Abstract
Background/Objectives
Self-reported physical activity (PA) has been linked to lower hip fracture and fall rates. The objective of this study was to determine the association between objectively measured PA, fractures and falls.
Design/Setting/Participants
2731 men (mean age 79 yrs) recruited at 6 US clinical sites into a longitudinal cohort study.
Measurements
Total and active energy expenditure (EE) and minutes per day spent in sedentary and moderate intensity activities were measured using the multi-sensor SenseWear Pro Armband (SWA)for at least 5 days. Energy expended at a metabolic equivalent (MET >3) was termed active EE. Incident non-spine fractures and falls were identified every 4 months.
Results
759 (28.2%) men fell at least once over 12 months of follow-up; 186 (6.8%) men experienced ≥1 fracture over an average follow-up of 3.5± 0.9 years.The association between PA and falling varied by age (p interaction=0.02). Men <age 80yrs, with the lowest active EE had a lower risk of falling (relative risk (RR) =0.75; p trend = 0.08)while men >80 yrs, with the lowest active EE had a higher risk of falling, RR=1.43, p trend=0.09. In multivariate models including health status, men in the lowest quintile of active EE had a significantly higher risk of fracture, hazard ratio (HR)=1.82 (95% confidence interval (CI) 1.10, 3.00), p trend=0.04. Men with less than 33 minutes/day of moderate activity had a 70% increased risk of fracture, HR=1.70(95% CI, 1.03, 2.80).
Conclusion
Age modifies the association between PA and falling. Interventions aimed at >30 minutes of moderate PA per day may reduce fracturesextending existing PA guidelines to the oldest old, the fastest growing proportion of those over age 65.
Keywords: Exercise, osteoporosis, population studies, falls, fractures, physical activity
INTRODUCTION
Falls and osteoporotic fractures are common among older adults: about 30% of community dwelling individuals fall at least once per year and 40% of these fallslead to injury1-4. Most fractures (>95%) occur because of a fall5and osteoporotic fractures, a major public health problem, results in morbidity, disability and reduced quality of life6. Given current demographic trends an increasing number of older men are at risk of falls and fractures.
A recent meta-analysis of the association between physical activity (PA) and hip fractures showed that moderate to vigorous activity was associated with a 45% (95% confidence interval (CI), 31-56%) lower risk of hip fracture among men and women 7. However, women comprised 79% of the subjects in the meta-analysis suggesting that studies in men were underpowered with imprecise estimates. Few epidemiological studies have examined the association of PA and other fractures, which account for 80% of the total fracture burden and results are inconclusive8.
Observational studies have also generally reported equivocal results about the association between usual PA and risk of falling, but some data suggest higher risk among the most active and least active, a so called U-shaped relationship 9-12. Two recent meta-analyses 11, 12 of randomized clinical trials of exercise programs and falls suggested that exercise may reduce falls, especially interventions that include balance exercises and a higher total dose of exercise13, 14. Interventions that included a walking program were associated with higher risk of falls than interventions without a walking program.
Most of these previous studies relied on self-report of PA via questionnaires which includeda limited number of select activities typically sports and leisure time activities12. Lower intensity activities and unstructured activities, which account for the majority of total energy expenditure (EE)15,are more difficult to quantify by self-report. In addition, self-report is subject to recall bias and typically overestimates actual amounts of PA16, 17. These limitations are exacerbated when assessing PA of older adults who are more likely to engage in PA on an irregular basis 18, 19.
The purpose of the current study was to determine the association of total and active EE and time spent in sedentary and moderate activities, all measured objectively, with incident falls and fractures in a large community based cohort of older men. We explored whether the association between activity and falls and fractures was linear or “U”shaped.
METHODS
Study Sample
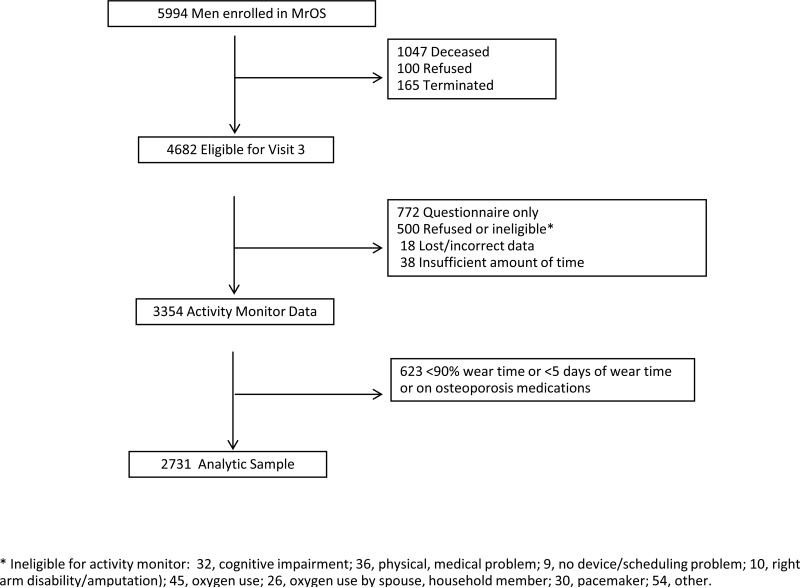
In 2000-2002, 5994 men enrolled in the Osteoporotic Fractures in Men Study (MrOS),a longitudinal cohort study designed to determine risk factors for osteoporosis, fractures and falls in six US clinical centers (Birmingham, AL; Minneapolis, MN; Palo alto, CA; Monongahela Valley nearPittsburgh, PA; Portland, OR and San Diego, CA). Men were recruited primarily through mass mailings targeted to age-eligible men. The MrOS study has been described in more detail previously 20. Briefly, all men were > age 65, able to walk independently and did not report bilateral hip replacements; 35% of men were age 65-69 and 11%, age 80 or older at baseline. Eleven percent of men were minorities; most rated their health as good to excellent and the mean (range) body mass index (BMI) was 26.9 kg/m2 (17-56) at the baseline visit.Men attended a baseline visit in 2000-02 and follow-up visit 4.5 years later.All activemen were then invited to a third visit in 2007-2009; of 4682 active men, 3354 (72%) wore an activity monitor, (Appendix, Figure 1). For this analysis we excluded 623 men who either reported use of an osteoporosis medication (e.g., bisphosphonates) at the third visit or who wore the activity monitor<90% of the prescribed time or for less than 5 days. The final analytical sample included 2,731 men. Written informed consent was obtained from each participant and the protocol was approved by the institutional review boards at each institution.
