Abstract
Among medical education institutions worldwide, the time allotted for anatomy instruction has decreased without any reasonable time optimization suggestions. In addition, the utility of cadaver dissection has long been debated. Herein, we surveyed students' perceptions of anatomy education with respect to time and hands-on cadaver dissection, at Seoul National University College of Medicine. With the help of a questionnaire, we surveyed third- and fourth-year students at our institute who had completed the anatomy module as freshmen as well as their clinical clerkship. At our institute, students complete 50 hours of anatomy lectures and 120 hours of dissection laboratory during their first year. According to the survey responses, they generally considered these durations to be adequate for achieving their anatomy education goals. Almost all the students regarded the dissection laboratory as an essential and most helpful modality. Thus, we suggest that these ranges of time along with cadaver dissection could be useful guidelines for optimized anatomy education. The survey data also indicated that a more clinically oriented anatomy education could improve students' results.
Keywords: Anatomy education, Cadaver dissection, Korean medical college
Introduction
Gross anatomy is the cornerstone of medical education; anatomical knowledge is undoubtedly essential for doctors regardless of their specialty [1-3], particularly since they continue to perform physical examinations, make medical decisions, communicate with colleagues, and provide explanations to patients. Furthermore, expert knowledge of anatomy is essential in the present day, particularly for surgeons, because of the development of various surgical techniques and emergence of more sophisticated imaging technologies [4]. Nevertheless, the time devoted to gross 2013anatomy education has steadily declined worldwide. For example, in the United States, marked reduction in anatomy teaching hours has been noted since 1939 [1, 5, 6]. Australian universities decreased anatomy education time by 80% because of the implementation of a problem-based graduate program [7]. Such reductions are justified in some ways. First, the biomedical knowledge that students are required to acquire from their preclinical curriculum has drastically increased. In addition, new disciplines such as the patient-doctor relationship, bioinformatics, and others, have been included in the curriculum without a corresponding extension of the total instruction time, resulting in a decrease in time devoted to anatomy. Another important factor is medical education's paradigm shift towards integrated, student-centered, and clinical competency-accentuated approaches represented by "Tomorrow's Doctors" [8, 9]. These curricular reforms have resulted in a reduction of not only the time allocated to gross anatomy education, but also, necessarily, its content [2].
Another point of contention concerning anatomy education is hands-on cadaver dissection. While many have insisted on its importance and even indispensability [10, 11], others have denied this claim [12]. In fact, hands-on dissection has frequently been replaced, at least in part, by other types of materials such as prosected materials, models, plastinated specimens, medical imaging, and computer-generated images [7, 13]. In some extreme cases, cadaver dissection has been completely abandoned [14].
The overall danger of this de-emphasis of anatomy education in medical programs is that students are less-than-adequately prepared to fulfill their later-appointed roles as doctors [1, 4, 15]. Until recently, no consensus has been reached on the necessary anatomy instruction time, or whether cadaver dissection is essential or can be replaced with other modules.
Worldwide trends in medical education have influenced Korean medical education for decades by the introduction of an integrated curriculum, implementation of problem-based learning, early exposure to clinics, and so on. These reforms have changed basic science education including anatomy. However, the changes that have actually occurred and students' perceptions of them have not yet been assessed.
In the present study, we evaluated students' responses to a survey on anatomy education including cadaver dissection to determine whether the allotted time for instruction is appropriate and whether the cadaver dissection laboratory is perceived to be meaningful.
