Abstract
Background:
A parental occupation such as anesthesia care provider can involve exposure of the parent to various chemicals in the work environment and has been correlated to skewed offspring sex ratios.
Objectives:
The objective was to conduct a nation-wide survey to observe (a) whether firstborn offspring sex ratio (OSR) in anesthesia providers is skewed towards increased female offspring, and (b) to identify potential factors influencing firstborn OSR, particularly those relating to the peri-conceptional practice of inhalational anesthesia induction among anesthesia providers.
Materials and Methods:
After institutional review board approval, a questionnaire was uploaded on SurveyMonkey and sent to anesthesia providers through their program coordinators in United States (US) to complete the survey.
Results:
The current US national total-population sex ratio is 0.97 male (s)/female with an at-birth sex ratio of 1.05 male (s)/female; comparatively, the results from anesthesia providers’ survey respondents (n = 314) were a total OSR of 0.93 male (s)/female (P = 0.61) with firstborn OSR 0.82 male (s)/female (a 6% increase in female offspring; P = 0.03), respectively. The only significant peri-conceptional factor related to anesthesia providers’ firstborn OSR’s skew was inhalational induction practice by anesthesia care provider favoring female offspring (P < 0.01).
Conclusion:
Based on the results of this limited survey, it can be concluded that anesthesia care providers who practice inhalation induction of anesthesia during the peri-conceptional period are significantly more likely to have firstborn female offspring.
Keywords: Anesthesia care providers, inhalational induction of anesthesia, offspring sex ratio, parental occupation, peri-conceptional factors
Introduction
Sex ratio is defined as the ratio of males to females in a population. A parental occupation such as anesthesia care provider can involve exposure of the parent to various chemicals in the work environment and has been correlated to skewed offspring sex ratios (OSR) favoring higher proportions of female offspring.[1] However, reported studies in anesthesiologists related to anesthesia practice and its effects on pregnancy including OSR were performed in the early 1970s and were based on small sample populations.[1–6] In addition to the documentation of higher risks for miscarriages, stillbirths, and fetal malformations in female anesthesia care providers, these studies that were performed before the advent of scavenger systems for anesthesia circuits (late 1970s - early 1980s[7]) had documented higher proportions of female offspring in male anesthesia care providers, secondary to occupational exposure to inhalational anesthetics.[2–5] With scavenger systems becoming standard of care for anesthesia care delivery environments in United States over the last three decades, it is valid to investigate whether these earlier reported effects are still evident in the current anesthesia care provider population. As scavenger systems for anesthesia circuits are largely ineffective to protect against occupational exposure to high concentrations of inhalational anesthetics during inhalational induction of anesthesia, an aim of the current study was to observe whether earlier reported effects might be dependent on the type of anesthesia induction.
The present study was designed to investigate firstborn OSR in anesthesia providers and potential factors influencing firstborn OSR. Other effects of occupational exposure to inhalational anesthetics such as incidence of miscarriages and fetal malformations were not investigated. To avoid an overly long questionnaire, only details regarding firstborn offspring were sought from the respondents. Therefore, the primary objectives of this current study were to conduct a nation-wide survey to observe (a) whether firstborn OSR in anesthesia providers is skewed towards female offspring and if so, (b) to identify potential factors influencing firstborn OSR, particularly related to the peri-conceptional practice of inhalational induction (INH) of anesthesia among anesthesia providers.
Materials and Methods
After institutional review board approval, a questionnaire (Appendix A) was uploaded on SurveyMonkey[8] and sent to anesthesia providers (anesthesiology residents/fellows, anesthesiologists, student registered nurse anesthetists, and certified registered nurse anesthetists) through their anesthesiology residency/fellowship program coordinators and nurse anesthetists’ program coordinators in United States (US). Survey respondents were asked to complete the survey to assess OSR
Among respondents’ biological children that were born without assisted reproductive technology (total OSR) and
Among respondents’ firstborn children (firstborn OSR)
Additionally, peri-conceptional factors known to confound OSRs were surveyed only for firstborn offspring:
Practice of INH
Operating room environment (with and without anesthesia scavenging systems)
Smoking
Heavy alcohol use
Obesity and nutritional supplements
Exogenous hormones use (birth control pills and fertility agents)
Physical stress in terms of work hours per week
Statistical analysis
Statistical analysis required ANOVA or t-test where appropriate for continuous data and Chi-squared tests for categorical data. Logistic regression analysis was performed on confounding factors to assess their predictive effect on firstborn OSR. Results were considered significant at a level of P < 0.05.