Objective Energy Expenditure and Physical Activity Assessment
Men were instructed to wear the multi-sensor SenseWear Pro Armband (SWA) (Body Media, Inc; Pittsburgh, PA) at all times, including while sleeping, for a typical 7 day period and to remove it only for brief periods for bathing and water activities. The armband was worn over the right triceps muscle, and data were sampled in 1 minute epochs from a heat flux sensor, a galvanic skin response sensor, a skin temperature sensor, a near body temperature sensor and bi-axial accelerometer. These data served as inputs in proprietary algorithms (Innerview Professional 5.1 software, Body Media, Inc; Pittsburgh, PA) along with height, weight, handedness and smoking status to estimate total EE in kilocalories per day (kcal/d). Energy expended at a moderate or greater intensity level was termed active EE. Minutes per day spent in sedentary (MET ≤1.5), moderate (METs 3-<6) and vigorous (METs >6) intensity activities were quantified. A validation study comparing the SenseWear Pro Armband with the criterion method of doubly labeled water showed acceptable levels of agreement for total EE and active EE in older adults 21.
Other Measurements
At the third clinic visit, weight was measured in light clothing without shoes and height by a Harpenden Stadiometer; BMI was computed as a kg/m2. Demographic, medical history, general health status, smoking and alcohol consumption were obtained from standardized questionnaires. History of fractures includes fractures before baseline (2000-2002) and all incident adjudicated fractures up to visit 3. Self-reported PA was assessed using the Physical Activity Scale for the Elderly (PASE) 22. Gait speed was measured in meters/seconds on a standard 6 m course. Self-report of a physician diagnosed cardiovascular disease (CVD), hypertension, diabetes, chronic obstructive pulmonary disease (COPD), Alzheimer's disease, Parkinson's, kidney or liver disease and non-skin cancers were recorded. We examined the prevalence of more than 1 of these comorbidities across physical activity quintiles. Participants also completed the Teng Modified Mini-Mental State (3MS) examination 23.
Bone Density Measurements
Total hip bone mineral density (BMD) (g/cm2) was measured at visit 3 using fan-beam DXA (QDR 4500W, Hologic Inc., Waltham, MA, USA) 20. A central quality-control lab, certification of DXA operators, and standardized procedures for scanning phantoms and participants were used to ensure reproducibility of DXA measurements.
Follow-up and Outcome Ascertainment
Fracture and fall events were reported by participants at 4 month intervals on brief mailed questionnaires. Participants were asked if they had fallen in the past 4 months; if so, the number of times they had sustained a fall and whether any fractures occurred over the 4 months was recorded. Subsequently, study physicians centrally adjudicated reported fractures from medical records. Deaths were confirmed with death certificates, 95% of these contacts were completed. The average follow-up for fractures was 3.5 ±0.9 years. For falls, we limited analyses to one year after the third clinic visit.
Statistical Analyses
The primary PA variables included total EE (kcal/d), active EE (kcal/d) and minutes per day spent in sedentary and moderate intensity activities. PAvariables were divided into quintiles. Differences in visit 3 characteristics across quintiles of total EE were tested using ANOVA or chi-square tests. We calculated the percentage of men with at least one fall across quintiles of PA. Negative binomial regression was used in the falls models to account for interdependence of recurrent events and estimated the relative risk (RR) 95% CI of falling versus no falls. Age-adjusted incidence rates of fracture per 1000 person years were calculated across quintiles of PA. Cox proportional hazards regression models were used to calculate the hazard ratio (HR) (95% CI) across quintiles of PA. The top quintile formed the referent group for all analyses with tests for trend across quintiles.
Base models for falls and fractures included age, race, clinic and season. Multivariate (MV) models for falls included the base model plus height, weight, self-reported history of diabetes, health status (good, excellent versus fair, poor, very poor), and smoking (current versus past or never). Multivariate models for fractures also included total hip BMD and fracture history. In subsequent models, we added fall history (year before visit 3) to the models to test whether history of falls attenuates the association between PA and fractures. We hypothesized that the association between PA and falls and fractures could differ by age and we ran separate models for the young old (<80) and the oldest old (≥80) and tested for an interaction. To test for the so called “U” shaped relationship9-12, we used quintile 3 as the referent and also ran a continuous model adding in a quadratic term but there was no evidence of a U-shaped relationship for either outcome(data not shown).All analyses were conducted using SAS version 9.1 (SAS Institute, Inc. Cary, North Carolina).
