Abstract
Background:
In patients with craniovertebral junction (CVJ) anomalies, the respiratory system is adversely affected in many ways. The sub-clinical manifestations may get aggravated in the postoperative period owing to anesthetic or surgical reasons. However, there is limited data on the incidence of postoperative pulmonary complications (PPCs) and associated risk factors in such patients, who undergo transoral odontoidectomy (TOO) and posterior fixation (PF) in the same sitting.
Materials and Methods:
Five years data of 178 patients with CVJ anomaly who underwent TOO and PF in the same sitting were analyzed retrospectively. Preoperative status, intraoperative variables, and PPCs were recorded. Patients were divided into two groups depending on the presence or absence of PPCs. Bivariate analysis was done to find out association between various risk factors and PPCs. Multivariate analysis was done to detect relative contribution of the factors shown to be significant in bivariate analysis. P < 0.05 was considered as significant.
Results:
The incidence of PPCs was found to be 15.7%. Factors significantly associated with PPCs were American Society of Anesthesiologists grade higher than II, preoperative lower cranial nerves palsy and respiratory involvement, duration of surgery, and intraoperative blood transfusion. In multivariate analysis, blood transfusion was found to be the sole contributing factor. The patients who developed PPCs had significantly prolonged stay in ICU and hospital.
Conclusion:
Patients with CVJ anomaly are at increased risk of developing PPCs. There is a strong association between intraoperative blood transfusion and PPCs. Patients with PPCs stay in the ICU and hospital for a longer period of time.
Keywords: Craniovertebral junction anomaly, posterior fixation, postoperative pulmonary complications, transoral odontoidectomy
Introduction
Craniovertebral junction (CVJ) anomalies are disorders that affect the cervical vertebral column and enclosed neuraxis at the junction of cranium and vertebral column.[1] The respiratory system is adversely affected in many ways in this group of patients.[2–4] There may be associated weakness and dysfunction of respiratory muscles, including diaphragm. Direct compression of medulla due to bony anomalies results in lower cranial nerve dysfunction or damage to the respiratory center. Cranial nerve dysfunction may cause poor gag and cough reflex resulting in frequent aspiration and pulmonary infection. Afferent respiratory dysfunction has also been described. At times the respiratory involvement may be concealed.[4,5] Significant reduction in postoperative pulmonary functions may occur as compared to preoperative values.[3] The sub-clinical manifestations get exaggerated in the postoperative period because of various anesthetic and surgical reasons.[3,6,7] Therefore, trachea in these patients is usually kept intubated or even, patients are tracheostomized and mechanically ventilated for variable time period to prevent airway complications after surgery.[4,8,9] This can further increase the incidence of pulmonary complications.
Quantification of the problem and identification of patients at risk for postoperative pulmonary complications (PPCs) can be of immense value for management of these patients. However, there is limited knowledge regarding the incidence of the respiratory complications following the definitive surgery, which includes transoral odontoidectomy (TOO) and posterior fixation (PF) performed in the same sitting. In our center, these patients are electively ventilated during the postoperative period for 12-24 h. Hence, we carried out a retrospective study to evaluate PPCs following TOO and PF performed in the same sitting and risk factors associated with it.
Materials and Methods
After obtaining Institutional ethical clearance, 178 patients with CVJ anomaly who underwent TOO and PF in the same sitting, between January 2002 and December 2006 (5 years) were studied. Data were collected by reviewing medical records of these patients. Anesthesia in them was induced either with thiopentone or propofol, fentanyl, and rocuronium was administered to facilitate tracheal intubation, which was achieved either with fiberoptic bronchoscope (awake or under anesthesia) or with direct laryngoscopy, aided by manual-in-line traction. Anesthesia was maintained with oxygen, nitrous oxide, sevoflurane or isoflurane rocuronium and fentanyl. Intraoperative monitoring consisted of invasive as well as non-invasive blood pressure, ECG, SpO2, end tidal carbon dioxide, temperature, urine output, and blood loss estimation. At the end of surgery, patients were electively ventilated in the neurosurgical ICU and trachea extubated next day morning or subsequently, when patients were deemed fit for extubation.
Preoperative data included age, gender, American Society of Anesthesiologists (ASA) grades, type of lesion, associated medical illnesses, and the status of cough and gag reflexes. Presence of respiratory involvement was considered, if there was any sign or symptom related to the respiratory system such as, productive cough, breathing difficulty, need of respiratory support, and presence of abnormal chest X-ray. The intraoperative data on duration of surgery and anesthesia, blood loss, intraoperative complications, fluid and blood administration, were collected. Postoperative data included PPCs, ICU and hospital stay. PPCs were defined as presence of purulent sputum with an increase in body temperature and/or elevated white blood cell count, atelectasis on X-ray chest requiring bronchoscopic aspiration, tracheo-bronchitis, pneumonia, respiratory distress requiring reintubation, and need for tracheostomy.
