycodone, other opioids | Oral or transdermal | From 7 days to 16 weeks | Opioids may be efficacious for short-term pain relief. Long-term efficacy was unclear. |
| Noble et al8 | Neuropathic pain, osteoarthritis, back pain | Morphine, tramadol, methadone, controlled-release oxycodone, extended-release oxymorphone, fentanyl, sufentanil, dihydrocodeine, buprenorphine | Oral, transdermal, or intrathecal | From 6–48 months | Weak evidence suggests that oral and intrathecal opioids reduce pain long-term in the relatively small proportion of individuals who continue treatment. |
| Nuesch et al9 | Osteoarthritis | Codeine, morphine, oxycodone, oxymorphone | Oral or transdermal | From 3 days to 3 months | The small to moderate beneficial effects of opioids are outweighed by large increases in the risk of adverse events. Therefore, opioids should not be routinely used, even if osteoarthritic pain is severe. |
Addiction hypothesis
The results on the editorials related to addiction in chronic nonmalignant pain patients are presented in Table 4. There were no editorials on this topic in 1983–1992, one in 1993–2002, and four in 2003–2012. For the same period, editorials on opioid addiction in general (the right side of Table 4) were numerous (171 from 2003–2012). As far as editorials on death associated with opioid treatment of chronic nonmalignant pain are concerned, only two were found – both recent – in 2010–2011.67,69
Table 4.
Editorials on opioid addiction in chronic pain patients
| Years | Number of editorials
|
|
|---|---|---|
| “Addiction”a AND “chronic pain”b | “Addiction”a | |
| 1973–1982 | – | 12 |
| 1983–1992 | 0 | 19 |
| 1993–2002 | 1c | 63 |
| 2003–2012 | 4d | 171 |
Notes:
OR “dependence” OR “abuse” OR “misuse;”
OR “neuropathic pain” NOT (“cancer pain” OR “terminal illness”);
reference 66;
references 67–70.
Representation of opioid addiction in the top 20 journals is shown in Table 5 (left side – opioid addiction in patients with chronic pain; right side – opioid addiction in general). Once again, the problem of opioid addiction in chronic pain patients was discussed in only six articles (five of which appeared in 2003–2012). The problem of death associated with opioid treatment of chronic pain was discussed only in three articles from the top journals.71,72,77
Table 5.
Articles on opioid addiction in chronic pain patients in the top 20 journalsa
| Years | Number of articles
|
|
|---|---|---|
| “Addiction”b AND “chronic pain”c | “Addiction”b | |
| 1973–1982 | – | 5 |
| 1983–1992 | 1d | 5 |
| 1993–2002 | 0 | 12 |
| 2003–2012 | 5e | 40 |
Notes:
List of top journals: Addiction, The American Journal of Psychiatry, Annals of Internal Medicine, Annals of Neurology, Archives of General Psychiatry, BMJ, The Journal of Clinical Investigation, The Journal of Pharmacology and Experimental Therapeutics, JAMA: The Journal of the American Medical Association, Lancet, The New England Journal of Medicine, Nature Medicine, Nature Neuroscience, Nature Reviews Drug Discovery, Nature Reviews Neuroscience, Nature, Pharmacological Reviews, Proceedings of the National Academy of Science of the United States of America, Science (New York, NY, USA), and Trends in Pharmacological Sciences;
OR “dependence” OR “abuse” OR “misuse;”
OR “neuropathic pain” NOT (“cancer pain” OR “terminal illness”);
reference 73;
references 74–78.
The topic-in-title articles (articles clearly announcing that they are devoted to opioid addiction, dependence, abuse, or misuse) are presented in Table 6. The right side of the table presents the articles on addiction-related problems in general, and the left side presents those specifically in chronic pain patients. It indicates that in 1983–1992 only two topic-in-title articles related to opioid addiction in chronic pain patients were published; in the next 10-year period, this number increased to 13; and was 51 for 2003–2012. It is of interest that in the 15 years following 1983, the word “addiction” in titles appeared only once; the word “abuse” was used in the rest of the article titles. On the other hand, topic-in-title articles on addiction-related problems in general (the right side of Table 6) were numerous (1,404 in 2003–2012). It is of interest that during 1983–2002 when opioids were introduced for the treatment of chronic nonmalignant pain, there was a clear decrease in the number of articles devoted to the problem of opioid addiction in general (from 893 in 1973–1982 to 536 and 628 in 1983–1992 and 1993–2002, respectively).
Table 6.
Topic-in-title articlesa on opioid addiction in chronic pain patients
| Years | Number of articles
|
|
|---|---|---|
| “Addiction”b AND “chronic pain”c | “Addiction”b | |
| 1973–1982 | – | 893 |
| 1983–1992 | 2d | 536 |
| 1993–2002 | 13e | 628 |
| 2003–2012 | 51f | 1,404 |
Notes:
Articles with titles clearly indicating that they are devoted to the addiction in chronic pain patients
OR “dependence” OR “abuse” OR “misuse”
OR “neuropathic pain” NOT (“cancer pain” OR “terminal illness”)
references 79–80
references 81–93;
references 94–144.
Topic-in-title articles on death associated with opioid addiction in chronic pain patients are presented in Table 7. This table indicates only four such articles, all in 2003–2012. Topic-in-title articles on death associated with opioid addiction in general (the right side of Table 7) were also very rare (two to four articles per decade).
Table 7.
Topic-in-title articlesa on death associated with opioid addiction in chronic pain patients
| Years | Number of articles
|
|
|---|---|---|
| “Death”b AND “addiction”c AND “chronic pain”d | “Death”b AND “addiction”c | |
| 1973–1982 | – | 4 |
| 1983–1992 | 0 | 3 |
| 1993–2002 | 0 | 2 |
| 2003–2012 | 4e | 4 |
Notes:
Articles with titles clearly indicating that they are devoted to death associated with addiction in chronic pain patients;
OR “mortality” OR “fatality;”
OR “dependence” OR “abuse” OR “misuse;”
OR “neuropathic pain” NOT (“cancer pain” OR “terminal illness”);
references 145–148.
Discussion
Efficacy hypothesis
Simple scientometric assessment of articles on long-term opioid treatment of chronic nonmalignant pain indicates the absence of high-quality evidence on efficacy. There is not a single RCT study lasting >3 months (Table 1). The longest randomized investigation (16 weeks) was limited by being an open study.65 All studies with opioid treatment ≥6 months (Table 2) were conducted without a proper control group;64 therefore, they do not provide the consistent good-quality evidence to support a strong clinical recommendation.1–3 Systematic reviews on opioid treatment of chronic nonmalignant pain have concluded that there is insufficient evidence to make a definite conclusion on the efficacy of long-term treatment.6–9
Addiction hypothesis
The problem of safety of opioid treatment revealed itself most dramatically in rising numbers of opioid overdose deaths. According to the 2008 National Survey on Drug Use and Health (NSDUH) sponsored by the Substance Abuse and Mental Health Service Administration (SAMHSA), there has been at least a ten-fold increase in the medical use of opioids from 1988–2007.149 In 2007, 11,499 deaths were caused by overdoses of opioids, roughly a four-fold increase compared with 1999. Remarkably, even an increase of that size somehow did not trigger a timely response by the medical journals. This phenomenon is especially noticeable if one looks at the number of editorials on death associated with opioid treatment of chronic pain patients. Only two editorials on this topic were found (both late, in 2010–2011), as if there had been no dramatic increase in opioid-related deaths in 1999–2007.
Opioid abuse, misuse, and addiction are the main reasons leading to the opioid overdose deaths. Somehow the introduction of opioid treatment of chronic nonmalignant pain did not result in editorials on opioid addiction in chronic pain patients: there were five editorials related to this topic, four of them published only in 2003–2012. Compare this with 171 editorials on opioid addiction in general published during this period (Table 4).
Representation for all types of articles (including letters and commentaries) on opioid addiction in the top 20 journals was also insufficient: zero articles in 1993–2002 (10–15 years after the introduction of treatment) and five in 2003–2012 (Table 5).
The topic-in-title articles clearly announce the topic under discussion; however, if the topic is an undesirable problem, authors often try to avoid naming it explicitly in the title. The lack of topic-in-title publications indicates that the topic is a neglected one.150 As indicated in the results of the present study, death associated with opioid addiction in chronic pain patients was not reflected in titles from 1983–2002; in 2003–2012, it was found in the titles of only four articles (Table 7). This tendency also applied to addiction, abuse, misuse, or dependence in opioid treatment of chronic pain. In 1983–1992, there were only two topic-in-title articles related to opioid addiction in chronic pain patients, at a time when there were 536 topic-in-title articles on opioid addiction in general (right side of Table 6). There were also profound differences in the numbers of addiction articles related specifically to chronic pain patients and to opioid addiction in general for the periods 1993–2002 and 2003–2012. Especially interesting was the decrease in the number of topic-in-title articles on opioid addiction in general during 1983–2002 (right side of Table 6) when opioid treatment for chronic nonmalignant pain was being introduced. Could the acceptance of this new indication for opioid treatment be responsible for such a change?
Estimates of the rate of addiction problems among chronic pain patients extremely varied. Hojsted and Sjogren reported that the rates of addiction associated with long-term opioid treatment were 0%–50% in noncancer patients and 0%–7.7% in cancer patients, depending on the subpopulation studied and the criteria used.108 This uncertainty is similar to that with the rate of iatrogenic addiction in patients treated with opioids for acute or subacute pain. A systematic review on this topic concluded, “It is not known whether the risk for iatrogenic addiction among patients treated with opioids for acute or subacute pain is relatively high (>10%) or low (0.1%).”151 The difficulty of estimating the risk of opioid addiction and abuse (see Jamison et al)152 calls into question the accuracy of reported rates of risk for opioid addiction.
One author of a study on the use of opioids in chronic nonmalignant pain has asked: “Is this treatment a lifetime sentence?”153 If not, another question should be: “Has the withdrawal syndrome after long-term opioid use been adequately studied?”; and not only acute withdrawal syndrome, but protracted withdrawal as well? The latter (also called protracted abstinence or chronic withdrawal syndrome) is characterized by generalized symptoms (eg, discomfort, fatigue, decreased blood pressure, pulse rate, and body temperature) lasting 3–9 months.154–156 Long-lasting (3–4 months) neurobiological alterations following withdrawal from opioids have been well confirmed in animal experiments.157 Lack of knowledge regarding the risk of addiction and even greater uncertainty regarding protracted withdrawal following cessation of long-term opioid treatment of chronic pain call for studies with high-quality evidence that supports reliable recommendations.
This study has a limitation related to the absence of exact definition of chronic nonmalignant pain. It is associated with the lack of definition for chronic pain in general. For example, the International Association for the Study of Pain Task Force on Taxonomy – in the classification of chronic pain – has chosen not to define chronic pain.158
Conclusion
There is no high-quality evidence on the efficacy of long-term opioid treatment of chronic nonmalignant pain. As a result, the strength of any recommendation regarding this treatment is weak. The safety of opioid treatment in terms of risk of addiction and overdose death has not properly been assessed due to the complexity of these outcomes. Until 2003, opioid addiction associated with the treatment of chronic nonmalignant pain was clearly a neglected topic of publication. However, this topic is now beginning to receive the attention it deserves.