RESULTS
Men with the highest total EE (>2683 kcal/day) were on average 7 years younger, more likely to be White, weighed about 17kgs more, had a faster gait speed and higher BMD and lean mass than men with lowest total EE (<1975kcal/day), Table 1. The most active men were also less likely to report diabetes or a previous fracture and more likely to report excellent/very good health status. The overall prevalence of current smoking was low but was slightly higher among the men with the lowest total EE. The differences in alcohol consumption across total EE quintiles, while statistically significant, were modest. Overall the prevalence of more than 1 comorbidity was high but decreased with increasing total EE. The most active men also had the highest cognitive function. Physical activity by self-report increased across quintiles of total EE. The proportion of active EE to total EE was higher among the most active men. The most active men (quintile 5) averaged of 154 minutes per day of moderate activity compared to 35 minutes per day among the least active.
Table 1.
Characteristics of men in the total population and across quintiles of total energy expenditure (EE)with tests for linear trend.
| Total EE Expenditure (kcal/d) |
|||||||
|---|---|---|---|---|---|---|---|
| All Subjects N=2731 | Q1 (<1944.4) | Q2 (1944.4 - 2162.0) | Q3 (2162.0 - <2377.2) | Q4 (2377.2 - 2661.2) | Q5 (>2661.2) | p-trend | |
| Age (years), mean (+/- SD) | 78.9 (5.1) | 82.8 (5.4) | 80.1 (5.0) | 78.4 (4.4) | 77.0 (4.0) | 76.2 (3.6) | <0.001 |
| White, n (%) | 2468 (90.4) | 468 (85.7) | 489 (89.7) | 497 (90.9) | 509 (93.2) | 505 (92.3) | <0.001 |
| BMI (kg/m2), mean (+/- SD) | 27.2 (3.7) | 25.4 (3.1) | 26.8 (3.4) | 27.3 (3.5) | 27.9 (3.9) | 28.4 (3.9) | <0.001 |
| Weight (kg), mean (+/- SD) | 82.0 (13.1) | 71.9 (9.5) | 79.6 (10.3) | 82.5 (11.5) | 85.5 (13.2) | 89.3 (13.4) | <0.001 |
| Height (cm), mean (+/- SD) | 173.6 (6.8) | 168.3 (5.3) | 172.2 (5.7) | 173.8 (5.9) | 176.2 (6.4) | 177.3 (6.7) | <0.001 |
| Total hip BMD, mean (+/- SD) | 0.95 (0.14) | 0.88 (0.14) | 0.94 (0.13) | 0.96 (0.14) | 0.97 (0.13) | 1.00 (0.14) | <0.001 |
| Alcohol (drinks/wk) | 2.9 (1.3) | 2.8 (1.3) | 2.8 (1.2) | 3.0 (1.2) | 3.0 (1.2) | 3.0 (1.3) | <0.01 |
| Gait speed (m/s) | 1.14 (0.23) | 1.1 (0.2) | 1.1 (0.2) | 1.2 (0.2) | 1.2 (0.2) | 1.2 (0.2) | <0.001 |
| Total body lean mass (kg) | 55.9 (7.1) | 49.2 (4.9) | 54.0 (5.3) | 56.0 (5.7) | 58.7 (6.4) | 61.1 (6.8) | <0.001 |
| Appendicular lean mass (kg) | 23.6 (3.4) | 20.4 (2.3) | 22.6 (2.5) | 23.6 (2.7) | 25.0 (3.1) | 26.1 (3.3) | <0.001 |
| Diabetes, n (%) | 416 (15.2) | 91 (16.7) | 105 (19.3) | 81 (14.8) | 74 (13.6) | 65 (11.9) | <0.01 |
| Fracture history, n (%) | 718 (26.4) | 153 (28.0) | 156 (28.6) | 149 (27.4) | 128 (23.6) | 132 (24.2) | 0.03 |
| Comorbidities* (1+), n (%) | 2173 (79.6) | 469 (85.9) | 445 (81.7) | 419 (76.6) | 439 (80.4) | 401 (73.3) | <0.001 |
| Teng 3MS (0-100), mean (+/- SD) | 97.2 (6.0) | 90.1 (8.0) | 92.1 (6.2) | 93.5 (5.1) | 94.0 (4.3) | 93.9 (5.0) | <0.001 |
| Smoke, n (%) | 51 (1.9) | 13 (2.4) | 12 (2.2) | 9 (1.7) | 8 (1.5) | 9 (1.7) | 0.23 |
| Health status, n (%) | |||||||
| Excellent/Very good | 2394 (87.8) | 434 (79.6) | 464 (85.3) | 488 (89.4) | 497 (91.0) | 511 (93.4) | <0.001 |
| PASE score, mean (+/-SD) | 135.9 (67.2) | 99.7 (60.0) | 123.8 (61.5) | 142.6 (61.7) | 147.6 (66.8) | 165.7 (67.0) | <0.001 |
| Active EE (kcal/d) , mean (+/-SD) | 500.8 (380.5) | 171.0 (116.9) | 286.3 (144.2) | 436.5 (193.7) | 581.4 (229.2) | 1027.5 (395.5) | <0.001 |
| Minutes (m/d) , mean (+/-SD) | |||||||
| Sedentary activity | 1235.4 (92.6) | 1305.4 (58.6) | 1278.2 (60.7) | 1244.5 (68.3) | 1214.7 (74.1) | 1134.2 (90.3) | <0.001 |
| Moderate activity | 82.6 (59.8) | 35.3 (25.5) | 53.0 (31.0) | 75.9 (39.2) | 94.5 (44.5) | 154.2 (66.1) | <0.001 |
| Vigorous activity | 10.8 (12.7) | 4.2 (5.0) | 6.3 (6.3) | 9.4 (8.6) | 12.5 (11.5) | 21.6 (18.6) | <0.001 |
Self-report of a physician diagnosed cardiovascular disease, hypertension, diabetes, chronic obstructive pulmonary disease, Alzheimer's disease, Parkinson's disease, kidney or liver disease and non-skin cancers.