Materials and Methods
To gauge student experiences of anatomy education, a questionnaire survey was conducted from the end of 2011 to the beginning of 2012, spanning the winter vacation period. The target respondents were principally third-year students, in addition to a smaller cohort of fourth-year peers from the Seoul National University College of Medicine (SNU CM) (Table 1). These students had completed an anatomy module as freshmen as well as their clinical clerkship, which included internal medicine, surgery, obstetrics and gynecology, pediatrics, psychiatry, emergency medicine, orthopedics, radiology, neurology, and nuclear medicine. The fourth-year students had also attended select clinical training (6 modules from courses in family medicine, anesthesiology, radiation oncology, urology, plastic surgery, neurosurgery, ophthalmology, otolaryngology, rehabilitation medicine, laboratory medicine, dermatology, and cardiovascular surgery, according to their choice). The questionnaire comprised questions on the students' anatomy education objectives, the levels of accomplishment they had achieved, the time adequacy and credits devoted to anatomy lectures and laboratory work, and the usefulness of cadaver dissection. The students were randomly selected, and they answered the questionnaire anonymously with yes-or-no or 5-point Likert scale responses according to the type of question. This study was exempted from Institutional Review Board review based on the Korean Bioethics and Safety Act and Seoul National University Medical College Human Research Protection Program (SNUMC HRPP) Standard Operating Procedure (IRB No. E-1301-004-453).
Table 1.
Numbers of respondents in this study
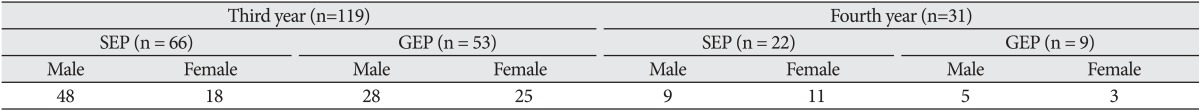
SEP, standard entry program; GEP, graduate entry program.
The R-package software version 2.10.1 (The R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analysis, and the P-value was set at 0.05.
Results
The present study enrolled 150 students, 119 of whom were in their third year (119/158, 75.8%) and 31 in their fourth year (31/148, 20.9%). Although the number of subjects were relatively small (fourth-year students for example, many of whom were graduating during the survey period, had not remained on campus), the response rate was 100%. The students' mean age was 25.3±2.7 years (range, 21-36 years); 90 were men, 57 were women, and the remaining 3 did not indicate their sex. The standard entry program (SEP) included 88 students, and the graduate entry program (GEP) included 62 students. Additional and more detailed statistics are provided in Table 1.
At SNU CM, the first semester of the 4-year medical education program includes 50 hours of anatomy lectures and 120 hours of dissection laboratory. We evaluated the students' perception of the anatomy education they received more than 2 (third-year students) or 3 (fourth-year students) years previously. For all items, no statistically significant differences in the responses were observed according to sex, age, student year, or specific program (SEP or GEP). Thus, we herein present the data in their entirety.
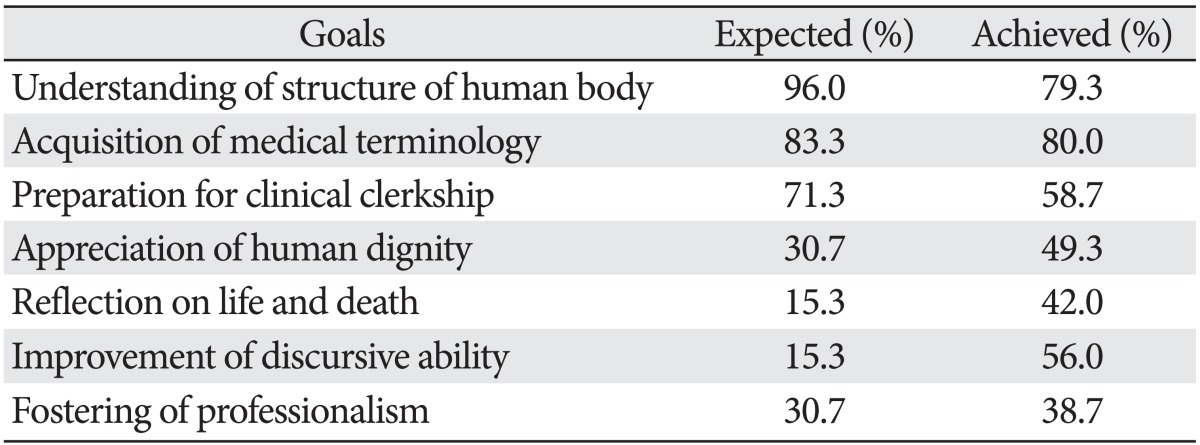
We first asked students what they thought about the ultimate goals of anatomy education and the extent to which they felt they had achieved them. We provided 7 possible answers and requested that they check those applicable to them: 1) acquisition of basic medical terminology, 2) understanding of the human body structure, 3) preparation for clinical clerkship, 4) appreciation of human dignity, 5) reflection on life and death, 6) improvement of discursive ability, and 7) fostering of professionalism.
