Abstract
BACKGROUND:
Submucosal myomas are associated with infertility and may be treated by hysteroscopic resection.
OBJECTIVE:
The aim of this retrospective study was to analyze 37 subfertile patients who unnderwent hysteroscopic myomectomy in a tertiary care center with particular regard to their postprocedure reproductive outcome.
MATERIALS AND METHODS:
The entire patient group (n = 37) underwent the procedure between March 2004 and March 2010. The submucosal myomas were type 0 (n = 27), type 1 (n = 8), and type 2 (n = 2). The mean myoma size was 2.1 cm; mean duration of the procedure was 54 mins and mean follow-up was 26 ± 10 months. 22 patients had one or more associated infertility factors.
RESULTS:
The complication rate was 5.4%. 11 patients (29.7%) conceived after the procedure. The pregnancy rate was better when myoma was the exclusive etiology of infertility (40%), when the myoma was completely intracavitary (33.3%), when the lesion was ≥ 30 mm in size (50%), and there were no associated intramural fibroids.
CONCLUSION:
Hysteroscopic myomectomy is a safe procedure to enhance fertility especially in cases with unexplained infertility.
KEY WORDS: Hysteroscopic myomectomy, infertility, myoma
INTRODUCTION
The association of subserous fibroids and intramural fibroids with infertility is controversial. But the role of submucous fibroids which are reported in 5%-18% of patients as a causal factor for infertility is likely. Submucous fibroids are postulated to cause menometrorrhagia, preterm delivery, postpartum hemorrhage, and puerperal infection.
In their submucosal location, myomas can be treated exclusively using surgical procedures and they may be accessible by operative hysteroscopy: The standard minimally invasive surgical approach. Though a large number of reports have been published on laparoscopic and laparotomic myomectomy, the studies available regarding hysteroscopic myomectomy are few in number by comparison. A few retrospective studies published in 1990s have demonstrated successful reproductive outcome after hysteroscopic removal of submucous myomas in infertile women. The aim of this retrospective study was to evaluate the subsequent fertility and outcome of pregnancy after hysteroscopic myomectomy according to (a) the characteristics of submucous fibroids and (b) association with intramural fibroids.
MATERIALS AND METHODS
The study was conducted in a tertiary care infertility center. The study was conducted during a period of 6 years from 2004 March to 2010 March. This was a retrospective cohort study.
In order to assess the other associated causes of infertility, patients were evaluated by follicular study, hormonal assessment, semen analysis, and laparoscopy. The details of subsequent fertility were obtained from hospital records and direct information from patients.
Inclusion criteria
All infertile patients with submucous fibroids confirmed on three-dimensional (3D) ultrasound.
Duration of infertility more than or equal to 12 months. Only those patients who had a follow-up of at least 12 months from the day of surgery were included.
Exclusion criteria
Azoospermia in male partner. Age of female partner more than 40 years.
Submucous fibroids were classified based on European Society of Gynaecological Endoscopy into type 0-whole of fibroid inside the uterine cavity. Type 1-less than 50% extension of submucous fibroid into myometrium. Type 2-more than 50% extension into myometrium.
A total of 48 patients had undergone hysteroscopic myomectomy during the study period. Of these, 37 patients who were subfertile and fulfilled our criteria were included.
In infertile patients, the duration of infertility ranged from 12 to 108 months, the mean duration being 42 months.
Surgical technique
Pre-operative treatment with leuprolide 3.75 mg once a month for 2 months were given in two cases when the size of fibroid was 4 cm. All myomectomies were performed under general anesthesia. In all 37 patients, resectoscope (26 Fr, Karl Storz, Tuttlingen, Germany) with a bipolar wire loop was used for the procedure with normal saline as distension medium. The intrauterine pressure was controlled by Hamou hysteromat, Karl Storz, Tuttlingen, Germany. Resection was carried out under video control from fundus to os using cutting current. For each patient, intra- and postoperative complications such as hemorrhage, perforation, or intravasation of fluid medium into circulation was recorded. The number of postoperative days spent in hospital was recorded. For 32 patients, simultaneous laparoscopy was performed. All these patients had a postoperative sonogram at the end of 3 months to evaluate the completion of the procedure. Five patients went in for IVF/ICSI, four had intrauterine insemination. Postoperative estrogen and progesterone was given in four patients, when the affected endometrial surface was too broad.
