Abstract
Background:
More than 3/4th of Indian population resides in rural areas. The public awareness towards “Anesthesia and Anesthesiologist” is limited even in urban population. There is no data available from rural India on this perspective. Our cross-sectional analysis highlights this lack of public awareness and discusses possible remedies to overcome these limitations.
Materials and Methods:
Surgical outpatient department of Comprehensive Rural Health Center (CRHC) Ballabgarh, Haryana (model CRHC for Indian health schemes) was screened for 6 months period. A questionnaire divided into 3 parts (Awareness about Anesthesiologist, Consent, Present surgical experience) was filled out for each patient. The patients on the basis of their answers were classified as “aware or unaware”, also source of patient information was analyzed.
Results:
Even with an extremely low threshold, only 36.44% of population could be classified as aware, and commonest source of their information was not anesthesiologist but surgeon (64.32%). 83.6% patients were not aware of contents of pre-operative consent they had signed and further, only 3.4% were aware of anesthesia-related issues. Pain was reported as the most common pre-operative fear and post-operative patient concern. 47.17% patients due to lack of pre-operative counseling were not able to recognize the type of anesthesia and thought they had received both general anesthesia and spinal anesthesia. At the end, after explaining the role of anesthesia for surgery, 99.06% patients presented desire to meet the anesthesiologist beforehand if they were to be operated in future.
Conclusion:
The rural awareness about anesthesia is extremely low likely because of low literacy rates and lack of pre-operative counseling by anesthesiologist. Both patient and anesthesiologist must understand the importance of consent, as it is not only a legal binding but can eliminate pre-operative factitious fears of patients and can improve patient satisfaction towards surgery.
Keywords: Anesthesia consent public awareness, rural India anesthesia awareness, rural survey anesthesia
Introduction
The concern of awareness under anesthesia has always challenged many anesthesiologists and has prompted immense research. However, awareness about anesthesia is still good despite the branch developing and evolving a century back. ‘Anesthesiology’ is a vital branch of medicine; however, public awareness about anesthesiology seems to be dismal beyond big cities. It is not uncommon for an anesthesiologist in India to face questions like, “Is anesthesia a separate medical science?” The burden of research is not only to develop safe anesthesia techniques but also to generate public awareness about anesthesia and the role of an anesthesiologist. Studies on anesthesia awareness have included urban population, neglecting 80% of Indian population residing in the rural areas. The national rural health programs add to public awareness on health issues but with limited goals. Maternal and child health programs have enhanced the public knowledge about possibility of ‘Painless labor;’ however, these programs have added very little to public knowledge about the primary role of anesthesia and the anesthesiologist in this.
To quantify anesthesia awareness in rural areas, we conducted a survey in general surgery outpatient department (OPD) in a World Health Organization approved health center. The Comprehensive Rural Health Center (CRHC) at Ballabgarh, Haryana, which is the theme model for rural healthcare centers in India, was chosen for the present study. This center is a joint association of All India Institute of Medical Sciences, New Delhi and the Haryana government. It has both inpatient and outpatient facilities and caters to a population of around 2.5 lakh.
There is no data on rural population awareness in any Indian published journal or book, and this is the first study of its kind. The study targeted not only to evaluate rural perspective on anesthesia but also to determine awareness about the involved anesthesiologist. By this study, we were also able to highlight the importance of launching national health/anesthesia-based awareness programs, as these programs were found to have significant positive impact on population awareness about labor analgesia. The outcome besides gauging our current rural public perspective also helped us evaluate strategies to improve peri-operative care.
Materials and Methods
A cross-sectional study screening surgical OPD was done, over a period of 6 months - from December 2011 to April 2012. Included patients belonged to either Ballabhgarh or neighboring villages (Dyalpur, Chainsa, Nawada, Garh Khera) and were scheduled for minor surgical procedures under general anesthesia (GA) or sub-arachnoid block (SAB). The patients were questioned in Hindi or their vernacular language using a three-sectioned questionnaire comprising of pre-operative and post-operative set of questions (Annexure attached).