Almost all the students (96.0%) considered the ultimate goal of anatomy education to be "understanding of the human body structure" (Table 2). A majority of students also felt that "acquisition of basic medical terminology" (83.3%) and "preparation for clinical clerkship" (71.3%) were the goals of anatomy education. Correspondingly, the students indicated that they had acquired "basic medical terminology" (80.0%) and an "understanding of the structure of the human body" (79.3%) through their anatomy education and that such knowledge was helpful in their clinical studies (58.7%) (Table 2). In addition, although they did not recognize other aspects such as "appreciation of human dignity," "reflection on life and death," or "fostering of professionalism" as major goals of anatomy education, almost 50% of the students had had a chance to reflect on life and death (42%), and many responded that their discursive ability improved through anatomy education (56.0%), perhaps specifically through participation in the team-based dissection laboratory.
Table 2.
Students' response for expectation and actual achievement for each goal
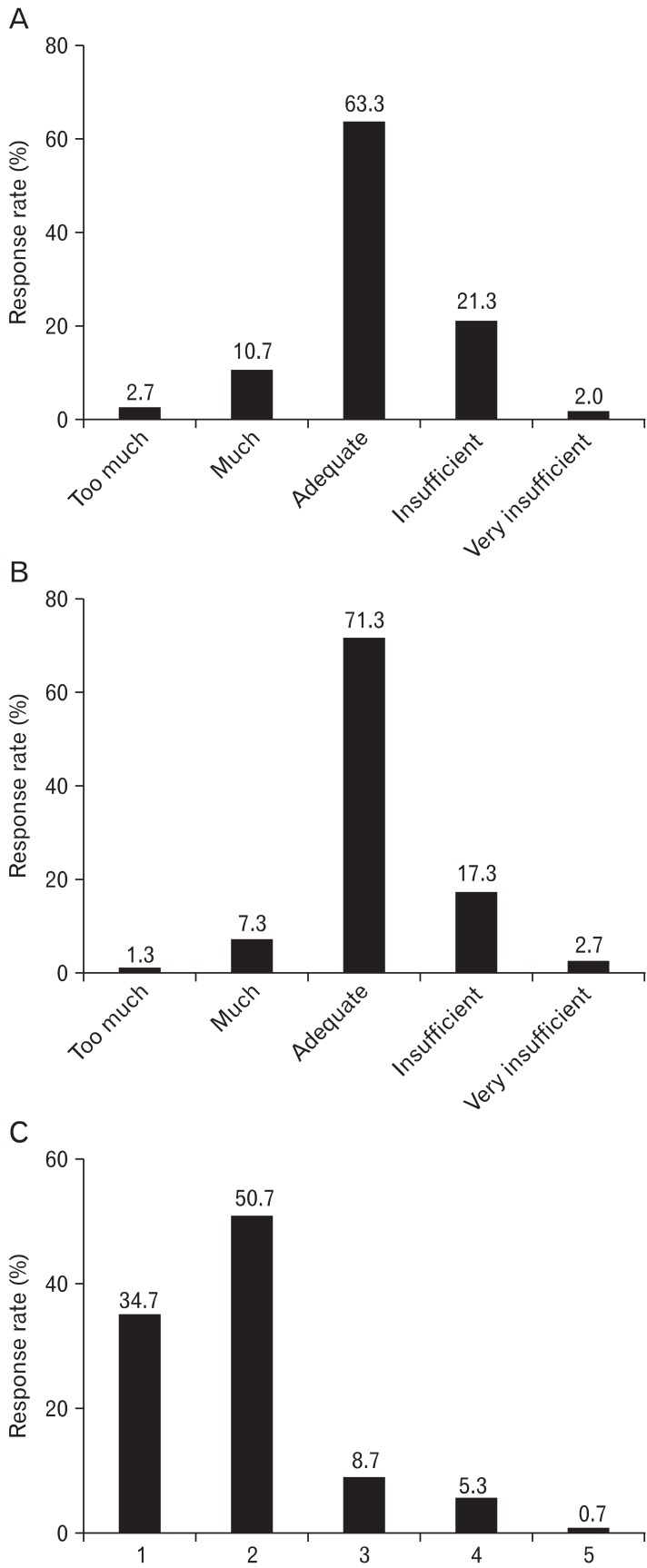
With regard to the adequacy of hours allocated for anatomy lectures and dissection laboratory for achieving the aforementioned goals, most of the students responded that they were adequate (lectures, 63.3%; laboratory, 71.3%) (Fig. 1A, B). Some students felt that the hours were somewhat excessive (lectures, 