Abstract
Neurofibroma is an uncommon benign tumor of the oral cavity derived from the cells that constitute the nerve sheath neurofibromatosis type 1 (NF1), also known as von Recklinghausen's disease, is the most common type of neurofibromatosis and accounts for about 90% of all cases. It is one of the most frequent human genetic diseases, with the prevalence of one case in 3,000 births. Neurofibroma is seen either as a solitary lesion or as part of the generalized syndrome of neurofibromatosis. The solitary form does not differ from the disseminated form or the multiple form of the disease, except that systemic and hereditary factors present in the disseminated form are absent in the solitary type. Oral cavity involvement by a solitary and peripheral plexiform neurofibroma in patients with no other signs of neurofibromatosis is uncommon. The expressivity of NF1 is extremely variable, with manifestations ranging from mild lesions to several complications and functional impairment. Oral manifestations can be found in almost 72% of NF1 patients. This is a case report of a 40-year-old lady with a history of multiple faint rounded densities in the skin, chest pain occasionally since 8 months and breathlessness since 1 year and swelling of the right side of the angle of the mandible with limited mouth opening.
Keywords: Neurofibromatosis, periodontal manifestations, von Recklinghausen
INTRODUCTION
The term neurofibromatosis is used for a group of genetic disorders that primarily affect the cell growth of neural tissues.[1] First described in 1882 by the German anatomopathologist von Recklinghausen. This disease is a slowly evolving neurodermic dysplasia.[2]
It is an autosomal dominant disorder that affects the bone, the nervous system, soft-tissue, and the skin.[3] At least eight different clinical phenotypes of neurofibromatosis have been identified and are linked to two genetic disorders.[3]
It is a neurocutaneous condition that can involve almost any organ.
Two major subtypes exist
Neurofibromatosis type 1(NF1), which is referred to as peripheral neurofibromatosis
Neurofibromatosis type 2, which is referred to as central neurofibromatosis
A third variant known as segmental neurofibromatosis-limited to a single body region.
NF1 occurs in approximately 2,500-3,300 live births, regardless of the race, age, sex or ethnic background.[3]
Mortality rate is higher than that of the healthy population because of the increased potential for malignant transformation of the diseased tissues and the development of neurofibroma. Patients with NF1 have an estimated 3-15% additional risk of malignant disease in their life-time.
Neurofibromatosis is an autosomal dominant neurogenic disorder.
Increased concentrations of nerve growth stimulating activity have been linked with the development of neurofibromatosis.
NF1 is linked to a large gene on 17q11.2. It encodes a protein neurofibromin has a guanosine triphosphatase region that binds to Ras and positively modulates conversion of guanosine triphosphate to guanosine diphosphate.[4] The protein has been shown to be essential for the negative regulation of Ras.
The NF1 gene has at least 59 exons and encodes the 327-D protein known as neurofibromin.
Truncations in neurofibromin led to the mutations responsible for the NF1 in most cases.
Unusual pigmentary patterns, cafè au lait spots, which are irregularly shaped, evenly pigmented, brown macules.
Lisch nodules are hamartomas of the iris that appear dome shaped and are found superficially around the eyes.
Axillary freckling known as the Crowe sign and inguinal freckling are seen.
Bone involvement can include pseudoarthrosis of the tibia, bowing of the long bones, and orbital defects.
Mild scoliosis and localized bony hypertrophy especially, on the face.
CASE REPORT
A 40-year-old lady reported to the Department of Periodontics M.S.R.D.C from Department of General Surgery M.S.R.M.C with a history of multiple faint rounded densities in the skin, chest pain occasionally, since 8 months and breathlessness since 1 year. Patient's immediate family did no report of neurofibromatosis. Swelling of the right side of the angle of the mandible with limited mouth opening [Figure 1]. There was buccal and cortical bone enlargement extending from anteriorly up to canine and posteriorly up to retro molar region [Figure 2]. Well-defined swelling present in the right palatal region, which was firm in consistency measuring 2 cm × 1 cm approximately and ovoid surface and normal in color [Figure 3]. Areas of oral melanin pigmentation was also seen [Figure 4].
Figure 1.

Swelling of the right side of the mandible
Figure 2.

Buccal and cortical bone enlargement
Figure 3.

Palatal swelling in the upper right molar region
Figure 4.