The first set of questions targeted to access the knowledge about “anesthesiologist and what activities he does in the field of medicine.” We also tried to access their source of current knowledge about the anesthesiologist. On the basis of responses, the patients were subdivided into 2 groups, patients answering 3 or more questions of 6 were considered to be aware about the anesthesiologist, and patients unable to answer 3 questions were categorized as unaware. Patients responding wrongly to a question were marked as “incorrect,” and any answer left blank was also counted as “incorrect.” Thus, all responses were categorized as either correct or incorrect for analysis purpose.
The second part of questionnaire was filled prior to discharge of the patient, which was either on the evening of the surgery or the next day morning. These questions evaluated the patient’s understanding about the consent for surgery and their level of understanding developed prior to signing this legal binding. The third set of questions evaluated experience towards surgery and experience acquired about anesthesia from the current surgery. Prior to surgery, all patients were informed that later they would be questioned about post-surgical experience. However, it was not disclosed that these question will be related to their anesthetic management, thus eliminating bias of these patients to become inclined to gain knowledge that they otherwise would not have acquired. It was also made sure that patients were informed about all aspects of the surgery and consent, as done routinely for any other patient. The same was done in surgical OPD itself after filling the first set of questions.
The patient satisfaction was evaluated on a scale of 0-100, with 0 being completely dissatisfied to 100 being highly satisfied. During questioning, we tried to separate satisfaction score on anesthesia point of view only (pain, post-operative nausea and vomiting {PONV}, agitation etc.) rather than surgical outcome. Help of family members was sought for extracting this information from the patient, wherever needed, as majority of patients were uneducated.
Results
The data obtained was summed up and presented as descriptive statistics. Total numbers of similar responses to a question were grouped and were expressed as proportion of total population using Microsoft Excel (2011 ver. for Mac, Microsoft Inc.) During the span of 6 months, we included 214 patients scheduled for minor elective surgeries from Ballabgarh and neighboring villages. Of these patients, 69% were males and 31% were females [Table 1]. Inguinal hernia repair was the most common procedure performed accounting for 49% of total surgeries. Other surgeries were open cholecystectomy (21%), mastectomy (14%), abscess drainage (13%) and procedures like toe amputation etc., (3%) Interestingly, 61.03% patients had exposure to anesthesia information previously, either due to their own or their close relative’s surgeries.
Table 1.
Patients characteristics
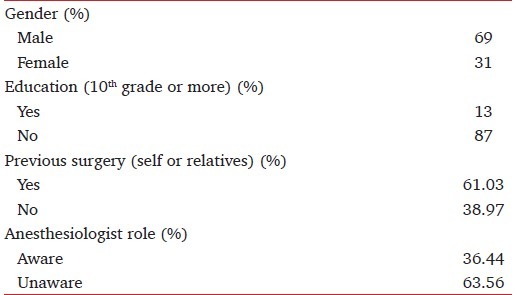
In the first part of survey, of 214 patients, only 1 patient was able to answer the role of anesthesiologist in the operating room correctly. Amongst very general questions about anesthesiologists, 21.05% were not aware of even the existence of anesthesiologist, and either answered wrongly or did not answer even 1 question correctly. 20.09% only could answer a single question correctly. 22.89%, 16.35%, and 5.14% patients could answer 2, 3, 4 questions, respectively. Patients who could be concluded to be well aware of anesthesia and could answer 5 questions were 14.48% [Figure 1]. Only 1 patient (0.46%) who was a school headmaster and had been operated previously in the city for traumatic fracture was able to answer all the 6 questions correctly. Labor analgesia has gained public awareness, as 44.08% patients had heard of it or had some idea about it.
Figure 1.

Graph showing “aware-unaware” population and number of questions answered
Patients qualified as aware about anesthesia were further asked about the source of this information. The most common source of knowledge was surgeon himself (64.32%), followed by 20.66% patients from previous experience of anesthesia and surgeries, and 11.27% of patients had obtained knowledge from friends and family anesthesia experiences. Mass media sources like television and newspapers, which are the major sources of information to urban population for health-related awareness, were only contributory to merely 3.76% of knowledge to aware patients.