13.4%; laboratory, 8.6%) or insufficient (lectures, 23.3%; laboratory, 20.0%). These respondents were of the opinion that 50 hours of lectures and 120 hours of laboratory were roughly adequate for gaining an understanding of the structure of the human body and acquiring basic medical terminology; this interpretation was supported by the responses to the question on the value of the 5 anatomy credits (out of the 19 total credits for the semester and 148 over 4 years) for those purposes. Eighty-five percent of the students responded positively, and only 6.0% responded negatively (Fig. 1C).
Fig. 1.
Response rates to the questions on the adequacy of time for anatomy lectures (A), laboratory (B), and credit for anatomy (C). On the X-axis in (C), 1=strongly agree, 2=agree, 3=neutral, 4=disagree, and 5=strongly disagree.
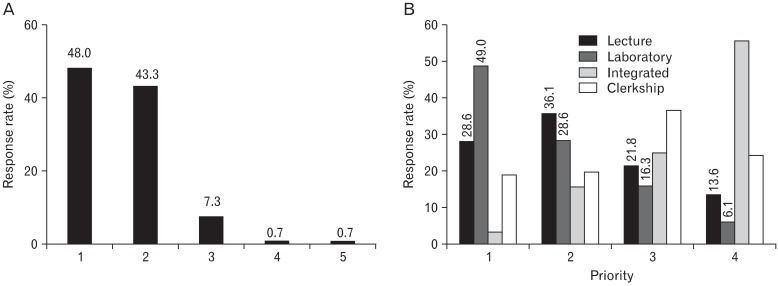
Regarding cadaver dissection, almost all the students (91.3%) considered it useful to the study of anatomy; only 1.3% replied negatively (Fig. 2A). In addition, 49.0% of the respondents believed that a dissection laboratory was the best method for acquiring anatomical knowledge compared with the anatomy module lectures, organ-based integrated course (second year) lectures, or clinical clerkship lectures (Fig. 2B). When asked about the need for additional anatomy education hours during clinical clerkship, 31.3% of the respondents agreed to the need for additional teaching hours, while 44.7% disagreed.
Fig. 2.
