Abstract
Purpose
Thanks to advancements in surgical techniques and instruments, many surgical modalities have been developed to replace transurethral resection of the prostate (TURP). However, TURP remains the gold standard for the surgical treatment of benign prostatic hyperplasia (BPH). We conducted a meta-analysis on the efficacy and safety of minimally invasive surgical therapies for BPH compared with TURP.
Methods
This meta-analysis used a Medline search assessing the period from 1997 to 2011. A total of 784 randomized controlled trials were identified in an electronic search. Among the 784 articles, 36 randomized controlled trials that provided the highest level of evidence (level 1b) were included in the meta-analysis. We also conducted a quality analysis of selected articles.
Results
Only 2 articles (5.56%) were assessed as having a low risk of bias by use of the Cochrane collaboration risk of bias tool. On the other hand, by use of the Jadad scale, there were 26 high-quality articles (72.22%). Furthermore, 28 articles (77.78%) were assessed as high-quality articles by use of the van Tulder scale. Holmium laser enucleation of the prostate (HoLEP) showed the highest reduction of the International Prostate Symptom Score compared with TURP (P<0.0001). Bipolar TURP, bipolar transurethral vaporization of the prostate, HoLEP, and open prostatectomy showed superior outcome in postvoid residual urine volume and maximum flow rate. The intraoperative complications of the minimally invasive surgeries had no statistically significant inferior outcomes compared with TURP. Also, there were no statistically significant differences in any of the modalities compared with TURP.
Conclusions
The selection of an appropriate surgical modality for BPH should be assessed by fully understanding each patient's clinical conditions.
Keywords: Prostatic hyperplasia, Holmium, Lasers, Potassium titanylphosphate, Transurethral resection of prostate, Meta-analysis
INTRODUCTION
Benign prostatic hyperplasia (BPH), which causes lower urinary tract symptoms (LUTS), is one of the most common diseases of aging men [1]. LUTS can reduce quality of life by impeding normal activities and causing complications such as acute urinary retention or urinary tract infection. BPH is histologically observed in about half of men in their 60s and in most men aged 80 and older [2]. Nowadays, various medications are used to treat LUTS resulting from BPH (LUTS/BPH); these include 5-alpha-reductase inhibitors (5-ARIs), alpha-adrenergic blockers, and others. Moreover, many surgical treatment methods have been introduced, such as resection or enucleation.
Currently, the gold standard surgical treatment for LUTS/BPH is transurethral resection of the prostate (TURP) [3,4]. However, TURP is associated with complications including bleeding, pain, infection, urethral stricture, bladder neck contraction, erectile dysfunction, incontinence, and retrograde ejaculation [5]. Therefore, many endoscopic surgical methods have been suggested to replace TURP as the new standard [6]. There has been a continuous rise in the use of minimally invasive surgical therapies for LUTS/BPH, including bipolar TURP, bipolar transurethral vaporization of the prostate (TUVP), holmium laser enucleation of the prostate (HoLEP), and potassium-titanyl-phosphate (KTP) laser vaporization of the prostate. So far, numerous articles have reported on comparisons of these new techniques with TURP. Ahyai et al. [6] reported a meta-analysis on functional outcomes and complications of transurethral prostatectomy for LUTS/BPH. According to those authors, many minimally invasive surgical therapies for LUTS/BPH showed statistically comparable efficacy and overall morbidity to TURP. However, that report included randomized controlled trials published from 1997 to 2009.
Therefore, we conducted a meta-analysis on the efficacy and safety of minimally invasive surgical therapies for LUTS/BPH compared with TURP by analyzing more recent articles that were published from 2010 to 2011. In addition, we assessed the quality of these articles by using the Jadad scale, the van Tulder scale (VTS), and Cochrane collaboration risk of bias tool (CCRBT).
MATERIALS AND METHODS
Searching Strategy
This meta-analysis used a Medline search assessing the period from 1997 to 2011. We searched published articles by using MeSH phrases such as "benign prostatic hyperplasia," "enlargement," and "obstruction"; "minimally invasive surgical therapy"; "randomized controlled trial [Publication Type]"; and the specific TURP name. There were no limitations on languages.
Study Selection
A total of 784 randomized controlled trials were identified in an electronic search. Among the 784 articles, 36 randomized controlled trials that provided the highest level of evidence (level 1b) were included in the meta-analysis. Studies that were not randomized or that had no comparator were excluded.