Among the procedures performed, 76.4% were performed under SAB and the rest under GA. The post-surgical questionnaire evaluated patient’s common apprehensions towards surgery and their actual anesthesia experience. On asking about any worries related to surgery, 92.3% patients said that they completely trusted the doctor and thus are not worried at all. However, on asking to provide single most possible concern that they are likely to face during surgery was pain in 46.95%, whereas 23% were scared of needle prick during surgery. 10.33% expressed fear of not regaining full consciousness after anesthesia, rest 19.72% were worried of variable complaints like prolonged hospital stay, increased cost of total surgery because of anesthesia drugs and ineffective drug leading to incomplete anesthesia (awareness). Post-surgical possible problems reported by patients were untreatable pain (86.38%), patients who were explained to be given GA were apprehensive about possibility about not waking up well after anesthesia or continued residual effect of anesthesia (7.98%), 5.16% patients when explained risks of GA were scared of possibility of PONV over other concerns. 0.47% patients did not express any answer and neither acknowledged any practical possibility of post-operative fear [Figure 2].
Figure 2.
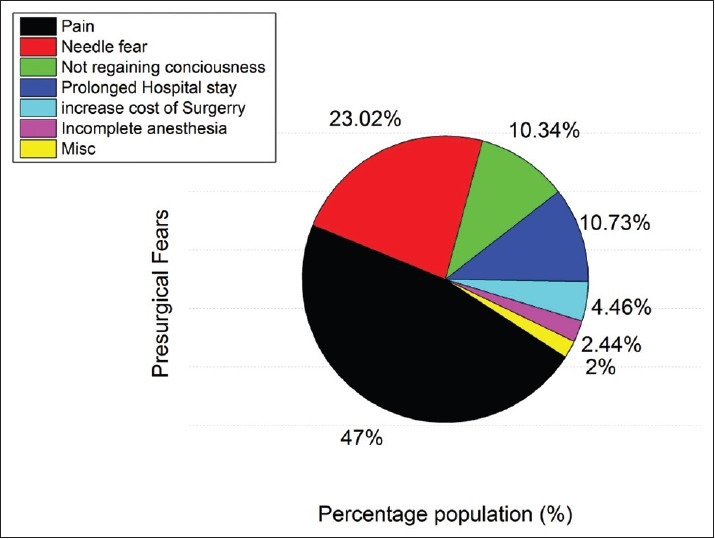
Pre-operative fears reported by patients
On being questioned about the pre-surgical consent, if they understand the possible risks associated with surgery and were it explained to them. 83.6% of patients were aware that they were made to sign a paper that had some information about the procedure, which was possibly the consent. On further asking that who explained them the risk involved, the answer was dismal from the anesthesiology perspective. The surgeon had explained the concerns to only 92.34% of those who had signed consent, and no role of anesthesiologist was mentioned. On evaluating patients on whether they were informed about any risk related to anesthesia in the consent, only 3.4% answered yes while the rest were completely unaware of such information.
47.17% of operated patients believed that they were given both regional and general anesthesia. 38.21% and 14.62% replied that they were given GA and regional anesthesia, respectively [Figure 3]. Common discomfort reported during surgery was cold (24.41%), vomiting (8.45%), shivering (6.10%), and light headedness (5.32%) etc., 36.15% had no complaints at all [Figure 4].
Figure 3.