Falls
A total of 759 (28.2%) men fell at least once over 12 months of follow-up Total EE and active EE were lower in men who fell compared to men who did not fall, during the 1 year of follow-up, Table 2. There was a linear decline in physical activity with increasing number of falls. The amount of sedentary activity increased with increasing fall risk. Nevertheless, the absolute differences in PA by fall status, while statistically significant, were small.
Table 2.
Objective energy expenditure and physical activity by fallsand non-spine fracture status.
| NoFalls (n=1937) | 1 Fall (n=379) | 2 or more Falls (n=380) | p-value | p-trend | |
|---|---|---|---|---|---|
| Total EE (Kcal/d) | |||||
| Mean (SD) | 2365.7 (427.0) | 2346.3 (434.8) | 2304.0 (445.5) | < 0.01 | 0.01 |
| Median | 2323.2 | 2286.2 | 2228.3 | ||
| Active EE (Kcal/d) | |||||
| Mean (SD) | 513.2 (380.4) | 504.8 (390.6) | 453.9 (371.4) | < 0.01 | 0.01 |
| Median | 419.4 | 392.4 | 360.2 | ||
| Sedentary (min/day) | |||||
| Mean (SD) | 1231.7 (91.9) | 1236.3 (93.5) | 1246.9 (94.3) | < 0.05 | 0.01 |
| Median | 1245.6 | 1246 | 1259.8 | ||
| Moderate (min/day) | |||||
| Mean (SD) | 84.4 (59.8) | 83.9 (61.5) | 75.0 (58.3) | < 0.01 | 0.05 |
| Median | 71.6 | 69.2 | 62.5 |
| Fracture | |||
|---|---|---|---|
| NO (n=2545) | YES (n=186) | p-value | |
| Total EE (Kcal/d) | |||
| Mean (SD) | 2356.6 (433.6) | 2270.8 (400.3) | 0.01 |
| Median | 2310.8 | 2170.3 | |
| Active EE (Kcal/d) | |||
| Mean (SD) | 506.3 (383.4) | 425.7 (330.4) | 0.002 |
| Median | 411.4 | 328.3 | |
| Sedentary (min/day) | |||
| Mean (SD) | 1234.2 (92.8) | 1250.9 (88.5) | 0.02 |
| Median | 1246.8 | 1264.4 | |
| Moderate (min/day) | |||
| Mean (SD) | 83.3 (60.1) | 72.5 (55.0) | 0.02 |
| Median | 70 | 59.8 | |
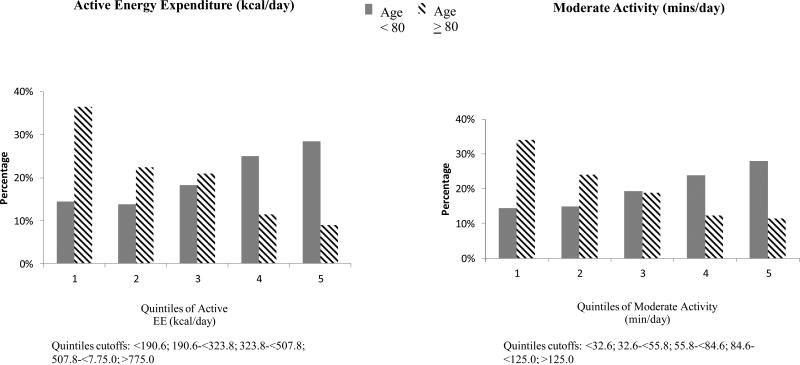
Significant interactions were observed between objective measures of PA and age for prediction of falls (Figure 1). Among men <80 years, the proportion of men who fell at least once was almost 3 times higher among men with the most active EE or the greatest number of minutes per day of moderate activity minutes compared with the lowest activity. In contrast, among men ≥ age 80, the proportion of men who fell was highest among men in the lowest quintile of active EE and moderate activity minutes.
Figure 1.
Proportion of men who fell at least once over 12 months of follow-up stratified by age, < 80 years and men ≥ 80 years.
In the MV models of active EE, men younger than 80 years with the lower active EE had a 25-47% lower risk of falling (p trend=0.08)compared to the most active men, Table 3. Similar results were observed for moderate activity. In contrast, among men≥80 years, men with the lowest active EE had a 43% higher risk of falling, RR=1.43(0.90, 2.26), (p trend= 0.09, p interaction=0.02). Men less than 80 years with the least amount of sedentary activity had a 29% (0.84, 1.99) higher risk of falling compared to men with the most sedentary activity, (p trend=0.10). In contrast, men ≥age 80with the least amount of sedentary activity were about 33% (0.42, 1.06) less likely to fall than men who were the mostsedentary (ptrend=0.09, p interaction p=0.01.
Table 3.