(A) Response rates to questions on the usefulness of the dissection laboratory for acquiring knowledge of anatomy. On the X-axis, 1=strongly agree, 2=agree, 3=neutral, 4=disagree, and 5=strongly disagree. Over 90% of the students found the hands-on dissection laboratory to be useful. (B) Response rates to questions asking students to determine the order of helpfulness for acquiring anatomical knowledge from anatomy lectures, anatomy laboratory, during organ-based integrated lectures, and lectures during clinical clerkship. On the X-axis, the numbers represent the order of preference.
Discussion
The education time at SNU CM comprising 50 h of lectures and 120 hours of dissection laboratory is 23% below and 44.4% above the Korean average, respectively [16]. Our students perceived the time and credits to be adequate for both lectures and laboratory (Fig. 1A, B).
Regarding the goals of anatomy education, students satisfactorily acquired basic medical terminology (80.0%) and an understanding of the human body structure (79.3%). However, during the same period, only 58.7% of our surveyed students felt that their anatomy education had been helpful for clinical clerkship (Table 2). This relatively negative response might be attributed to anatomy instruction content. Anatomical knowledge related to physical examination [17] and clinical procedures [18] should be perceived by students as "helpful" for their clinical clerkship. However, if what they learn proves to be not fully relevant to their clinical practice, they will not perceive their anatomy education to be helpful. In this regard, the American Association of Clinical Anatomists (AACA) once suggested a curriculum that ensures "a solid anatomical basis for current and future medical practice," focused on the "significance of anatomical terminology, normal variation, 3-dimensional relationships, functional and living anatomy, and imaging technology as applied to patient care" [19]. They named this discipline "clinical anatomy." Another important aspect of such education is the mode of content delivery to students. Learning is facilitated when its performance is context-bound [20-22] and its purpose is clear [23]. Indeed, the importance of clinical context in anatomy education is well emphasized in the literature [21, 22, 24]. Clinically oriented anatomy education has been delivered in several ways. Clinical cases frequently have been utilized for this purpose [25, 26], sometimes in association with problem-based or team-based learning. Clinical relevancy can also be implemented in the dissection laboratory, for example, laparoscopy [27], basic clinical procedures [28], or surgical procedures [29] on cadavers. These approaches triggered student interest, made anatomy easy to understand, and resulted in higher test scores. In short, clinical context is supported by many authors who believe that teaching methods need to be tailored to make anatomy more relevant and helpful for clinical education. At SNU CM, anatomy is taught in a traditional didactic manner, even if reflection on or review of its clinical aspects is not proscribed. The dissection laboratory is usually conducted with reference to Grant's Dissector, although some clinical tasks are given to students during the laboratory time [30]. Thus, many of the human body structures that were satisfactorily understood in the anatomy module by the students in this study (79.3%) might not be very relevant to human health and disease. This might be the reason why almost 50% of SNU CM students considered the anatomy they learned to not be sufficiently preparatory for clinical education. If that is the case, the educational content needs to be refined according to the purposes and priorities of clinically oriented anatomy. Nonetheless, careful consideration is required before considerable expense and effort is incurred in instituting new methods such as laparoscopy or surgical procedures.
The usefulness of cadaver dissection to anatomy education has long been debated. While some authors argue that the dissection laboratory is indispensable for anatomy education [10, 31], others note possible disadvantages of dissection compared to other tools such as prosection [32, 33]. The issue of dissection versus prosection aside, some observers argue in favor of complete cadaver-less anatomy education [12]. It is difficult to conclude, based on our present results, whether dissection is more beneficial than prosection or any other teaching tool such as computer images. However, we can at least declare that dissection is far from meaningless. Our students regarded the 120 h dedicated to cadaver dissection as adequate (Fig. 1A); moreover, they perceived hands-on dissection as a necessary tool for studying anatomy, and considered it more valuable to the acquisition of anatomical knowledge than lectures (Fig. 2). Interestingly, a study conducted by the Ulm University Faculty of Medicine found that >70% of the students perceived the dissection course to be "very important"; furthermore, they ranked anatomy as the most important preclinical subject, both before and after a 16-week dissection course [34]. Therefore, we may regard dissection as the primary tool for laboratory work in anatomy education, whereas other tools such as prosected specimens and computer-aided multimedia can be supplementary, particularly for complicated 3-dimensional structures, to enhance understanding [35]. In such a case, supplemental tools would be sufficient for self-learning and do not necessarily have to be utilized during curricular hours.