Supplementary materials
List of articles on long-term opioid treatment of chronic nonmalignant pain (1983–2012)
- Adams EH, Breiner S, Cicero TJ, et al. A comparison of the abuse liability of tramadol, NSAIDs, and hydrocodone in patients with chronic pain. J Pain Symptom Manage. 2006;31:465–476. doi: 10.1016/j.jpainsymman.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Adams LL, Gatchel RJ, Robinson RC, et al. Development of a self-report screening instrument for assessing potential opioid medication misuse in chronic pain patients. J Pain Symptom Manage. 2004;27:440–459. doi: 10.1016/j.jpainsymman.2003.10.009. [DOI] [PubMed] [Google Scholar]
- Adams NJ, Plane MB, Fleming MF, Mundt MP, Saunders LA, Stauffacher EA. Opioids and the treatment of chronic pain in a primary care sample. J Pain Symptom Manage. 2001;22:791–796. doi: 10.1016/s0885-3924(01)00320-7. [DOI] [PubMed] [Google Scholar]
- Alexander GC, Kruszewski SP, Webster DW. Rethinking opioid prescribing to protect patient safety and public health. JAMA. 2012;14(308):1865–1866. doi: 10.1001/jama.2012.14282. [DOI] [PubMed] [Google Scholar]
- Alford DP. Opioids for chronic pain in patients with substance abuse: too much, too little or just right? Pain. 2009;145:267–268. doi: 10.1016/j.pain.2009.06.036. [DOI] [PubMed] [Google Scholar]
- Allan L, Richarz U, Simpson K, Slappendel R. Transdermal fentanyl versus sustained release oral morphine in strong-opioid naïve patients with chronic lower back pain. Spine. 2005;30:2484–2490. doi: 10.1097/01.brs.0000186860.23078.a8. [DOI] [PubMed] [Google Scholar]
- Anderson VC, Burchiel KJ, Cooke B. A prospective, randomized trial of intrathecal injection vs. epidural infusion in the selection of patients for continuous intrathecal opioid therapy. Neuromodulation. 2003;6:142–152. doi: 10.1046/j.1525-1403.2003.03023.x. [DOI] [PubMed] [Google Scholar]
- Anderson VC, Burchiel KJ. A prospective study of long-term intrathecal morphine in the management of chronic nonmalignant pain. Neurosurgery. 1999;44:289–300. doi: 10.1097/00006123-199902000-00026. [DOI] [PubMed] [Google Scholar]
- Andrews CM, Krantz MJ, Wedam EF, Marcuson MJ, Capacchione JF, Haigney MC. Methadone-induced mortality in the treatment of chronic pain: role of QT prolongation. Cardiol J. 2009;16:210–217. [PubMed] [Google Scholar]
- Angel IF, Gould HJ, Jr, Carey ME. Intrathecal morphine pump as a treatment option in chronic pain of nonmalignant origin. Surg Neurol. 1998;49:92–98. doi: 10.1016/s0090-3019(97)00287-5. [DOI] [PubMed] [Google Scholar]
- Aronoff GM. Opioids in chronic pain management: is there a significant risk of addiction? Curr Rev Pain. 2000;4:112–121. doi: 10.1007/s11916-000-0044-0. [DOI] [PubMed] [Google Scholar]
- Ballantyne JC, LaForge KS. Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 2007;129:235–255. doi: 10.1016/j.pain.2007.03.028. [DOI] [PubMed] [Google Scholar]
- Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003;349:1943–1953. doi: 10.1056/NEJMra025411. [DOI] [PubMed] [Google Scholar]
- Ballantyne JC. Chronic opioid therapy and its utility in different populations. Pain. 2012;153:2303–2304. doi: 10.1016/j.pain.2012.07.015. [DOI] [PubMed] [Google Scholar]
- Ballantyne JC. Opioids for chronic pain: taking stock. Pain. 2006;125:3–4. doi: 10.1016/j.pain.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Balousek S, Plane MB, Fleming M. Prevalence of interpersonal abuse in primary care patients prescribed opioids for chronic pain. J Gen Intern Med. 2007;22:1268–1273. doi: 10.1007/s11606-007-0257-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron MJ, McDonald PW. Significant pain reduction in chronic pain patients after detoxification from high-dose opioid. J Opioid Manag. 2006;2:277–282. doi: 10.5055/jom.2006.0041. [DOI] [PubMed] [Google Scholar]
- Barry DT, Irwin KS, Jones ES, et al. Opioids, chronic pain, and addiction in primary care. J Pain. 2010;11:1442–1450. doi: 10.1016/j.jpain.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker WC, Fiellin DA, Gallagher RM, Barth KS, Ross JT, Oslin DW. The association between chronic pain and prescription drug abuse in veterans. Pain Med. 2009;10:531–536. doi: 10.1111/j.1526-4637.2009.00584.x. [DOI] [PubMed] [Google Scholar]
- Belgrade MJ. Opioids for chronic nonmalignant pain. Choosing suitable candidates for long-term therapy. Postgrad Med. 1999;106:115–116. doi: 10.3810/pgm.1999.11.769. [DOI] [PubMed] [Google Scholar]
- Bjornaas MA, Bekken AS, Ojlert A, et al. A 20-year prospective study of mortality and causes of death among hospitalized opioid addicts in Oslo. BMC Psychiatry. 2008;8:8. doi: 10.1186/1471-244X-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blondell RD, Ashrafoun L, Dambra CM, Foschio EM, Zielinski AL, Salcedo DM. A clinical trial comparing tapering doses of buprenorphine with steady doses for chronic pain and co-existent opioid addiction. J Addict Med. 2010;4:140–146. doi: 10.1097/ADM.0b013e3181ba895d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohmfalk GL. Management of chronic pain. JAMA. 1989;261:381. [PubMed] [Google Scholar]
- Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305:1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- Boudreau D, Von Korff M, Rutter CM, et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf. 2009;18:1166–1175. doi: 10.1002/pds.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braden JB, Fan MY, Edlund MJ, Martin BC, DeVries A, Sullivan MD. Trends in use of opioids by noncancer pain type 2000–2005 among Arkansas Medicaid and HealthCore enrollees: results from the TROUP study. J Pain. 2008;9:1026–1035. doi: 10.1016/j.jpain.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braden JB, Russo J, Fan MY, et al. Emergency department visits among recipients of chronic opioid therapy. Arch Intern Med. 2010;170:1425–1432. doi: 10.1001/archinternmed.2010.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braden JB, Sullivan MD, Ray GT, et al. Trends in long-term opioid therapy for noncancer pain among persons with a history of depression. Gen Hosp Psychiatry. 2009;31:564–570. doi: 10.1016/j.genhosppsych.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodner R, Taub A. Chronic pain exacerbated by long-term narcotic use in patients with non-malignant disease: Clinical syndrome and treatment. Mt Sinai J Med. 1978;45:233–237. [PubMed] [Google Scholar]
- Brushwood DB, Rich BA, Coleman JJ, Bolen J, Wong W. Legal liability perspectives on abuse-deterrent opioids in the treatment of chronic pain. J Pain Palliat Care Pharmacother. 2010;24:333–348. doi: 10.3109/15360288.2010.524979. [DOI] [PubMed] [Google Scholar]
- Butler SF, Budman SH, Fanciullo GJ, Jamison RN. Cross validation of the current opioid misuse measure to monitor chronic pain patients on opioid therapy. Clin J Pain. 2010;26:770–776. doi: 10.1097/AJP.0b013e3181f195ba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler SF, Budman SH, Fernandez KC, Fanciullo GJ, Jamison RN. Cross-validation of a screener to predict opioid misuse in chronic pain patients (SOAPP-R) J Addict Med. 2009;3:66–73. doi: 10.1097/ADM.0b013e31818e41da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell JR, Hale ME, Boyd RE, et al. Treatment of osteoarthritis pain with controlled release oxycodone or fixed combination oxycodone plus acetaminophen added to nonsteroidal anti-inflammatory drugs: a double blind, randomized, multicenter, placebo controlled trial. J Rheumatol. 1999;26:862–869. [PubMed] [Google Scholar]
- Caldwell JR, Rapoport RJ, Davis JC, Offenberg HL, Marker HW, Roth SH, et al. Efficacy and safety of a once-daily morphine formulation in chronic, moderate-to severe osteoarthritis pain: results form a randomized, placebo-controlled, double-blind trial and an open-label extension trial. J Pain Symptom Manage. 2002;23:278–291. doi: 10.1016/s0885-3924(02)00383-4. [DOI] [PubMed] [Google Scholar]
- Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 versus 2000. Pain. 2004;109:514–519. doi: 10.1016/j.pain.2004.03.006. [DOI] [PubMed] [Google Scholar]
- CDC Unintentional drug poisoning in the United States 2010www.cdc.gov/HomeandRecreationalSafety/PoisoningAccessed December 12, 2012
- Chabal C, Erjavec MK, Jacobson L, Mariano A, Chaney E. Prescription opiate abuse in chronic pain patients: clinical criteria, incidence, and predictors. Clin J Pain. 1997;13:150–155. doi: 10.1097/00002508-199706000-00009. [DOI] [PubMed] [Google Scholar]
- Chancellor J, Martin M, Leidgens H, Baker MG, Müller-Schwefe GH. Stated preferences of physicians and chronic pain sufferers in the use of classic strong opioids. Value Health. 2012;15:106–117. doi: 10.1016/j.jval.2011.07.002. [DOI] [PubMed] [Google Scholar]
- Chao J. Retrospective analysis of Kadian (morphine sulfate sustained-release capsules) in patients with chronic, nonmalignant pain. Pain Med. 2005;6:262–265. doi: 10.1111/j.1526-4637.2005.05033.x. [DOI] [PubMed] [Google Scholar]
- Chindalore VL, Craven RA, Yu KP, Butera PG, Burns LH, Friedmann N. Adding ultra low-dose naltrexone to oxycodone enhances and prolongs analgesia: A randomized, controlled trial of oxytrex. Pain. 2005;6:392–399. doi: 10.1016/j.jpain.2005.01.356. [DOI] [PubMed] [Google Scholar]
- Chou R, Clark E, Helfand M. Comparative efficacy and safety of long-acting oral opioids for chronic non-cancer pain: a systematic review. J Pain Symptom Manage. 2003;26:1036–1048. doi: 10.1016/j.jpainsymman.2003.03.003. [DOI] [PubMed] [Google Scholar]
- Chou R, Fanciullo GJ, Fine PG, Miaskowski C, Passik SD, Portenoy RK, American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10:113–130. doi: 10.1016/j.jpain.2008.10.009. [DOI] [PubMed] [Google Scholar]
- Christo PJ, Grabow TS, Raja SN. Opioid effectiveness, addiction, and depression in chronic pain. Adv Psychosom Med. 2004;25:123–137. doi: 10.1159/000079062. [DOI] [PubMed] [Google Scholar]
- Clark MR, Stoller KB, Brooner RK. Assessment and management of chronic pain in individuals seeking treatment for opioid dependence disorder. Can J Psychiatry. 2008;53:496–508. doi: 10.1177/070674370805300804. [DOI] [PubMed] [Google Scholar]
- Clausen T, Waal H, Thoresen M, Gossop M. Mortality among opiate users: opioid maintenance therapy, age and causes of death. Addiction. 2009;104:1356–1362. doi: 10.1111/j.1360-0443.2009.02570.x. [DOI] [PubMed] [Google Scholar]
- Cohen MJ, Jasser S, Herron PD, Margolis CG. Ethical perspectives: opioid treatment of chronic pain in the context of addiction. Clin J Pain. 2002;18:S99–S107. doi: 10.1097/00002508-200207001-00012. [DOI] [PubMed] [Google Scholar]
- Compton P, Athanasos P. Chronic pain, substance abuse and addiction. Nurs Clin North Am. 2003;38:525–537. doi: 10.1016/s0029-6465(02)00100-7. [DOI] [PubMed] [Google Scholar]
- Compton P, Drakjian J, Miotto K. Screening for addiction in patients with chronic pain and “problematic” substance use: evaluation of a pilot assessment tool. J Pain Symptom Manage. 1998;16:355–363. doi: 10.1016/s0885-3924(98)00110-9. [DOI] [PubMed] [Google Scholar]
- Compton P, Estepa CA. Addiction in patients with chronic pain. Lippincotts Prim Care Pract. 2000;4:254–272. [PubMed] [Google Scholar]
- Couto J, Romney M, Leider H, Sharma S, Goldfarb N. High rates of inappropriate drug use in the chronic pain population. Population Health Management. 2009;12:185–190. doi: 10.1089/pop.2009.0015. [DOI] [PubMed] [Google Scholar]
- Dellemijn P. Are opioids effective in relieving neuropathic pain? Pain. 1999;80:453–462. doi: 10.1016/S0304-3959(98)00256-5. [DOI] [PubMed] [Google Scholar]
- Dellemijn PL. Opioids in non-cancer pain: a life-time sentence? Eur J Pain. 2001;5:333–339. doi: 10.1053/eujp.2001.0240. [DOI] [PubMed] [Google Scholar]
- Denisco RA, Chandler RK, Compton WM. Addressing the intersecting problems of opioid misuse and chronic pain treatment. Exp Clin Psychopharmacol. 2008;16:417–428. doi: 10.1037/a0013636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSio JM, Bacon DR, Peer G, Lema MJ. Intravenous abuse of transdermal fentanyl therapy in a chronic pain patient. Anesthesiology. 1993;79:1139–1141. doi: 10.1097/00000542-199311000-00036. [DOI] [PubMed] [Google Scholar]
- Dhalla IA, Mamdani MM, Sivilotti ML, Kopp A, Qureshi O, Juurlink DN. Prescribing of opioid analgesics and related mortality before and after the introduction of long-acting oxycodone. CMAJ. 2009;181:891–896. doi: 10.1503/cmaj.090784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillie KS, Fleming MF, Mundt MP, French MT. Quality of life associated with daily opioid therapy in a primary care chronic pain sample. J Am Board Fam Med. 2008;21:108–117. doi: 10.3122/jabfm.2008.02.070144. [DOI] [PubMed] [Google Scholar]
- Dubner R. A call for more science, not more rhetoric, regarding opioids and neuropathic pain. Pain. 1991;47:1–2. doi: 10.1016/0304-3959(91)90002-F. [DOI] [PubMed] [Google Scholar]
- Duensing L, Eksterowicz N, Macario A, Brown M, Stern L, Ogbonnaya A. Patient and physician perceptions of treatment of moderate-to-severe chronic pain with oral opioids. Curr Med Res Opin. 2010;26:1579–1585. doi: 10.1185/03007991003783747. [DOI] [PubMed] [Google Scholar]
- Dunbar SA, Katz NP. Chronic opioid therapy for nonmalignant pain in patients with a history of substance abuse: report of 20 cases. J Pain Symptom Manage. 1996;11:163–171. doi: 10.1016/0885-3924(95)00165-4. [DOI] [PubMed] [Google Scholar]
- Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152:85–92. doi: 10.1059/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Martin BC, Fan MY, Devries A, Braden JB, Sullivan MD. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP study. Drug Alcohol Depend. 2010;112:90–98. doi: 10.1016/j.drugalcdep.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Steffick D, Hudson T, Harris KM, Sullivan M. Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain. 2007;129:355–362. doi: 10.1016/j.pain.2007.02.014. [DOI] [PubMed] [Google Scholar]
- Edlund MJ, Sullivan M, Steffick D, Harris KM, Wells KB. Do users of regularly prescribed opioids have higher rates of substance use problems than nonusers? Pain Med. 2007;8:647–656. doi: 10.1111/j.1526-4637.2006.00200.x. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Wasan AD, Michna E, Greenbaum S, Ross E, Jamison RN. Elevated pain sensitivity in chronic pain patients at risk for opioid misuse. J Pain. 2011;9:953–963. doi: 10.1016/j.jpain.2011.02.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eriksen J, Sjøgren P, Bruera E, Ekholm O, Rasmussen NK. Critical issues on opioids in chronic non-cancer pain: an epidemiological study. Pain. 2006;125:172–179. doi: 10.1016/j.pain.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Evans PJD. Narcotic addiction in patients with chronic pain. Anaesthesia. 1981;36:597–602. doi: 10.1111/j.1365-2044.1981.tb10323.x. [DOI] [PubMed] [Google Scholar]
- Fernandez W, Hackman H, McKeown L, Anderson T, Huma B. Trends in opioid-related fatal overdoses in Massachusetts, 1990–2003. J Subst Abuse Treat. 2006;31:151–156. doi: 10.1016/j.jsat.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Finlayson RE, Maruta T, Morse RM, Martin MA. Substance dependence and chronic pain: experience with treatment and follow-up results. Pain. 1986;26:175–180. doi: 10.1016/0304-3959(86)90073-4. [DOI] [PubMed] [Google Scholar]
- Finlayson RE, Maruta T, Morse RM, Swenson WM, Martin MA. Substance dependence and chronic pain: profile of 50 patients treated in an alcohol and drug dependence unit. Pain. 1986;26:167–174. doi: 10.1016/0304-3959(86)90072-2. [DOI] [PubMed] [Google Scholar]
- Fishbain D, Johnson S, Webster L, Greene L, Faysal J. Review of regulatory programs and new opioid technologies in chronic pain management: balancing the risk of medication abuse with medical need. J Manag Care Pharm. 2010;16:276–287. doi: 10.18553/jmcp.2010.16.4.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbain DA, Gallagher RM. Comments on “prescription drug dependence and evolving beliefs about chronic pain management”. Am J Psychiatry. 2006;163:2194. doi: 10.1176/ajp.2006.163.12.2194a. [DOI] [PubMed] [Google Scholar]
- Fishbain DA, Lewis JE, Gao J, Cole B, Rosomoff RS. Alleged breaches of “standards of medical care” in a patient overdose death possibly related to chronic opioid analgesic therapy, application of the controlled substances model guidelines: case report. Pain Med. 2009;10:565–572. doi: 10.1111/j.1526-4637.2008.00523.x. [DOI] [PubMed] [Google Scholar]
- Fishbain DA, Rosomoff HL, Rosomoff RS. Drug abuse, dependence, and addiction in chronic pain patients. Clin J Pain. 1992;2:77–85. doi: 10.1097/00002508-199206000-00003. [DOI] [PubMed] [Google Scholar]
- Foley KM, Fins JJ, Inturrissi CE. A true believer’s flawed analysis. Arch Intern Med. 2011;171:739–740. doi: 10.1001/archinternmed.2011.166. [DOI] [PubMed] [Google Scholar]
- Foley KM. Opioids and chronic neuropathic pain. N Engl J Med. 2003;348:1279–1281. doi: 10.1056/NEJMe030014. [DOI] [PubMed] [Google Scholar]
- France RD, Urban BJ, Keefe FJ. Long-term use of narcotic analgesics in chronic pain. Soc Sci Med. 1984;19:1379–1382. doi: 10.1016/0277-9536(84)90027-3. [DOI] [PubMed] [Google Scholar]
- Franklin GM, Rahman EA, Turner JA, Danielle WE, Fulton-Kehoe D. Opioid use for chronic, low back pain. A prospective, population-based study among injured workers in Wasington state. 2002–2005. Clin J Pain. 2009;25:743–751. doi: 10.1097/AJP.0b013e3181b01710. [DOI] [PubMed] [Google Scholar]
- Fredheim OM, Kaasa S, Dale O, et al. Opioid switching from oral slow release morphine to oral methadone may improve pain control in chronic non-malignant pain: a nine-month follow-up study. Palliat Med. 2006;20:35–41. doi: 10.1191/0269216306pm1099oa. [DOI] [PubMed] [Google Scholar]
- Fugelstad A, Ahlner J, Brandt L, et al. Use of morphine and 6-monoacetyl-morphine in blood for the evaluation of possible risk factors for sudden death in 192 heroin users. Addiction. 2003;98:463–470. doi: 10.1046/j.1360-0443.2003.00330.x. [DOI] [PubMed] [Google Scholar]
- Furlan A, Sandoval J, Mailis-Gagnon A, Tunks E. Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ. 2006;174:1589–1594. doi: 10.1503/cmaj.051528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagnon B, Bruera E. Differences in the ratios of morphine to methadone in patients with neuropathic pain versus non-neuropathic pain. J Pain Symptom Manage. 1999;18:120–125. doi: 10.1016/s0885-3924(99)00049-4. [DOI] [PubMed] [Google Scholar]
- Galer BS, Lee D, Ma T, Nagle B, Schlagheck TG. MorphiDex (morphine sulfate/dextromethorphan hydrobromide combination) in the treatment of chronic pain: three multicenter, randomized double-blind, controlled clinical trials fail to demonstrate enhanced opioid analgesia or reduction in tolerance. Pain. 2005;115:284–295. doi: 10.1016/j.pain.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Gammaitoni AR, Galer BS, Lacouture P, Domingos J, Schlagheck T. Effectiveness and safety of new oxycodone/acetaminophen formulations with reduced acetaminophen for the treatment of low back pain. Pain Med. 2003;4:21–30. doi: 10.1046/j.1526-4637.2003.03002.x. [DOI] [PubMed] [Google Scholar]
- Gatti A, Reale C, Occhioni R, et al. Standard therapy with opioids in chronic pain management: ORTIBER study. Clin Drug Investig. 2009;29:17–23. doi: 10.2165/0044011-200929001-00003. [DOI] [PubMed] [Google Scholar]
- Gilron I, Bailey JM, Tu D, Holden RR, Weaver DF, Houlden RL. Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med. 2005;352:1324–1334. doi: 10.1056/NEJMoa042580. [DOI] [PubMed] [Google Scholar]
- Gimbel JS, Richards P, Portenoy RK. Controlled-release oxycodone for pain in diabetic neuropathy: a randomized controlled trial. Neurology. 2003;60:927–934. doi: 10.1212/01.wnl.0000057720.36503.2c. [DOI] [PubMed] [Google Scholar]
- Goldman B. Use and abuse of opioid analgesics in chronic pain. Can Fam Physician. 1993;39:571–576. [PMC free article] [PubMed] [Google Scholar]
- Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171:686–691. doi: 10.1001/archinternmed.2011.117. [DOI] [PubMed] [Google Scholar]
- Gourlay D, Heit H. Universal precautions in pain medicine: A rational approach to the treatment of chronic pain. Pain Med. 2005;6:107–112. doi: 10.1111/j.1526-4637.2005.05031.x. [DOI] [PubMed] [Google Scholar]
- Grady D, Berkowitz SA, Katz MH. Opioids for chronic pain. Arch Intern Med. 2011;171:1426–1427. doi: 10.1001/archinternmed.2011.213. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Gustavsson A, Bjorkman J, Ljungcrantz C, et al. Pharmaceutical treatment patterns for patients with a diagnosis related to chronic pain initiating a slow-release strong opioid treatment in Sweden. Pain. 2012;153:2325–2331. doi: 10.1016/j.pain.2012.07.011. [DOI] [PubMed] [Google Scholar]
- Hale ME, Ahdieh H, Ma T, Rauck R, Oxymorphone ER Study Group 1 Efficacy and safety of OPANA ER (oxymorphone extended release) for relief of moderate to severe chronic low back pain in opioid-experienced patients: a 12-week, randomized, double-blind, placebo-controlled study. J Pain. 2007;8:175–184. doi: 10.1016/j.jpain.2006.09.011. [DOI] [PubMed] [Google Scholar]
- Hale ME, Dvergsten C, Gibel J. Efficacy and safety of oxymorphone extended release in chronic low back pain: results of a randomized, double-blind, placebo- and active-controlled phase III study. J Pain. 2005;6:21–28. doi: 10.1016/j.jpain.2004.09.005. [DOI] [PubMed] [Google Scholar]
- Hale ME, Fleischmann R, Salzman R, Wild J, Iwan T, Swanton RE, et al. Efficacy and safety of controlled-release versus immediate-release oxycodone randomized, double-blind evaluation in patients with chronic back pain. Clin J Pain. 1999;15:179–183. doi: 10.1097/00002508-199909000-00004. [DOI] [PubMed] [Google Scholar]
- Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300:2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- Halpern L. Substitution-detoxification and its role in the management of chronic benign pain. J Clin Psychiat. 1982;43:10–14. [PubMed] [Google Scholar]
- Harati Y, Gooch C, Swenson M, et al. Maintenance of the long-term effectiveness of tramadol in treatment of the pain of diabetic neuropathy. J Diabetes Complications. 2000;14:65–70. doi: 10.1016/s1056-8727(00)00060-x. [DOI] [PubMed] [Google Scholar]
- Harke H, Gretenkort P, Ladleif HU, Rahman S, Harke O. The response of neuropathic pain and pain in complex regional pain syndrome 1 to carbamazepine and sustained-release morphine in patients pretreated with spinal cord stimulation: a double-blinded randomized study. Anesth Analg. 2001;92:488–495. doi: 10.1097/00000539-200102000-00039. [DOI] [PubMed] [Google Scholar]
- Hassenbusch SJ, Stanton-Hicks M, Covington EC, Walsh JG, Guthrey DS. Long-term intraspinal infusions of opioids in the treatment of neuropathic pain. J Pain Symptom Manage. 1995;10:527–543. doi: 10.1016/0885-3924(95)00087-f. [DOI] [PubMed] [Google Scholar]
- Heimer R, Dasgupta N, Irwin KKS, et al. Chronic pain, addiction severity, and misuse of opioids in Cumberland County, Maine. Addict Behav. 2012;37:346–349. doi: 10.1016/j.addbeh.2011.11.017. [DOI] [PubMed] [Google Scholar]
- Heit HA. Addiction, physical dependence, and tolerance: precise definitions to help clinicians evaluate and treat chronic pain patients. J Pain Palliat Care Pharmacother. 2003;17:15–29. doi: 10.1080/j354v17n01_03. [DOI] [PubMed] [Google Scholar]
- Hill CS. Government regulatory influences on opioid prescribing and their impact on the treatment of pain of non-malignant origin. J Pain Symptom Manage. 1996;11:287–298. doi: 10.1016/0885-3924(95)00203-0. [DOI] [PubMed] [Google Scholar]
- Hoffmann NG, Olofsson O, Salen B, Wickstrom L. Prevalence of abuse and dependency in chronic pain patients. Int J Addict. 1995;30:919–927. doi: 10.3109/10826089509055820. [DOI] [PubMed] [Google Scholar]
- Højsted J, Nielsen PR, Guldstrand SK, Frich L, Sjøgren P. Classification and identification of opioid addiction in chronic pain patients. Eur J Pain. 2010;14:1014–1020. doi: 10.1016/j.ejpain.2010.04.006. [DOI] [PubMed] [Google Scholar]
- Højsted J, Sjørgren P. Addiction to opioids in chronic pain patients: a literature review. Eur J Pain. 2007;11:490–518. doi: 10.1016/j.ejpain.2006.08.004. [DOI] [PubMed] [Google Scholar]
- Huse E, Larbig W, Flor H, Birbaumer N. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90:47–55. doi: 10.1016/s0304-3959(00)00385-7. [DOI] [PubMed] [Google Scholar]
- Ives TJ, Chelminski PR, Hammett-Stabler CA, et al. Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Serv Res. 2006;6:46. doi: 10.1186/1472-6963-6-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadad AR, Carroll D, Glynn CJ, Moore RA, McQuay HJ. Morphine responsiveness of chronic pain: double-blind randomised crossover study with patient-controlled analgesia. Lancet. 1992;339:1367–1371. doi: 10.1016/0140-6736(92)91194-d. [DOI] [PubMed] [Google Scholar]
- Jamison RN, Raymond SA, Slawsby EA, Nedeljkovic SS, Katz NP. Opioid therapy for chronic noncancer back pain. A randomized prospective study. Spine. 1998;23:2591–2600. doi: 10.1097/00007632-199812010-00014. [DOI] [PubMed] [Google Scholar]
- Jamison RN, Ross EL, Michna E, Chen LQ, Holcomb C, Wasan AD. Substance misuse treatment for high-risk chronic pain patients on opioid therapy: a randomized trial. Pain. 2010;150:390–400. doi: 10.1016/j.pain.2010.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamison RN, Ross EL, Wasan AD, Michna E. Comment on Ballantyne and LaForge, Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 2007;132:218–219. doi: 10.1016/j.pain.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Jamison RN, Serraillier J, Michna E. Assessment and treatment of abuse risk in opioid prescribing for chronic pain. Pain Res Treat. 2011 Oct 10; doi: 10.1155/2011/941808. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joranson DE, Ryan KM, Gilson AM, et al. Trends in medical use and abuse of opioid analgesics. JAMA. 2000;283:1710–1714. doi: 10.1001/jama.283.13.1710. [DOI] [PubMed] [Google Scholar]
- Kahan M, Srivastava A, Wilson L, Gourlay D, Midmer D. Misuse of and dependence on opioids: study of chronic pain patients. Can Fam Physician. 2006;52:1081–1087. [PMC free article] [PubMed] [Google Scholar]
- Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain. 2004;112:372–380. doi: 10.1016/j.pain.2004.09.019. [DOI] [PubMed] [Google Scholar]
- Kanoff RB. Intraspinal delivery of opiates by an implantable, programmable pump in patients with chronic, intractable pain of nonmalignant origin. J Am Osteopath Assoc. 1994;94:487–493. [PubMed] [Google Scholar]
- Katz MH. Long-term opioid treatment of nonmalignant pain: a believer loses his faith. Arch Intern Med. 2010;170:1422–1424. doi: 10.1001/archinternmed.2010.335. [DOI] [PubMed] [Google Scholar]
- Katz N, Sun S, Johnson F, Stauffer J. ALO-01 (morphine sulfate and naltrexone hydrochloride) extended-release capsules in the treatment of chronic pain of osteoarthritis of the hip or knee pharmacokinetics, efficacy, and safety. J Pain. 2010;11:303–311. doi: 10.1016/j.jpain.2009.07.017. [DOI] [PubMed] [Google Scholar]
- Katz WA. Opioids for nonmalignant pain. Rheum Dis Clin North Am. 2008;34:387–413. doi: 10.1016/j.rdc.2008.04.004. [DOI] [PubMed] [Google Scholar]