Relative Risk (RR) of falling across quintiles of objective physical activity stratified by age.
| Age <80 | Age ≥80 | ||||||
|---|---|---|---|---|---|---|---|
| N (%) | RR1 (95% CI) | RR2 (95% CI) | N (%) | RR1 (95% CI) | RR2 (95% CI) | p-interaction | |
| Total EE (kcal/d) | |||||||
| Q1 (<1975.0) | 40 (10.0) | 1.04 (0.66, 1.64) | 0.78 (0.44, 1.37) | 134 (37.3) | 1.07 (0.63, 1.83) | 1.24 (0.70, 2.21) | 0.50 |
| Q2 (1975.0 - <2201.6) | 64 (16.0) | 0.87 (0.59, 1.26) | 0.71 (0.47, 1.09) | 100 (27.9) | 1.17 (0.69, 1.99) | 1.30 (0.75, 2.25) | |
| Q3 (2201.6 - <2407.4) | 77 (19.3) | 0.66 (0.47, 0.94) | 0.57 (0.40, 0.80) | 60 (16.7) | 0.81 (0.47, 1.40) | 0.92 (0.52, 1.61) | |
| Q4 (2407.4 - <2683.2) | 93 (23.3) | 0.69 (0.50, 0.95) | 0.65 (0.47, 0.90) | 41 (11.4) | 1.11 (0.61, 2.00) | 1.07 (0.60, 1.91) | |
| Q5 (>2683.2) | 126 (31.5) | Ref | Ref | 24 (6.7) | Ref | Ref | |
| P trend | 0.93 | 0.27 | 0.63 | 0.27 | |||
| Active EE (kcal/d) | |||||||
| Q1 (<190.6) | 58 (14.5) | 0.94 (0.62, 1.41) | 0.75 (0.48, 1.19) | 131 (36.5) | 1.67 (1.05, 2.65) | 1.43 (0.90, 2.26) | 0.02 |
| Q2 (190.6 - <323.8) | 55 (13.8) | 0.63 (0.41, 0.96) | 0.53 (0.36, 0.79) | 80 (22.3) | 1.13 (0.69, 1.85) | 1.11 (0.68, 1.79) | |
| Q3 (323.8 - <507.8) | 73 (18.3) | 0.70 (0.49, 1.01) | 0.63 (0.44, 0.90) | 75 (20.9) | 1.10 (0.68, 1.79) | 1.12 (0.69, 1.82) | |
| Q4 (507.8 - <775.0) | 100 (25.0) | 0.70 (0.51, 0.97) | 0.66 (0.48, 0.92) | 41 (11.4) | 0.97 (0.56, 1.69) | 1.00 (0.58, 1.70) | |
| Q5 (>775.0) | 114 (28.5) | Ref | Ref | 32 (8.9) | Ref | Ref | |
| P trend | 0.42 | 0.08 | 0.01 | 0.09 | |||
| Sedentary activity (mins/day) | |||||||
| Q1 (>1159.8) | 107 (26.7) | 1.09 (0.73, 1.63) | 1.29 (0.84, 1.99) | 36 (10.0) | 0.56 (0.35, 0.88) | 0.67 (0.42, 1.06) | 0.01 |
| Q2 (1159.8 - <1224.8) | 94 (23.5) | 0.95 (0.63, 1.43) | 1.08 (0.69, 1.68) | 44 (12.3) | 0.62 (0.41, 0.95) | 0.78 (0.51, 1.18) | |
| Q3 (1224.8 - <1269.8) | 72 (18.0) | 0.95 (0.62, 1.44) | 0.98 (0.63, 1.52) | 84 (23.4) | 0.70 (0.49, 1.01) | 0.85 (0.59, 1.22) | |
| Q4 (1269.8 - <1314.0) | 62 (15.2) | 0.75 (0.49, 1.17) | 0.81 (0.52, 1.28) | 82 (22.8) | 0.78 (0.55, 1.13) | 0.87 (0.60, 1.24) | |
| Q5 (>1314.0) | 65 (16.3) | Ref | Ref | 113 (31.5) | Ref | Ref | |
| P trend | 0.36 | 0.10 | 0.005 | 0.08 | |||
| Moderate activity (mins/day) | |||||||
| Q1 (<32.6) | 57 (14.3) | 0.93 (0.62, 1.40) | 0.76 (0.48, 1.20) | 122 (34.0) | 1.83 (1.21, 2.79) | 1.54 (0.99, 2.39) | 0.01 |
| Q2 (32.6 - <55.8) | 59 (14.8) | 0.68 (0.46, 1.01) | 0.59 (0.40, 0.87) | 86 (24.0) | 1.23 (0.80, 1.91) | 1.18 (0.77, 1.83) | |
| Q3 (55.8 - <84.6) | 77 (19.3) | 0.77 (0.54, 1.11) | 0.68 (0.48, 0.98) | 67 (18.7) | 1.17 (0.74, 1.84) | 1.15 (0.73, 1.82) | |
| Q4 (84.6 - <125.0) | 95 (23.8) | 0.81 (0.58, 1.14) | 0.79 (0.56, 1.10) | 44 (12.3) | 1.08 (0.64, 1.82) | 1.13 (0.69, 1.86) | |
| Q5 (>125.0) | 112 (28.0) | Ref | Ref | 40 (11.4) | Ref | Ref | |
| P trend | 0.42 | 0.10 | 0.003 | 0.06 | |||
RR1= Base model=Adjusted for age, race, clinic, season.
RR2= Multivariate model=Base model + health status, height, weight, smoking, diabetes.
Fractures
A total of 1861 (6.8%) men experienced ≥ 1 fracture over an average follow-up of 3.5 ± 0.9 years. Men who experienced an incident fracture had lower PA and greater sedentary activity than men without a fracture, Table 2. The greatest differences were observed for active EE and moderate intensity activities where the median was 25% and 17% lower, respectively among the men who experienced an incident fracture compared to men without a fracture.
Higher levels of total EE, active EE and moderate intensity activity were associated with lower rates of fracture while men with higher sedentary activity had a higher rate of fracture, Table 4. There was no evidence of an interaction of physical activity with age for fracture (data not shown). The hazard ratio for fractures was higher among men with the least amount of total EE. Similar results were observed for active EE where men with less than 190.6 kcal/day of active EE had an 82% increased risk of fracture compared to the men with the greatest active EE (>775kcal/d), HR=1.82 (1.10, 3.00), p trend=0.04. Men with the least sedentary activity had a lower fracture risk but this association was slightly attenuated in the MV models, p trend=0.09. Participating in less than 33 minutes of moderate activity (quintile 1) was associated with a 70% increased risk of fracture compared to most active men. Individuals who have a history of falls may adjust their physical activity because of a fear of falling but adding fall history to our fracture models had no effect (data not shown).
