Abstract
Objective
Effective communication between intensive care unit (ICU) providers and families is crucial given the complexity of decisions made regarding goals of therapy. Using video images to supplement medical discussions is an innovative process to standardize and improve communication. In this six-month, quasi-experimental, pre-post intervention study we investigated the impact of a cardiopulmonary resuscitation (CPR) video decision support tool upon knowledge about CPR among surrogate decision makers for critically ill adults.
Methods
We interviewed surrogate decision makers for patients aged 50 and over, using a structured questionnaire that included a four-question CPR knowledge assessment similar to those used in previous studies. Surrogates in the post-intervention arm viewed a three-minute video decision support tool about CPR before completing the knowledge assessment and completed questions about perceived value of the video.
Results
We recruited 23 surrogates during the first three months (pre-intervention arm) and 27 surrogates during the latter three months of the study (post-intervention arm). Surrogates viewing the video had more knowledge about CPR (p=0.008); average scores were 2.0 (SD 1.1) and 2.9 (SD 1.2) (out of a total of 4) in pre-intervention and post-intervention arms. Surrogates who viewed the video were comfortable with its content (81% very) and 81% would recommend the video. CPR preferences for patients at the time of ICU discharge/death were distributed as follows: pre-intervention: full code 78%, DNR 22%; post-intervention: full code 59%, DNR 41% (p=0.23).
Introduction
Shared decision making in the intensive care unit (ICU) is a challenging endeavor due to the number of medical interventions available, and to the difficulty in prognosticating the success of these interventions in the face of much uncertainty.1,2 Reliance on surrogates to make highly preference-sensitive decisions that are consistent with the wishes of patients is an important but challenging feature of the decision making process.3,4 Effective communication between critical care providers and surrogates, who are often family members, is a critical ingredient to informed decision making regarding goals of care, including whether or not to pursue cardiopulmonary resuscitation (CPR) in the intensive care unit (ICU).5
Interventions to alter clinicians' communication behavior are labor intensive and difficult to implement and sustain on a large scale. Several well-conducted, multicenter trials that sought to improve communication with families have had no effect on patient or family outcomes, length of stay, or resource use.6–9 Innovative interventions to improve understanding and better inform decision making between critical care providers and surrogates may help allay these present gaps in communication.
Video decision support tools represent an innovative and powerful tool to better inform the decision making process in the ICU by standardizing and improving communication between providers and surrogates. Decision support tools have been well established as an effective means of helping patients make informed decisions that are consistent with their values.10 There is a growing body of work exploring the use of video decision support tools to educate patients and their families about life-prolonging interventions. A video decision support tool is not meant to substitute for conversations with patients' physicians, but to enhance them. For example, among patients with cancer and dementia, when compared to verbal communication alone, patients who viewed videos were more knowledgeable about their options, more certain of their decisions, and more likely to avoid life-prolonging interventions if the predicted success rate were low.11–15 To the best of our knowledge, video decision support tools have not been introduced to the critical care setting to improve communication and better inform decision making.
Almost all surrogates of critically ill patients are asked to establish goals of care for their loved one, including whether their loved one should undergo CPR. Yet most people hold misconceptions about what CPR entails and its effectiveness.16 We hypothesized that a CPR video decision support tool would introduce an element of standardization to the communication process and better inform surrogates of patients admitted to the ICU about decisions surrounding CPR. We conducted a six-month pre-post intervention study and compared surrogates' knowledge of CPR in the context of usual care with surrogates' knowledge of CPR after viewing a CPR video decision support tool. A secondary aim was to compare the code status of patients at ICU discharge or death.
Materials and Methods
Participants
We recruited surrogate decision makers of consecutive patients admitted to the Massachusetts General Hospital (MGH) medical ICU over the course of six months within the first 72 hours of ICU admission. All patients were considered for our study if they met the following eligibility criteria: aged 50 years of age or older, not capable of making medical decisions on his/her own as determined by the medical attending, presence of a family member or loved one who was the surrogate decision maker, and likely to survive >24h as determined by the attending physician. Notably, as part of standard of care, all surrogates and family members of patients in this ICU are invited to participate in family meetings within the first 72 hours of admission.