- Keller CE, Ashrafoun L, Neumann AM, Van Klein J, Fox CH, Blondell RD. Practices, perceptions, and concerns of primary care physicians about opioid dependence associated with the treatment of chronic pain. Subst Abus. 2012;33:103–113. doi: 10.1080/08897077.2011.630944. [DOI] [PubMed] [Google Scholar]
- Kennedy JA, Crowley TJ. Chronic pain and substance abuse: a pilot study of opioid maintenance. J Subst Abuse Treat. 1990;7:233–238. doi: 10.1016/0740-5472(90)90046-s. [DOI] [PubMed] [Google Scholar]
- Kirsh K, Jass C, Bennett D, Hagen E, Passik S. Initial development of a survey tool to detect issues of chemical coping in chronic pain patients. Palliat Support Care. 2007;5:219–226. doi: 10.1017/s1478951507000387. [DOI] [PubMed] [Google Scholar]
- Kivitz A, Ma C, Ahdieh H, Galer BS. A 2-week, multicenter, randomized, double-blind, placebo-controlled, dose-ranging, phase III trial comparing the efficacy of oxymorphone extended release and placebo in adults with pain associated with osteoarthritis of the hip or knee. Clin Ther. 2006;28:352–364. doi: 10.1016/j.clinthera.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Kjaersgaard-Andersen P, Nafei A, Skov O, Madsen F, Andersen HM, Kroner K, et al. Codeine plus paracetamol versus paracetamol in longer-term treatment of chronic pain due to osteoarthritis of the hip. A randomised, double-blind, multi-centre study. Pain. 1990;43:309–318. doi: 10.1016/0304-3959(90)90028-C. [DOI] [PubMed] [Google Scholar]
- Kouyanou K, Pither CE, Wessely S. Medication misuse, abuse and dependence in chronic pain patients. J Psychosom Res. 1997;43:497–504. doi: 10.1016/s0022-3999(97)00171-2. [DOI] [PubMed] [Google Scholar]
- Krebs EE, Becker WC, Zerzan J, Bair MJ, McCoy K, Hui S. Comparative mortality among Department of Veterans Affairs patients prescribed methadone or long-acting morphine for chronic pain. Pain. 2011;152:1789–1795. doi: 10.1016/j.pain.2011.03.023. [DOI] [PubMed] [Google Scholar]
- Ladouceur R. Should we prescribe opioids for chronic noncancer pain? Can Fam Physician. 2011;57:864–865. [PMC free article] [PubMed] [Google Scholar]
- Langford R, McKenna F, Ratcliffe S, Vojtassak J, Richarz U. Transdermal fentanyl for improvement of pain and functioning in osteoarthritis: a randomized, placebo-controlled trial. Arthritis Rheum. 2006;54:1829–1837. doi: 10.1002/art.21884. [DOI] [PubMed] [Google Scholar]
- Liebschutz JM, Alford DP. Safe opioid prescribing: a long way to go. J Gen Intern Med. 2011;26:951–952. doi: 10.1007/s11606-011-1797-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang DY, Guo T, Liao G, Kingery WS, Peltz G, Clark JD. Chronic pain and genetic background interact and influence opioid analgesia, tolerance, and physical dependence. Pain. 2006;121:232–240. doi: 10.1016/j.pain.2005.12.026. [DOI] [PubMed] [Google Scholar]
- Lipman AG. Treatment options for chronic pain management: opioids revisited. Manag Care. 2007;16:5–9. [PubMed] [Google Scholar]
- Maier C, Hildebrandt J, Klinger R, Henrich-Eberl C, Lindena G, MONTAS Study Group Morphine responsiveness, efficacy and tolerability in patients with chronic non-tumor associated pain – results of a doubleblind placebo-controlled trial (MONTAS) Pain. 2002;97:223–233. doi: 10.1016/S0304-3959(02)00020-9. [DOI] [PubMed] [Google Scholar]
- Manchikanti KN, Manchikanti L, Damron KS, Pampati V, Fellows B. Increasing deaths from opioid analgesics in the United States: An evaluation in an interventional pain management practice. J Opioid Manage. 2008;4:271–283. doi: 10.5055/jom.2008.0031. [DOI] [PubMed] [Google Scholar]
- Manchikanti L, Ailinani H, Koyyalagunta D, et al. A systematic review of randomized trials of long-term opioid management for chronic non-cancer pain. Pain Physician. 2011;14:91–121. [PubMed] [Google Scholar]
- Manchikanti L, Cash KA, Damron KS, Manchukonda R, Pampati V, McManus CD. Controlled substance abuse and illicit drug use in chronic pain patients: an evaluation of multiple variables. Pain Physician. 2006;9:215–225. [PubMed] [Google Scholar]
- Manchikanti L, Damron KS, McManus CD, Barnhill RC. Patterns of illicit drug use in patients with chronic pain at initial evaluation: a prospective, observational study. Pain Physician. 2004;7:431–437. [PubMed] [Google Scholar]
- Manchikanti L, Fellows B, Ailinani H, Pampati V. Therapeutic use, abuse and nonmedical use of opioids: a ten-year perspective. Pain Physician. 2010;13:401–435. [PubMed] [Google Scholar]
- Manchikanti L, Giordano J, Boswell MV, Fellows B, Manchukonda R, Pampati V. Psychological factors as predictors of opioid abuse and illicit drug use in chronic pain patients. J Opioid Manag. 2007;3:89–100. doi: 10.5055/jom.2007.0045. [DOI] [PubMed] [Google Scholar]
- Manchikanti L, Manchukonda R, Damron KS, Brandon D, McManus CD, Cash K. Does adherence monitoring reduce controlled substance abuse in chronic pain patients? Pain Physician. 2006;9:57–60. [PubMed] [Google Scholar]
- Manchikanti L, Manchukonda R, Pampati V, Damron KS. Evaluation of abuse of prescription and illicit drugs in chronic pain patients receiving short-acting (hydrocodone) or long-acting (methadone) opioids. Pain Physician. 2005;8:257–261. [PubMed] [Google Scholar]
- Manubay JM, Muchow C, Sullivan MA. Prescription drug abuse: epidemiology, regulatory issues, chronic pain management with narcotic analgesics. Prim Care. 2011;38:71–90. doi: 10.1016/j.pop.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markenson JA, Croft J, Zhang PG, Richards P. Treatment of persistent pain associated with osteoarthritis with controlled-release oxycodone tablets in a randomized controlled clinical trial. Clin Pain. 2005;21:524–535. doi: 10.1097/01.ajp.0000146215.86038.38. [DOI] [PubMed] [Google Scholar]
- Martell BA, O’Connor PG, Kerns RD, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146:116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- Martin TJ, Ewan E. Chronic pain alters drug self-administration: implications for addiction and pain mechanisms. Exp Clin Psychopharmacol. 2008;16:357–366. doi: 10.1037/a0013597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maruta T, Swanson DW, Finlayson RE. Drug abuse and dependency in patients with chronic pain. Mayo Clin Proc. 1979;54:241–244. [PubMed] [Google Scholar]
- Matsumoto AK, Babul N, Ahdieh H. Oxymorphone extended-release tablets relieve moderate to severe pain and improve physical function in osteoarthritis: results of a randomized, double-blind, placebo- and active-controlled phase III trial. Pain Med. 2005;6:357–366. doi: 10.1111/j.1526-4637.2005.00057.x. [DOI] [PubMed] [Google Scholar]
- McCarberg BH. Chronic pain: reducing costs through early implementation of adherence testing and recognition of opioid misuse. Postgrad Med. 2011;123:132–139. doi: 10.3810/pgm.2011.11.2503. [DOI] [PubMed] [Google Scholar]
- McIlwain H, Ahdieh H. Safety tolerability, and effectiveness of oxymorphone extended release for moderate to severe osteoarthritis pain: a one-year study. Am J Ther. 2005;12:106–112. doi: 10.1097/01.mjt.0000139442.65914.f9. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, McClair VL. Epidemiology of substance use disorders. Hum Genet. 2012;131:779–789. doi: 10.1007/s00439-012-1168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michna E, Ross EL, Hynes WL, et al. Predicting aberrant drug behavior in patients treated for chronic pain: importance of abuse history. J Pain Symptom Manage. 2004;28:250–258. doi: 10.1016/j.jpainsymman.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Milligan K, Lanteri-Minet M, Borchert K, et al. Evaluation of long-term efficacy and safety of transdermal fentanyl in the treatment of chronic noncancer pain. J Pain. 2001;2:197–204. doi: 10.1054/jpai.2001.25352. [DOI] [PubMed] [Google Scholar]
- Miotto K, Compton P, Ling W, Conolly M. Diagnosing addictive disease in chronic pain patients. Psychosomatics. 1996;37:223–235. doi: 10.1016/S0033-3182(96)71561-X. [DOI] [PubMed] [Google Scholar]
- Miotto K, McCann MJ, Rawson RA, Frosch D, Ling W. Overdose, suicide attempts and death among a cohort of naltrexone-treated opioid addicts. Drug Alcohol Depend. 1997;45:131–134. doi: 10.1016/s0376-8716(97)01348-3. [DOI] [PubMed] [Google Scholar]
- Mironer YE, Tollison CD. Methadone in the intrathecal treatment of chronic nonmalignant pain resistant to other neuroaxial agents: the first experience. Neuromodulation. 2001;4:25–31. doi: 10.1046/j.1525-1403.2001.00025.x. [DOI] [PubMed] [Google Scholar]
- Mitchell AM, Dewey CM. Chronic pain in patients with substance abuse disorder: general guidelines and an approach to treatment. Postgrad Med. 2008;120:75–79. doi: 10.3810/pgm.2008.04.1763. [DOI] [PubMed] [Google Scholar]
- Modesto-Lowe V, Brooks D, Freedman K, Hargus E. Addiction and chronic pain: diagnostic and treatment dilemmas. Conn Med. 2007;71:139–144. [PubMed] [Google Scholar]
- Morasco BJ, Dobscha SK. Prescription medication misuse and substance use disorder in VA primary care patients with chronic pain. Gen Hosp Psychiatry. 2008;30:93–99. doi: 10.1016/j.genhosppsych.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Moulin DE, Iezzi A, Amireh R, Sharpe WK, Boyd D, Merskey H. Randomised trial of oral morphine for chronic non-cancer pain. Lancet. 1996;347:143–147. doi: 10.1016/s0140-6736(96)90339-6. [DOI] [PubMed] [Google Scholar]
- Müller FO, Odendaal CL, Müller FR, Raubenheimer J, Middle MV, Kummer M. Comparison of the efficacy and tolerability of a paracetamol/codeine fixed-dose combination with tramadol in patients with refractory chronic back pain. Arzneimittelforschung. 1998;48:675–679. [PubMed] [Google Scholar]
- Mystakidou K, Parpa E, Tsilika E, et al. Long-term management of noncancer pain with transdermal therapeutic system-fentanyl. J Pain. 2003;4:298–306. doi: 10.1016/s1526-5900(03)00632-1. [DOI] [PubMed] [Google Scholar]
- Nedeljkovic SS, Wasan A, Jamison RN. Assessment of efficacy of long-term opioid therapy in pain patients with substance abuse potential. Clin J Pain. 2002;18:S39–S51. doi: 10.1097/00002508-200207001-00005. [DOI] [PubMed] [Google Scholar]
- Nicholson B, Ross E, Sasaki J, Weil A. Randomized trial comparing polymer-coated extended-release morphine sulfate to controlled-release oxycodone HCl in moderate to severe nonmalignant pain. Curr Med Res Opin. 2006;22:1503–1514. doi: 10.1185/030079906X115603. [DOI] [PubMed] [Google Scholar]
- Noble M, Tregear SJ, Treadwell JR, Schoelles K. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage. 2008;35:214–228. doi: 10.1016/j.jpainsymman.2007.03.015. [DOI] [PubMed] [Google Scholar]
- Nüesch E, Rutjes AW, Husni E, Welch V, Jüni P. Oral or transdermal opioids for osteoarthritis of the knee or hip. Cochrane Database Syst Rev. 2009;4:CD003115. doi: 10.1002/14651858.CD003115.pub3. [DOI] [PubMed] [Google Scholar]
- Okie S. A flood of opioids, a rising tide of deaths. N Engl J Med. 2010;363:1981–1985. doi: 10.1056/NEJMp1011512. [DOI] [PubMed] [Google Scholar]
- Olsen Y, Daumit GL. Chronic pain and narcotics: a dilemma for primary care. J Gen Intern Med. 2002;17:238–240. doi: 10.1046/j.1525-1497.2002.20109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pade PA, Cardon KE, Hoffman RM, Geppert CM. Prescription opioid abuse, chronic pain, and primary care: a co-occurring disorders, clinic in the chronic disease model. J Subst Abuse Treat. 2012;43:446–450. doi: 10.1016/j.jsat.2012.08.010. [DOI] [PubMed] [Google Scholar]
- Panjabi SS, Panjabi RS, Shepherd MD, Lawson KA, Johnsrud M, Barner J. Extended-release, once-daily morphine (Avinza) for the treatment of chronic nonmalignant pain: effect on pain, depressive symptoms, and cognition. Pain Med. 2008;9:985–993. doi: 10.1111/j.1526-4637.2008.00483.x. [DOI] [PubMed] [Google Scholar]
- Park J, Lavin R. Risk factors associated with opioid medication misuse in community-dwelling older adults with chronic pain. Clin J Pain. 2010;26:647–655. doi: 10.1097/AJP.0b013e3181e94240. [DOI] [PubMed] [Google Scholar]
- Passik S, Kirsh K, Donaghy K, Portenoy R. Pain and aberrant drug-related behaviors in medically ill patients with and without histories of substance abuse. Clin J Pain. 2006;22:173–181. doi: 10.1097/01.ajp.0000161525.48245.aa. [DOI] [PubMed] [Google Scholar]
- Paulozzi L, Budnitz D, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15:618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Logan JE, Hall AJ, McKinstry E, Kaplan JA, Crosby AE. A comparison of drug overdose deaths involving methadone and other opioid analgesics in West Virginia. Addiction. 2009;104:1541–1548. doi: 10.1111/j.1360-0443.2009.02650.x. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Ryan GW. Opioid analgesics and rates of fatal drug poisoning in the United States. Am J Prev Med. 2006;31:506–511. doi: 10.1016/j.amepre.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Weisler RH, Patkar AA. A national epidemic of unintentional prescription opioid overdose deaths: how physicians can help control it. J Clin Physychiatry. 2011;72:589–592. doi: 10.4088/JCP.10com06560. [DOI] [PubMed] [Google Scholar]
- Peat S, Sweet P, Miah Y, Barklamb M, Larsen U. Assessment of analgesia in human chronic pain. Randomized double-blind crossover study of once daily repro-dose morphine versus MST continus. Eur J Clin Pharmacol. 1999;55:577–581. doi: 10.1007/s002280050675. [DOI] [PubMed] [Google Scholar]