Statistical analysis
Fertility was analyzed according to the type of fibroids, size, number of myomas, associated intramural fibroids, associated factors contributing to infertility, and time to conception using SPSS software. Analysis was performed using Chi-square test and Chi-square test modified by Yates. A P value of 0.045 was regarded as the upper limit of significance.
RESULTS
The mean patient age was 32 years (range: 24 to 40 years). The mean duration of infertility was 42 months (range: 12 to 108 months). The mean follow-up was 26 ± 10 months. A total of 12 patients were symptomatic (32.43%). The most common symptoms were menorrhagia which was present in seven patients and dysmenorrhea/pelvic pain in five patients.
Of the 37 patients, simultaneous laparoscopy was performed in 32. The average time taken for the procedure was 54 mins (range: 20-180) including associated laparoscopy and the treatment of intraoperative complications. The average duration of hospital stay was 40 h.
Removal of subserous myoma was performed in 14 cases. All cases of intramural fibroids found close to endometrium or distorting endometrium as previously diagnosed by 3D or four-dimensional ultrasound and intramural fibroids more than 4 cm were resected by simultaneous laparoscopy performed in nine cases. Two of the patients with intramural myoma had undergone hysteroscopic myomectomy as part of pre in vitro fertilization (IVF) workup and intramural myomectomy was not performed in them. The size of intramural fibroids was 3 and 2.5 cm in these cases.
There were two complications in this series (5.4%). One patient had intraoperative hemorrhage which was controlled with intrauterine Foleys for 8 h and one pint of blood transfusion. Other patient had a uterine perforation which was managed laparoscopically. No complications with regard to fluid imbalance was noted.
A total of 11 patients conceived after hysteroscopic myomectomy, that is, 29.7%.
Analysis of fertility according to unifactorial or multifactorial infertility
Of the 37 patients, 22 had other factors contributing to infertility. Eleven had associated mild, moderate, or severe endometriosis. Endometriotic cystectomy or fulguration of deposits was done for them, three had polycystic ovaries which were punctured, two had associated male factor infertility, and three had tubal pathology. Tubal cannulation was done in one patient. Two had a combination of these factors.
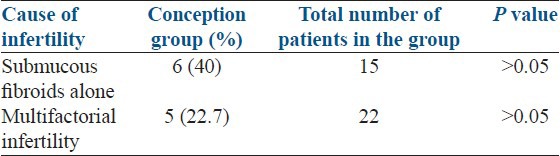
Among those with multifactorial infertility, 22.7% conceived. In contrast, in those with submucous fibroids with no other identifiable cause, 40% conceived. The value, though substantially higher than those with multifactorial infertility, was not statistically significant [Table 1].
Table 1.
Pregnancy outcome in patients according to associated infertility factors
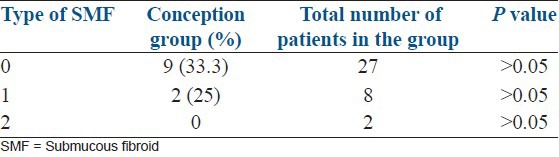
Analysis according to the type of submucus myoma
In our study population, 33.3% of patients with type 0 submucous fibroids conceived, while 25% of those with type 1 conceived. There were no pregnancies among those with type 2 fibroids [Table 2].
Table 2.
Pregnancy outcome according to the type of myomas
Fertility according to the number of submucous fibroids
Of the 37, 28 patients had only one, six had two submucous fibroids, and three patients had three submucous myomas. None of the patients with three or more submucous fibroids conceived. Of those with only one submucous fibroid, 32.1% conceived, while in those with two or more submucous myomas, only 22% conceived. Thus, conception varied inversely with the number of myomas, though this was not found to be statistically significant [Table 3].
Table 3.