Surrogates were required to be over the age of 21, English speaking, and not vision impaired. Additional family members were permitted to witness the interview or view the video, but only the responses of the primary surrogate decision maker were recorded and analyzed. In situations where there was no appointed health care proxy, the medical team identified the family member acting as primary decision maker for the patient. The majority of interviews were conducted by a single physician (JBM). Approval for the project was granted by the institutional review board of MGH.
Study design
The study was a six-month, quasi-experimental, pre-post intervention trial. A structured verbal questionnaire was designed following a review of the communication and decision making critical care literature and in consultation with experts in intensive care and decision making. The questionnaire was adapted from prior studies.11–15 The baseline assessment included age, sex, self-reported race and ethnicity, religion and intensity of religious practice, educational status, and marital status. Surrogates provided this information for themselves and for the patient and indicated whether the patient had engaged in prior conversations about goals of therapy and/or had completed any advance directives (either identified a health care proxy and/or drafted a living will). Simplified Acute Physiology Score (SAPS) was recorded for each patient, and surrogates were also asked to rate their family member's health status just prior to admission.
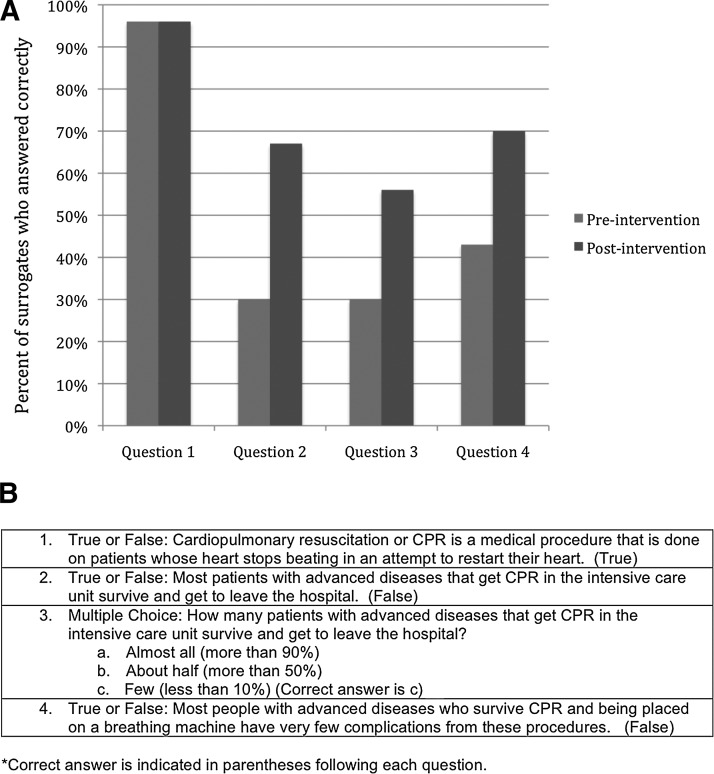
Surrogates in the pre-intervention arm of the study completed a four-question knowledge assessment about CPR similar to those that have been used in previous studies (see Fig. 1B). Surrogates in the post-intervention arm of the study viewed a three-minute video decision support tool about CPR, followed by the same four-question knowledge assessment.
FIG. 1.
Panel A. Responses to CPR knowledge assessment by study arm. Panel B. Knowledge assessment questionnaire.
The knowledge measurement included four questions, three true/false queries, and one multiple-choice item, which were intended to measure the participants' understanding of CPR and were used and validated in our previous studies (see Fig. 1B).11–15 Overall scores ranged from 0 to 4, with higher scores representing more knowledge of the choices of medical care. Surrogates in the post-intervention arm of our study viewed the CPR video decision support tool before answering the knowledge questions. The three-minute video decision support tool was shown on a laptop computer in a private family conference room in the ICU or in the patient's room at the family's request. The narrated video depicts simulation of CPR, with compression and shocks delivered to a mannequin by three physicians, as well as simulated intubation during cardiac resuscitation. Additionally, the video shows a real patient intubated and sedated in an ICU setting undergoing routine medication administration by a critical care nurse. The video was developed by the investigative team with experience in video-assisted medical decision making.