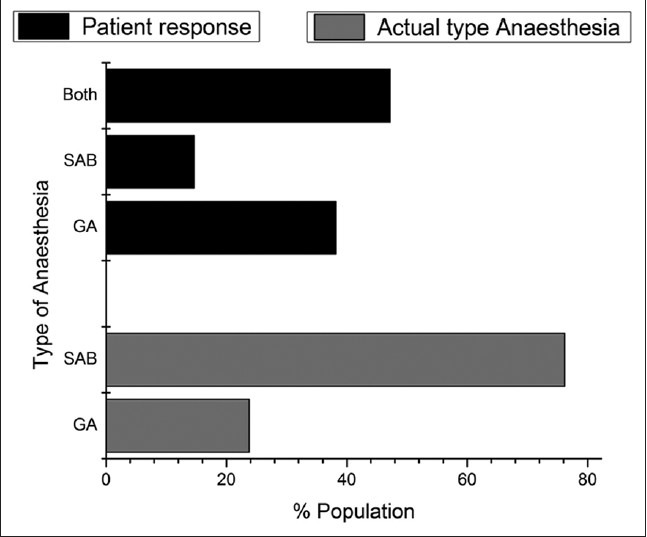
Comparison between actual type of anesthesia given and patient perception. (GA = General anesthesia, SAB = Sub-arachnoid Block)
Figure 4.
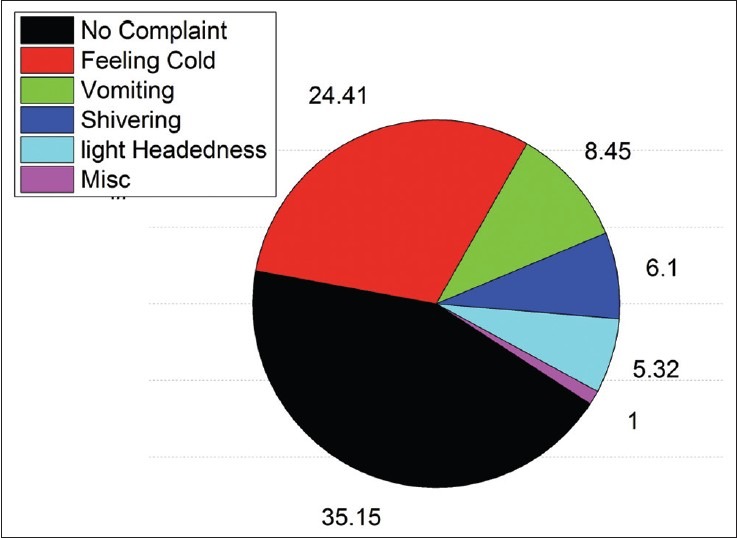
Intra-operative problems reported by patients
In post-operative period, 51.90% patients reported no discomfort. Common problems reported were pain (16.19%), vomiting (9.52%), irritation in throat (5.24%), and difficulty in vocalizing (4.29%). 75.12% of patients said that they were almost 100% satisfied with overall peri-operative experience. 21.13% had satisfaction score around 75% and 2.82% were around 25-50 satisfied with surgical experience. Only 0.94% reported that they were completely dissatisfied and were unhappy with their surgical experience. The understanding of such questionnaire shows its awareness value as at the end, on being asked “if you are operated another time will you like to meet your anesthetist prior to surgery” - the answer was yes for 99.06% and only 1 patient still didn’t approve the need to meet anesthesiologist pre-operatively and insisted the decision to be left on surgeon.
Discussion
India’s population was around 1.2 billion in the 2011 census,[1] of which 72.18% resides in rural area.[2] It is ironical that there is no anesthesia awareness data available for the three fourth population of our country. All the awareness studies conducted in India in the field of anesthesia are on urban population.[3,4] By the present study, we evaluated how well ‘Anesthesiologists’ are known to this rural population. Once lack of awareness is quantified, appropriate steps can be suggested on the basis of magnitude of the problem to rectify it.
Patients were not informed about the type of questions they would be asked about anesthesia at the end of the procedure. This was done to eliminate any bias, which would have prompted the patient in study to be more inclined toward acquiring anesthesia knowledge, which otherwise would have not been done.