Data Extraction
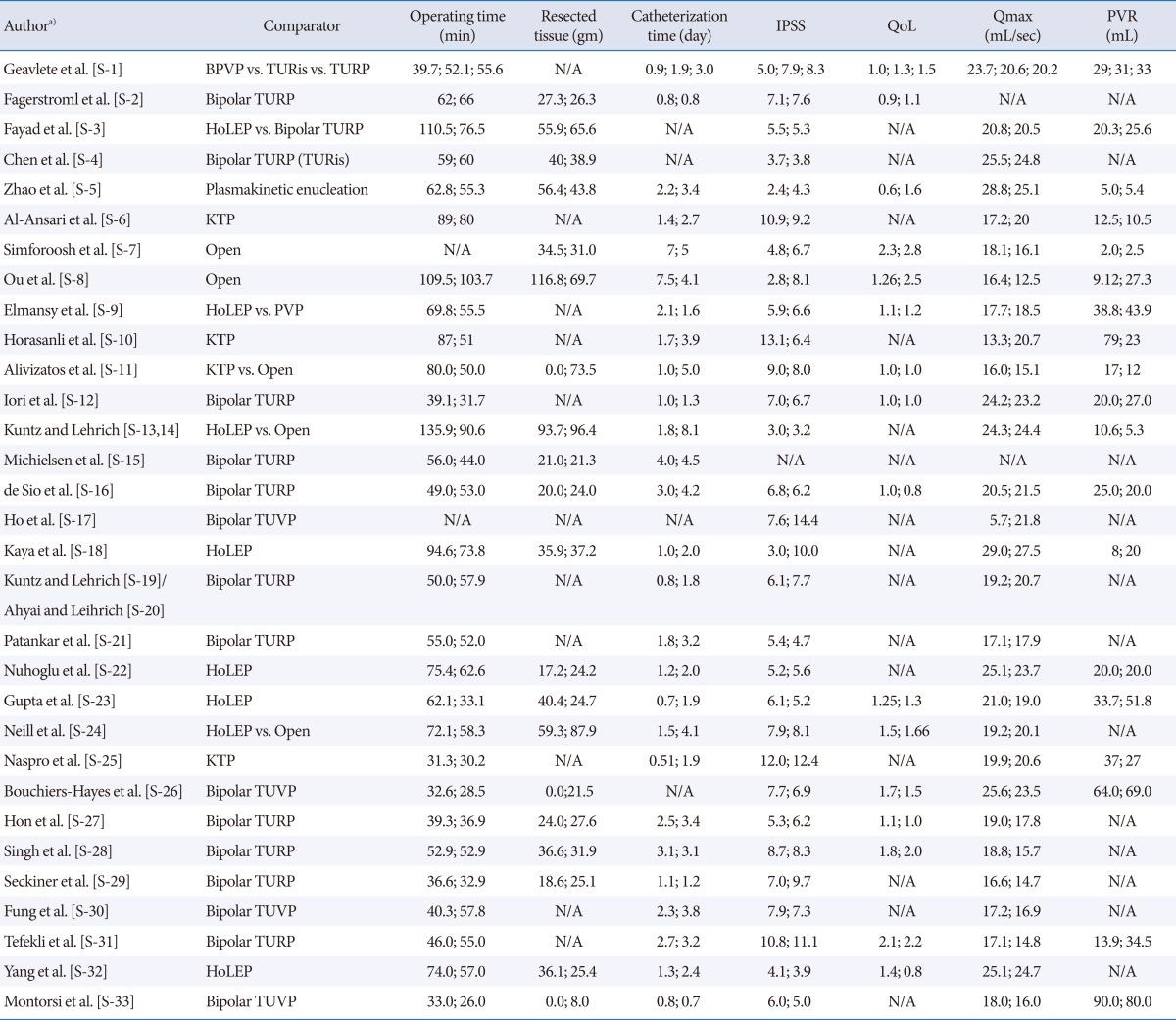
We collected the following data: comparator; name of first author; year of publication; number of patients in each group; follow-up period; baseline data, including age, prostate volume (cm3), International Prostate Symptom Score (IPSS), quality of life (QoL) score, postvoiding residual urine volume (PVR; mL), and maximum flow rate (Qmax; mL/sec) before the procedure (Table 1); perioperative outcomes, including operative time (min), weight of resected tissue (g), and length of catheter use (day); functional outcomes, including IPSS and Qmax after the surgery; and complications (Table 2).
Table 1.