Pregnancy outcome according to number and size of submucous fibroids
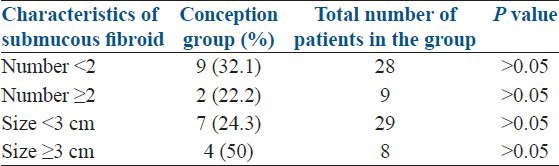
Fertility according to the size of submucous myomas
The mean number of myomas removed was 1.343 (range: 1-3). The average size of myoma removed was 2.1 cm. The diameter of the largest myoma was 4 cm.
In those with size less than 3 cm, 24.3% and those with fibroids moré than 3 cm, -50% conceived [Table 3]. Thus, it was found that removal of submucous fibroids more than 3 cm has a beneficial effect on fertility, though this was not statistically significant.
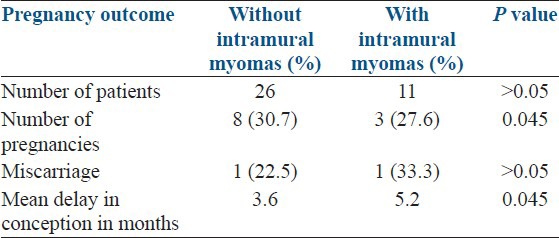
According to the presence of associated intramural fibroid
Eight out of the 26 patients with submucous myoma alone conceived, while among those with associated intramural fibroids, three patients conceived. The conception rate was higher in those without associated intramural myoma-30.7% when compared to those with associated intramural myoma-27.6% and this was found to be statistically significant P = 0.045.
Nine of the 11 patients with an intramural myoma had undergone a intramural myomectomy. In the remaining two patients, the size of intramural myoma was less than 4 cm and had undergone hysteroscopy as part of pre IVF workup and intramural myomectomy was not performed in them. Of the nine patients operated, there were three pregnancies, that is, 33.3%. No pregnancies occurred in the group which did not undergo intramural myomectomy. But due to the small size of the sample (n = 2), a comparison was not possible between the two groups.
The miscarriage rate was found to be much higher in patients with associated intramural myoma-33.3% versus those with no associated intramural myoma-12.5%. However, this was not found to be statistically significant Tab.
The mean time taken to conceive was increased significantly in those with intramural fibroids than those without intramural fibroid [Table 4].
Table 4.
Fertility according to the presence of associated intramural fibroids
Analysis according to primary or secondary infertility
Of the 37 patients analyzed, 23 had primary infertility and 14 had secondary infertility. Eight (34.7%) of those with primary infertility conceived, while three (21.42%) of those with secondary infertility conceived. This difference was not statistically significant.
DISCUSSION
In our experience, the pregnancy rate after hysteroscopic myomectomy in infertile patients was 29.7%. Little data are available about fertility after hysteroscopic myomectomy for submucous myoma. In a series of 13 infertile women by Corson and Brooks,[1,2] a pregnancy rate of 76.9% was observed after hysteroscopic myomectomy. The pregnancy rates after the procedure as reported by various studies have been described in Table 5.[3,4,5,6,7]
Table 5.
Summary of studies reporting on the reproductive outcome after hysteroscopic myomectomy
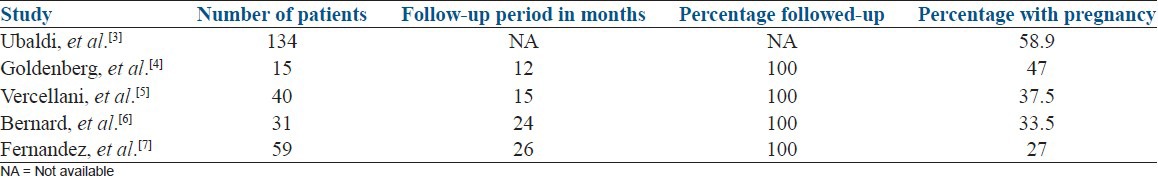
Many of these series report better results than those achieved in the present study. Nevertheless, the current results are similar to those reported in two studies, namely a pregnancy rate of 33.5% in 31 women (Bernard et al.[6]) and a rate of 28.7% in 14 women (Hucke et al.[8]). All these studies thus conclusively prove that submucous fibroids are associated with infertility and their removal considerably improves fertility.