- Peles E, Schreiber S, Adelson M. Documented poor sleep among methadone-maintained patients is associated with chronic pain and benzodiazepine abuse, but not with methadone use. Eur Neuropsychopharmacol. 2009;19:581–588. doi: 10.1016/j.euroneuro.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Peloso PM, Bellamy N, Bensen W, Thomson GTD, Harsanyi Z, Babul N, et al. Double blind randomized placebo control trial of controlled release codeine in the treatment of osteoarthritis of the hip or knee. J Rheumatol. 2000;27:764–771. [PubMed] [Google Scholar]
- Pillet S, Eschiti V. Managing chronic pain in patients with cancer who have a history of substance abuse. Clin J Oncol Nurs. 2008;12:663–667. doi: 10.1188/08.CJON.663-667. [DOI] [PubMed] [Google Scholar]
- Pohl M, Smith L. Chronic pain and addiction: challenging co-occurring disorders. J Phsychoactive Drugs. 2012;44:119–124. doi: 10.1080/02791072.2012.684621. [DOI] [PubMed] [Google Scholar]
- Popenhagen MP. Collaborative practice. Undertreatment of pain and fears of addiction in pediatric chronic pain patients: how do we stop the problem? J Spec Pediatr Nurs. 2006;11:61–67. doi: 10.1111/j.1744-6155.2006.00044.x. [DOI] [PubMed] [Google Scholar]
- Portenoy RK, Farrar JT, Backonja MM, et al. Long-term use of controlled-release oxycodone for noncancer pain: results of a 3-year registry study. Clin J Pain. 2007;23:287–299. doi: 10.1097/AJP.0b013e31802b582f. [DOI] [PubMed] [Google Scholar]
- Portenoy RK, Foley KM. Chronic use of opioid analgesics in nonmalignant pain – report of 38 cases. Pain. 1986;25:171–186. doi: 10.1016/0304-3959(86)90091-6. [DOI] [PubMed] [Google Scholar]
- Portenoy RK. Appropriate use of opioids for persistent non-cancer pain. Lancet. 2004;364:739–740. doi: 10.1016/S0140-6736(04)16951-1. [DOI] [PubMed] [Google Scholar]
- Portenoy RK. Opioid therapy for chronic nonmalignant pain: a review of the critical issues. J Pain Symptom Manage. 1996;11:203–217. doi: 10.1016/0885-3924(95)00187-5. [DOI] [PubMed] [Google Scholar]
- Potter M, Schafer S, Gonzalez-Mendez E, et al. Opioids for chronic non-malignant pain. Attitudes and practices of primary care physicians in the UCSF/Stanford Collaborative Research Network. University of California, San Francisco. J Fam Pract. 2001;50:145–151. [PubMed] [Google Scholar]
- Quiding H, Grimstad J, Rusten K, Stubhaug A, Bremnes J, Breivik H. Ibuprofen plus codeine, ibuprofen, and placebo in a single- and multidose cross-over comparison for coxarthrosis pain. Pain. 1992;50:303–307. doi: 10.1016/0304-3959(92)90035-A. [DOI] [PubMed] [Google Scholar]
- Rainov NG, Heidecke V, Burkert W. Long-term intrathecal infusion of drug combinations for chronic back and leg pain. J Pain Symptom Manage. 2001;22:862–871. doi: 10.1016/s0885-3924(01)00319-0. [DOI] [PubMed] [Google Scholar]
- Raja SN, Haythornthwaite JA, Pappagallo M, et al. Opioids versus antidepressants in postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology. 2002;59:1015–1021. doi: 10.1212/wnl.59.7.1015. [DOI] [PubMed] [Google Scholar]
- Rauck RL, Bookbinder SA, Bunker TR, et al. The ACTION study: a randomized, open-label, multicenter trial comparing once-a-day extended-release morphine sulfate capsules (AVINZA) to twice-a-day controlled-release oxycodone hydrochloride tablets (OxyContin) for the treatment of chronic, moderate to severe low back pain. J Opioid Manag. 2006;2:155–166. doi: 10.5055/jom.2006.0025. [DOI] [PubMed] [Google Scholar]
- Reid MC, Engles-Horton LL, Weber MB, Kerns RD, Rogers EL, O’Connor PG. Use of opioid medications for chronic noncancer pain syndromes in primary care. J Gen Intern Med. 2002;17:173–179. doi: 10.1046/j.1525-1497.2002.10435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisfield GM, Sloan PA. Physician identification of opioid diversion: a difficult diagnosis. J Opioid Manag. 2012;8:5–6. doi: 10.5055/jom.2012.0090. [DOI] [PubMed] [Google Scholar]
- Ringe JD, Faber H, Bock O, et al. Transdermal fentanyl for the treatment of back pain caused by vertebral osteoporosis. Rheumatol Int. 2002;22:199–203. doi: 10.1007/s00296-002-0217-8. [DOI] [PubMed] [Google Scholar]
- Rosenblatt RA, Catlin M. Opioids for chronic pain: first do no harm. Ann Fam Med. 2012;10:300–301. doi: 10.1370/afm.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum A, Marsch LA, Joseph H, Portenoy RK. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol. 2008;16:405–416. doi: 10.1037/a0013628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowbotham MC, Reisner-Keller LA, Fields HL. Both intravenous lidocaine and morphine reduce the pain of postherpetic neuralgia. Neurology. 1991;41:1024–1028. doi: 10.1212/wnl.41.7.1024. [DOI] [PubMed] [Google Scholar]
- Rowbotham MC, Twilling L, Davies PS, Reisner L, Taylor K, Mohr D. Oral opioid therapy for chronic peripheral and central neuropathic pain. N Engl J Med. 2003;348:1223–1232. doi: 10.1056/NEJMoa021420. [DOI] [PubMed] [Google Scholar]
- Saffer K, Colombo C, Brown D, Mundt MP, Fleming MF. Addiction Severity Index in a chronic pain sample receiving opioid therapy. J Subst Abuse Treat. 2007;33:303–311. doi: 10.1016/j.jsat.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salzman RT, Roberts MS, Wild J, Fabian C, Reder RF, Goldenheim PD. Can a controlled-release oral dose form of oxycodone be used as readily as an immediate-release form for the purpose of titrating to stable pain control? J Pain Symptom Manage. 1999;18:271–279. doi: 10.1016/s0885-3924(99)00079-2. [DOI] [PubMed] [Google Scholar]
- Sandkühler J, Kress HG. Opioids for chronic nonmalignant and neuropathic pain. Eur J Pain. 2005;9:99–100. doi: 10.1016/j.ejpain.2004.12.001. [DOI] [PubMed] [Google Scholar]
- Saroyan JM, Cheng WY, Taylor DC, Afzal A, Sonty N, Sullivan MA. Select practice behaviors of clinicians on the use of opioids for adolescents with subacute and chronic nonmalignant pain. J Opioid Manag. 2011;7:123–134. doi: 10.5055/jom.2011.0055. [DOI] [PubMed] [Google Scholar]
- Saunders KW, Dunn KM, Merrill JO, et al. Relationship of opioid use and dosage levels to fractures in older chronic pain patients. J Gen Intern Med. 2010;25:310–315. doi: 10.1007/s11606-009-1218-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage SR. Management of opioid medications in patients with chronic pain and risk of substance misuse. Curr Psychiatry Rep. 2009;11:377–384. doi: 10.1007/s11920-009-0057-2. [DOI] [PubMed] [Google Scholar]
- Schieffer BM, Pham Q, Labus J, Baria A, Van Vort W, Davis P, Davis F, Naliboff BD. Pain medication beliefs and medication misuse in chronic pain. J Pain. 2005;6:620–629. doi: 10.1016/j.jpain.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Schneider J P, Kirsh KL. Defining clinical issues around tolerance, hyperalgesia, and addiction: a quantitative and qualitative outcome study of long-term opioid dosing in a chronic pain practice. J Opioid Manag. 2010;6:385–395. doi: 10.5055/jom.2010.0036. [DOI] [PubMed] [Google Scholar]
- Schneider JP. Chronic pain management: evaluating the use of opioids. Case Manager. 1999;10:61–66. doi: 10.1016/s1061-9259(99)80109-x. [DOI] [PubMed] [Google Scholar]
- Schofferman J. Long-term opioid analgesic therapy for severe refractory lunbar spine pain. Clin J Pain. 1999;15:136–140. doi: 10.1097/00002508-199906000-00011. [DOI] [PubMed] [Google Scholar]
- Sees KL, Clark HW. Opioid use in the treatment of chronic pain: assessment of addiction. J Pain Symptom Manage. 1993;8:257–264. doi: 10.1016/0885-3924(93)90154-n. [DOI] [PubMed] [Google Scholar]
- Sehgal N, Manchikanti L, Smith HS. Prescription opioid abuse in chronic pain: a review of opioid abuse predictors and strategies to curb opioid abuse. Pain Physician. 2012;15:ES67–ES92. [PubMed] [Google Scholar]
- Serban S. Drug abuse in the chronic pain patient. Int Anesthesiol Clin. 2011;49:135–145. doi: 10.1097/AIA.0b013e31820aae93. [DOI] [PubMed] [Google Scholar]
- Simpson RK, Jr, Edmondson EA, Constant CF, Collier C. Transdermal fentanyl as treatment for chronic low back pain. J Pain Symptom Manage. 1997;14:218–224. doi: 10.1016/s0885-3924(97)00183-8. [DOI] [PubMed] [Google Scholar]
- Sjøgren P, Grønbaek M, Peuckmann V, Ekholm O. A population-based cohort study on chronic pain: the role of opioids. Clin J Pain. 2010;26:763–769. doi: 10.1097/AJP.0b013e3181f15daf. [DOI] [PubMed] [Google Scholar]
- Solanki DR, Koyyalagunta D, Shah RV, Silverman SM, Manchikanti L. Monitoring opioid adherence in chronic pain patients: assessment of risk of substance misuse. Pain Physician. 2011;14:E119–E131. [PubMed] [Google Scholar]
- Solomon DH, Rassen JA, Glynn RJ, et al. The comparative safety of opioids for nonmalignant pain in older adults. Arch Intern Med. 2010;170:1979–1986. doi: 10.1001/archinternmed.2010.450. [DOI] [PubMed] [Google Scholar]
- Starrels JL, Becker WC, Alford DP, Kapoor A, Williams AR, Turner BJ. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152:712–720. doi: 10.7326/0003-4819-152-11-201006010-00004. [DOI] [PubMed] [Google Scholar]
- Streltzer J, Johansen L. Prescription drug dependence and evolving beliefs about chronic pain management. Am J Psychiatry. 2006;163:594–598. doi: 10.1176/ajp.2006.163.4.594. [DOI] [PubMed] [Google Scholar]
- Streltzer J, Ziegler P, Johnson B. Cautionary guidelines for the use of opiods in chronic pain. American Academy of Addiction Psychiatry. Am J Addict. 2009 Jan-Feb;18:1–4. doi: 10.1080/10550490802544508. [DOI] [PubMed] [Google Scholar]
- Sullivan MD. Limiting the potential harms of high-dose opioid therapy: comment on “Opioid dose and drug-related mortality in patients with nonmalignant pain”. Arch Intern Med. 2011;171:691–693. doi: 10.1001/archinternmed.2011.101. [DOI] [PubMed] [Google Scholar]
- Sullivan MD, Edlund MJ, Fan MY, Devries A, Brennan Braden J, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000–2005 in commercial and Medicaid Insurance plans: The increase in legitimate use as well as abuse. JAMA. 2007;297:249–251. [Google Scholar]
- Tennant F, Moll D, DePaulo V. Topical morphine for peripheral pain. Lancet. 1993;342:1047–1048. doi: 10.1016/0140-6736(93)92900-e. [DOI] [PubMed] [Google Scholar]
- Tennant FSJ, Uelmen GF. Narcotic maintenance for chronic pain. Medical and legal guidelines. Postgrad Med. 1983;73:81–83. doi: 10.1080/00325481.1983.11698315. [DOI] [PubMed] [Google Scholar]
- Tennant FS., Jr (-)-alpha-Acetylmethadol for treatment of chronic pain patients who abuse opioids. Drug Alcohol Depend. 1983;12:243–247. doi: 10.1016/0376-8716(83)90066-2. [DOI] [PubMed] [Google Scholar]
- Tetrault JM, Desai RA, Becker WC, Fiellin DA, Concato J, Sullivan LE. Gender and non-medical use of prescription opioids: results from a national US survey. Addiction. 2008;103:258–268. doi: 10.1111/j.1360-0443.2007.02056.x. [DOI] [PubMed] [Google Scholar]
- Thurel C, Bardin T, Boccard E. Analgesic efficacy of an association of 500-mg paracetamol plus 30-mg codeine versus 400-mg paracetamol plus 30-mg dextropropoxyphene in repeated doses for chronic lower back pain. Curr Ther Res. 1991;50:463–473. [Google Scholar]
- Toblin RL, Paulozzi LJ, Logan JE, Hall AJ, Kaplan JA. Mental illness and psychotropic drug use among prescription drug overdose deaths: A medical examiner chart review. J Clin Psychiatry. 2010;71:491–496. doi: 10.4088/JCP.09m05567blu. [DOI] [PubMed] [Google Scholar]
- Trescot AM, Helm S, Hansen H, et al. Opioids in the management of chronic non-cancer pain: An update of American Society of the Interventional Pain Physicians’ (ASIPP) guidelines. Pain Physician. 2008;11:S5–S62. [PubMed] [Google Scholar]
- Tulchinsky A. Comment on Ballantyne JC, LaForge KS. Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 2007;132:222–223. doi: 10.1016/j.pain.2007.08.018. [DOI] [PubMed] [Google Scholar]
- Turk DC, Swanson KS, Gatchel RJ. Predicting opioid misuse by chronic pain patients: a systematic review and literature synthesis. Clin J Pain. 2008;24:497–508. doi: 10.1097/AJP.0b013e31816b1070. [DOI] [PubMed] [Google Scholar]
- Tutak U, Doleys DM. Intrathecal infusion systems for treatment of chronic low back and leg pain of noncancer origin. South Med J. 1996;89:295–300. doi: 10.1097/00007611-199603000-00007. [DOI] [PubMed] [Google Scholar]
- Von Korff M, Deyo RA. Potent opioids for chronic musculoskeletal pain: flying blind? Pain. 2004;109:207–209. doi: 10.1016/j.pain.2004.02.019. [DOI] [PubMed] [Google Scholar]
- Von Korff M, Kolodny A, Deyo R, Chou R. Long-term opioid therapy reconsidered. Ann Intern Med. 2011;155:325–328. doi: 10.1059/0003-4819-155-5-201109060-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Korff MR. Opioids for chronic noncancer pain: as the pendulum swings, who should set prescribing standards for primary care? Ann Fam Med. 2012;10:302–303. doi: 10.1370/afm.1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner EA. Opioids for the treatment of chronic noncancer pain. Am J Med. 2012;125:1155–1161. doi: 10.1016/j.amjmed.2012.04.032. [DOI] [PubMed] [Google Scholar]
- Wasan AD, Correll DJ, Kissin I, O’Shea S, Jamison RN. Iatrogenic addiction in patients treated for acute or subacute pain: a systematic review. J Opioid Manag. 2006;2:16–22. doi: 10.5055/jom.2006.0003. [DOI] [PubMed] [Google Scholar]
- Wasan AD, Ross EL, Michna E, et al. Craving of prescription opioids in patients wth chronic pain: a longitudinal outcomes trial. J Pain. 2012;13:146–154. doi: 10.1016/j.jpain.2011.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson CP, Babul N. Efficacy of oxycodone in neuropathic pain. A randomized trial in postherpetic neuralgia. Neurology. 1998;50:1837–1841. doi: 10.1212/wnl.50.6.1837. [DOI] [PubMed] [Google Scholar]
- Watson CP, Moulin D, Watt-Watson J, Gordon A, Eisenhoffer J. Controlled-release oxycodone relieves neuropathic pain: a randomized controlled trial in painful diabetic neuropathy. Pain. 2003;105:71–78. doi: 10.1016/s0304-3959(03)00160-x. [DOI] [PubMed] [Google Scholar]