Summary of (mean) baseline characteristics from included randomised trials comparing minimally invasive therapies with transurethral resection of the prostate
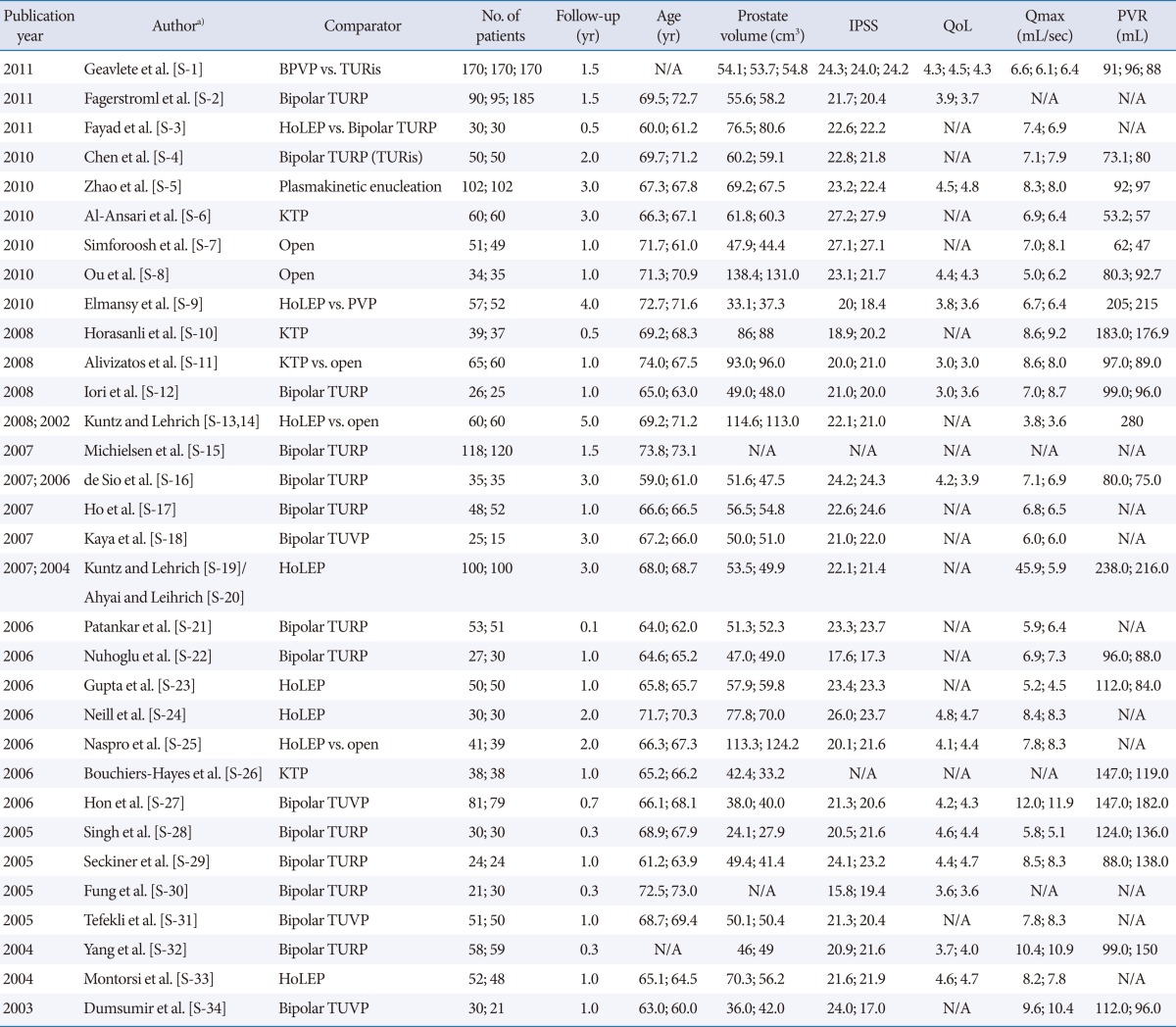
IPSS, International Prostate Symptom Score; QoL, quality of life; Qmax, maximum flow rate; PVR, postvoid residual urine volume; BPVP, bipolar plasma vaporization of the prostate; TURis, transurethral resection of prostate in saline; N/A, not available; TURP, transurethral resection of prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate; PVP, plasma vaporization of the prostate; TUVP, transurethral vaporisation of the prostate.
a)Supplementary material for authors can be found via http://www.einj.org/src/sm/inj-17-59-s001.pdf.
Table 2.
Summary of (mean) outcome data from included randomised studies comparing minimally invasive surgical therapies with transurethral resection of the prostate
IPSS, International Prostate Symptom Score; QoL, quality of life; Qmax, maximum flow rate; PVR, postvoid residual urine volume; BPVP, bipolar plasma vaporization of the prostate; TURis, transurethral resection of prostate in saline; TURP, transurethral resection of prostate; N/A, not available; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate; PVP, plasma vaporization of the prostate; TUVP, transurethral vaporisation of the prostate.
a)Supplementary material for authors can be found via http://www.einj.org/src/sm/inj-17-59-s001.pdf.
Quality Analysis
We assessed the quality of the selected articles by using the Jadad scale, VTS, and CCRBT [7]. All quality assessments of articles were performed by two reviewers. If there were different outcomes, the two reviewers and a third reviewer resolved the discrepancy in the results through discussion.