Any patient who answered 3 questions from part 1 of the questionnaire was considered aware. A low threshold was kept to include patients with even a slight idea about anesthesia in aware category. The reason for keeping this high sensitivity to classify awareness was due to lack of healthcare-related information available in rural areas. On screening, 87% of patients listed were either completely uneducated or had not completed education till 10th standard. As there are no integrated programs promoting anesthesia-based knowledge, especially in rural areas, despite this low threshold, we found a low awareness. Naithani et al. found much higher awareness scores in a similar study.[4] This difference was possibly because the population included was from a city where level of education is higher.
It was dismal to find that only 36.44% could finally be included in the aware subgroup out of 61.03% patients questioned, who had either themselves or their first kin had undergone surgery. This highlights the shortcomings of the peri-operative team, as patients were unable to recognize the importance of the anesthesiologist in surgical outcome. This can be attributed to a possible neglect by the anesthesiologists at explaining about anesthesia procedures and outcomes. Operative teams must realize the importance of educating and involving the individual patient in peri-operative decision-making.
In a similar study conducted in United Kingdom, about 80% of involved population was able to correctly answer the role of anesthesiologist.[5] This contrast noted in present survey is probably because of higher illiteracy rate of Indian rural population with only 13% of the study population being educated more than 10th grade. Improving the education level of population can improve these results, which are reflected by studies done on Indian urban population. Ironically, for the information about anesthesia, most patients (64.32%) reported the surgeon as the only source, when this should have been the anesthesiologist’s domain. Mass media sources should be promoted by making educational documentaries on anesthesia and its role to make public aware and thus helping in making wise choices when being operated.
An encouraging aspect found in present survey is that 44.08% population was aware or had heard of painless labor. This is highlights the role of successful government programs on maternal and child health, which does provide labor-related information.[6,7] There are no integrated health programs for population-based education on anesthesia and its ability to effect patient’s outcome. Many primary level health centers/medical camps in India under health schemes perform daycare-based short surgical procedures under anesthesia, but the patient awareness level is still low. A simple and economical method is to update these patients on the anesthesia aspects and establishing educational programs in these health centers or camps. The target audience for these awareness programs should not only include general population but also general practitioners and paramedical staff. These health professionals are the first contact for patients in rural health system, and information about anesthesia provided by them is likely to have more impact. These planned awareness programs should also encourage targeted audience to further spread information to acquaintances making awareness programs effective and economical.
Consent is a medico-legal binding between patient and doctor, both patient and anesthesiologist must understand its implications. For majority of patients, it was a paper signed by them, which was a formality in form of paperwork needed prior to surgery. 16.4% patients either did not either sign it or did not remember signing, which underline a major failure of peri-operative team. The validation of consent seems to be a universal problem as Brezis et al. also reported that more than 50% patients did not remember any information related to consent.[8] This is a result of negligence of the involved doctors and can amount to legally punishable professional neglect. Anesthesiologist must realize that explaining the content of the consent is important, and surgeons possibly will fall short in explaining anesthesia-related possible complications, as seen in present study.
The quality of explained consent can be inferred from the fact that 41.17% patients thought that they were given both regional and general anesthesia. A well-explained consent can also eliminate theoretical concerns like not waking after surgery (19.72%) and can also assure patients that anesthesia is necessity for surgery and is not an added cost procedure. Pain has been found to be most common pre-operative cause of anxiety and fear of patients,[9,10] thus while informing content of consent, a possible note about post-operative pain management can have significant role in eliminating anxiety. Consent must not add fear to patients mind, as found in 0.47% of our patients, who otherwise would have not have even known about PONV and now were afraid of it.
Operative room temperatures often tend to be lower than required; this factor possibly was the cause of cold (24.41%) and shivering (6.10%) in patients. This is an easily modifiable factor and can significantly improve patients experience towards surgery. With availability of good analgesics, pain is often not a major post-operative complaint, which is highlighted by 51.90% patients reporting no significant post-operative problems. Systematized patient follow-up in post-operative recovery room can eliminate problems of PONV and pain.