The video was vetted by an expert panel of intensivists, decision making and health literacy experts, and also shown to focus groups of patients and their families.17 Filming was performed without stage directions or prompts, in order to convey realism.18,19 Consent to film the video and for its use in research was obtained from the filmed patients and their families.
For those participants who viewed the video, we measured the perceived value of the video by asking subjects to rate on a four-point scale whether they were comfortable viewing the video, if they would recommend the video to others, and if they found the video helpful in their understanding of their choices.
Finally, a medical chart review was performed for all patients at time of discharge from the ICU or death to ascertain actual code status (e.g., full code or DNR).
Analysis
The primary outcome measure was overall score on the CPR knowledge assessment. Secondary outcome measures included participants' perceived value of the video as well as CPR preferences at time of death/discharge from ICU.
Participants' baseline characteristics were summarized using proportions for categorical variables and means (standard deviation) for continuous variables. Differences between pre-intervention and post-intervention groups in mean scores of the knowledge assessment were compared with a two-sample t-test assuming normal distribution in scores. Differences between preferences regarding CPR at time of death/ICU discharge were compared between the pre-intervention and post-intervention groups using Fisher's exact tests.
All reported p values were two sided, with p<0.05 representing statistical significance. A priori statistical calculations suggested that at least 22 surrogates in each arm would be required for 80% power to detect differences in mean knowledge scores of 2 (based on differences in knowledge scores in prior studies). A standard deviation of 2.3 was estimated based on prior studies; a very similar six-item knowledge assessment score had a standard deviation of approximately 1.3 and higher standard deviation would be expected on this instrument with fewer items. Data were analyzed using statistical software SAS (SAS version 9.3; SAS Institute, Inc., Cary, NC).
Results
Participants
A total of 39 surrogates met eligibility criteria and were approached to participate in the pre-intervention arm, and 42 surrogates met eligibility criteria and were approached to participate in the post-intervention arm of the study. The most commonly cited reason for declining to participate was “feeling overwhelmed.” A total of 23 (79%) surrogates participated in the pre-intervention arm, and a total of 27 (64%) surrogates participated in the post-intervention arm of the study. Baseline characteristics are presented in Table 1. Most surrogate decision makers were adult children of the patient (61% and 55%), white (88%), and well educated (84% some college and beyond). The population was quite ill, with about two-thirds of patients intubated and 22% ICU mortality in both groups. Differences between the two groups at baseline (including SAPS score) did not reach statistical significance.
Table 1.
Study Population
|
Surrogates |
Pre-intervention arm |
Post-intervention arm |
|---|---|---|
| N | 23 | 27 |
| Relationship to patient | ||
| Spouse, N (%) | 5 (22) | 8 (30) |
| Child/child-in-law, N (%) | 14 (61) | 15 (55) |
| Other, N (%) | 4 (17) | 4 (15) |
| Age, mean (SD) | 51 (14) | 57 (10) |
| Female, N (%) | 17 (74) | 15 (56) |
| White, N (%) | 20 (87) | 24 (89) |
| College education or higher, N (%) | 20 (87) | 22 (81) |
| Patients | ||
| N | 23 | 27 |
|---|---|---|
| Patient age, mean (SD) | 71 (12) | 71 (10) |
| Female, N (%) | 10 (43) | 13 (48) |
| SAPS, mean (SD) | 68 (15) | 70 (15) |
| SAPS, % mortality (SD) | 50 (24) | 54 (26) |
| Intubated patients, N (%) | 16 (70) | 18 (67) |
| Died before ICU discharge, N (%) | 5 (22) | 6 (22) |
SAPS, Simplified Acute Physiology Score.