Statistical Analysis
The primary endpoint of the present analysis was functional outcomes, including IPSS/QoL and Qmax/PVR; perioperative results, including operative time (min) and length of catheter use (day); and incidence rate of complications, including bleeding, blood transfusion, conversion to TURP, capsule perforation, transurethral resection syndrome, acute urinary retention, clot retention, secondary apical resection, secondary coagulation revision, secondary bleeding, infection, urethral stricture, bladder neck stenosis, urgency, stress urinary incontinence, and reoperation/intervention requirement. Pooled odds ratios and 95% confidence intervals were calculated for the dichotomous and continuous outcome data between the various operative methods and TURP, respectively. The Q-statistic was used to analyze heterogeneity [8]. If I2 >50%, we considered it as heterogeneous and a random effect model was performed. IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA) and SAS ver. 9.1.3 (SAS Institute, Cary, NC, USA) were used for the statistical analysis. All tests were two-sided, with a significance level of 0.05.
RESULTS
Quality Analysis of Selected Articles
Among the 36 articles, only 2 articles (5.56%) were assessed as having a low risk of bias, 7 articles (19.44%) were assessed as having a moderate risk of bias, and 27 articles (0.75%) were evaluated as having a high risk of bias by use of the CCRBT. On the other hand, by use of the Jadad scale, there were 26 high-quality articles (72.22%). Furthermore, 28 articles (77.78%) were assessed as high-quality articles by use of the VTS.
Meta-Analysis of Functional Outcomes
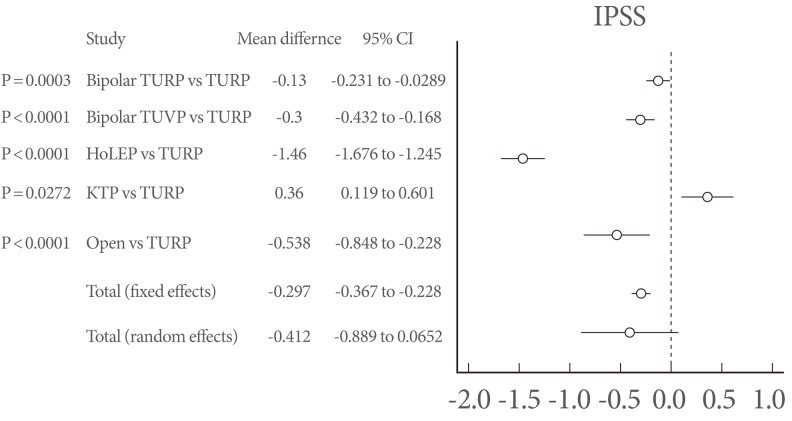
IPSS (Fig. 1) and QoL (Fig. 2)
Fig. 1.
Forest plot of International Prostate Symptom Score (IPSS). CI, confidence interval; TURP, transurethral resection of the prostate; IPSS, International Prostate Symptom Score; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
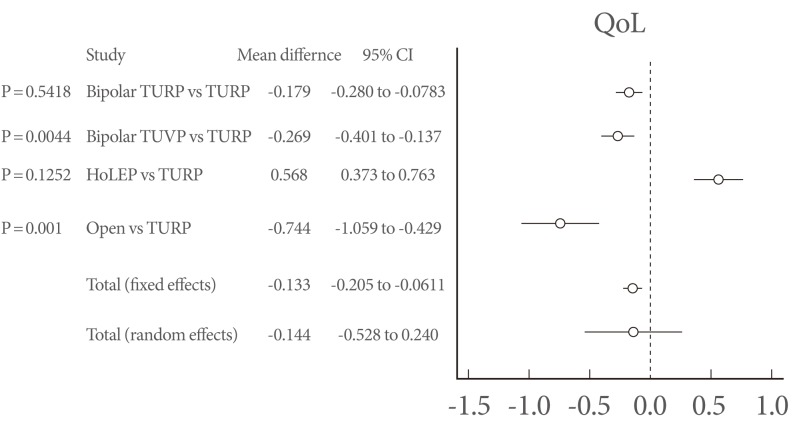
Fig. 2.
Forest plot of quality of life (QoL, question 8 of the IPSS). CI, confidence interval; TURP, transurethral resection of the prostate; IPSS, International Prostate Symptom Score; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
Only KTP laser vaporization of the prostate showed an inferior outcome compared with TURP (P=0.0272). Otherwise, HoLEP showed the highest reduction of the IPSS compared with TURP (P<0.0001). Moreover, only HoLEP showed a higher QoL, although it was not statistically significant (P=0.1252).