Another benefit of cadaver dissection is that it can be a platform for learning several various attributes of professionalism, among which are leadership skills [36, 37]. Cadaver dissection can be considered ideal in this regard, particularly because it is introduced early in students' medical education and is conducted in small-group settings. Perhaps most fundamentally, cadavers, which are donated human bodies, provide students with insight into humanity and morality [38]. Facing the cadaver itself, for example, requires students to confront and reflect on the concept of life and death [36]. Cadaver dissection also is a chance for students to learn to collaborate with peers. In support of this contention, our results showed that although non-biomedical aspects such as appreciation of human dignity, death, and professionalism were not frequently regarded as the ultimate goals of the dissection laboratory or emphasized by instructors, almost 50% of the students surveyed had a chance to contemplate them (Table 2). As for the students' discursive ability with their peers, >50% of the survey respondents (56.0%) indicated an improvement.
In conclusions SNU CM's 50-hour lecture and 120-hour dissection laboratory appear adequate, and at least not insufficient, for anatomy education. Nevertheless, this study suggests the need for major educational refinements. First, we should redefine the core content of anatomy education to make it more clinically oriented. Doing so, we believe, can deliver anatomical knowledge to students more effectively, save instruction time, and most importantly, enhance the clinical relevance of anatomy education. Second, we should utilize the dissection laboratory as a tool for fostering professionalism. To this end, a well-structured approach will be required.
References
- 1.Cottam WW. Adequacy of medical school gross anatomy education as perceived by certain postgraduate residency programs and anatomy course directors. Clin Anat. 1999;12:55–65. doi: 10.1002/(SICI)1098-2353(1999)12:1<55::AID-CA8>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 2.Older J. Anatomy: a must for teaching the next generation. Surgeon. 2004;2:79–90. doi: 10.1016/s1479-666x(04)80050-7. [DOI] [PubMed] [Google Scholar]
- 3.Turney BW. Anatomy in a modern medical curriculum. Ann R Coll Surg Engl. 2007;89:104–107. doi: 10.1308/003588407X168244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raftery AT. Basic surgical training. 1: Postgraduate surgical examinations in the UK and Ireland. Clin Anat. 1996;9:163–166. doi: 10.1002/(SICI)1098-2353(1996)9:3<163::AID-CA5>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 5.Gartner LP. Anatomical sciences in the allopathic medical school curriculum in the United States between 1967-2001. Clin Anat. 2003;16:434–439. doi: 10.1002/ca.10159. [DOI] [PubMed] [Google Scholar]
- 6.Drake RL, McBride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009;2:253–259. doi: 10.1002/ase.117. [DOI] [PubMed] [Google Scholar]
- 7.Craig S, Tait N, Boers D, McAndrew D. Review of anatomy education in Australian and New Zealand medical schools. ANZ J Surg. 2010;80:212–216. doi: 10.1111/j.1445-2197.2010.05241.x. [DOI] [PubMed] [Google Scholar]
- 8.General Medical Council. Tomorrow's Doctors. Recommendations on undergraduate medical education 1993 [Internet] General Medical Council; 1993. [cited 2013 Jun 1]. Available from: http://www.gmc-uk.org/education/undergraduate/historic_policy.asp. [Google Scholar]