Statistical analysis was done using STATA 9.0 (College station TX) software. The patients were divided into two groups for the presence or absence of PPCs. Bivariate analysis was done to detect significant risk factors for the development of PPCs. Student’s t-test was used for analysis of continuous variables such as age, duration of surgery and anesthesia, hospital and ICU stay, blood loss and fluid infusion. Chi-square or Fisher’s exact test was done for categorical variables such as lower cranial nerve palsy, and respiratory involvement. Factors found significant in the bivariate analysis were entered in a logistic regression model for a multivariate analysis. This was done to detect relative contribution of the factors shown to be significant by bivariate analysis. P < 0.05 was considered as significant.
Results
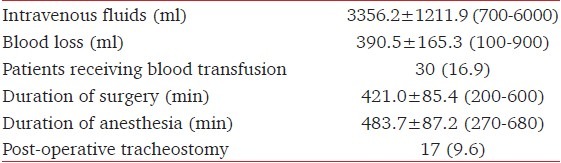
A total of 178 patients underwent TOO and PF over 5 years. The median age was 25 years (range 5-56 years) and most of the patients were males (74%) [Table 1]. Majority of patients (80.9%) had congenital CVJ lesions [Table 2]. Preoperative respiratory involvement was noted in 12 (6.7%) patients. Four patients (2.2%) required intubation in the preoperative period. Lower cranial nerves palsy was present in 10.1% of patients. These patients had either difficulty in swallowing, weak cough, and gag reflexes or frequent aspiration episodes. Tracheal intubation was performed using fiberoptic bronchoscope in 151 patients (84.8%), while in 23 patients (12.9%) direct laryngoscopy with manual in-line stabilization technique was used. The mean duration of surgery was 421.0 ± 85.4 min while the mean duration of anesthesia was 483.7 ± 87.2 min [Table 3].
Table 1.
Demographic data and pre-operative characteristics of the patients mean±SD or percentage or range
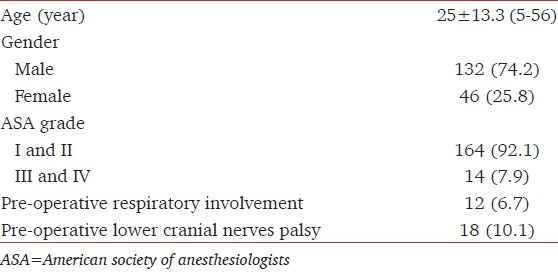
Table 2.
Type of craniovertebral junction anomalies
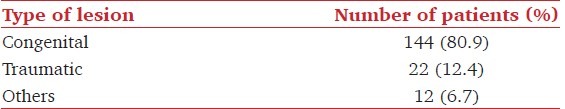
Table 3.
Intraoperative and post-operative data of the patients (Percentage, mean±SD or range)
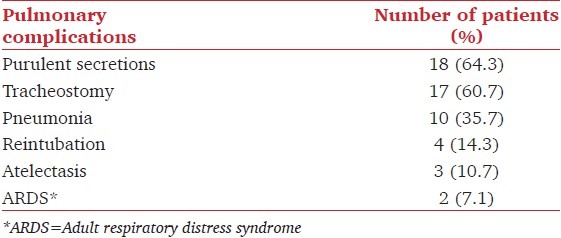
The overall incidence of PPCs in the postoperative period was 15.7%., the commonest (10.1%) being purulent secretions requiring antibiotics [Table 4]. Postoperative elective tracheostomy was performed in 17 (9.5%) patients for difficult weaning from mechanical ventilation. Emergency tracheostomy was done in one patient after failure of both conventional laryngoscopic and fiberoptic intubation. Three patients (1.7%) required bronchoscopic aspiration for atelectasis. Two patients (1.1%) died of respiratory distress syndrome.
Table 4.