Postoperative reproductive outcome is adversely affected by the presence of additional infertility factors. The pregnancy rate was 40% when the myoma was the only apparent cause, compared with 22.7% with the presence of additional factors.
Our results were further analyzed according to the type of fibroids. We found that the results are best with type 0 fibroids-33.3% and the rates drastically fell with increasing intramural extension. The reduction in fertility rates with increasing intramural extension was also reported in a study by Ioannis et al.,[9] It was a small study that looked at 25 patients. They found a fertility rate of 57.15% in type 0, 42.8% in type 1, and 25% in type 2 fibroids.
The initial size of the myoma also influenced the pregnancy rate. Paradoxically, in the current study, the rate was higher among those with larger myomas (≥30 mm). This observation is important; indeed, the large size of the myoma was in these cases the sole factor for infertility, and reinforced the fact that myomas could be a cause of infertility. Similar results were obtained in a myomectomy via laparotomy series (Sudik et al.[10]), while another group (Varasteh et al.[11]) reported similar findings when using hysteroscopy, with a cumulative pregnancy rate of 25% for myomas <20 mm and 75% for those >30 mm. These results offer indirect proof that large myomas are a valid cause of infertility, mainly because of the mechanical distortion and the dystrophy that they cause.
The study analyzed conceptions in patients undergoing hysteroscopic myomectomy with associated intramural fibroids. The pregnancy rate was significantly higher in those without associated intramural fibroids than those with intramural fibroids in our study even after their correction. Comparing those patients in whom intramural fibroids were left alone with those in whom they were corrected, we found that there were no conceptions in the uncorrected group. However, the sample size was too small (n = 2) to make any statistical inference.
In the current study, 75% of the pregnancies occurred during the 1st year, with a mean surgery to conception time span of 4 months. This short delay of conception has also been observed by others (Rosenfeld[12] ; Goldenberg et al.[4]). It is, therefore, strongly recommended that patients attempt to conceive soon after the procedure. The delay in conception was significantly higher in those with intramural fibroids. The study results of Gilles Bernard and Emile Darai also has similar results. They also found a statistically significant negative correlation of intramural myomas with term delivery rate and early conception after hysteroscopic myomectomy. The rate of miscarriage was found to be higher in patients with associated intramural fibroid when compared with those without intramural fibroid- 33.3% versus 12.5%. However, the difference was not statistically significant. This result is in accordance with those of Matsunaga and Shiota[13] which suggests that myomas increase the risk of miscarriage. The difference could not be due to cavity distortion as that was corrected by laparohysteroscopy. Therefore, the results reinforce the hypothesis that other mechanisms may contribute like endometrial atrophy, hyperplasia, vascular factors, and inflammation.[14] In fertile women, expression of molecular markers of endometrial receptivity HOXA11, leukemia-inhibiting factor, and basic transcriptional element-binding protein 1 rises during luteal phase with the peak occurring during implantation window. In a study by Shokrazadeh and Alizadeh,[15] endometrial levels of HOXA11, LIF, and BTEB1 m RNA were significantly reduced in infertile patients with uterine fibroid as compared with healthy fertile controls at the time of implantation. Other causes implicated are adhesion molecules,[16] epidermal growth factor,[17,18] insulin like growth factor,[19] and transforming growth factor present in fibroids. The effect of fibroids on miscarriage is controversial. Several authors have reported a decrease in miscarriage rate after myomectomy.[20] Several groups (Fahri et al.;[21] Eldar-Geva et al.;[22] Stovall et al.;[23] Rackow et al.[24]) have suggested that submucosal leiomyomas and fibroids distorting the endometrial cavity were associated with a reduction in the efficacy of assisted reproduction technique cycles due to reduced implantation and delivery rates (Pritts et al.[25]) (Home and Crithchley[26]) and that myomectomy should be completed prior to IVF cycles. Our results were also analyzed according to the type of infertility. In the present study, no difference in subsequent fertility was found between primary and secondary infertility.