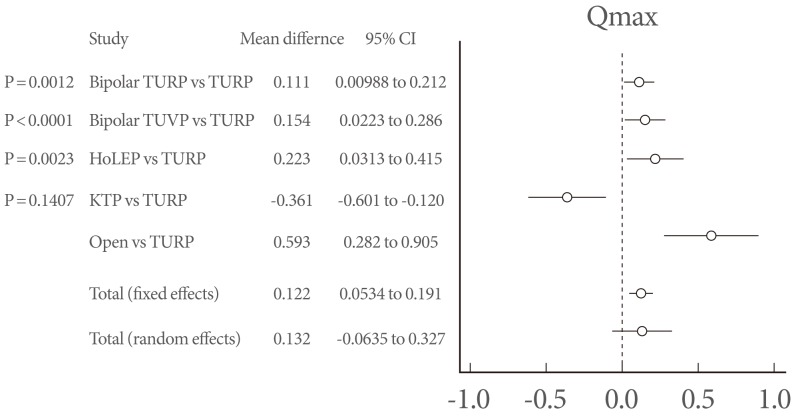
Maximum flow rate (Fig. 3) and postvoid residual urine volume (Fig. 4)
Fig. 3.
Forest plot of maximum flow rate (Qmax). CI, confidence interval; TURP, transurethral resection of the prostate; IPSS, International Prostate Symptom Score; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
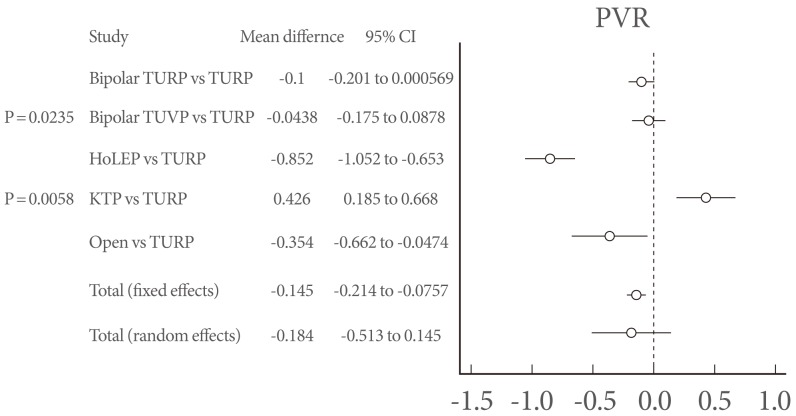
Fig. 4.
Forest plot of postvoid residual urine volume (PVR). CI, confidence interval; TURP, transurethral resection of the prostate; IPSS, International Prostate Symptom Score; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
Only KTP showed an inferior outcome in Qmax and PVR (P=0.1407, P=0.0058). However, bipolar TURP, bipolar TUVP, HoLEP, and open prostatectomy showed a superior outcome in Qmax and PVR. Open prostatectomy and HoLEP could not be statistically analyzed for PVR owing to insufficient data.
Meta-Analysis of Complications Of Surgery
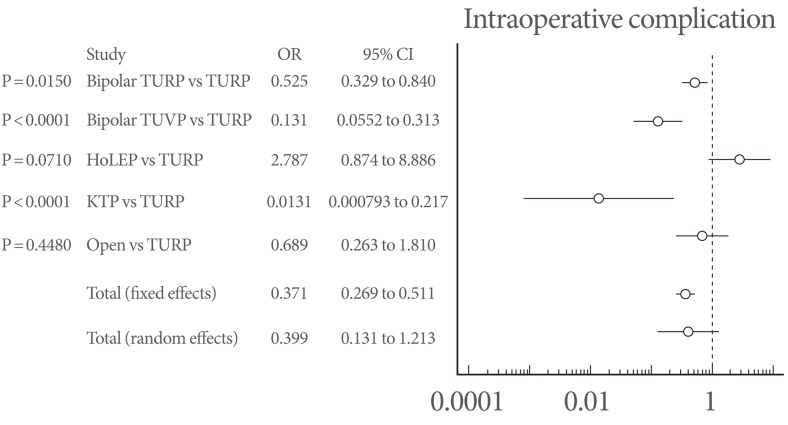
Intraoperative complications (Fig. 5)
Fig. 5.
Forest plot of intraoperative complications. TURP, transurethral resection of the prostate; OR, odds ratio; CI, confidence interval; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
No surgical methods showed statistically significant inferior outcomes compared with TURP. However, HoLEP showed the highest complication rate (P=0.0710) and KTP showed a statistically significantly lower complication rate than TURP (P<0.0001). HoLEP showed the highest incidence of bladder mucosal injury, and TURP showed the highest incidence of intraoperative transfusion (Table 3).
Table 3.