Results
The response rate to the survey provided a total of 443 respondents [Figure 1], of which 314 respondents were found to be eligible for survey analysis [Figure 2]. The data results from eligible responses’ analysis showed that compared to the US total-population sex ratio of 0.97 male (s)/female,[9,10] the total OSR for survey respondents was 0.93 male (s)/female (power 1-β > 0.99; P = 0.61). As compared to US at-birth sex ratio of 1.05 male (s)/female,[11] firstborn OSR from the survey was 0.82 male (s)/female (a 6% increase in female offspring; power 1-β = 0.61; P = 0.03). The abovementioned survey data-derived OSRs were statistically compared to general population data based on the statistical methods as applied by Wyatt and Wilson.[5]
Figure 1.
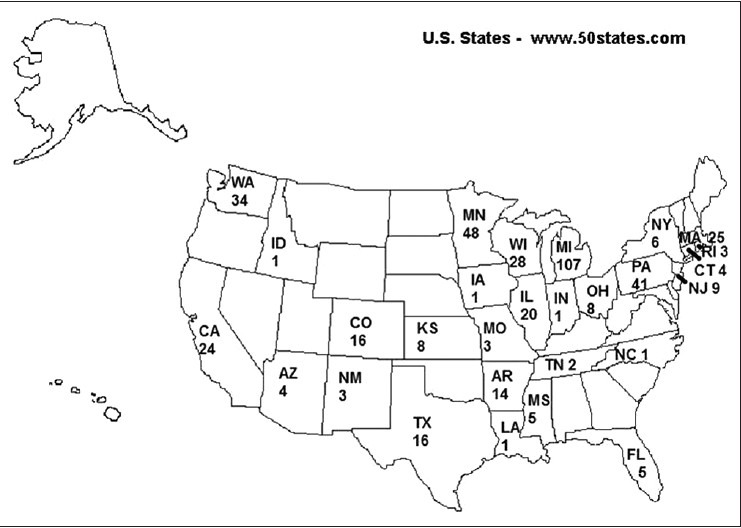
Responders’ Numbers depending on their State of Origin across the United States (adapted from free blank U.S. States Map available at www.50states.com)
Figure 2.
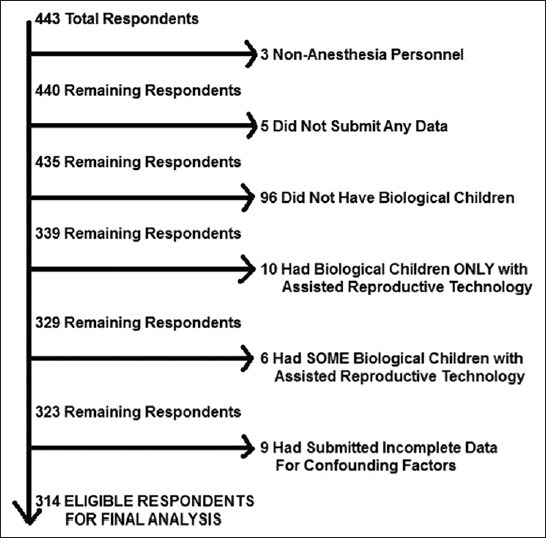
Distribution of respondents to deduce the final eligible respondents for comparative analysis
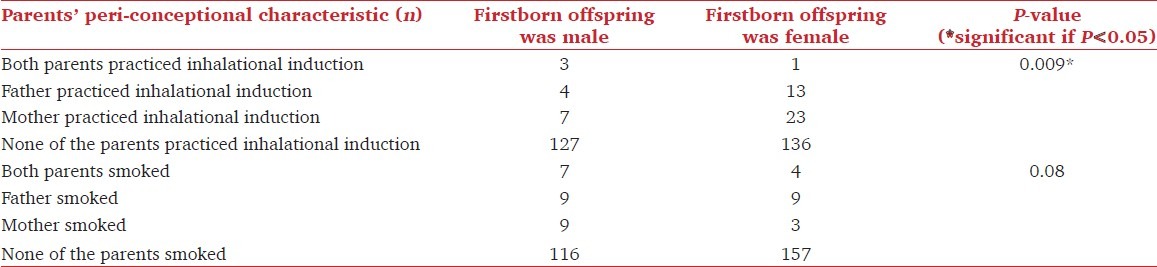
Male respondents’ age (paternal age) at the time of conception of firstborn child was not significantly different (29 ± 5 years if firstborn offspring was male; 30.05 ± 5.09 years if firstborn offspring was female; P = 0.21); however, female respondents’ age (maternal age) at the time of conception of firstborn child was significantly lower if their firstborn offspring were males (28.51 ± 4.3 