CONCLUSIONS
Hysteroscopic myomectomy is a safe and an effective procedure which enhances fertility. Completely intracavitary myomas and absence of other contributing factors seem to be the best prognostic factors for further fertility. Removal of large myomas (more than 3 cm) has a much more beneficial effect on fertility than small ones. The mechanisms by which leiomyomas interfere with fertility are unclear, but presence of intramural myomas was found to impair delivery rate and fertility in our study. Since in the majority of patients in this series, intramural myomas which cause cavity distortion and large intramural myomas had been removed previously or by simultaneous laparoscopy, an independent assessment of their effect on fertility and pregnancy outcome was not possible. However, based on this study, removal of associated intramural myomas seems to be a wise option in patients undergoing hysteroscopic myomectomy who are desirous of childbearing.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Corson SL, Brooks PG. Resectoscopic myomectomy. Fertil Steril. 1991;55:1041–4. doi: 10.1016/s0015-0282(16)54349-0. [DOI] [PubMed] [Google Scholar]
- 2.Brooks PG, Loffer FD, Serden SP. Resectoscopic removal of symptomatic intrauterine lesions. J Reprod Med. 1989;34:435–7. [PubMed] [Google Scholar]
- 3.Ubaldi F, Tournaye H, Camus M, Van der Pas H, Gepts E, Devroey P. Fertility after hysteroscopic myomectomy. Hum Reprod Update. 1999;1:81–90. doi: 10.1093/humupd/1.1.81. [DOI] [PubMed] [Google Scholar]
- 4.Goldenberg M, Sivan E, Sharabi Z, Bider D, Rabinovici J, Seidman DS. Outcome of hysteroscopic resection of submucous myomas for infertility. Fertil Steril. 1995;64:714–6. doi: 10.1016/s0015-0282(16)57844-3. [DOI] [PubMed] [Google Scholar]
- 5.Vercellini P, Zàina B, Yaylayan L, Pisacreta A, De Giorgi O, Crosignani PG. Hysteroscopic myomectomy: Long term effects on menstrual pattern and fertility. Obstet Gynecol. 1999;94:341–7. doi: 10.1016/s0029-7844(99)00346-4. [DOI] [PubMed] [Google Scholar]
- 6.Bernard G, Darai E, Poncelet C, Benifla J-L, Madelenet P. Fertility after hysteroscopic myomectomy: Effect of intramural fibroids associated. Eur J Obstetr Gynaecol Reprod Biol. 2000;88:85–90. doi: 10.1016/s0301-2115(99)00123-2. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez H, Sefriou O, Virelizier C, Gervaise A, Gomel V, Frydman R. Hysteroscopic resection of submucosal myomas in patients with infertility. Hum Reprod. 2001;16:1489–92. doi: 10.1093/humrep/16.7.1489. [DOI] [PubMed] [Google Scholar]
- 8.Hucke J, Campo RL, De Bruvne F, Freikha AA. Hysteroscopic resection of submucous myoma. Geburtshilfe Frauenheilkd. 1992;52:214–8. doi: 10.1055/s-2007-1026132. [DOI] [PubMed] [Google Scholar]
- 9.Ioannis S, Aristotelis A, Antonios T, Panagiolis S, John B. Fertility rates after hysteroscopic rescection of submucous myomas depending on their type. Gynaecol Surg. 2006;3:206–10. [Google Scholar]
- 10.Sudik R, Husch K, Steller J, Daume E. Fertility and pregnancy outcome after myomectomy in sterility patients. Eur J Obstet Gynecol Reprod Biol. 1996;65:209–14. doi: 10.1016/0301-2115(95)02363-1. [DOI] [PubMed] [Google Scholar]
- 11.Varasteh NN, Neuwirth RS, Levin B, Kelly MD. Pregnancy rates after hysteroscopic polypectomy and myomectomy in infertile women. Obstet Gynecol. 1999;94:168–71. doi: 10.1016/s0029-7844(99)00278-1. [DOI] [PubMed] [Google Scholar]