Outcomes
Primary outcome, CPR knowledge assessment
Surrogates who viewed the video had more knowledge about CPR (p=0.008) compared to surrogates who did not view the video. Average knowledge scores were 2.9 (1.2 SD) and 2.0 (1.1 SD) in post-intervention and pre-intervention arms respectively (p=0.008). Surrogates in both groups had similar responses to question 1, but differed with respect to the remaining questions. (see Fig. 1A.)
Secondary outcomes, comfort with video
The video was highly acceptable to the participants: 25 (93%, 95%CI: 76%–99%) were either “very” or “somewhat” comfortable watching the video; 22 (81%, 95% CI: 67%–96%) would “definitely” or “probably” recommend the video to other surrogates; and 18 (67%, 95% CI: 49%–84%) found the video either “very” or “somewhat” helpful.
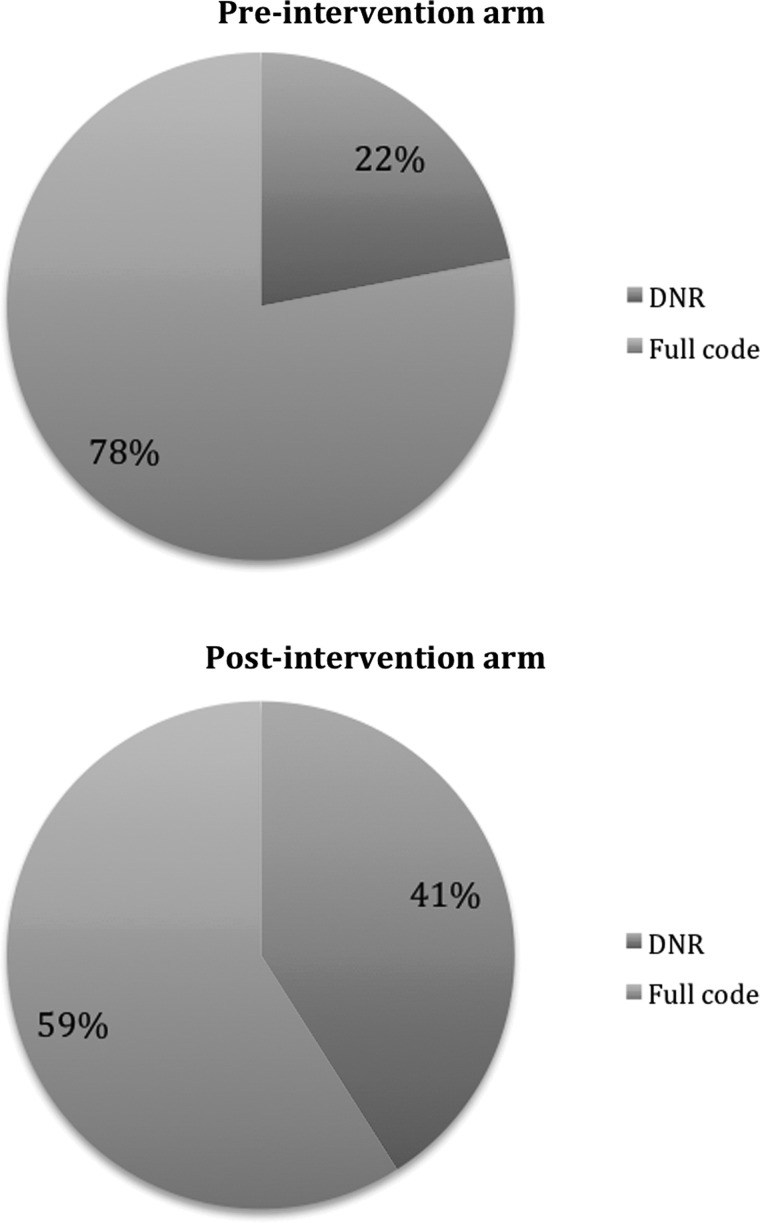
CPR preferences at death/ICU discharge
CPR preferences for patients between the two arms of the study at time of ICU discharge or death differed, though did not reach statistical significance (p=0.23). Based on chart review, 78% of surrogates in the pre-intervention arm decided that their family member would want to be full code, and 22% indicated that their family member would not want to be resuscitated. Among surrogates in the post-intervention arm of the study, 59% decided that their family member would want to be full code, and 41% indicated that their family member would prefer to be DNR (see Fig. 2).