years versus 30.27 ± 4.3 years; P = 0.01). Logistic regression analysis observed that other significant peri-conceptional confounding factors for firstborn OSR included INH practice by respondents (OSR 0.41 male (s)/female instead of 0.91 male (s)/female; power 1-β = 0.70; P = 0.02) and smoking by respondents (OSR 2.12 male (s)/female instead of 0.75 male (s)/female; power 1-β = 0.68; P = 0.02). None of the other surveyed factors significantly affected firstborn OSR; even absence of anesthesia gas scavenging systems in operating rooms did not affect firstborn OSR significantly [Tables 1 and 2]. After combining the respondents and their spouses for sub-group analysis of male/female anesthesia providers and male/female smokers, smoking’s effect on firstborn OSR disappeared (P = 0.02 changed to P = 0.08) and INH practice’s effect on firstborn OSR accentuated (P = 0.02 changed to P = 0.009) after correction for parental sex [Table 3]. At time of conception of their firstborn child, the duration of cumulative occupational exposure to waste anesthetic gases was not significantly different among anesthesia care providers (3.4 ± 5.8 years for male offspring; 3.8 ± 4.8 years for female offspring; P = 0.26).
Table 1.
Peri-conceptional confounding factors for firstborn offspring sex ratio (OSR) among survey responders
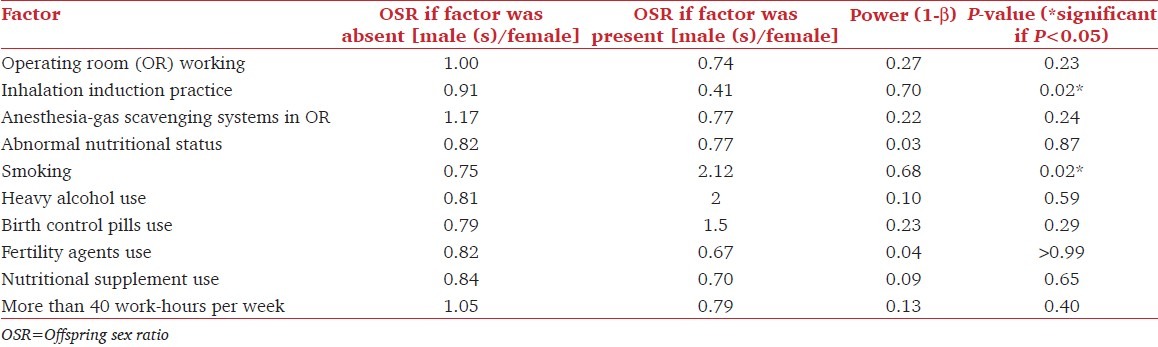
Table 2.
Peri-conceptional confounding factors for firstborn offspring sex ratio (osr) among survey responders’ spouses
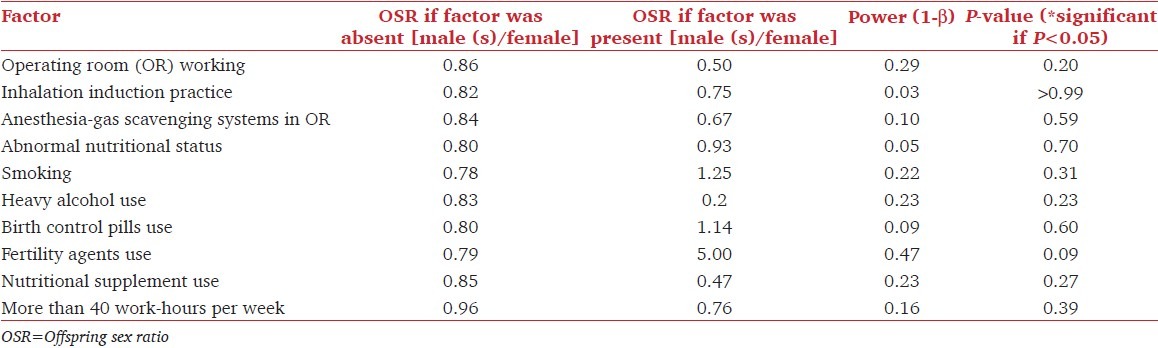
Table 3.