Patients in rural areas do not see a doctor-patient relationship as a legal binding unlike in major cities. They seem to completely trust the treating physician and thus do not question much. The same attitude is responsible for 75.12% patients being completely satisfied after surgery, despite 63.85% having reported at least one problem in post-operative period.
One positive aspect was that when the patients were asked whether they would like to see their anesthesiologist prior to next surgery, 99.06% replied as yes. It is human nature to be inquisitive, a patient undergoing surgery will be naturally be more concerned to know what is likely to happen to him! It is the lack of communication from the side of anesthesiologists that current patient knowledge levels are dismal. Simple efforts like educating patients can make things different.
This cross-sectional study is the first step towards quantifying problem neglected by us. Rural population, which accounts for around 3/4th of total Indian population, is completely unaware that anesthesiology has evolved into a specialization in modern medicine and that it plays a significant role determining surgical outcome. Inferences from present study highlight neglect on anesthesiologist’s attitude towards interacting with patients. Role of pre-operative consent is vital in making patients understand ‘anesthesiologist and anesthesia’ better. It also eliminates anxiety of patients towards surgery. The anesthesiologist should share equal responsibility of explaining terms of consent and possible risks involved in surgery. Mass media sources and government health education programs play an instrumental role in achieving the above targets, and their success is highlighted by increased awareness about labor analgesia in rural India.
Annexure

Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.India’s population rises to 1.2billion: Census of India 2011[Internet] The Times Of India. [Last accessed on 2012 Jun 24]. Available from: http://www.articles.timesofindia.indiatimes.com/2011-03-31/india/29365261_1_population-literacy-rate-census-commissioner .
- 2.Wikipedia contributors. Wikipedia, the free encyclopedia. Wikimedia Foundation, Inc.; 2012. [Last accessed on 2012 Jun 24]. Demographics of India [Internet] Available from: http://www.en.wikipedia.org/w/index.php?title=Demographics_of_Indiaandoldid=4980658 . [Google Scholar]
- 3.Mathur SK, Dube SK, Jain S. Knowledge about anaesthesia and anaesthesiologist amongst general population in India. Indian J Anaesth. 2009;53:179–86. [PMC free article] [PubMed] [Google Scholar]
- 4.Naithani U, Purohit D, Bajaj P. Public awareness about anaesthesia and anaesthesiologist: A Survey. Indian J Anaesth. 2007;51:420. [Google Scholar]
- 5.Swinhoe CF, Groves ER. Patients’ knowledge of anaesthetic practice and the rôle of anaesthetists. Anaesthesia. 1994;49:165–6. doi: 10.1111/j.1365-2044.1994.tb03380.x. [DOI] [PubMed] [Google Scholar]
- 6.Biswas AB, Das DK, Roy RN, Saha I, Shrivastava P, Mitra K. Awareness and perception of mothers about functioning and different services of ICDS in two districts of West Bengal. Indian J Public Health. 2010;54:33–5. doi: 10.4103/0019-557X.70549. [DOI] [PubMed] [Google Scholar]
- 7.Bhandari N, Kabir AK, Salam MA. Mainstreaming nutrition into maternal and child health programmes: Scaling up of exclusive breastfeeding. Matern Child Nutr. 2008;4:5–23. doi: 10.1111/j.1740-8709.2007.00126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brezis M, Israel S, Weinstein-Birenshtock A, Pogoda P, Sharon A, Tauber R. Quality of informed consent for invasive procedures. Int J Qual Health Care. 2008;20:352–7. doi: 10.1093/intqhc/mzn025. [DOI] [PubMed] [Google Scholar]
- 9.Chew ST, Tan T, Tan SS, Ip-Yam PC. A survey of patients’ knowledge of anaesthesia and perioperative care. Singapore Med J. 1998;39:399–402. [PubMed] [Google Scholar]
- 10.Hume MA, Kennedy B, Asbury AJ. Patient knowledge of anaesthesia and peri-operative care. Anaesthesia. 1994;49:715–8. doi: 10.1111/j.1365-2044.1994.tb04408.x. [DOI] [PubMed] [Google Scholar]