FIG. 2.
Preferences for CPR in the pre-intervention and post-intervention groups at time of ICU discharge or death.
Discussion
The use of a video decision support tool to supplement goals of therapy discussions regarding CPR is an innovative way to enhance communication between health care providers and patients' families in the critical care setting. When surrogate decision makers for critically ill adults viewed a video about CPR, their knowledge of CPR was superior to those who had not viewed the video. Overwhelmingly, surrogates felt comfortable viewing the video and would recommend the video to others. Our study was not powered to detect a difference in the secondary endpoint of code status. Accordingly, it is unclear if the improved knowledge of CPR practices and outcomes created by the video will impact surrogate decision making, and if so, if the decisions will be more aligned with patient preferences.
Effective communication between providers and surrogates regarding CPR is both challenging and critical for informed decision making in the ICU setting.1–4 There is evidence that surrogates' knowledge of intensive care, and their understanding of their family members' preferences, even when there have been explicit conversations about advance care planning, is poor.20,21 Standardization of many critical care interventions has been demonstrated to improve outcomes.22 Standardizing processes to improve provider-family communication may also lead to improvements in the decision making process in the ICU setting. Video decision support tools can augment existing communication between the ICU team and surrogates of critically ill patients by providing standardized information that is critical for informed decision making in a format that is easy for surrogates to understand. Improving knowledge about CPR empowers surrogates by increasing their understanding of the implications of particular choices and decisions they make on behalf of their critically ill family members. Our study builds upon prior studies of video decision support tools for decision making regarding goals of therapy.11–15 Prior work using videos emphasized the impact of video decision support tools on preferences of care in patients with advanced cancer and older patients in the outpatient setting who were making hypothetical decisions. The present study extends this work by using video in the critical care setting with surrogates who are actually making decisions about the medical care of their family member. These findings also suggest the potential for the CPR video to inform the surrogate's own end-of-life preferences.
Our study has several important limitations. First, while the video was shown to surrogates actually making decisions, it was not incorporated into the family meetings, thus was excluded from real-time clinical decision making with the primary medical team, denying us the opportunity to isolate the effect of the video upon choices recorded in the medical record. Our priority during this first study of a video support tool in the critical care setting was to explore whether such a video would be palatable for surrogates. Second, the timing of showing the video may not have been optimal. While surrogates are often asked to make decisions about potentially life prolonging therapy upon patients' arrival to the ICU and may benefit from early educational interventions, they are not consistently at the bedside within the first hours of admission. We chose a 72-hour period for recruitment knowing that it is a period of time when goals of therapy are frequently discussed during required initial family meetings with the ICU teams. Third, the knowledge assessment had only four questions. Additional items would demonstrate more nuanced differences in types of knowledge deficits between groups, for example, by more directly asking about level of functionality/discharge disposition after CPR, and types of complications.
Fourth, video can introduce bias depending on the perspective of those creating the video.23 To minimize this possibility, significant input was solicited from intensivists, ethicists, and palliative care providers. Fifth, our sample was mostly white, and well-educated. The results may not be generalizable to other groups and geographies. Finally, viewing a video does not guarantee harmonization between surrogate decision making and patient wishes; while it would be optimal for surrogates and patients to view a video about goals of therapy together, when patients are well, it is not always possible. Patients were followed until death or ICU discharge only; following patients and decisions over a longer period of time, i.e., 6 or 12 months, might have allowed us to explore the impact upon family decision making and on time to treatment withdrawal.