Sub-group analysis of significant peri-conceptional factors corrected for parental sex to elicit effect’s significance on offspring sex ratio
Discussion
The results of this survey raise potential occupational safety concerns regarding the influence of INH on OSR. INH is the standard of care, especially for pediatric anesthesia work environments. Anesthesia care providers practicing INH can be exposed to high concentrations of waste anesthesia gas exposure.[12,13] This occupational exposure can be affected by differing techniques of INH such as conventional stepwise INH or vital capacity rapid INH.[14,15] Another factor affecting occupation exposure to anesthetic gasses may be the scavenging or extraction methods of the waste anesthesia gases.[16–18]
The viability of male-sex determining Y-bearing sperms[19] may be affected by occupational exposure to waste anesthetic gases that may affect OSR in anesthesia care providers[1] (both male providers as well as female providers). Such effects could occur from anesthetic exposure affecting Y-bearing spermatozoa in paternal genital tract (pre-coital life cycle of sperm) as well as in maternal genital tract (post-coital life cycle of sperm). However, spermatozoa functionality tests following occupational exposure to anesthetics have been sparsely investigated.[1] Other peri-conceptional factors that may alter OSR include parental exposure to smoking,[20–22] alcohol abuse,[23–26] stress,[27] obesity,[28] or the use of hormones (exogeneous or endogeneous).[29]
The present survey was designed so that anesthesia providers could compare the anesthesia care provider community’s OSR (total OSR) with the total-population sex ratio in US. However, their firstborn OSR was compared with at-birth sex ratio in US. OSR for the firstborn offspring only (and not for each offspring) was used as the primary outcome because it was the authors’ view that such intricate details regarding OSR-related peri-conceptional confounding factors would be best remembered by the parents for their firstborn children; and limiting the investigation to firstborn OSR would exclude the potential peri-conceptional confounding factor of cumulative occupational exposure to inhalational anesthetics for later-born OSR. Moreover, it was the authors’ view that questionnaire process would be overly long if OSR-related peri-conceptional confounding factors had to be assessed for each offspring.
As the significant findings (INH practice) for the firstborn OSR were adequately powered (1-β = 0.70), these results may instigate future studies to investigate effects of INH practice on the later-born OSR. As the absence of anesthesia gas scavenging systems in operating rooms was insignificant but underpowered (power 1-β = 0.22; P = 0.24) confounding factor, the survey results suggest that the leakage around the face-mask during INH practice and consequent exposure to transient but high concentrations of inhalational anesthetics may be the primary underlying mechanism for firstborn OSR’s skew. Scavenging systems attached to anesthesia machines are primarily efficient in maintaining the operating room environments during maintenance of inhalational anesthesia but are largely ineffective to protect against occupational exposure at the time of inhalational induction of anesthesia. The accentuation of the significance after correction for parental sex (P = 0.009 vs. P =0.02) even though the cumulative occupational exposure years were insignificantly different (P = 0.26) at the time of first conceptions in anesthesia providers (both male as well as female providers) suggest acute (not chronic) effects of waste anesthetic gases on firstborn OSR [Table 3]. Moreover, maternal genital tract’s role in determining firstborn OSR may be related to maternal age (a potential confounding factor) because per our limited results, older female anesthesia care providers more often bore firstborn female offspring. However, these observations need validation in a larger survey sample population to confirm whether these effects on OSR are secondary to direct effects of waste anesthetic gases and/or immunological changes against Y-bearing sperms induced by exposure to waste anesthetic gases. Additionally, the future studies may need to further elicit whether
OSR’s skew is related to effects on the germ cells and/or sperms if the OSR’s skew is secondary to only male anesthesia care providers’ occupational exposure, or
OSR’s skew is related to Y-bearing sperms failing to fertilize as many ova as X-bearing sperms and/or male zygotes failing to implant and/or survive as term fetus if the OSR’s skew is secondary to only female anesthesia care providers’ occupational exposure.
There were some limitations to the present study.
Not surveying for the age of respondents’ spouses during their firstborn children’s peri-conceptional period meant that assessment of parental age as confounding factor could not be analyzed.
Questions could have been framed more clearly to prevent the responders from submitting data related to their children born with assisted reproductive technology [Figure 2].
Despite the adequate statistical power for INH practice’s effect on OSR’s skew, effects of other peri-conceptional confounding factors could have been underestimated due to the lack of statistical power [Tables 1 and 2].