Types of post-operative pulmonary complications (n=28)
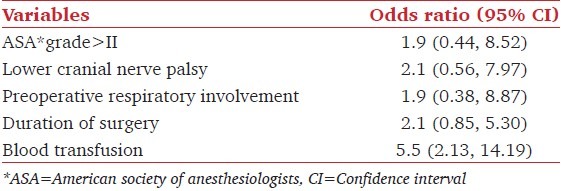
Various factors included in the bivariate analysis for the determination of the risk factors associated with PPCs are depicted in [Table 5]. These variables were divided into two groups based on presence of PPCs. There were no significant differences in respect of age, sex, type of lesion, blood loss and fluid infusion between the two groups. Patients belonging to good ASA grades (I and II) had significantly lower incidence of PPCs compared to poor grade ASA (ASA III and IV patients), (14% in good ASA grade vs. 35.7% in poor ASA grade, P = 0.04). PPCs were significantly more in presence of preoperative LCN palsies, preoperative respiratory involvement and prolonged surgery (P = 0.04). Blood loss was insignificantly greater in patients with PPCs as compared to those without PPCs (437.5 ml in patients with PPCs vs. 381.7 ml in patients without PPCs, P = 0.37). PPCs were more frequent in those patients who received intraoperative blood transfusion (P = <0.001). The mean duration of ICU and hospital stay after surgery was significantly longer in patients who had PPCs as compared to patients without PPCs (9.5 ± 14.8 days vs. 2.7 ± 1.8 days, (P < 0.001); 22.6 ± 16.8 days vs. 7.6 ± 2.8 days (P < 0.001), respectively). The variables which were found significant in the bivariate analysis were included for multivariate analysis [Table 6]. Blood transfusion was found to be the only significant risk factor for the development of PPCs.
Table 5.
Comparison of different variables in patients with and without post-operative pulmonary complications (n=178)*
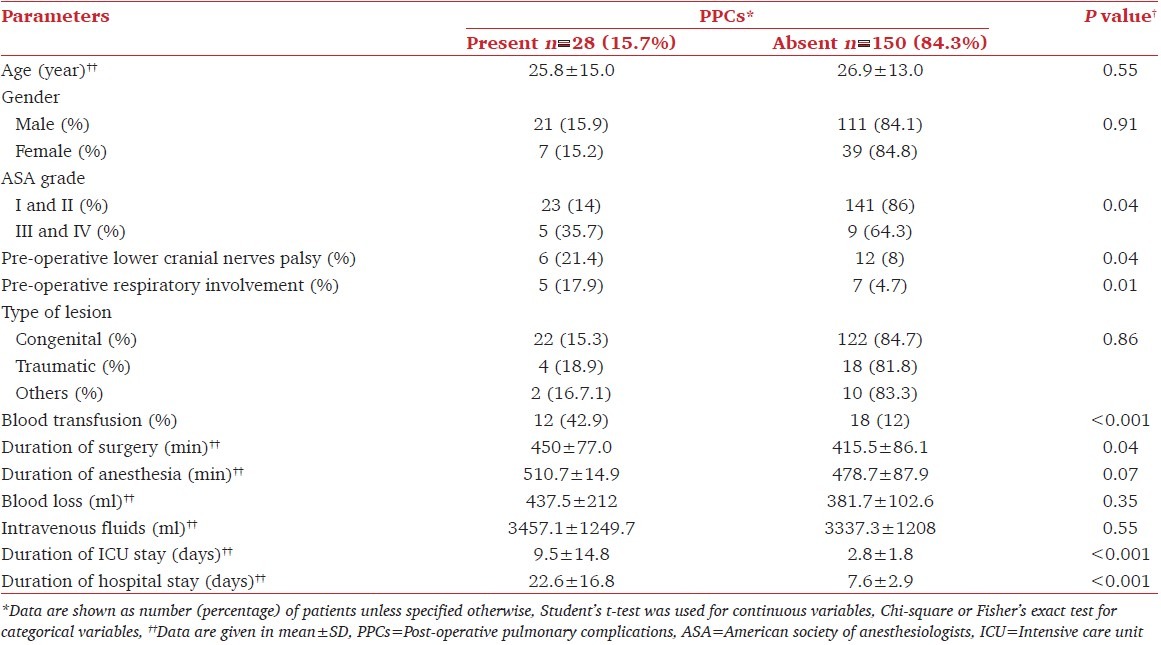
Table 6.
Results of multivariate analysis
Discussion
It is evident from our study that PPCs are relatively common in patients with CVJ anomaly who were operated for TOO and PF in the same sittings. PPCs increased the duration of ICU and hospital stay of these patients. The risk factors were poor ASA grades, preoperative lower cranial nerves palsy, or respiratory involvement, prolonged duration of surgery, and intraoperative blood transfusion.