Now that we have demonstrated feasibility, acceptability, and effectiveness of the video decision support tool in the medical ICU, larger, randomized trials in medical and other ICUs (surgical, cardiac) will study the value of incorporation of the video into real-time clinical decision making, for further assessment of
impact upon decision making
variation by surrogate levels of experience
consistency and duration of surrogate choices over time
outcomes important to surrogates (e.g., satisfaction, emotional distress)
outcomes important to the health care system (e.g., use of nonbeneficial resources)
Using video to explore other important possibly life-prolonging therapeutic decision branch points (i.e., renal replacement therapy, tracheostomy, percutaneous endoscopic gastrostomy), and refining video content to include more contextual information (i.e., about critically ill end-stage cancer patients) may be helpful to surrogates and health care providers. Racial disparities have been observed in goals of therapy decision making in the ICU.24 Video decision support tools in the outpatient setting have been demonstrated to eliminate disparities in preferences, and can be explored in the ICU setting as well. In the future it will also be important to explore the impact of a video decision support tool over time upon communication practices in the ICU in general, among trainees, nurses, physicians, etc. – not only as it relates to end-of-life decision making. Finally, it will be important to determine which surrogate populations are most likely to benefit from the video medium and how the video may be used for critically ill patients making their own decisions.
Conclusion
A video decision support tool about CPR was successfully utilized in an adult MICU and demonstrated improvement in surrogate comprehension about CPR, and importantly, a high level of comfort with visual representation of CPR, paving the way for future use of this important communication method. The overall goal is to better educate surrogates, to empower them, and to improve their ability to participate in the shared decision making process and make more informed decisions, in keeping with the patient's values.
Acknowledgments
We would like to thank the clinical nurses of the medical ICU on Blake 7 at the Massachusetts General Hospital, whose support of this project was instrumental in its success.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Curtis JR. Vincent JL. Ethics and end-of-life care for adults in the intensive care unit. Lancet. 2010;376(9749):1347–1353. doi: 10.1016/S0140-6736(10)60143-2. [DOI] [PubMed] [Google Scholar]
- 2.Rocker G. Cook D. Sjokvist P. Weaver B. Finfer S. McDonald E, et al. Clinician predictions of intensive care unit mortality. Crit Care Med. 2004;32(5):1149–1154. doi: 10.1097/01.ccm.0000126402.51524.52. [DOI] [PubMed] [Google Scholar]
- 3.Curtis JR. Tonelli MR. Shared decision-making in the ICU: Value, challenges, and limitations. Am J Respir Crit Care Med. 2011;183(7):840–841. doi: 10.1164/rccm.201011-1836ED. [DOI] [PubMed] [Google Scholar]
- 4.White DB. Braddock CH., 3rd Bereknyei S. Curtis JR. Toward shared decision making at the end of life in intensive care units: Opportunities for improvement. Arch Intern Med. 2007;167(5):461–467. doi: 10.1001/archinte.167.5.461. [DOI] [PubMed] [Google Scholar]
- 5.Truog RD. Campbell ML. Curtis JR. Haas CE. Luce JM. Rubenfeld GD, et al. Recommendations for end-of-life care in the intensive care unit: A consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med. 2008;36(3):953–963. doi: 10.1097/CCM.0B013E3181659096. [DOI] [PubMed] [Google Scholar]