Intraoperative complications
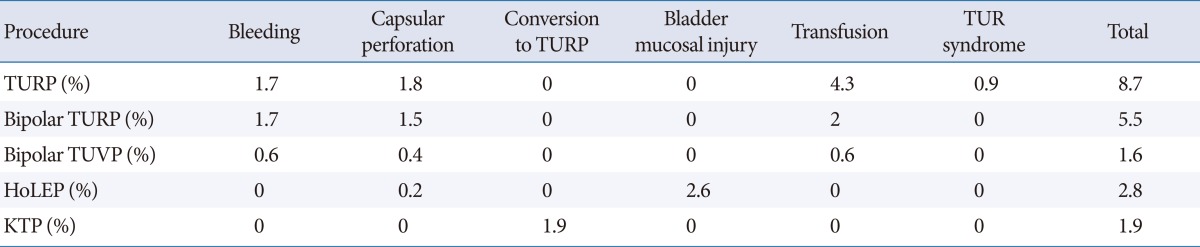
TURP, transurethral resection of prostate; TUVP, transurethral vaporisation of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
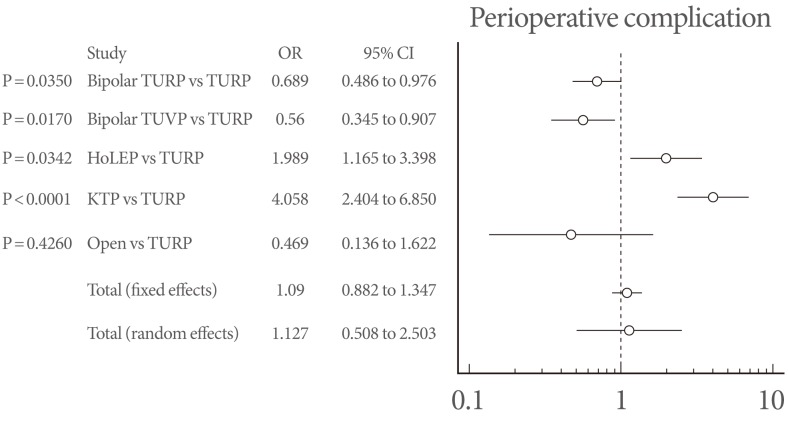
Perioperative complications (Fig. 6)
Fig. 6.
Forest plot of perioperative complications. OR, odds ratio; CI, confidence interval; TURP, transurethral resection of the prostate; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
KTP and HoLEP showed statistically significantly inferior outcomes compared with TURP (P<0.0001, P=0.0342, respectively). Acute urinary retention, secondary apical resection, and febrile urinary tract infection occurred most commonly with KTP. TURP showed the highest occurrence rate of clot retention and hematuria episodes (Table 4).
Table 4.
Perioperative complication
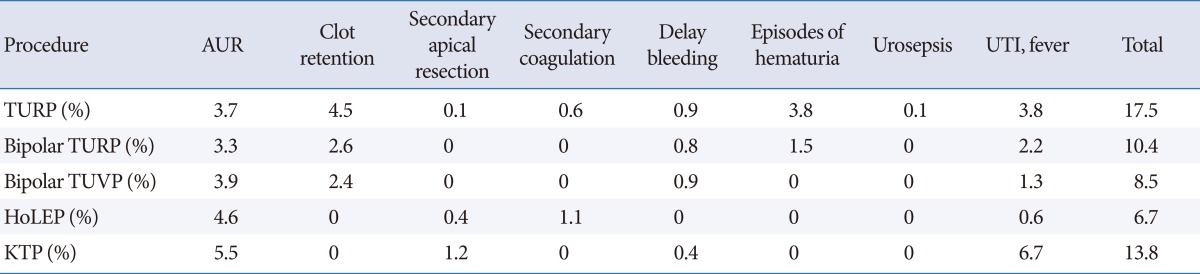
AUR, acute urinary retention; UTI, urinary tract infection; TURP, transurethral resection of prostate; TUVP, transurethral vaporisation of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
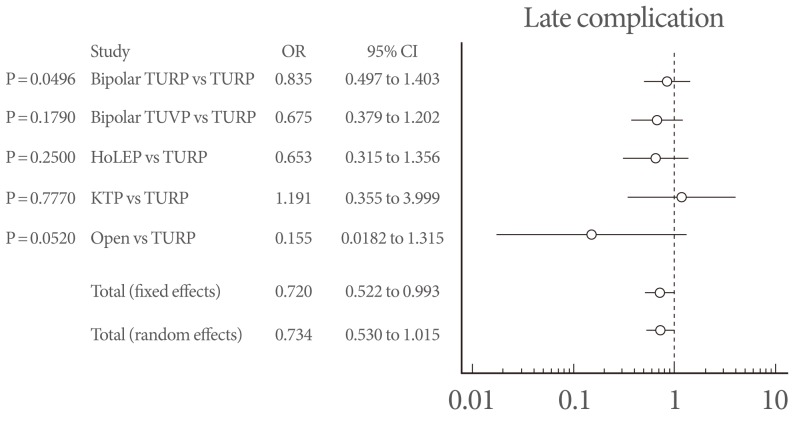
Late complications (Fig. 7)
Fig. 7.