- Watterson O, Simpson DD, Sells SB. Death rates and causes of death among opioid addicts in community drug treatment programs during 1970–1973. Am J Drug Alcohol Abuse. 1975;2:99–111. doi: 10.3109/00952997509002726. [DOI] [PubMed] [Google Scholar]
- Weaver MF, Schnoll SH. Opioid treatment of chronic pain in patients with addiction. J Pain Palliat Care Pharmacother. 2002;16:5–26. doi: 10.1080/j354v16n03_02. [DOI] [PubMed] [Google Scholar]
- Webster L, St Marie B, McCarberg B, Passik SD, Panchal SJ, Voth E. Current status and evolving role of abuse-deterrent opioids in managing patients with chronic pain. J Opioid Manag. 2011;7:235–245. doi: 10.5055/jom.2011.0066. [DOI] [PubMed] [Google Scholar]
- Wiedemer NL, Harden PS, Arndt IO, Gallagher RM. The opioid renewal clinic: a primary care, managed approach to opioid therapy in chronic pain patients at risk for substance abuse. Pain Med. 2007;8:573–584. doi: 10.1111/j.1526-4637.2006.00254.x. [DOI] [PubMed] [Google Scholar]
- Wilsey BL, Fishman S, Li CS, Storment J, Albanese A. Markers of abuse liability of short- vs long-acting opioids in chronic pain patients: a randomized cross-over trial. Pharmacol Biochem Behav. 2009;94:98–107. doi: 10.1016/j.pbb.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson PR. Opioids and chronic pain. Clin J Pain. 1997;13:1–2. doi: 10.1097/00002508-199703000-00001. [DOI] [PubMed] [Google Scholar]
- Wilsey BL, Fishman SM, Tsodikov A, Ogden C, Symreng I, Ernst A. Psychological comorbidities predicting prescription opioid abuse among patients in chronic pain presenting to the emergency department. Pain Med. 2008;9:1107–1117. doi: 10.1111/j.1526-4637.2007.00401.x. [DOI] [PubMed] [Google Scholar]
- Woodcock J. A difficult balance – pain management, drug safety, and the FDA. N Engl J Med. 2009;361:2105–2107. doi: 10.1056/NEJMp0908913. [DOI] [PubMed] [Google Scholar]
- Wu SM, Compton P, Bolus R, et al. The addiction behaviors checklist: validation of a new clinician-based measure of inappropriate opioid use in chronic pain. J Pain Symptom Manage. 2006;32:342–351. doi: 10.1016/j.jpainsymman.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Smith BW. Impact of controlled-release oxycodone on efficacy beliefs and coping efforts among osteoarthritis patients with moderate to severe pain. Clin J Pain. 2005;21:471–477. doi: 10.1097/01.ajp.0000139910.97211.37. [DOI] [PubMed] [Google Scholar]
- Zenz M, Strumpf M, Tryba M. Long-term oral opioid therapy in patients with chronic nonmalignant pain. J Pain Symptom Manage. 1992;7:69–77. doi: 10.1016/0885-3924(92)90116-y. [DOI] [PubMed] [Google Scholar]
- Zgierska A, Miller M, Rabago D. Patient satisfaction, prescription drug abuse, and potential unintended consequences. JAMA. 2012;307:1377–1378. doi: 10.1001/jama.2012.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zochodne DW, Max MB. An old acquaintance: opioids in neuropathic pain. Neurology. 2003;60:894–895. doi: 10.1212/wnl.60.6.894. [DOI] [PubMed] [Google Scholar]
Footnotes
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.Chalmers TC, Smith H, Jr, Blackburn B, et al. A method for assessing the quality of a randomized control trial. Control Clin Trials. 1981;2(1):31–49. doi: 10.1016/0197-2456(81)90056-8. [DOI] [PubMed] [Google Scholar]
- 2.Evidence-Based Medicine Working Group Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992;268(17):2420–2425. doi: 10.1001/jama.1992.03490170092032. [DOI] [PubMed] [Google Scholar]
- 3.Guyatt GH, Oxman AD, Kunz R, et al. GRADE Working Group Going from evidence to recommendations. BMJ. 2008;336(7652):1049–1051. doi: 10.1136/bmj.39493.646875.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McQuay H, Moore A. An Evidence-Based Resource for Pain Relief. Oxford; Oxford University Press; 1998. [Google Scholar]
- 5.Loeser JD.Five crises in pain management Pain Clinical Updates 20122011–4.Available from: http://www.iasp-pain.org/AM/AMTemplate.cfm?Section=HOME,HOME&CONTENTID=15698&TEMPLATE=/CM/ContentDisplay.cfm&SECTION=HOME,HOMEAccessed June 6, 2013 [Google Scholar]
- 6.Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic noncancer pain: systematic review of efficacy and safety. Pain. 2004;112(3):372–380. doi: 10.1016/j.pain.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 7.Martell BA, O’Connor PG, Kerns RD, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146(2):116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 8.Noble M, Tregear SJ, Treadwell JR, Schoelles K. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage. 2008;35(2):214–228. doi: 10.1016/j.jpainsymman.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 9.Nuesch E, Rutjes AW, Husni E, Welch V, Juni P. Oral or transdermal opioids for osteoarthritis of the knee or hip [review] Cochrane Database Syst Rev. 2009;4:CD003115. doi: 10.1002/14651858.CD003115.pub3. [DOI] [PubMed] [Google Scholar]
- 10.Kissin I. Can a bibliometric indicator predict the success of a drug? Scientometrics. 2011;86(3):785–795. [Google Scholar]
- 11.France RD, Urban BJ, Keefe FJ. Long-term use of narcotic analgesics in chronic pain. Soc Sci Med. 1984;19(12):1379–1382. doi: 10.1016/0277-9536(84)90027-3. [DOI] [PubMed] [Google Scholar]
- 12.Portenoy RK, Foley KM. Chronic use of opioid analgesics in non-malignant pain: report of 38 cases. Pain. 1986;25(2):171–186. doi: 10.1016/0304-3959(86)90091-6. [DOI] [PubMed] [Google Scholar]
- 13.Zenz M, Strumpf M, Tryba M. Long-term oral opioid therapy in patients with chronic nonmalignant pain. J Pain Symptom Manage. 1992;7(2):69–77. doi: 10.1016/0885-3924(92)90116-y. [DOI] [PubMed] [Google Scholar]
- 14.Tennant F, Moll D, DePaulo V. Topical morphine for peripheral pain. Lancet. 1993;342(8878):1047–1048. doi: 10.1016/0140-6736(93)92900-e. [DOI] [PubMed] [Google Scholar]
- 15.Kanoff RB. Intraspinal delivery of opiates by an implantable, programmable pump in patients with chronic, intractable pain of nonmalignant origin. J Am Osteopath Assoc. 1994;94(6):487–493. [PubMed] [Google Scholar]
- 16.Hassenbusch SJ, Stanton-Hicks M, Covington EC, Walsh JG, Guthrey DS. Long-term intraspinal infusions of opioids in the treatment of neuropathic pain. J Pain Symptom Manage. 1995;10(7):527–543. doi: 10.1016/0885-3924(95)00087-f. [DOI] [PubMed] [Google Scholar]
- 17.Tutak U, Doleys DM. Intrathecal infusion systems for treatment of chronic low back and leg pain of noncancer origin. South Med J. 1996;89(3):295–300. doi: 10.1097/00007611-199603000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Simpson RK, Jr, Edmondson EA, Constant CF, Collier C. Transdermal fentanyl as treatment for chronic low back pain. J Pain Symptom Manage. 1997;14(4):218–224. doi: 10.1016/s0885-3924(97)00183-8. [DOI] [PubMed] [Google Scholar]
- 19.Angel IF, Gould HJ, Jr, Carey ME. Intrathecal morphine pump as a treatment option in chronic pain of nonmalignant origin. Surg Neurol. 1998;49(1):92–98. doi: 10.1016/s0090-3019(97)00287-5. [DOI] [PubMed] [Google Scholar]
- 20.Anderson VC, Burchiel KJ. A prospective study of long-term intrathecal morphine in the management of chronic nonmalignant pain. Neurosurgery. 1999;44(2):289–300. doi: 10.1097/00006123-199902000-00026. [DOI] [PubMed] [Google Scholar]
- 21.Hale ME, Fleischmann R, Salzman R, et al. Efficacy and safety of controlled-release versus immediate-release oxycodone randomized, double-blind evaluation in patients with chronic back pain. Clin J Pain. 1999;15(3):179–183. doi: 10.1097/00002508-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Salzman RT, Roberts MS, Wild J, Fabian C, Reder RF, Goldenheim PD. Can a controlled-release oral dose form of oxycodone be used as readily as an immediate-release form for the purpose of titrating to stable pain control? J Pain Symptom Manage. 1999;18(4):271–279. doi: 10.1016/s0885-3924(99)00079-2. [DOI] [PubMed] [Google Scholar]
- 23.Schofferman J. Long-term opioid analgesic therapy for severe refractory lumbar spine pain. Clin J Pain. 1999;15(2):136–140. doi: 10.1097/00002508-199906000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Harati Y, Gooch C, Swenson M, et al. Maintenance of the long-term effectiveness of tramadol in treatment of the pain of diabetic neuropathy. J Diabetes Complications. 2000;14(2):65–70. doi: 10.1016/s1056-8727(00)00060-x. [DOI] [PubMed] [Google Scholar]
- 25.Milligan K, Lanteri-Minet M, Borchert K, et al. Evaluation of long-term efficacy and safety of transdermal fentanyl in the treatment of chronic noncancer pain. J Pain. 2001;2(4):197–204. doi: 10.1054/jpai.2001.25352. [DOI] [PubMed] [Google Scholar]
- 26.Mironer YE, Tollison CD. Methadone in the intrathecal treatment of chronic nonmalignant pain resistant to other neuroaxial agents: the first experience. Neuromodulation. 2001;4(1):25–31. doi: 10.1046/j.1525-1403.2001.00025.x. [DOI] [PubMed] [Google Scholar]
- 27.Ringe JD, Faber H, Bock O, et al. Transdermal fentanyl for the treatment of back pain caused by vertebral osteoporosis. Rheumatol Int. 2002;22(5):199–203. doi: 10.1007/s00296-002-0217-8. [DOI] [PubMed] [Google Scholar]
- 28.Anderson VC, Burchiel KJ, Cooke B. A prospective, randomized trial of intrathecal injection vs epidural infusion in the selection of patients for continuous intrathecal opioid therapy. Neuromodulation. 2003;6(3):142–152. doi: 10.1046/j.1525-1403.2003.03023.x. [DOI] [PubMed] [Google Scholar]
- 29.Gammaitoni AR, Galer BS, Lacouture P, Domingos J, Schlagheck T. Effectiveness and safety of new oxycodone/acetaminophen formulations with reduced acetaminophen for the treatment of low back pain. Pain Med. 2003;4(1):21–30. doi: 10.1046/j.1526-4637.2003.03002.x. [DOI] [PubMed] [Google Scholar]
- 30.Mystakidou K, Parpa E, Tsilika E, et al. Long-term management of noncancer pain with transdermal therapeutic system-fentanyl. J Pain. 2003;4(6):298–306. doi: 10.1016/s1526-5900(03)00632-1. [DOI] [PubMed] [Google Scholar]
- 31.Allan L, Richarz U, Simpson K, Slappendel R. Transdermal fentanyl versus sustained release oral morphine in strong-opioid naïve patients with chronic low back pain. Spine (Phila Pa 1976) 2005;30(22):2484–2490. doi: 10.1097/01.brs.0000186860.23078.a8. [DOI] [PubMed] [Google Scholar]
- 32.Chao J. Retrospective analysis of Kadian (morphine sulfate sustained-release capsules) in patients with chronic, nonmalignant pain. Pain Med. 2005;6(3):262–265. doi: 10.1111/j.1526-4637.2005.05033.x. [DOI] [PubMed] [Google Scholar]
- 33.McIlwain H, Ahdieh H. Safety tolerability, and effectiveness of oxy-morphone extended release for moderate to severe osteoarthritis pain: a one-year study. Am J Ther. 2005;12(2):106–112. doi: 10.1097/01.mjt.0000139442.65914.f9. [DOI] [PubMed] [Google Scholar]
- 34.Nicholson B, Ross E, Sasaki J, Weil A. Randomized trial comparing polymer-coated extended-release morphine sulfate to controlled-release oxycodone HCl in moderate to severe nonmalignant pain. Curr Med Res Opin. 2006;22(8):1503–1514. doi: 10.1185/030079906X115603. [DOI] [PubMed] [Google Scholar]
- 35.Rauck RL, Bookbinder SA, Bunker TR, et al. The ACTION study: a randomized, open-label, multicenter trial comparing once-a-day extended-release morphine sulfate capsules (Avinza) to twice-a-day controlled-release oxycodone hydrochloride tablets (OxyContin) for the treatment of chronic, moderate to severe low back pain. J Opioid Manag. 2006;2(3):155–166. doi: 10.5055/jom.2006.0025. [DOI] [PubMed] [Google Scholar]
- 36.Portenoy RK, Farrar JT, Backonja MM, et al. Long-term use of controlled-release oxycodone for noncancer pain: results of a 3-year registry study. Clin J Pain. 2007;23(4):287–299. doi: 10.1097/AJP.0b013e31802b582f. [DOI] [PubMed] [Google Scholar]
- 37.Panjabi SS, Panjabi RS, Shepherd MD, Lawson KA, Johnsrud M, Barner J. Extended-release, once-daily morphine (Avinza) for the treatment of chronic nonmalignant pain: effect on pain, depressive symptoms, and cognition. Pain Med. 2008;9(8):985–993. doi: 10.1111/j.1526-4637.2008.00483.x. [DOI] [PubMed] [Google Scholar]
- 38.Gatti A, Reale C, Occhioni R, et al. Standard therapy with opioids in chronic pain management: ORTIBER study. Clin Drug Investig. 2009;29(Suppl 1):17–23. doi: 10.2165/0044011-200929001-00003. [DOI] [PubMed] [Google Scholar]
- 39.Kjaersgaard-Andersen P, Nafei A, Skov O, et al. Codeine plus paracetamol versus paracetamol in longer-term treatment of chronic pain due to osteoarthritis of the hip. A randomised, double-blind, multi-centre study. Pain. 1990;43(3):309–318. doi: 10.1016/0304-3959(90)90028-C. [DOI] [PubMed] [Google Scholar]
- 40.Quiding H, Grimstad J, Rusten K, Stubhaug A, Bremnes J, Breivik H. Ibuprofen plus codeine, ibuprofen, and placebo in a single- and multidose cross-over comparison for coxarthrosis pain. Pain. 1992;50(3):303–307. doi: 10.1016/0304-3959(92)90035-A. [DOI] [PubMed] [Google Scholar]
- 41.Moulin DE, Iezzi A, Amireh R, Sharpe WK, Boyd D, Merskey H. Randomised trial of oral morphine for chronic non-cancer pain. Lancet. 1996;347(8995):143–147. doi: 10.1016/s0140-6736(96)90339-6. [DOI] [PubMed] [Google Scholar]
- 42.Watson CP, Babul N. Efficacy of oxycodone in neuropathic pain: a randomized trial in postherpetic neuralgia. Neurology. 1998;50(6):1837–1841. doi: 10.1212/wnl.50.6.1837. [DOI] [PubMed] [Google Scholar]
- 43.Muller FO, Odendaal CL, Muller FR, Raubenheimer J, Middle MV, Kummer M. Comparison of the efficacy and tolerability of a paracetamol/codeine fixed-dose combination with tramadol in patients with refractory chronic back pain. Arzneimittelforschung. 1998;48(6):675–679. [PubMed] [Google Scholar]