- 6.SUPPORT Principal Investigators: A controlled trial to improve care for seriously ill hospitalized patients: The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) JAMA. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- 7.Curtis JR. Nielsen EL. Treece PD. Downey L. Dotolo D. Shannon SE, et al. Effect of a quality-improvement intervention on end-of-life care in the intensive care unit: A randomized trial. Am J Respir Crit Care Med. 2011;183(3):348–355. doi: 10.1164/rccm.201006-1004OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daly BJ. Douglas SL. O'Toole E. Gordon NH. Hejal R. Peerless J, et al. Effectiveness trial of an intensive communication structure for families of long-stay ICU patients. Chest. 2010;138(6):1340–1348. doi: 10.1378/chest.10-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burns JP. Mello MM. Studdert DM. Puopolo AL. Truog RD. Brennan TA. Results of a clinical trial on care improvement for the critically ill. Crit Care Med. 2003;31(8):2107–2117. doi: 10.1097/01.CCM.0000069732.65524.72. [DOI] [PubMed] [Google Scholar]
- 10.Stacey D. Bennett CL. Barry MJ. Col NF. Eden KB. Holmes-Rovner M, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011;(10) doi: 10.1002/14651858.CD001431.pub3. CD001431. [DOI] [PubMed] [Google Scholar]
- 11.Volandes AE. Barry MJ. Chang Y. Paasche-Orlow MK. Improving decision making at the end of life with video images. Med Decis Making. 2010;30(1):29–34. doi: 10.1177/0272989X09341587. [DOI] [PubMed] [Google Scholar]
- 12.Volandes AE. Lehmann LS. Cook EF. Shaykevich S. Abbo ED. Gillick MR. Using video images of dementia in advance care planning. Arch Intern Med. 2007;167(8):828–833. doi: 10.1001/archinte.167.8.828. [DOI] [PubMed] [Google Scholar]
- 13.Volandes AE. Mitchell SL. Gillick MR. Chang Y. Paasche-Orlow MK. Using video images to improve the accuracy of surrogate decision-making: A randomized controlled trial. J Am Med Dir Assoc. 2009;10(8):575–580. doi: 10.1016/j.jamda.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volandes AE. Paasche-Orlow MK. Barry MJ. Gillick MR. Minaker KL. Chang Y, et al. Video decision support tool for advance care planning in dementia: Randomised controlled trial. BMJ. 2009;338:b2159. doi: 10.1136/bmj.b2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El-Jawahri A. Podgurski LM. Eichler AF. Plotkin SR. Temel JS. Mitchell SL, et al. Use of video to facilitate end-of-life discussions with patients with cancer: A randomized controlled trial. J Clin Oncol. 2010;28(2):305–310. doi: 10.1200/JCO.2009.24.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marco CA. Larkin GL. Cardiopulmonary resuscitation: Knowledge and opinions among the U.S. general public. State of the science-fiction. Resuscitation. 2008;79(3):490–498. doi: 10.1016/j.resuscitation.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 17.Gillick M. Volandes A. The psychology of using and creating video decision aids for advance care planning. In: Lynch TE, editor. Psychology of Decision Making in Medicine and Health Care. New York, NY: Nova Science Publishers; 2007. pp. 193–206. [Google Scholar]
- 18.Grant B. Sloniowski J. Documenting the Documentary: Close Readings of Documentary Film and Video. Detroit, MI: Wayne State University Press; 1998. [Google Scholar]
- 19.Volandes A. El-Jawahri A. Improving CPR decision-making for patients and families with video decision aids. In: Doyle LJ, editor; Saltsman RA, editor. Cardiopulmonary Resuscitation: Procedures and Challenges. Nova Science Publishers; 2012. [Google Scholar]
- 20.Rodriguez RM. Navarrete E. Schwaber J. McKleroy W. Clouse A. Kerrigan SF, et al. A prospective study of primary surrogate decision makers' knowledge of intensive care. Crit Care Med. 2008;36(5):1633–1636. doi: 10.1097/CCM.0b013e31816a0784. [DOI] [PubMed] [Google Scholar]
- 21.Shalowitz DI. Garrett-Mayer E. Wendler D. The accuracy of surrogate decision makers: A systematic review. Arch Intern Med. 2006;166(5):493–497. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 22.Hasibeder WR. Does standardization of critical care work? Curr Opin Crit Care. 2010;16(5):493–498. doi: 10.1097/MCC.0b013e32833cb84a. [DOI] [PubMed] [Google Scholar]
- 23.Volandes AE. Barry MJ. Wood F. Elwyn G. Audio-video decision support for patients: The documentary genre as a basis for decision aids. Health Expect. 2011 doi: 10.1111/j.1369-7625.2011.00727.x. (Epub ahead of print.)aw. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muni S. Engelberg RA. Treece PD. Dotolo D. Curtis JR. The influence of race/ethnicity and socioeconomic status on end-of-life care in the ICU. Chest. 2011;139(5):1025–1033. doi: 10.1378/chest.10-3011. [DOI] [PMC free article] [PubMed] [Google Scholar]