Forest plot of late complications. OR, odds ratio; CI, confidence interval; TURP, transurethral resection of the prostate; TUVP, transurethral vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
There were no statistically significant differences in any of the modalities compared with TURP. However, bladder neck contracture, urethral stricture, dysuria, and reintervention episode occurred more commonly in the KTP group than in the others (Table 5).
Table 5.
Late operative complication
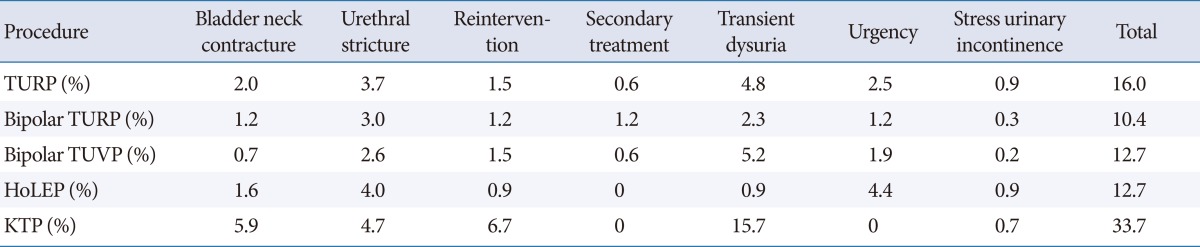
TURP, transurethral resection of prostate; TUVP, transurethral vaporisation of the prostate; HoLEP, holmium laser enucleation of the prostate; KTP, potassium-titanyl-phosphate.
DISCUSSION
BPH results from the proliferation of smooth muscle cells and epithelial cells in the prostatic transitional zone [9]. The treatment of LUTS/BPH is aimed at improving QoL and preventing complications such as urinary tract infection and urinary retention. Treatment methods are largely divided into surgery, medical treatment, and watchful waiting [10]. Watchful waiting is applicable to patients with mild symptoms or with moderate-to-severe symptoms but no complications. This treatment option requires measurement of prostate volume and Qmax annually [11]. For medical management, representative drugs are 5-ARIs and alpha-adrenergic blockers. 5-ARI lowers the serum dihydrotestosterone level and reduces the volume of the prostate [12]. Alpha-adrenergic blockers improve voiding symptoms by relaxation of smooth muscle in the prostate [13]. However, when patients have concomitant complications such as hematuria, infection, or urinary tract obstruction, surgical management is warranted [14]. Many surgical techniques have been developed, such as open prostatectomy, HoLEP, KTP, TURP, bipolar TURP, and bipolar TUVP. Until now, TURP has remained the gold standard treatment option for LUTS/BPH [11]. However, TURP faces many challenges, such as morbidity and functional outcomes [15].
TURP
Accord to our results, TURP was one of the most effective surgical modalities for relieving the obstruction due to BPH. This method needed less reintervention and showed effectiveness for relieving the voiding symptoms, including reduction of IPSS and improvement of Qmax. However, as shown in Tables 3 and 4, TURP has many intraoperative and perioperative complications, such as bleeding, clot retention, and transfusion. Nonetheless, the late complication rate was not inferior compared with other surgical methods. Considering these results, TURP is a worthy mode of surgical intervention for treating LUTS/BPH.
Bipolar TURP
In our meta-analysis, bipolar TURP showed comparable functional outcomes to TURP. Moreover, bipolar TURP showed a shorter length of Foley catheterization and lower intraoperative and perioperative complications. However, to replace TURP, long-term, large-scale, randomized controlled trials will be needed.
HoLEP
Many articles have shown that for large prostates, HoLEP shows superior functional outcomes to open prostatectomy [16,17]. Some parameters of HoLEP, such as length of hospital stay and duration of Foley catheterization, showed supremacy to TURP. Moreover, HoLEP seemed to be effective for avoiding intraoperative and perioperative complications, even though it showed bladder mucosal injury during morcellation of resected prostate adenoma. To confirm the effectiveness and safety of HoLEP, many studies should be performed in relatively small prostates, and long-term comparative studies are needed.