To validate and extend the results of this present study that focused on firstborn offspring, a larger number of surveyed anesthesia care providers will be required in future studies with additional focus on peri-conceptional factors related to every offspring born to anesthesia care providers irrespective of their birth order. A larger number based future study should also interpret our results for the four couples wherein both parents practiced inhalational induction during peri-conceptional period.
Conclusion
Based on the results of this limited survey, it can be concluded that anesthesia care providers who practice inhalation induction of anesthesia during the peri-conceptional period are significantly more likely to have firstborn female offspring.
Acknowledgement
The authors are deeply grateful to all the program coordinators and respondents across the United States that made this survey feasible to be completed, analyzed and presented in the present form. The authors are also grateful to Dr Ronald Thomas, Children’s Research Center of Michigan, Wayne State University, Detroit, Michigan who completed Logistic Regression Analysis for the confounding factors in the study. Finally, the authors appreciate the efforts of anesthesia residents Dr Michelle Daryanani and Dr Arvind Srirajakalidindi, Detroit Medical Center, Detroit, Michigan for their efforts during the research project execution and completion of the written manuscript.
Appendix A

Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Grant VJ, Metcalf LE. Paternal occupation and offspring sex ratio. Psychol Evol Gend. 2003;5:191–209. [Google Scholar]
- 2.Askrog V, Harvald B. Teratogenic effects of inhalation anesthetics. Nord Med. 1970;83:498–500. [PubMed] [Google Scholar]
- 3.Cohen EN, Bellville JW, Brown BW., Jr Anesthesia, pregnancy, and miscarriage: A study of operating room nurses and anesthetists. Anesthesiol. 1971;35:343–7. doi: 10.1097/00000542-197110000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Knill-Jones RP, Rodrigues LV, Moir DD, Spence AA. Anaesthetic practice and pregnancy.Controlled survey of women anaesthetists in the United Kingdom. Lancet. 1972;1:1326–8. doi: 10.1016/s0140-6736(72)91048-3. [DOI] [PubMed] [Google Scholar]
- 5.Wyatt R, Wilson AM. Children of anaesthetists. Br Med J. 1973;1:675. doi: 10.1136/bmj.1.5854.675-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knill-Jones RP, Newman BJ, Spence AA. Anesthetic practice and pregnancy. Controlled survey of male anaesthetists in the United Kingdom. Lancet. 1975;2:807–9. [PubMed] [Google Scholar]
- 7.Google.com/patents [Internet] California: Google Inc; c2012. [Last updated on 2012 August; cited 2012 Aug 13]. Available from: http://www.google.com/patents/US4248219 . [Google Scholar]
- 8.Surveymonkey.com [Internet] California: SurveyMonkey®; c1999-2012. [Last cited on 2012 Aug 13]. [updated 2012 August] Available from: http://www.surveymonkey.com . [Google Scholar]
- 9.CIA.gov/library {Internet] District of Columbia: Central Intelligence Agency; c2012. [updated 2012 August; cited 2012 August 13]. Available from: https://www.cia.gov/library/publications/the-world-factbook/fields/2018.html . [Google Scholar]
- 10.Quickfacts.Census.gov [Internet] District of Columbia: United States Census Bureau; c2012. [updated 2012 June 7]. Available from: http://www.quickfacts.census.gov/qfd/states/00000.html. [Last cited on 2012 Aug 13] [Google Scholar]
- 11.Egan JF, Campbell WA, Chapman A, Shamshirsaz AA, Gurram P, Benn PA. Distortions of sex ratios at birth in the United States; evidence for prenatal gender selection. Prenat Diagn. 2011;31:560–5. doi: 10.1002/pd.2747. [DOI] [PubMed] [Google Scholar]
- 12.Hasei M, Hirata T, Nishihara H, Tanigami H, Takashina M, Mori T. Occupational exposure of operating room staff to anesthetic gases during inhaled induction-a comparison with intravenous anesthesia induction. Masui. 2003;52:394–8. [PubMed] [Google Scholar]