- 9.General Medical Council. Tomorrow's Doctors. Regulating doctors, ensuring good medical practice 2003 [Internet] General Medical Council; 1993. [cited 2013 Jun 1]. Available from: http://www.gmc-uk.org/education/undergraduate/historic_policy.asp. [Google Scholar]
- 10.Granger NA. Dissection laboratory is vital to medical gross anatomy education. Anat Rec B New Anat. 2004;281:6–8. doi: 10.1002/ar.b.20039. [DOI] [PubMed] [Google Scholar]
- 11.Pawlina W, Lachman N. Dissection in learning and teaching gross anatomy: rebuttal to McLachlan. Anat Rec B New Anat. 2004;281:9–11. doi: 10.1002/ar.b.20038. [DOI] [PubMed] [Google Scholar]
- 12.McLachlan JC, Bligh J, Bradley P, Searle J. Teaching anatomy without cadavers. Med Educ. 2004;38:418–424. doi: 10.1046/j.1365-2923.2004.01795.x. [DOI] [PubMed] [Google Scholar]
- 13.Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: a review for its modernization. Anat Sci Educ. 2010;3:83–93. doi: 10.1002/ase.139. [DOI] [PubMed] [Google Scholar]
- 14.Plaisant O, Cabanis EA, Delmas V. Going back to dissection in a medical curriculum: the paradigm of Necker-Enfants Malades. Surg Radiol Anat. 2004;26:504–511. doi: 10.1007/s00276-004-0271-x. [DOI] [PubMed] [Google Scholar]
- 15.Fitzgerald JE, White MJ, Tang SW, Maxwell-Armstrong CA, James DK. Are we teaching sufficient anatomy at medical school? The opinions of newly qualified doctors. Clin Anat. 2008;21:718–724. doi: 10.1002/ca.20662. [DOI] [PubMed] [Google Scholar]
- 16.Hwang YI. Analysis of anatomy education in Korean medical schools; Proceedings of the 59th Annual Meeting of Korean Association of Anatomists; 2009 Oct 22-23; Daegu, Korea. Seoul: Korean Association of Anatomists; p. 53. [Google Scholar]
- 17.Educational Affairs Committee, American Association of Clinical Anatomists. Clinical anatomy and the physical examination part I: thorax, abdomen, perineum, and pelvis. Clin Anat. 2001;14:332–348. doi: 10.1002/ca.1061. [DOI] [PubMed] [Google Scholar]
- 18.American Association of Clinical Anatomists, Educational Affairs Committee. The clinical anatomy of several invasive procedures. Clin Anat. 1999;12:43–54. doi: 10.1002/(SICI)1098-2353(1999)12:1<43::AID-CA7>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 19.A clinical anatomy curriculum for the medical student of the 21st century: gross anatomy. Clin Anat. 1996;9:71–99. doi: 10.1002/(SICI)1098-2353(1996)9:2<71::AID-CA1>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 20.Godden DR, Baddeley AD. Context-dependent memory in two natural environments: on land and underwater. Br J Psychol. 1975;66:325–331. [Google Scholar]
- 21.Koens F, Mann KV, Custers EJ, Ten Cate OT. Analysing the concept of context in medical education. Med Educ. 2005;39:1243–1249. doi: 10.1111/j.1365-2929.2005.02338.x. [DOI] [PubMed] [Google Scholar]
- 22.Koens F, Ten Cate OT, Custers EJ. Context-dependent memory in a meaningful environment for medical education: in the classroom and at the bedside. Adv Health Sci Educ Theory Pract. 2003;8:155–165. doi: 10.1023/a:1024993619713. [DOI] [PubMed] [Google Scholar]