Areas of oral melanin pigmentation
General examination
For establishing a diagnosis of neurofibromatosis two or more of the criteria described by Gutman et al. needs to be fulfilled, which includes:
-
Six or more café au lait macules:
- Diameter ≥1.5 cm in post-pubertal individuals
- ≥0.5 cm in pre-pubertal individuals
Two or more neurofibromas of any type, or one plexiform neurofibroma
Multiple freckles in the axillary area or groin
Optic glioma
Two or more Lisch nodules (hamartomas of iris)
-
A distinct osseous lesion, such as
- Sphenoid dysplasia
- Thinning of the long bone cortex with or without pseudoarthrosis
A first-degree relative (parent, sibling or offspring) who meets the above criteria for NF1.
In the present case, diagnostic criteria set by Gutman et al. 1997 were fulfilled. They include:
6 café au lait spots
Specific bone changes, thinning of long bones scoliosis was present.
Gingival status
Enlargement of the interproximal, marginal, and attached gingiva.
Periodontal status
Generalized pockets and generalized grade I mobility seen.
Oral prophylaxis and polishing were done and oral hygiene instructions were given with 0.2% chlorhexidine mouthwash.
Biopsy of the suspected lesion was taken.
Incisional biopsy from the buccal cortex and the palatal region was carried out under local anesthesia. After 1 week, patient had reduced enlargement of the gums [Figures 5 and 6].
Figure 5.
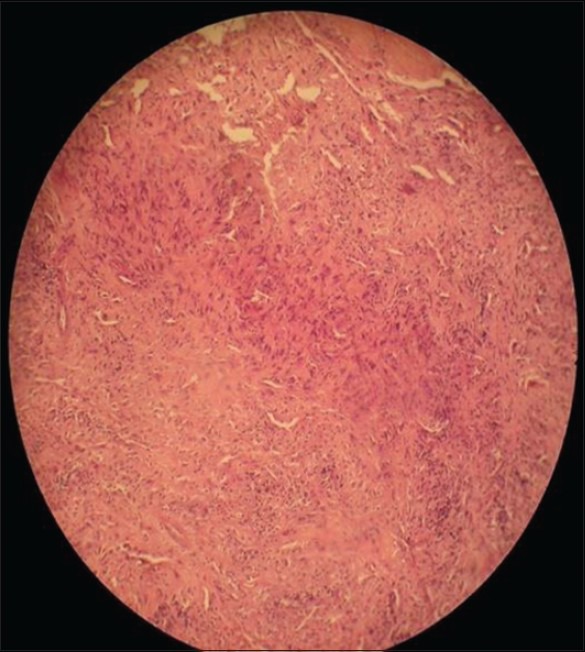
H/P slide showing fibrous dysplasia
Figure 6.

Post operative view-labial
Differential diagnosis
Considering the intra and extraoral and radiographic findings the following were considered for differential diagnosis:
McCune Albright syndrome
Multiple lipomatosis
Proteus syndrome
HISTOPATHOLOGY
Histological sections showed numerous trabecula of woven bone within a proliferating fibroblastic stroma. This confirmed fibrous dysplasia. The subcutaneous nodule showed epidermis lined by stratified squamous epithelium and a well-circumscribed benign spindle cell tumor composed of spindle cells with wavy nucleus and cytoplasm, congested blood vessels suggesting neurofibroma [Figure 7].
Figure 7.