Table 4.
Incidence rate(per 1000 person yrs). (95% confidence interval) and hazard ratio (95% confidence interval (CI)) of non-spine fractures across quintiles of objective physical activity.
| Incidence Rate (95% CI) | Base Model HR (95% CI) | MV Model HR (95% CI) | |
|---|---|---|---|
| Total EE (kcal/d) per 1SD increase HR=0.86 (0.72, 1.02) p=0.08 | |||
| Q1 (<1975.0) | 20.2 (12.9, 27.6) | 1.59 (0.96, 2.62) | 1.71 (0.94, 3.11) |
| Q2 (1975.0 - <2201.6) | 24.8 (17.5, 32.3) | 1.56 (0.97, 2.52) | 1.70 (1.01, 2.85) |
| Q3 (2201.6 - <2407.4) | 12.7 (7.8, 17.6) | 0.84 (0.49, 1.42) | 0.90 (0.52, 1.56) |
| Q4 (2407.4 - <2683.2) | 15.9 (9.1, 22.7) | 0.99 (0.60, 1.65) | 1.00 (0.59, 1.68) |
| Q5 (≥2683.2) | 16.1 (8.7, 23.4) | Ref | Ref |
| P trend | --- | 0.02 | 0.02 |
| Active EE (kcal/d) per 1SD increase HR=0.80 (0.67, 0.96) p=0.02 | |||
| Q1 (<190.6) | 29.1 (20.1, 38.0) | 2.11 (1.31, 3.40) | 1.82 (1.10, 3.00) |
| Q2 (190.6 - <323.8) | 16.2 (10.5, 22.0) | 1.16 (0.69, 1.93) | 1.02 (0.60, 1.72) |
| Q3 (323.8 - <507.8) | 16.6 (10.8, 22.4) | 1.10 (0.66, 1.85) | 1.04 (0.62, 1.76) |
| Q4 (507.8 - <775.0) | 16.1 (10.6, 21.5) | 1.25 (0.76, 2.06) | 1.20 (0.72, 2.00) |
| Q5 (≥775.0) | 18.0 (8.6, 27.5) | Ref | Ref |
| P trend | --- | 0.004 | 0.04 |
| Sedentary activity (min/d) per 1SD increase HR=1.20 (1.02, 1.42) p=0.03 | |||
| Q1 (<1159.8) | 15.7 (9.5, 21.8) | 0.64 (0.40, 1.04) | 0.72 (0.43, 1.20) |
| Q2 (1159.8 - <1224.8) | 14.1 (8.7, 19.4) | 0.58 (0.36, 0.94) | 0.65 (0.39, 1.08) |
| Q3 (1224.8 - <1269.8) | 20.4 (13.7, 27.4) | 0.76 (0.49, 1.17) | 0.83 (0.53, 1.30) |
| Q4 (1269.8 - <1314.0) | 20.9 (14.0, 27.7) | 0.82 (0.54, 1.26) | 0.93 (0.60, 1.42) |
| Q5 (≥1314.0) | 23.2 (16.0, 30.4) | Ref | Ref |
| P trend | --- | 0.02 | 0.09 |
| Moderate activity (min/d) per 1SD increase HR=0.83 (0.70, 0.98) p=0.03 | |||
| Q1 (<32.6) | 27.3 (19.2, 35.4) | 1.84 (1.15, 2.92) | 1.70(1.03, 2.80) |
| Q2 (32.6 - <55.8) | 14.9 (9.6, 20.3) | 1.05 (0.63, 1.75) | 0.96 (0.56, 1.62) |
| Q3 (55.8 - <84.6) | 21.0 (14.4, 27.6) | 1.29 (0.80, 2.09) | 1.25 (0.76, 2.04) |
| Q4 (84.6 - <125.0) | 14.7 (9.3, 20.1) | 1.02 (0.61, 1.69) | 1.01 (0.60, 1.70) |
| Q5 (≥125.0) | 18.3 (9.2, 27.4) | Ref | Ref |
| P trend | --- | 0.01 | 0.07 |
Base model=Adjusted for age, race, clinic, season. Ref=referent.
Multivariate model=Base model + health status, height, weight, smoking, diabetes, fracture history, BMD total hip.
DISCUSSION
Our prospective results demonstrated important interactions between age and PA for fall risk whereby the oldest old men (≥ age 80) were at a greater risk of falling at lower activity levels and higher sedentary activity. The opposite was true for the men< age of 80 yrs. These associations were consistent across all of the activity variables and were independent of important confounding variables. The higher risk of falling among the younger men at greater levels of activity may reflect greater exposure to higher fall risk circumstances. Physical activities may displace the body's center of gravity and balance predisposing one to a fall. This acute risk of a fall during physical activity appears to be greatest in the young old. On the other hand, the greater risk of falling among oldest men at lower physical activity levels may reflect a combination of poor muscle strength and balance, functional impairment and poor health status which place them at a higher risk of falls. To our knowledge, no previous study identified this important interaction with age and fall risk. However, our results are consistent with a previous randomized clinical trial which showed that among individuals with poor baseline physical function (e.g., perhaps older individuals), the risk of falls decreased for exercise participants. But, among those with better baseline physical function (e.g., perhaps younger individuals), the exercise intervention led to an increased risk of falling 24.