- 13.Hoerauf KH, Wallner T, Akça O, Taslimi R, Sessler DI. Exposure to sevoflurane and nitrous oxide during four different methods of anesthetic induction. Anesth Analg. 1999;88:925–9. doi: 10.1097/00000539-199904000-00045. [DOI] [PubMed] [Google Scholar]
- 14.Epstein RH, Stein AL, Marr AT, Lessin JB. High concentration versus incremental induction of anesthesia with sevoflurane in children: A comparison of induction times, vital signs, and complications. J Clin Anesth. 1998;10:41–5. doi: 10.1016/s0952-8180(97)00218-3. [DOI] [PubMed] [Google Scholar]
- 15.Martín-Larrauri R, Gilsanz F, Rodrigo J, Vila P, Ledesma M, Casimiro C. Conventional stepwise vs. vital capacity rapid inhalation induction at two concentrations of sevoflurane. Eur J Anaesthesiol. 2004;21:265–71. doi: 10.1017/s026502150400403x. [DOI] [PubMed] [Google Scholar]
- 16.Sanabria Carretero P, Rodríguez Pérez E, Jiménez Mateos E, Palomero Rodríguez E, Goldman Tarlousky L, Gilsanz Rodriguez F, et al. Occupational exposure to nitrous oxide and sevoflurane during pediatric anesthesia: Evaluation of an anesthetic gas extractor. Rev Esp Anestesiol Reanim. 2006;53:618–25. [PubMed] [Google Scholar]
- 17.Byhahn C, Strouhal U, Westphal K. Exposure of anesthetists to sevoflurane and nitrous oxide during inhalation anesthesia induction in pediatric anesthesia. Anaesthesiol Reanim. 2000;25:12–6. [PubMed] [Google Scholar]
- 18.Byhahn C, Heller K, Lischke V, Westphal K. Surgeon’s occupational exposure to nitrous oxide and sevoflurane during pediatric surgery. World J Surg. 2001;25:1109–12. doi: 10.1007/BF03215855. [DOI] [PubMed] [Google Scholar]
- 19.Books.Google.com [Internet] California: Google Inc.; c2012. [updated 2012 August]. Available from: http://www.books.google.com/books?id=ExmLlSUCI_UCandq=anesthesiologists#v=snippetandq=anesthesiologistsandf=false. [Last cited on 2012 Aug 13]. [Google Scholar]
- 20.Obel C, Henriksen TB, Hedegaard M, Bech BH, Wisborg K, Olsen J. Periconceptional smoking and the male to female ratio in the offspring--re-assessment of a recently proposed hypothesis. Int J Epidemiol. 2003;32:470–1. doi: 10.1093/ije/dyg089. [DOI] [PubMed] [Google Scholar]
- 21.Parazzini F, Chatenoud L, Maffioletti C, Chiaffarino F, Caserta D. Periconceptional smoking and male:female ratio of newborns. Eur J Public Health. 2005;15:613–4. doi: 10.1093/eurpub/cki052. [DOI] [PubMed] [Google Scholar]
- 22.Fukuda M, Fukuda K, Shimizu T, Andersen CY, Byskov AG. Parental periconceptional smoking and male:female ratio of newborn infants. Lancet. 2002;359:1407–8. doi: 10.1016/S0140-6736(02)08362-9. [DOI] [PubMed] [Google Scholar]
- 23.Chaudhuri AC. The Effect of the Injection of Alcohol into the Male Mouse upon the Secondary Sex Ratio Among the Offspring. J Exp Biol. 1928;5:185–6. [Google Scholar]
- 24.Dickinson H, Parker L. Do alcohol and lead change the sex ratio? J Theor Biol. 1994;169:313–5. doi: 10.1006/jtbi.1994.1152. [DOI] [PubMed] [Google Scholar]
- 25.Kaneda I. The physical values for Japanese infants and preschool children in 2000 (in Japanese) Tokyo: Maternal and Child Health Division, Ministry of Health, Labour and Welfare, Japan; 2002. pp. 54–6. [Google Scholar]
- 26.Fukuda M, Fukuda K, Shimizu T, Andersen CY, Byskiv AG. Periconceptual parental smoking and sex ratio of offspring. Lancet. 2002;360:1515–6. [Google Scholar]
- 27.Navara KJ. Programming of offspring sex ratios by maternal stress in humans: Assessment of physiological mechanisms using a comparative approach. J Comp Physiol B. 2010;180:785–96. doi: 10.1007/s00360-010-0483-9. [DOI] [PubMed] [Google Scholar]
- 28.Abu-Rmeileh NM, Watt G, Lean ME. Sex Distribution of Offspring-Parents Obesity: Angel’s Hypothesis Revisited. Hum Biol. 2011;83:523–30. doi: 10.3378/027.083.0406. [DOI] [PubMed] [Google Scholar]
- 29.James WH. Offspring sex ratios at birth as markers of paternal endocrine disruption. Environ Res. 2006;100:77–85. doi: 10.1016/j.envres.2005.03.001. [DOI] [PubMed] [Google Scholar]