- 12.Rosenfeld DL. Abdominal myomectomy for otherwise unexplained infertility. Fertil Steril. 1986;46:328–30. doi: 10.1016/s0015-0282(16)49536-1. [DOI] [PubMed] [Google Scholar]
- 13.Matsunaga E, Shiota K. Ectopic pregnancy and myoma uteri: Teratogenic effects and maternal characteristics. Teratology. 1980;21:61–9. doi: 10.1002/tera.1420210108. [DOI] [PubMed] [Google Scholar]
- 14.Deligdish L, Lowenthal M. Endometrial changes associated with myomata of the uterus. J Clin Pathol. 1970;23:676–80. doi: 10.1136/jcp.23.8.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shokrazadeh N, Alizadeh Z. Semi quantitative analysis of endometrial receptivity marker mRNA expression in the mid secretory endometrium of patients with uterine fibromas. Afr J Biotechnol. 2012;11:6220–5. [Google Scholar]
- 16.MacCalman CD, Furth EE, Omigbodun A, Bronner M, Coutifaris C, Strauss JF., 3rd Regulation expression of cadherin -11 in human epithelial cells: A role for cadherin-11 in trophoblast-endometrium interactions? Dev Dyn. 1996;206:201–11. doi: 10.1002/(SICI)1097-0177(199606)206:2<201::AID-AJA9>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 17.Hoffman GE, Rao V, Barrow GH, Sultz GE, Sanfillipo JS. Binding sites for epidermal growth factor in human uterine tissues and leiomyomas. J Clin Endocrinol Metabol. 1984;58:880–4. doi: 10.1210/jcem-58-5-880. [DOI] [PubMed] [Google Scholar]
- 18.Rein MS, Friedman AJ, Barber RL, Pavelka K, Fletcher JA, Morton CC. Cytogenetic abnormalities in uterine leiomyomata. Obstet Gynecol. 1991;97:1923–6. [PubMed] [Google Scholar]
- 19.Tommola P, Pekonen F, Rutanen EM. Binding of epidermal growth factor and insulin-like growth factor I in human myometrium and leiomyomata. Obstet Gynecol. 1989;74:658–62. [PubMed] [Google Scholar]
- 20.Verkauf BS. Myomectomy for fertility enhancement and preservation. Fertil Steril. 1992;58:1–15. doi: 10.1016/s0015-0282(16)55128-0. [DOI] [PubMed] [Google Scholar]
- 21.Farhi J, Ashkenazi J, Feldberg D, Dicker D, Orvieto R, Ben Rafael Z. Effect of uterine leiomyomata on the results of in-vitro fertilization treatment. Hum Reprod. 1995;10:2576–8. doi: 10.1093/oxfordjournals.humrep.a135748. [DOI] [PubMed] [Google Scholar]
- 22.Eldar-Geva T, Meagher S, Healy DL, MacLachlan V, Breheny S, Wood C. Effect of intramural, subserosal, and submucosal uterine fibroids on the outcome of assisted reproductive technology treatment. Fertil Steril. 1998;70:687–91. doi: 10.1016/s0015-0282(98)00265-9. [DOI] [PubMed] [Google Scholar]
- 23.Stovall DW, Parrish SB, Van Voorhis BJ, Hahn SJ, Sparks AE, Syrop CH. Uterine leiomyomas reduce the efficacy of assisted reproduction cycles: Results of a matched follow-up study. Hum Reprod. 1998;13:192–7. doi: 10.1093/humrep/13.1.192. [DOI] [PubMed] [Google Scholar]
- 24.Rackow BW, Arici A. Fibroids and in vitro fertilization: Which comes first? Curr Opin Obstet Gynecol. 2005;17:225–31. doi: 10.1097/01.gco.0000169097.52848.ee. [DOI] [PubMed] [Google Scholar]
- 25.Pritts EA, Parker WH, Olive DL. Fibroids and infertility: An updated systematic review of evidence. Fertil Steril. 2009;91:1215–23. doi: 10.1016/j.fertnstert.2008.01.051. [DOI] [PubMed] [Google Scholar]
- 26.Home AW, Critchley HO. The effects of uterine fibroids on embryo implantation. Semin Reprod Med. 2007;25:483–9. doi: 10.1055/s-2007-991046. [DOI] [PubMed] [Google Scholar]