Patients with CVJ anomaly undergoing TOO and PF are more prone to develop postoperative respiratory complications.[10] They develop preoperative respiratory problems due to lower cranial nerves palsy, leading to pulmonary aspiration, poor cough, and prolonged confinement to the bed, atelectasis, and poor respiratory muscles weakness.[4,10] These problems get aggravated after general anesthesia and surgery.[11] Crockard et al. in their study reported 25% incidence of PPCs following TOO and PF,[8] which is higher as compared to 15.7% observed in our study. Possible reasons for lower complication rate in our series may be improved surgical technique and availability of better diagnostic facilities. Reddy et al. suggested special considerations in these patients, who are more prone to develop PPCs.[12] Monitoring the respiratory functions along with physiotherapy for several days after the definitive surgery has been advocated to prevent PPCs. Terao et al. observed that combined anterior-posterior approach for cervical spine surgery involved greater risk of post-operative emergency airway management in comparison to other cervical spine surgeries.[13] The most common cause for reintubation and delayed extubation in their study was pharyngeal swelling.
The etiology of respiratory dysfunctions in CVJ anomaly patients is multifactorial.[5,7,10] It is considered to be the consequence of repeated trauma to the cervicomedullary junction because of compression by the bony anomalies. The medullary control of breathing, respiratory motor function or sensory inputs all may be affected by lesions at this location. Cervical nerve root may be involved because of vascular compression and ischemia causing phrenic nerve damage and diaphragmatic palsy.
Rosomoff et al. has described the reduced vital capacity, maximum breathing capacity and lung compliance, despite absence of clinical evidence of pulmonary diseases in patients of CVJ anomalies.[5] The respiratory impairment is occult in majority of cases, and is evident only on laboratory testing. In our study, the patients did not undergo preoperative pulmonary function testing. Subjective assessment, therefore, might have missed the presence of respiratory dysfunctions in the preoperative period.
The incidence of pulmonary complications was significantly more in patients who received blood transfusion during intraoperative period. We observed blood transfusion to be an independent risk factor for the development of PPCs. Blood transfusion is known to cause immunotolerance and immunosuppression, which in turn predispose to nosocomial and postoperative infections. Several studies have shown that infection rates are increased following transfusion of homologous blood.[14–19] In our series incidence of PPCs was noted in 42.9% patients who received intraoperative blood transfusion. Immunomodulation associated with blood transfusion was the most likely reason behind increased rate of pulmonary complications.
Apart from blood transfusion, the factors which were found significant in the bivariate analysis were not found significant in the multivariate analysis. This may be because of “type II error” that occurred with a less number of patients with certain variables. The retrospective nature of our study is also a limitation because data on various factors were not recorded during the perioperative period. Therefore, the influence of those variables on our patients is not known.
To conclude, patients with CVJ anomaly are at increased risk of developing PPCs. There is a strong association between perioperative blood transfusion and PPCs. The patients who develop pulmonary complications during postoperative period have significantly longer stay in the ICU and hospital. Nevertheless, large prospective studies are required to substantiate our findings and to identify various other factors influencing the development of PPCs, in these patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Menezes AH. Congenital and acquired abnormalities of the craniovertebral junction. In: Youmans JR, editor. Neurological Surgery. Philadelphia: WB Saunders Company; 1996. pp. 1035–89. [Google Scholar]
- 2.Khosla VK, Gupta SK, Sawhney IM. Neurology in Tropics. New Delhi: B. I. Churchil Livingstone Pvt. Ltd.; 1999. Cranio-vertebral junction anomalies; pp. 639–66. [Google Scholar]