Our results suggest that fall prevention strategies aimed at reducing the incidence of falls need to take into consideration the age of the patient. Among the young-old, care must be taken to select physical activities that do not expose individuals to a higher risk of falls. For the oldest old, interventions aimed at increasing active EE or time spent in moderate activities >30 minutes a day may reduce fall risk.
For fractures, we found no evidence of an interaction with age suggesting that although more active younger men fall more, there was no increase in fractures. Among the total population, men with the lowest levels of total EE, active EE and moderate activity were at a 70-80% increased risk of fracture, independent of age, BMD, fall history, health status, body weight and other important variables. The observation that total EE was important suggests that any EE may help to lower fracture risks. Most previous studies typically quantified leisure time or recreational activities which ignore large components of total EE. For approximately every 400 kcal/d increase inactive EE there was about a 20% lower risk of fracture. These results are novel and important since our population of men was considerably older than men from other prospective studies
Our results suggest that active EE of approximately 200 kcal/day or 30 minutes of moderate activity may reduce the risk of fracture. These results lend further support to federal exercise guidelines that endorse moderate intensity activities for at least 30 minutes on most days or preferably all days of the week 26. Evidence of the applicability of these guidelines to the oldest old is sparse but important given their high prevalence of sedentary lifestyles. These activity levels are attainable in most older people. Activities such as walking 3 mph, bowling, golfing with a cart, vacuuming or car washing are all activities that meet this criteria and could be incorporated into older people's lifestyle.
Prospective studies have also examined physical “inactivity” defined as time spent reading, watching television or sitting and found that greater amounts of sedentary activity were associated with an increased risk of hip fracture 27, 28. Consistent with these observations, men with the least sedentary activity had about a 30% lower risk of fracture. Approximately each 90 minute increase in sedentary activity was associated with about a 20% increase in fracture.
Our study is limited by its observational design. Randomized clinical trials provide the strongest evidence about the causal relationship between an exposure e.g., PA and fracture risk. The Lifestyle Intervention and Independence for Elders (LIFE) Study is a phase 3 randomized trial of 1600 sedentary older persons followed for an average of 3.7 years 29. This study will test whether a supervised moderate intensity PA program reduces mobility disability and fall injuries but the study is not powered to show a decrease in fractures. A fracture trial would be cost-prohibitive, requiring a very large sample size and many years of follow-up. For example, to observe a 20% decrease in hip fracture risk, a 5 year trial would need to enroll about 35,000 men in each group 7. A. Bradford Hill summarized several criteria that guide the consideration of causality 30. The observation that increased PA reduces fracture risk meets several of these criteria: strength and dose response of the association (70-80% reduced risk); consistency across many different activity variables; temporal sequence of events (prospective design of our study) and biological plausibility (improved BMD, muscle strength, physical performance and balance).
The primary limitation of observational studies is the inability to balance confounding variables across activity groups. Health status is the most important confounder of the association between PA and fractures. “Healthier” individuals are more active because they chose to and because they are capable of participating. Indeed, a greater proportion of men who had the highest EE reported excellent/very good health status. Nevertheless, 80% of the least active men also reported very good to excellent health status. We adjusted for health status, age and other important confounding variables in our multivariate model and our results remained statistically significant.
There are a number of strengths to our study. We objectively measure PA using state of the art monitors in almost 3000 men with an average age of 79 years and followed these men for 3.5 years with 95% complete follow-up. We collected detailed information about potential confounders. There are, however, additional limitations. We studied a cohort of generally healthy men who were able to return for clinic visits and wear a activity monitor for a mean of 5 days. Therefore, our results may not be generalizable to sicker, older men or women. Hip fractures are the most devastating type of fracture and we were unable to examine hip fractures alone. However, non-spine fractures account for 80% of all osteoporotic fractures. A recent report from Norway showed stronger associations between leisure time and fractures at weight bearing sites 8 but we had too few fractures to stratify by weight bearing status. Because of our observational design, there could still be residual confounding by unmeasured factors. We assessed falls every 4 months and may have, therefore, underreported the true incidence of falls. Finally, more accurate recall of falls may vary by activity level. This could lead to misclassification of fall status and would tend to bias our results to the null.
In conclusion, age modifies the association between PA and falls. Higher activity places men <80 yrs at greater risk of falling but oldest old (≥80 yrs) men, at a lower risk of falling. Interventions to reduce falls need to be tailored for specific age groups. Men who maintained active EE >200 kcal/day or 30 min/day of moderate activity had a reduced risk of fracture. Our results extend existing PA guidelines to the oldest-old, the fastest growing proportion of those over age 65.
ACKNOWLEDGEMENT
Jane A. Cauley: Grants/Funds, NIH (NIAMS/NIA)
Stephanie L. Harrison: Employed by CPMC
Kristine E. Ensrud: Grants/Funds, NIH; Consultant, DMSB for Merck Sharpe & Dohme
Funding: The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR), and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140.
Sponsor's Role: None
Appendix
Appendix, Figure 1.
Footnotes
Author Contributions: JAC had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: JAC, Eric Orwoll, Dawn C. Mackey. Acquisition of data: Jane A. Cauley, SLH, Peggy M. Cawthon, Kristine E. Ensrud, Eric Orwoll. Analysis and interpretation of data: Jane A. Cauley, Stephanie L. Harrison, Peggy M. Cawthon, Michelle E. Danielson, Eric Orwoll, Dawn C. Mackey. Drafting of the manuscript: Jane A. Cauley. Critical revision of the manuscript for important intellectual content: Peggy M. Cawthon, Kristine E. Ensrud, Michelle E. Danielson, Eric Orwoll, Dawn C. Mackey. Statistical analysis: Jane A. Cauley, Stephanie L. Harrison, Dawn C. Mackey, Obtaining funding: Jane A. Cauley, Kristine E. Ensrud, Eric Orwoll. Administrative, technical or material support: Jane A. Cauley, Peggy M. Cawthon, Michelle E. Danielson, Eric Orwoll, Dawn C. Mackey.