- 44.Caldwell JR, Hale ME, Boyd RE, et al. Treatment of osteoarthritis pain with controlled release oxycodone or fixed combination oxycodone plus acetaminophen added to nonsteroidal antiinflammatory drugs: a double blind, randomized, multicenter, placebo controlled trial. J Rheumatol. 1999;26(4):862–869. [PubMed] [Google Scholar]
- 45.Peat S, Sweet P, Miah Y, Barklamb M, Larsen U. Assessment of analgesia in human chronic pain. Randomized double-blind crossover study of once daily repro-dose morphine versus MST continus. Eur J Clin Pharmacol. 1999;55(8):577–581. doi: 10.1007/s002280050675. [DOI] [PubMed] [Google Scholar]
- 46.Peloso PM, Bellamy N, Bensen W, et al. Double blind randomized placebo control trial of controlled release codeine in the treatment of osteoarthritis of the hip or knee. J Rheumatol. 2000;27(3):764–771. [PubMed] [Google Scholar]
- 47.Harke H, Gretenkort P, Ladleif HU, Rahman S, Harke O. The response of neuropathic pain and pain in complex regional pain syndrome 1 to carbamazepine and sustained-release morphine in patients pretreated with spinal cord stimulation: a double-blinded randomized study. Anesth Analg. 2001;92(2):488–495. doi: 10.1097/00000539-200102000-00039. [DOI] [PubMed] [Google Scholar]
- 48.Huse E, Larbig W, Flor H, Birbaumer N. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90(1–2):47–55. doi: 10.1016/s0304-3959(00)00385-7. [DOI] [PubMed] [Google Scholar]
- 49.Caldwell JR, Rapoport RJ, Davis JC, et al. Efficacy and safety of a once-daily morphine formulation in chronic, moderate-to severe osteoarthritis pain: results form a randomized, placebo-controlled, double-blind trial and an open-label extension trial. J Pain Symptom Manage. 2002;23(4):278–291. doi: 10.1016/s0885-3924(02)00383-4. [DOI] [PubMed] [Google Scholar]
- 50.Maier C, Hildebrandt J, Klinger R, Henrich-Eberl C, Lindena G, MONTAS Study Group Morphine responsiveness, efficacy and tolerability in patients with chronic non-tumor associated pain: results of a doubleblind placebo-controlled trial (MONTAS) Pain. 2002;97(3):223–233. doi: 10.1016/S0304-3959(02)00020-9. [DOI] [PubMed] [Google Scholar]
- 51.Raja SN, Haythornthwaite JA, Pappagallo M, et al. Opioids versus anti-depressants in postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology. 2002;59(7):1015–1021. doi: 10.1212/wnl.59.7.1015. [DOI] [PubMed] [Google Scholar]
- 52.Gimbel JS, Richards P, Portenoy RK. Controlled-release oxycodone for pain in diabetic neuropathy: a randomized controlled trial. Neurology. 2003;60(6):927–934. doi: 10.1212/01.wnl.0000057720.36503.2c. [DOI] [PubMed] [Google Scholar]
- 53.Rowbotham MC, Twilling L, Davies PS, Reisner L, Taylor K, Mohr D. Oral opioid therapy for chronic peripheral and central neuropathic pain. N Engl J Med. 2003;348(13):1223–1232. doi: 10.1056/NEJMoa021420. [DOI] [PubMed] [Google Scholar]
- 54.Watson CP, Moulin D, Watt-Watson J, Gordon A, Eisenhoffer J. Controlled-release oxycodone relieves neuropathic pain: a randomized controlled trial in painful diabetic neuropathy. Pain. 2003;105(1–2):71–78. doi: 10.1016/s0304-3959(03)00160-x. [DOI] [PubMed] [Google Scholar]
- 55.Chindalore VL, Craven RA, Yu KP, Butera PG, Burns LH, Friedmann N. Adding ultra low-dose naltrexone to oxycodone enhances and prolongs analgesia: a randomized, controlled trial of Oxytrex. J Pain. 2005;6(6):392–399. doi: 10.1016/j.jpain.2005.01.356. [DOI] [PubMed] [Google Scholar]
- 56.Hale ME, Dvergsten C, Gimbel J. Efficacy and safety of oxymorphone extended release in chronic low back pain: results of a randomized, double-blind, placebo- and active-controlled Phase III study. J Pain. 2005;6(1):21–28. doi: 10.1016/j.jpain.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 57.Gilron I, Bailey JM, Tu D, Holden RR, Weaver DF, Houlden RL. Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med. 2005;352(13):1324–1334. doi: 10.1056/NEJMoa042580. [DOI] [PubMed] [Google Scholar]
- 58.Markenson JA, Croft J, Zhang PG, Richards P. Treatment of persistent pain associated with osteoarthritis with controlled-release oxycodone tablets in a randomized controlled clinical trial. Clin J Pain. 2005;21(6):524–535. doi: 10.1097/01.ajp.0000146215.86038.38. [DOI] [PubMed] [Google Scholar]
- 59.Matsumoto AK, Babul N, Ahdieh H. Oxymorphone extended-release tablets relieve moderate to severe pain and improve physical function in osteoarthritis: results of a randomized, double-blind, placebo- and active-controlled Phase III trial. Pain Med. 2005;6(5):357–366. doi: 10.1111/j.1526-4637.2005.00057.x. [DOI] [PubMed] [Google Scholar]
- 60.Kivitz A, Ma C, Ahdieh H, Galer BS. A 2-week, multicenter, randomized, double-blind, placebo-controlled, dose-ranging, Phase III trial comparing the efficacy of oxymorphone extended release and placebo in adults with pain associated with osteoarthritis of the hip or knee. Clin Ther. 2006;28(3):352–364. doi: 10.1016/j.clinthera.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 61.Langford R, McKenna F, Ratcliffe S, Vojtassak J, Richarz U. Transdermal fentanyl for improvement of pain and functioning in osteoarthritis: a randomized, placebo-controlled trial. Arthritis Rheum. 2006;54(6):1829–1837. doi: 10.1002/art.21884. [DOI] [PubMed] [Google Scholar]
- 62.Hale ME, Ahdieh H, Ma T, Rauck R, Oxymorphone ER Study Group 1 Efficacy and safety of OPANA ER (oxymorphone extended release) for relief of moderate to severe chronic low back pain in opioid-experienced patients: a 12-week, randomized, double-blind, placebo-controlled study. J Pain. 2007;8(2):175–184. doi: 10.1016/j.jpain.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 63.Katz N, Sun S, Johnson F, Stauffer J. ALO-01 (morphine sulfate and naltrexone hydrochloride) extended-release capsules in the treatment of chronic pain of osteoarthritis of the hip or knee pharmacokinetics, efficacy, and safety. J Pain. 2010;11(4):303–311. doi: 10.1016/j.jpain.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 64.Grimes DA, Schulz KF. An overview of clinical research: the lay of the land. Lancet. 2002;359(9300):57–61. doi: 10.1016/S0140-6736(02)07283-5. [DOI] [PubMed] [Google Scholar]
- 65.Jamison RN, Raymond SA, Slawsby EA, Nedeljkovic SS, Katz NP. Opioid therapy for chronic noncancer back pain. A randomized prospective study. Spine (Phila Pa 1976) 1998;23(23):2591–2600. doi: 10.1097/00007632-199812010-00014. [DOI] [PubMed] [Google Scholar]
- 66.Olsen Y, Daumit GL. Chronic pain and narcotics: a dilemma for primary care. J Gen Intern Med. 2002;17(3):238–240. doi: 10.1046/j.1525-1497.2002.20109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Katz MH. Long-term opioid treatment of nonmalignant pain: a believer loses his faith. Arch Intern Med. 2010;170(16):1422–1424. doi: 10.1001/archinternmed.2010.335. [DOI] [PubMed] [Google Scholar]
- 68.Liebschutz JM, Alford DP. Safe opioid prescribing: a long way to go. J Gen Intern Med. 2011;26(9):951–952. doi: 10.1007/s11606-011-1797-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grady D, Berkowitz SA, Katz MH. Opioids for chronic pain. Arch Intern Med. 2011;171(16):1426–1427. doi: 10.1001/archinternmed.2011.213. [DOI] [PubMed] [Google Scholar]
- 70.Reisfield GM, Sloan PA. Physician identification of opioid diversion: a difficult diagnosis. J Opioid Manag. 2012;8(1):5–6. doi: 10.5055/jom.2012.0090. [DOI] [PubMed] [Google Scholar]
- 71.Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. doi: 10.1059/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 73.Bohmfalk GL. Management of chronic pain. JAMA. 1989;261(3):381. [PubMed] [Google Scholar]
- 74.Streltzer J, Johansen L. Prescription drug dependence and evolving beliefs about chronic pain management. Am J Psychiatry. 2006;163(4):594–598. doi: 10.1176/ajp.2006.163.4.594. [DOI] [PubMed] [Google Scholar]
- 75.Fishbain DA, Gallagher RM. Comments on “prescription drug dependence and evolving beliefs about chronic pain management.”. Am J Psychiatry. 2006;163(12):2194. doi: 10.1176/ajp.2006.163.12.2194a. [DOI] [PubMed] [Google Scholar]
- 76.Starrels JL, Becker WC, Alford DP, Kapoor A, Williams AR, Turner BJ. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152(11):712–720. doi: 10.7326/0003-4819-152-11-201006010-00004. [DOI] [PubMed] [Google Scholar]
- 77.Alexander GC, Kruszewski SP, Webster DW. Rethinking opioid prescribing to protect patient safety and public health. JAMA. 2012;308(18):1865–1866. doi: 10.1001/jama.2012.14282. [DOI] [PubMed] [Google Scholar]
- 78.Zgierska A, Miller M, Rabago D. Patient satisfaction, prescription drug abuse, and potential unintended consequences. JAMA. 2012;307(13):1377–1378. doi: 10.1001/jama.2012.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tennant FS., Jr (-)-alpha-Acetylmethadol for treatment of chronic pain patients who abuse opioids. Drug Alcohol Depend. 1983;12(3):243–247. doi: 10.1016/0376-8716(83)90066-2. [DOI] [PubMed] [Google Scholar]
- 80.Kennedy JA, Crowley TJ. Chronic pain and substance abuse: a pilot study of opioid maintenance. J Subst Abuse Treat. 1990;7(4):233–238. doi: 10.1016/0740-5472(90)90046-s. [DOI] [PubMed] [Google Scholar]
- 81.Goldman B. Use and abuse of opioid analgesics in chronic pain. Can Fam Physician. 1993;39:571–576. [PMC free article] [PubMed] [Google Scholar]
- 82.Sees KL, Clark HW. Opioid use in the treatment of chronic pain: assessment of addiction. J Pain Symptom Manage. 1993;8(5):257–264. doi: 10.1016/0885-3924(93)90154-n. [DOI] [PubMed] [Google Scholar]
- 83.DeSio JM, Bacon DR, Peer G, Lema MJ. Intravenous abuse of transdermal fentanyl therapy in a chronic pain patient. Anesthesiology. 1993;79(5):1139–1141. doi: 10.1097/00000542-199311000-00036. [DOI] [PubMed] [Google Scholar]
- 84.Hoffmann NG, Olofsson O, Salen B, Wickstrom L. Prevalence of abuse and dependency in chronic pain patients. Int J Addict. 1995;30(8):919–927. doi: 10.3109/10826089509055820. [DOI] [PubMed] [Google Scholar]
- 85.Miotto K, Compton P, Ling W, Conolly M. Diagnosing addictive disease in chronic pain patients. Psychosomatics. 1996;37(3):223–235. doi: 10.1016/S0033-3182(96)71561-X. [DOI] [PubMed] [Google Scholar]
- 86.Dunbar SA, Katz NP. Chronic opioid therapy for nonmalignant pain in patients with a history of substance abuse: report of 20 cases. J Pain Symptom Manage. 1996;11(3):163–171. doi: 10.1016/0885-3924(95)00165-4. [DOI] [PubMed] [Google Scholar]
- 87.Chabal C, Erjavec MK, Jacobson L, Mariano A, Chaney E. Prescription opiate abuse in chronic pain patients: clinical criteria, incidence, and predictors. Clin J Pain. 1997;13(2):150–155. doi: 10.1097/00002508-199706000-00009. [DOI] [PubMed] [Google Scholar]
- 88.Kouyanou K, Pither CE, Wessely S. Medication misuse, abuse and dependence in chronic pain patients. J Psychosom Res. 1997;43(5):497–504. doi: 10.1016/s0022-3999(97)00171-2. [DOI] [PubMed] [Google Scholar]
- 89.Compton P, Darakjian J, Miotto K. Screening for addiction in patients with chronic pain and “problematic” substance use: evaluation of a pilot assessment tool. J Pain Symptom Manage. 1998;16(6):355–363. doi: 10.1016/s0885-3924(98)00110-9. [DOI] [PubMed] [Google Scholar]
- 90.Compton P, Estepa CA. Addiction in patients with chronic pain. Lippincotts Prim Care Pract. 2000;4(3):254–272. [PubMed] [Google Scholar]
- 91.Nedeljkovic SS, Wasan A, Jamison RN. Assessment of efficacy of long-term opioid therapy in pain patients with substance abuse potential. Clin J Pain. 2002;18(Suppl 4):S39–S51. doi: 10.1097/00002508-200207001-00005. [DOI] [PubMed] [Google Scholar]
- 92.Cohen MJ, Jasser S, Herron PD, Margolis CG. Ethical perspectives: opioid treatment of chronic pain in the context of addiction. Clin J Pain. 2002;18(Suppl 4):S99–S107. doi: 10.1097/00002508-200207001-00012. [DOI] [PubMed] [Google Scholar]
- 93.Weaver MF, Schnoll SH. Opioid treatment of chronic pain in patients with addiction. J Pain Palliat Care Pharmacother. 2002;16(3):5–26. doi: 10.1080/j354v16n03_02. [DOI] [PubMed] [Google Scholar]
- 94.Compton P, Athanasos P. Chronic pain, substance abuse and addiction. Nurs Clin North Am. 2003;38(3):525–537. doi: 10.1016/s0029-6465(02)00100-7. [DOI] [PubMed] [Google Scholar]
- 95.Heit HA. Addiction, physical dependence, and tolerance: precise definitions to help clinicians evaluate and treat chronic pain patients. J Pain Palliat Care Pharmacother. 2003;17(1):15–29. doi: 10.1080/j354v17n01_03. [DOI] [PubMed] [Google Scholar]
- 96.Adams LL, Gatchel RJ, Robinson RC, et al. Development of a self-report screening instrument for assessing potential opioid medication misuse in chronic pain patients. J Pain Symptom Manage. 2004;27(5):440–459. doi: 10.1016/j.jpainsymman.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 97.Michna E, Ross EL, Hynes WL, et al. Predicting aberrant drug behavior in patients treated for chronic pain: importance of abuse history. J Pain Symptom Manage. 2004;28(3):250–258. doi: 10.1016/j.jpainsymman.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 98.Schieffer BM, Pham Q, Labus J, et al. Pain medication beliefs and medication misuse in chronic pain. J Pain. 2005;6(9):620–629. doi: 10.1016/j.jpain.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 99.Rosenblum A, Joseph H, Fong C, Kipnis S, Cleland C, Portenoy RK. Prevalence and characteristics of chronic pain among chemically dependent patients in methadone maintenance and residential treatment facilities. JAMA. 2003;289:2370–2378. doi: 10.1001/jama.289.18.2370. [DOI] [PubMed] [Google Scholar]
- 100.Manchikanti L, Manchukonda R, Damron KS, Brandon D, McManus CD, Cash K. Does adherence monitoring reduce controlled substance abuse in chronic pain patients? Pain Physician. 2006;9(1):57–60. [PubMed] [Google Scholar]