- 3.Rath GP, Bithal PK, Guleria R, Chaturvedi A, Kale SS, Gupta V, et al. A comparative study between pre-operative and post-operative pulmonary functions and diaphragmatic movements in congenital craniovertebral junction anomalies. J Neurosurg Anesthesiol. 2006;18:256–61. doi: 10.1097/00008506-200610000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Krieger AJ, Rosomoff HL, Kuperman AS, Zingesser LH. Occult respiratory dysfunction in a craniovertebral anomaly. J Neurosurg. 1969;31:15–20. doi: 10.3171/jns.1969.31.1.0015. [DOI] [PubMed] [Google Scholar]
- 5.Rosomoff HL. Occult respiratory and autonomic dysfunction in craniovertebral anomalies and upper cervical spinal disease. Spine (Phila Pa 1976) 1986;11:345–7. doi: 10.1097/00007632-198605000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Toyoda H, Nakamura H, Konishi S, Terai H, Takaoka K. Does chronic cervical myelopathy affect respiratory function? J Neurosurg Spine. 2004;1:175–8. doi: 10.3171/spi.2004.1.2.0175. [DOI] [PubMed] [Google Scholar]
- 7.Lindberg P, Gunnarsson L, Tokics L, Secher E, Lundquist H, Brismar B, et al. Atelectasis and lung function in the post-operative period. Acta Anaesthesiol Scand. 1992;36:546–53. doi: 10.1111/j.1399-6576.1992.tb03516.x. [DOI] [PubMed] [Google Scholar]
- 8.Crockard HA, Pozo JL, Ransford AO, Stevens JM, Kendall BE, Essigman WK. Transoral decompression and posterior fusion for rheumatoid atlanto-axial subluxation. J Bone Joint Surg Br. 1986;68:350–6. doi: 10.1302/0301-620X.68B3.3733795. [DOI] [PubMed] [Google Scholar]
- 9.Menezes AH, VanGilder JC. Transoral-transpharyngeal approach to the anterior craniocervical junction. Ten-year experience with 72 patients. J Neurosurg. 1988;69:895–903. doi: 10.3171/jns.1988.69.6.0895. [DOI] [PubMed] [Google Scholar]
- 10.Howard RS, Henderson F, Hirsch NP, Stevens JM, Kendall BE, Crockard HA. Respiratory abnormalities due to craniovertebral junction compression in rheumatoid disease. Ann Rheum Dis. 1994;53:134–6. doi: 10.1136/ard.53.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Almenrader N, Patel D. Spinal fusion surgery in children with non-idiopathic scoliosis: Is there a need for routine post-operative ventilation? Br J Anaesth. 2006;97:851–7. doi: 10.1093/bja/ael273. [DOI] [PubMed] [Google Scholar]
- 12.Reddy KR, Rao GS, Devi BI, Prasad PV, Ramesh VJ. Pulmonary function after surgery for congenital atlantoaxial dislocation: A comparison with surgery for compressive cervical myelopathy and craniotomy. J Neurosurg Anesthesiol. 2009;21:196–201. doi: 10.1097/ANA.0b013e31819f1cce. [DOI] [PubMed] [Google Scholar]
- 13.Terao Y, Matsumoto S, Yamashita K, Takada M, Inadomi C, Fukusaki M, et al. Increased incidence of emergency airway management after combined anterior-posterior cervical spine surgery. J Neurosurg Anesthesiol. 2004;16:282–6. doi: 10.1097/00008506-200410000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Taylor RW, O’Brien J, Trottier SJ, Manganaro L, Cytron M, Lesko MF, et al. Red blood cell transfusions and nosocomial infections in critically ill patients. Crit Care Med. 2006;34:2302–8. doi: 10.1097/01.CCM.0000234034.51040.7F. [DOI] [PubMed] [Google Scholar]
- 15.Hill GE, Frawley WH, Griffith KE, Forestner JE, Minei JP. Allogeneic blood transfusion increases the risk of post-operative bacterial infection: A meta-analysis. J Trauma. 2003;54:908–14. doi: 10.1097/01.TA.0000022460.21283.53. [DOI] [PubMed] [Google Scholar]
- 16.Houbiers JG, van de Velde CJ, van de Watering LM, Hermans J, Schreuder S, Bijnen AB, et al. Transfusion of red cells is associated with increased incidence of bacterial infection after colorectal surgery: A prospective study. Transfusion. 1997;37:126–34. doi: 10.1046/j.1537-2995.1997.37297203513.x. [DOI] [PubMed] [Google Scholar]
- 17.Leal-Noval SR, Rincón-Ferrari MD, García-Curiel A, Herruzo-Avilés A, Camacho-Laraña P, Garnacho-Montero J, et al. Transfusion of blood components and post-operative infection in patients undergoing cardiac surgery. Chest. 2001;119:1461–8. doi: 10.1378/chest.119.5.1461. [DOI] [PubMed] [Google Scholar]
- 18.Chelemer SB, Prato BS, Cox PM, Jr, O’Connor GT, Morton JR. Association of bacterial infection and red blood cell transfusion after coronary artery bypass surgery. Ann Thorac Surg. 2002;73:138–42. doi: 10.1016/s0003-4975(01)03308-2. [DOI] [PubMed] [Google Scholar]
- 19.Acheson AG, Brookes MJ, Spahn DR. Effects of allogeneic red blood cell transfusions on clinical outcomes in patients undergoing colorectal cancer surgery: A systematic review and meta-analysis. Ann Surg. 2012;256:235–44. doi: 10.1097/SLA.0b013e31825b35d5. [DOI] [PubMed] [Google Scholar]