Conflict of Interest: None of the authors have any conflicts to report.
REFERENCES
- 1.Rubenstein LZ. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age Ageing. 2006 Sep;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 2.Masud T, Morris RO. Epidemiology of falls. Age Ageing. 2001 Nov;30(Suppl 4):3–7. doi: 10.1093/ageing/30.suppl_4.3. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Kumar C. The patient who falls: “It's always a trade-off”. JAMA. 2010 Jan 20;303(3):258–66. doi: 10.1001/jama.2009.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Website. Falls Among Older Adults: An Overview. 2012 http://wwwcdcgov/HomeandRecreationalSafety/Falls/adultfallshtml Accessed March.
- 5.Grisso JA, Kelsey JL, Strom BL, et al. Risk factors for falls as a cause of hip fracture in women. The Northeast Hip Fracture Study Group. N Engl J Med. 1991 May 9;324(19):1326–31. doi: 10.1056/NEJM199105093241905. [DOI] [PubMed] [Google Scholar]
- 6.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002 May 18;359(9319):1761–7. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 7.Moayyeri A. The association between physical activity and osteoporotic fractures: a review of the evidence and implications for future research. Ann Epidemiol. 2008 Nov;18(11):827–35. doi: 10.1016/j.annepidem.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Morseth B, Ahmed LA, Bjornerem A, et al. Leisure time physical activity and risk of non-vertebral fracture in men and women aged 55 years and older: the Tromso Study. Eur J Epidemiol. 2012 Mar 4; doi: 10.1007/s10654-012-9665-y. [DOI] [PubMed] [Google Scholar]
- 9.Graafmans WC, Ooms ME, Hofstee HM, et al. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996 Jun 1;143(11):1129–36. doi: 10.1093/oxfordjournals.aje.a008690. [DOI] [PubMed] [Google Scholar]
- 10.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988 Dec 29;319(26):1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 11.O'Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993 Feb 1;137(3):342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 12.Gregg EW, Pereira MA, Caspersen CJ. Physical activity, falls, and fractures among older adults: a review of the epidemiologic evidence. J Am Geriatr Soc. 2000 Aug;48(8):883–93. doi: 10.1111/j.1532-5415.2000.tb06884.x. [DOI] [PubMed] [Google Scholar]
- 13.Sherrington C, Whitney JC, Lord SR, et al. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008 Dec;56(12):2234–43. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- 14.de Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BC. Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int. 2009 Dec;20(12):2111–25. doi: 10.1007/s00198-009-0938-6. [DOI] [PubMed] [Google Scholar]
- 15.Weller I, Corey P. The impact of excluding non-leisure energy expenditure on the relation between physical activity and mortality in women. Epidemiology. 1998 Nov;9(6):632–5. [PubMed] [Google Scholar]
- 16.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000 Jun;71(2 Suppl):S1–14. [PubMed] [Google Scholar]
- 17.Lichtman SW, Pisarska K, Berman ER, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992 Dec 31;327(27):1893–8. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- 18.Matthews CE. Physical activity in the United States measured by accelerometer: comment. Med Sci Sports Exerc. 2008 Jun;40(6):1188. doi: 10.1249/MSS.0b013e31817057da. author reply 9. [DOI] [PubMed] [Google Scholar]
- 19.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008 Jan;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 20.Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study--a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005 Oct;26(5):569–85. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Mackey DC, Manini TM, Schoeller DA, et al. Validation of an armband to measure daily energy expenditure in older adults. J Gerontol A Biol Sci Med Sci. 2011 Oct;66(10):1108–13. doi: 10.1093/gerona/glr101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993 Feb;46(2):153–62. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 23.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987 Aug;48(8):314–8. [PubMed] [Google Scholar]
- 24.Morgan RO, Virnig BA, Duque M, Abdel-Moty E, Devito CA. Low-intensity exercise and reduction of the risk for falls among at-risk elders. J Gerontol A Biol Sci Med Sci. 2004 Oct;59(10):1062–7. doi: 10.1093/gerona/59.10.m1062. [DOI] [PubMed] [Google Scholar]
- 25.Cawthon PM, Fullman RL, Marshall L, et al. Physical performance and risk of hip fractures in older men. J Bone Miner Res. 2008 Jul;23(7):1037–44. doi: 10.1359/JBMR.080227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007 Aug 28;116(9):1081–93. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 27.Gregg EW, Cauley JA, Seeley DG, Ensrud KE, Bauer DC. Physical activity and osteoporotic fracture risk in older women. Study of Osteoporotic Fractures Research Group. Ann Intern Med. 1998 Jul 15;129(2):81–8. doi: 10.7326/0003-4819-129-2-199807150-00002. [DOI] [PubMed] [Google Scholar]
- 28.Michaelsson K, Olofsson H, Jensevik K, et al. Leisure physical activity and the risk of fracture in men. PLoS Med. 2007 Jun;4(6):e199. doi: 10.1371/journal.pmed.0040199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fielding RA, Rejeski WJ, Blair S, et al. The Lifestyle Interventions and Independence for Elders Study: design and methods. J Gerontol A Biol Sci Med Sci. 2011 Nov;66(11):1226–37. doi: 10.1093/gerona/glr123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hill AB. Statistical Evidence and Inference. In: Press U, editor. Principles of Medical Statistics. Oxford; NY: 1971. pp. 309–23. [Google Scholar]