- 23.Regehr G, Norman GR. Issues in cognitive psychology: implications for professional education. Acad Med. 1996;71:988–1001. doi: 10.1097/00001888-199609000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Zumwalt AC, Lufler RS, Monteiro J, Shaffer K. Building the body: active learning laboratories that emphasize practical aspects of anatomy and integration with radiology. Anat Sci Educ. 2010;3:134–140. doi: 10.1002/ase.153. [DOI] [PubMed] [Google Scholar]
- 25.Drake RL. A unique, innovative, and clinically oriented approach to anatomy education. Acad Med. 2007;82:475–478. doi: 10.1097/ACM.0b013e31803eab41. [DOI] [PubMed] [Google Scholar]
- 26.Vasan NS, DeFouw DO, Holland BK. Modified use of team-based learning for effective delivery of medical gross anatomy and embryology. Anat Sci Educ. 2008;1:3–9. doi: 10.1002/ase.5. [DOI] [PubMed] [Google Scholar]
- 27.Park A, Schwartz RW, Witzke DB, Roth JS, Mastrangelo M, Birch DW, Jennings CD, Lee EY, Hoskins J. A pilot study of new approaches to teaching anatomy and pathology. Surg Endosc. 2001;15:245–250. doi: 10.1007/s004640000310. [DOI] [PubMed] [Google Scholar]
- 28.Wilson DR, Nava PB. Medical student responses to clinical procedure teaching in the anatomy lab. Clin Teach. 2010;7:14–18. doi: 10.1111/j.1743-498X.2009.00349.x. [DOI] [PubMed] [Google Scholar]
- 29.Nutt J, Mehdian R, Parkin I, Dent J, Kellett C. Cadaveric surgery: a novel approach to teaching clinical anatomy. Clin Teach. 2012;9:148–151. doi: 10.1111/j.1743-498X.2012.00536.x. [DOI] [PubMed] [Google Scholar]
- 30.Kang SH, Shin JS, Hwang YI. The use of specially designed tasks to enhance student interest in the cadaver dissection laboratory. Anat Sci Educ. 2012;5:76–82. doi: 10.1002/ase.1251. [DOI] [PubMed] [Google Scholar]
- 31.Aziz MA, McKenzie JC, Wilson JS, Cowie RJ, Ayeni SA, Dunn BK. The human cadaver in the age of biomedical informatics. Anat Rec. 2002;269:20–32. doi: 10.1002/ar.10046. [DOI] [PubMed] [Google Scholar]
- 32.Topp KS. Prosection vs. dissection, the debate continues: rebuttal to Granger. Anat Rec B New Anat. 2004;281:12–14. doi: 10.1002/ar.b.20037. [DOI] [PubMed] [Google Scholar]
- 33.Winkelmann A, Hendrix S, Kiessling C. What do students actually do during a dissection course? First steps towards understanding a complex learning experience. Acad Med. 2007;82:989–995. doi: 10.1097/ACM.0b013e31814a51ef. [DOI] [PubMed] [Google Scholar]
- 34.Bockers A, Jerg-Bretzke L, Lamp C, Brinkmann A, Traue HC, Böckers TM. The gross anatomy course: an analysis of its importance. Anat Sci Educ. 2010;3:3–11. doi: 10.1002/ase.124. [DOI] [PubMed] [Google Scholar]
- 35.Bergman EM, van der Vleuten CP, Scherpbier AJ. Why don't they know enough about anatomy? A narrative review. Med Teach. 2011;33:403–409. doi: 10.3109/0142159X.2010.536276. [DOI] [PubMed] [Google Scholar]
- 36.Escobar-Poni B, Poni ES. The role of gross anatomy in promoting professionalism: a neglected opportunity! Clin Anat. 2006;19:461–467. doi: 10.1002/ca.20353. [DOI] [PubMed] [Google Scholar]
- 37.Lachman N, Pawlina W. Integrating professionalism in early medical education: the theory and application of reflective practice in the anatomy curriculum. Clin Anat. 2006;19:456–460. doi: 10.1002/ca.20344. [DOI] [PubMed] [Google Scholar]
- 38.Gunderman RB, Wilson PK. Viewpoint: exploring the human interior: the roles of cadaver dissection and radiologic imaging in teaching anatomy. Acad Med. 2005;80:745–749. doi: 10.1097/00001888-200508000-00008. [DOI] [PubMed] [Google Scholar]