- 101.Adams EH, Breiner S, Cicero TJ, et al. A comparison of the abuse liability of tramadol, NSAIDs, and hydrocodone in patients with chronic pain. J Pain Symptom Manage. 2006;31(5):465–476. doi: 10.1016/j.jpainsymman.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 102.Manchikanti L, Cash KA, Damron KS, Manchukonda R, Pampati V, McManus CD. Controlled substance abuse and illicit drug use in chronic pain patients: an evaluation of multiple variables. Pain Physician. 2006;9(3):215–225. [PubMed] [Google Scholar]
- 103.Wu SM, Compton P, Bolus R, et al. The addiction behaviors checklist: validation of a new clinician-based measure of inappropriate opioid use in chronic pain. J Pain Symptom Manage. 2006;32(4):342–351. doi: 10.1016/j.jpainsymman.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 104.Fleming MF, Balousek SL, Klessig CL, Mundt MP, Brown DD. Substance use disorders in a primary care sample receiving daily opioid therapy. J Pain. 2007;8(7):573–582. doi: 10.1016/j.jpain.2007.02.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kahan M, Srivastava A, Wilson L, Gourlay D, Midmer D. Misuse of and dependence on opioids: study of chronic pain patients. Can Fam Physician. 2006;52(9):1081–1087. [PMC free article] [PubMed] [Google Scholar]
- 106.Saffer K, Colombo C, Brown D, Mundt MP, Fleming MF. Addiction Severity Index in a chronic pain sample receiving opioid therapy. J Subst Abuse Treat. 2007;33(3):303–311. doi: 10.1016/j.jsat.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Modesto-Lowe V, Brooks D, Freedman K, Hargus E. Addiction and chronic pain: diagnostic and treatment dilemmas. Conn Med. 2007;71(3):139–144. [PubMed] [Google Scholar]
- 108.Hojsted J, Sjogren P. Addiction to opioids in chronic pain patients: a literature review. Eur J Pain. 2007;11(5):490–518. doi: 10.1016/j.ejpain.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 109.Ballantyne JC, LaForge KS. Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 2007;129(3):235–255. doi: 10.1016/j.pain.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 110.Manchikanti L, Giordano J, Boswell MV, Fellows B, Manchukonda R, Pampati V. Psychological factors as predictors of opioid abuse and illicit drug use in chronic pain patients. J Opioid Manag. 2007;3(2):89–100. doi: 10.5055/jom.2007.0045. [DOI] [PubMed] [Google Scholar]
- 111.Balousek S, Plane MB, Fleming M. Prevalence of interpersonal abuse in primary care patients prescribed opioids for chronic pain. J Gen Intern Med. 2007;22(9):1268–1273. doi: 10.1007/s11606-007-0257-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jamison RN, Ross EL, Wasan AD, Michna E. Comment on Ballantyne and LaForge. Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 2007;132(1–2):218–219. doi: 10.1016/j.pain.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 113.Wiedemer NL, Harden PS, Arndt IO, Gallagher RM. The opioid renewal clinic: a primary care, managed approach to opioid therapy in chronic pain patients at risk for substance abuse. Pain Med. 2007;8(7):573–584. doi: 10.1111/j.1526-4637.2006.00254.x. [DOI] [PubMed] [Google Scholar]
- 114.Tulchinsky A. Comment on Ballantyne JC, LaForge KS. Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 2007;132(1–2):222–223. doi: 10.1016/j.pain.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 115.Wilsey BL, Fishman SM, Tsodikov A, Ogden C, Symreng I, Ernst A. Psychological comorbidities predicting prescription opioid abuse among patients in chronic pain presenting to the emergency department. Pain Med. 2008;9(8):1107–1117. doi: 10.1111/j.1526-4637.2007.00401.x. [DOI] [PubMed] [Google Scholar]
- 116.Morasco BJ, Dobscha SK. Prescription medication misuse and substance use disorder in VA primary care patients with chronic pain. Gen Hosp Psychiatry. 2008;30(2):93–99. doi: 10.1016/j.genhosppsych.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 117.Mitchell AM, Dewey CM. Chronic pain in patients with substance abuse disorder: general guidelines and an approach to treatment. Postgrad Med. 2008;120(1):75–79. doi: 10.3810/pgm.2008.04.1763. [DOI] [PubMed] [Google Scholar]
- 118.Turk DC, Swanson KS, Gatchel RJ. Predicting opioid misuse by chronic pain patients: a systematic review and literature synthesis. Clin J Pain. 2008;24(6):497–508. doi: 10.1097/AJP.0b013e31816b1070. [DOI] [PubMed] [Google Scholar]
- 119.Clark MR, Stoller KB, Brooner RK. Assessment and management of chronic pain in individuals seeking treatment for opioid dependence disorder. Can J Psychiatry. 2008;53(8):496–508. doi: 10.1177/070674370805300804. [DOI] [PubMed] [Google Scholar]
- 120.Martin TJ, Ewan E. Chronic pain alters drug self-administration: implications for addiction and pain mechanisms. Exp Clin Psychopharmacol. 2008;16(5):357–366. doi: 10.1037/a0013597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Denisco RA, Chandler RK, Compton WM. Addressing the intersecting problems of opioid misuse and chronic pain treatment. Exp Clin Psychopharmacol. 2008;16(5):417–428. doi: 10.1037/a0013636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Becker WC, Fiellin DA, Gallagher RM, Barth KS, Ross JT, Oslin DW. The association between chronic pain and prescription drug abuse in veterans. Pain Med. 2009;10(3):531–536. doi: 10.1111/j.1526-4637.2009.00584.x. [DOI] [PubMed] [Google Scholar]
- 123.Alford DP. Opioids for chronic pain in patients with substance abuse: too much, too little or just right? Pain. 2009;145(3):267–268. doi: 10.1016/j.pain.2009.06.036. [DOI] [PubMed] [Google Scholar]
- 124.Wilsey BL, Fishman S, Li CS, Storment J, Albanese A. Markers of abuse liability of short- vs long-acting opioids in chronic pain patients: a randomized cross-over trial. Pharmacol Biochem Behav. 2009;94(1):98–107. doi: 10.1016/j.pbb.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Savage SR. Management of opioid medications in patients with chronic pain and risk of substance misuse. Curr Psychiatry Rep. 2009;11(5):377–384. doi: 10.1007/s11920-009-0057-2. [DOI] [PubMed] [Google Scholar]
- 126.Jamison RN, Ross EL, Michna E, Chen LQ, Holcomb C, Wasan AD. Substance misuse treatment for high-risk chronic pain patients on opioid therapy: a randomized trial. Pain. 2010;150(3):390–400. doi: 10.1016/j.pain.2010.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Edlund MJ, Martin BC, Fan MY, Devries A, Braden JB, Sullivan MD. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP study. Drug Alcohol Depend. 2010;112(1–2):90–98. doi: 10.1016/j.drugalcdep.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Fishbain D, Johnson S, Webster L, Greene L, Faysal J. Review of regulatory programs and new opioid technologies in chronic pain management: balancing the risk of medication abuse with medical need. J Manag Care Pharm. 2010;16(4):276–287. doi: 10.18553/jmcp.2010.16.4.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hojsted J, Nielsen PR, Guldstrand SK, Frich L, Sjogren P. Classification and identification of opioid addiction in chronic pain patients. Eur J Pain. 2010;14(10):1014–1020. doi: 10.1016/j.ejpain.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 130.Manchikanti L, Singh A. Therapeutic opioids: a ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician. 2008;11(2 Suppl):S63–S88. [PubMed] [Google Scholar]
- 131.Barry DT, Irwin KS, Jones ES, et al. Opioids, chronic pain, and addiction in primary care. J Pain. 2010;11(12):1442–1450. doi: 10.1016/j.jpain.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Park J, Lavin R. Risk factors associated with opioid medication misuse in community-dwelling older adults with chronic pain. Clin J Pain. 2010;26(8):647–655. doi: 10.1097/AJP.0b013e3181e94240. [DOI] [PubMed] [Google Scholar]
- 133.Butler SF, Budman SH, Fanciullo GJ, Jamison RN. Cross validation of the current opioid misuse measure to monitor chronic pain patients on opioid therapy. Clin J Pain. 2010;26(9):770–776. doi: 10.1097/AJP.0b013e3181f195ba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Brushwood DB, Rich BA, Coleman JJ, Bolen J, Wong W. Legal liability perspectives on abuse-deterrent opioids in the treatment of chronic pain. J Pain Palliat Care Pharmacother. 2010;24(4):333–348. doi: 10.3109/15360288.2010.524979. [DOI] [PubMed] [Google Scholar]
- 135.Serban S. Drug abuse in the chronic pain patient. Int Anesthesiol Clin. 2011;49(1):135–145. doi: 10.1097/AIA.0b013e31820aae93. [DOI] [PubMed] [Google Scholar]
- 136.Schneider JP, Kirsh KL. Defining clinical issues around tolerance, hyperalgesia, and addiction: a quantitative and qualitative outcome study of long-term opioid dosing in a chronic pain practice. J Opioid Manag. 2010;6(6):385–395. doi: 10.5055/jom.2010.0036. [DOI] [PubMed] [Google Scholar]
- 137.Manubay JM, Muchow C, Sullivan MA. Prescription drug abuse: epidemiology, regulatory issues, chronic pain management with narcotic analgesics. Prim Care. 2011;38(1):71–90. doi: 10.1016/j.pop.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Edwards RR, Wasan AD, Michna E, Greenbaum S, Ross E, Jamison RN. Elevated pain sensitivity in chronic pain patients at risk for opioid misuse. J Pain. 2011;12(9):953–963. doi: 10.1016/j.jpain.2011.02.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Webster L, St Marie B, McCarberg B, Passik SD, Panchal SJ, Voth E. Current status and evolving role of abuse-deterrent opioids in managing patients with chronic pain. J Opioid Manag. 2011;7(3):235–245. doi: 10.5055/jom.2011.0066. [DOI] [PubMed] [Google Scholar]
- 140.McCarberg BH. Chronic pain: reducing costs through early implementation of adherence testing and recognition of opioid misuse. Postgrad Med. 2011;123(6):132–139. doi: 10.3810/pgm.2011.11.2503. [DOI] [PubMed] [Google Scholar]
- 141.Heimer R, Dasgupta N, Irwin KS, et al. Chronic pain, addiction severity, and misuse of opioids in Cumberland County, Maine. Addict Behav. 2012;37(3):346–349. doi: 10.1016/j.addbeh.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 142.Keller CE, Ashrafioun L, Neumann AM, Van Klein J, Fox CH, Blondell RD. Practices, perceptions, and concerns of primary care physicians about opioid dependence associated with the treatment of chronic pain. Subst Abus. 2012;33(2):103–113. doi: 10.1080/08897077.2011.630944. [DOI] [PubMed] [Google Scholar]
- 143.Sehgal N, Manchikanti L, Smith HS. Prescription opioid abuse in chronic pain: a review of opioid abuse predictors and strategies to curb opioid abuse. Pain Physician. 2012;15(Suppl 3):ES67–ES92. [PubMed] [Google Scholar]
- 144.Pohl M, Smith L. Chronic pain and addiction: challenging co-occurring disorders. J Psychoactive Drugs. 2012;44(2):119–124. doi: 10.1080/02791072.2012.684621. [DOI] [PubMed] [Google Scholar]
- 145.Andrews CM, Krantz MJ, Wedam EF, Marcuson MJ, Capacchione JF, Haigney MC. Methadone-induced mortality in the treatment of chronic pain: role of QT prolongation. Cardiol J. 2009;16(3):210–217. [PubMed] [Google Scholar]
- 146.Krebs EE, Becker WC, Zerzan J, Bair MJ, McCoy K, Hui S. Comparative mortality among Department of Veterans Affairs patients prescribed methadone or long-acting morphine for chronic pain. Pain. 2011;152(8):1789–1795. doi: 10.1016/j.pain.2011.03.023. [DOI] [PubMed] [Google Scholar]
- 147.Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171(7):686–691. doi: 10.1001/archinternmed.2011.117. [DOI] [PubMed] [Google Scholar]
- 148.Sullivan MD. Limiting the potential harms of high-dose opioid therapy: comment on “opioid dose and drug-related mortality in patients with nonmalignant pain.”. Arch Intern Med. 2011;171(7):691–693. doi: 10.1001/archinternmed.2011.101. [DOI] [PubMed] [Google Scholar]
- 149.Substance Abuse and Mental Health Services Administration . Results From the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2009. [Google Scholar]
- 150.Kissin I, Gelman S. Chronic postsurgical pain: still a neglected topic? J Pain Res. 2012;5:473–489. doi: 10.2147/JPR.S35145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wasan AD, Correll DJ, Kissin I, O’Shea S, Jamison RN. Iatrogenic addiction in patients treated for acute or subacute pain: a systematic review. J Opioid Manag. 2006;2(1):16–22. doi: 10.5055/jom.2006.0003. [DOI] [PubMed] [Google Scholar]
- 152.Jamison RN, Serraillier J, Michna E. Assessment and treatment of abuse risk in opioid prescribing for chronic pain. Pain Res Treat. 2011;2011:941808. doi: 10.1155/2011/941808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Dellemijn PL. Opioids in non-cancer pain: a life-time sentence? Eur J Pain. 2001;5(3):333–339. doi: 10.1053/eujp.2001.0240. [DOI] [PubMed] [Google Scholar]
- 154.Kolb L. Clinical contribution to drug addiction: the struggle for cure and the conscious reasons for relapse. J Nerv Ment Dis. 1927;66:22–43. [PMC free article] [PubMed] [Google Scholar]
- 155.Martin WR, Jasinski DR. Physiological parameters of morphine in man – tolerance, early abstinence, protracted abstinence. J Psychiatr Res. 1969;7(1):9–17. doi: 10.1016/0022-3956(69)90007-7. [DOI] [PubMed] [Google Scholar]
- 156.Satel SL, Kosten TR, Schuckit MA, Fischman MW. Should protracted withdrawal from drugs be included in DSM-IV? Am J Psychiatry. 1993;150(5):695–704. doi: 10.1176/ajp.150.5.695. [DOI] [PubMed] [Google Scholar]
- 157.Le Merrer J, Befort K, Gardon O, et al. Protracted abstinence from distinct drugs of abuse shows regulation of a common gene network. Addict Biol. 2012;17(1):1–12. doi: 10.1111/j.1369-1600.2011.00365.x. [DOI] [PubMed] [Google Scholar]
- 158.Merskey H, Bogduk N, International Association for the Study of Pain . Classification of Chronic Pain. 2nd ed. Seattle, WA: IASP Press; 1994. [Google Scholar]