KTP Laser Vaporization of the Prostate
For small to moderate prostate volume, KTP showed comparable functional outcomes, such as for Qmax, PVR, IPSS, and QoL, to TURP. Also, KTP had some benefits, such as a lower incidence of intraoperative complications compared with TURP in patients with a small to moderate prostate volume. However, KTP showed a higher incidence of late complications, such as bladder neck contracture and urethral stricture. Thus, long-term, large-scale randomized controlled studies, conducted for large prostates, should be conducted to prove the usefulness and safety of KTP.
We conducted a meta-analysis of transurethral surgeries for LUTS/BPH. It will be helpful to identify the advantages and disadvantages of each surgical modality. However, we conducted the meta-analysis without a quality analysis of the articles. This is a limitation of the present study even though we performed our analysis of the articles that showed the highest level of evidence.
In conclusion, this study showed statistically comparable efficacy and overall morbidity of transurethral surgeries compared with TURP. Functional outcomes and complications at each step varied for each modality. The selection of an appropriate surgical modality for BPH should be assessed by fully understanding each patient's clinical conditions.
Footnotes
No potential conflict of interest relevant to this article was reported.
SUPPLEMENTARY MATERIALS
Supplementary material can be found via http://www.einj.org/src/sm/inj-17-59-s001.pdf.
References
- 1.Lepor H. Pathophysiology, epidemiology, and natural history of benign prostatic hyperplasia. Rev Urol. 2004;6(Suppl 9):S3–S10. [PMC free article] [PubMed] [Google Scholar]
- 2.Hoke GP, McWilliams GW. Epidemiology of benign prostatic hyperplasia and comorbidities in racial and ethnic minority populations. Am J Med. 2008;121(8 Suppl 2):S3–S10. doi: 10.1016/j.amjmed.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 3.Speakman MJ. Who should be treated and how? Evidence-based medicine in symptomatic BPH. Eur Urol. 1999;36(Suppl 3):40–51. doi: 10.1159/000052348. [DOI] [PubMed] [Google Scholar]
- 4.Souverein PC, Erkens JA, de la Rosette JJ, Leufkens HG, Herings RM. Drug treatment of benign prostatic hyperplasia and hospital admission for BPH-related surgery. Eur Urol. 2003;43:528–534. doi: 10.1016/s0302-2838(03)00089-7. [DOI] [PubMed] [Google Scholar]
- 5.Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP): incidence, management, and prevention. Eur Urol. 2006;50:969–979. doi: 10.1016/j.eururo.2005.12.042. [DOI] [PubMed] [Google Scholar]
- 6.Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, et al. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol. 2010;58:384–397. doi: 10.1016/j.eururo.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Chung JH, Kang DH, Jo JK, Lee SW. Assessing the quality of randomized controlled trials published in the Journal of Korean Medical Science from 1986 to 2011. J Korean Med Sci. 2012;27:973–980. doi: 10.3346/jkms.2012.27.9.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Auffenberg GB, Helfand BT, McVary KT. Established medical therapy for benign prostatic hyperplasia. Urol Clin North Am. 2009;36:443–459. doi: 10.1016/j.ucl.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines) Eur Urol. 2004;46:547–554. doi: 10.1016/j.eururo.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 11.McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011;185:1793–1803. doi: 10.1016/j.juro.2011.01.074. [DOI] [PubMed] [Google Scholar]
- 12.Marberger M, Harkaway R, de la Rosette J. Optimising the medical management of benign prostatic hyperplasia. Eur Urol. 2004;45:411–419. doi: 10.1016/j.eururo.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 13.Chapple CR. Alpha adrenoceptor antagonists in the year 2000: is there anything new? Curr Opin Urol. 2001;11:9–16. doi: 10.1097/00042307-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Taylor J, Harrison SC, Assassa RP, McGrother CW Leicestershire MRC Incontinence Study Group. The pattern and progression of lower urinary tract symptoms after transurethral prostatectomy compared with those seen in the general population. Eur Urol. 2007;51:1023–1029. doi: 10.1016/j.eururo.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 15.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989;141:243–247. doi: 10.1016/s0022-5347(17)40731-2. [DOI] [PubMed] [Google Scholar]
- 16.Naspro R, Suardi N, Salonia A, Scattoni V, Guazzoni G, Colombo R, et al. Holmium laser enucleation of the prostate versus open prostatectomy for prostates >70 g: 24-month follow-up. Eur Urol. 2006;50:563–568. doi: 10.1016/j.eururo.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 17.Kuntz RM, Lehrich K. Transurethral holmium laser enucleation versus transvesical open enucleation for prostate adenoma greater than 100 gm.:: a randomized prospective trial of 120 patients. J Urol. 2002;168(4 Pt 1):1465–1469. doi: 10.1016/S0022-5347(05)64475-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material can be found via http://www.einj.org/src/sm/inj-17-59-s001.pdf.