Post operative view-lingual
DISCUSSION
NF1 is due to an alteration of the NF1 gene. This gene is a tumor suppressor gene located I the long arm of chromosome 17 (17q11.2).[1,5,6] The loss of this gene's function due to mutation determines an increase in cell proliferation and the development of tumors.[1]
Pigmented lesions are a common manifestation in NF1. These lesions usually appear during the 1st years of life or are present at birth, either as café au lait spots or as freckles.[1,3,4,5,7] Café au lait spots are hyper pigmented macule that may vary in color form light brown to dark brown. Their borders may be smooth or irregular. They may appear anywhere on the skin, but they are less common on the face.[1] Our patient exhibited six café au lait spots and freckles over her back. Just as related in the literature, the patient reported that many pigmented lesions were present at birth and other ones appeared during childhood.[1,5,7]
It is rarely present at birth but appears in late childhood or early adolescence.[1] The number of localized neurofibromas generally increases with age, and there is an increase in size and number of lesions during the pregnancy and puberty.[1,4] Our patient also reported an increase other lesions during puberty and pregnancy.
Short stature has long been known to a feature of NF1 and it was also observed in our patient.[4] Morbidity of plexiform neurofibromas in NF1 is high since they tend to grow until reaching a great size and producing disfigurement. Besides, the risk of malignization is between 2% and 5%.[1,2]
Bone involvement in NF1 may be due to both external resorption and to internal osteolytic defects. It is well-known that in NF1 bone malformations such as kyphoscoliosis or pseudoarthrosis may appear, and Temperomandibular joint may be involved.[4,7,8] Skeletal involvement is present in almost 40% of patients with NF1, being scoliosis the most common skeletal pathology.[5,8,9] Our patient reported of scoliosis.
Oral cavity involvement appears in 66-72% of the cases of NF1. Lengthening of fungiform papilla happens in 50% of cases and is the most frequent finding. In 2% of neurofibromatosis patients, oral neurofibromatosis patient's oral neurofibromas can be seen. Neurofibromas may appear in every tissue, soft or hard, in the oral cavity.[1,2,5,7,10] In the case reported here the neurofibroma was located in the palate. NF1 patient may also show facial disfigurement due to hypo or hyperplasia of maxilla, mandible, malar bone, and TMJ. Facial plexiform neurofibromas may also cause a facial asymmetry as seen in this case.[1,5]
Histologically, neurofibromas are composed of a mixture of Schwann cells, perineural cells and endoneural fibrobalsts, and they are not capsulated.[2,4,11] Schwann cells account for about 36-80% of lesional cells. These constitute the predominant cellular type and they usually have widened nuclei with an undulated shape and sharp corners.[11]
CONCLUSION
NF1 is one of the most common genetic disease and its oral manifestations are very common, dentists should be aware of the characteristics of this disease. A strict multidisciplinary monitoring will be necessary to intercept any neurological complication or sarcomatous evolution at the earliest possible stage.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Cunha KS, Barboza EP, Dias EP, Oliveira FM. Neurofibromatosis type I with periodontal manifestation. A case report and literature review. Br Dent J. 2004;196:457–60. doi: 10.1038/sj.bdj.4811175. [DOI] [PubMed] [Google Scholar]
- 2.Go JH. Benign peripheral nerve sheath tumor of the tongue. Yonsei Med J. 2002;43:678–80. doi: 10.3349/ymj.2002.43.5.678. [DOI] [PubMed] [Google Scholar]
- 3.Gómez-Oliveira G, Fernández-Alba Luengo J, Martín-Sastre R, Patiño-Seijas B, López-Cedrún-Cembranos JL. Plexiform neurofibroma of the cheek mucosa. A case report. Med Oral. 2004;9:263–7. [PubMed] [Google Scholar]
- 4.Marx RE, Stern D, editors. Illinois: Quintessence Publishing Co, Inc; 2003. Oral and Maxillofacial Pathology: A Rationale for Diagnosis and Treatment. [Google Scholar]
- 5.Bongiorno MR, Pistone G, Aricò M. Manifestations of the tongue in Neurofibromatosis type 1. Oral Dis. 2006;12:125–9. doi: 10.1111/j.1601-0825.2005.01168.x. [DOI] [PubMed] [Google Scholar]
- 6.Lin V, Daniel S, Forte V. Is a plexiform neurofibroma pathognomonic of neurofibromatosis type I? Laryngoscope. 2004;114:1410–4. doi: 10.1097/00005537-200408000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Bekisz O, Darimont F, Rompen EH. Diffuse but unilateral gingival enlargement associated with von Recklinghausen neurofibromatosis: A case report. J Clin Periodontol. 2000;27:361–5. doi: 10.1034/j.1600-051x.2000.027005361.x. [DOI] [PubMed] [Google Scholar]
- 8.Singh K, Samartzis D, An HS. Neurofibromatosis type I with severe dystrophic kyphoscoliosis and its operative management via a simultaneous anterior-posterior approach: A case report and review of the literature. Spine J. 2005;5:461–6. doi: 10.1016/j.spinee.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 9.Hillier JC, Moskovic E. The soft-tissue manifestations of neurofibromatosis type 1. Clin Radiol. 2005;60:960–7. doi: 10.1016/j.crad.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Bhattacharyy I, Cohen D. Oral neurofibroma. 2006. Apr, citado 5 junio2006 Available from: http://www.emedicine.com/derm/topic674.htm .
- 11.Ide F, Shimoyama T, Horie N, Kusama K. Comparative ultrastructural and immunohistochemical study of perineurioma and neurofibroma of the oral mucosa. Oral Oncol. 2004;40:948–53. doi: 10.1016/j.oraloncology.2004.04.015. [DOI] [PubMed] [Google Scholar]


