Abstract
Background
This study compared the association between the 3 definitions of metabolic syndrome (MetS) suggested by the World Health Organization (WHO), National Cholesterol Education Programme (NCEP ATP III), and International Diabetes Federation (IDF), and the risk of cardiovascular diseases (CVD) and shows the prevalence and characteristics of persons with MetS in continental vs. coastal regions and rural vs. urban residence in Croatia.
Material/Methods
A prospective multicenter study was conducted on 3245 participants ≥40 years, who visited general practices from May to July 2008 for any reason. This was a cross-sectional study of the Cardiovascular Risk and Intervention Study in Croatia-family medicine project (ISRCTN31857696).
Results
All analyzed MetS definitions showed an association with CVD, but the strongest was shown by NCEP ATP III; coronary disease OR 2.48 (95% CI 1.80–3.82), cerebrovascular disease OR 2.14 (1.19–3.86), and peripheral artery disease OR 1.55 (1.04–2.32), especially for age and male sex. According to the NCEP ATP III (IDF), the prevalence was 38.7% (45.9%) [15.9% (18.6%) in men, and 22.7% (27.3%) in women, and 28.4% (33.9%) in the continental region, 10.2% (10.9%) in the coastal region, 26.2% (31.5%) in urban areas, and 12.4% (14.4%) in rural areas. Older age, male sex, and residence in the continental area were positively associated with MetS diagnosis according to NCEP ATP III, and current smoking and Mediterranean diet adherence have protective effects.
Conclusions
The NCEP ATP III definition seems to provide the strongest association with CVD and should therefore be preferred for use in this population.
Keywords: metabolic syndrome X, cardiovascular diseases, family practice
Background
Metabolic syndrome (MetS) is defined as a cluster of risk factors [1,2] that identifies persons with increased risk of cardiovascular disease (CVD). The prediction of CVD onset does not have to be better than the Framingham score and Systematic Coronary Risk Evaluation (SCORE), based on the main factors of cardiovascular risk (age, sex, systolic blood pressure, smoking, total, and HDL and LDL cholesterol) [3,4]. The epidemiological proportions of MetS prevalence support its importance in the past 5 decades in countries where the population was found to have increased food consumption and insufficient physical activity [5]. Recent studies indicate that MetS is inferior in establishing rules for the prediction of either type 2 diabetes mellitus (DM2) or coronary heart disease (CHD) [6]. MetS, as a predictor of CVD, has also been studied due to the existence of different definitions [7]. The most frequently mentioned definitions are the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults, Adult Treatment Panel III, the new World Health Organization (WHO) definition, the modified International Diabetes Federation (IDF) definition [8–10], and that of the American College of Endocrinology (AACE) [11]. The WHO and the European Group for the Study of Insulin Resistance Guidelines (EGIR) [12] have been primarily proposed for the needs of research, and the NCEP and IDF definitions were designed for clinical use. This indicates that the role of MetS as a CVD predictor is still uncertain and insufficiently researched. Differences in the definition of MetS create confusion in the timely detection of persons with increased cardiovascular risk in general practitioners’ practices.
Although there are studies about MetS in the Republic of Croatia [13–19], there have been few population studies that analyzed the predictive relevance of the association of each definition with CVD been sparse. We aimed to determine if, defined on the basis of the WHO, NCEP, or IDF criteria, MetS was associated with an increased risk of developing CVD in the population under a family physicians’ care, living in various life conditions (region, rural vs. urban), and depending on age and sex.
Material and Methods
Study design
This study was conducted within the randomized clinical research of the Cardiovascular Risk and Intervention Study in Croatia-family medicine (CRISIC-fm) in the Republic of Croatia and was registered as a clinical trial (International Standard Randomized Controlled Trial Number Register – ISRCTN31857696). It was a two-phase study that ran from May through July 2008.
Participants
The study included 3245 participants of both sexes, aged ≥40. Exclusion criteria were the inability to communicate due to conditions such as dysphasia, aphasia, serious dementia or psychiatric decompensation, and an expected survival of less than 6 months.
Sampling
The sample was two-stage, disproportionate, and mixed-sex. The first phase was to establish a quadruple stratified representative sample of family medicine physicians according to regions (coastal and continental), population size (up to 3999 inhabitants; 4000 to 9999; 10 000 to 29 999; 30 000 to 89 999; and 90 000 and over), rural area (<4000 inhabitants), urban area (>4000 inhabitants), and the number of the insured individuals contracted between family medicine practitioners and the Croatian Health Insurance (HZZO) in 2007 (up to 1399; 1400 to 1799; and ≥1800).
For each initially contacted physician, a reserve sample of 4 more GPs was made, according to the 4-fold stratum. If a GP declined to participate, the nearest GP from a reserve sample was invited. All GPs were verbally informed in detail about the study and then signed a consent form to participate in the research. The sample size needed to reach 95% confidence interval and the desired power of statistical tests. Of the 82 GPs invited to participate in this study, 64 of them accepted (78%), of which 5 declined participation at first follow-up, so the total number of GPs in the final sample was 59.
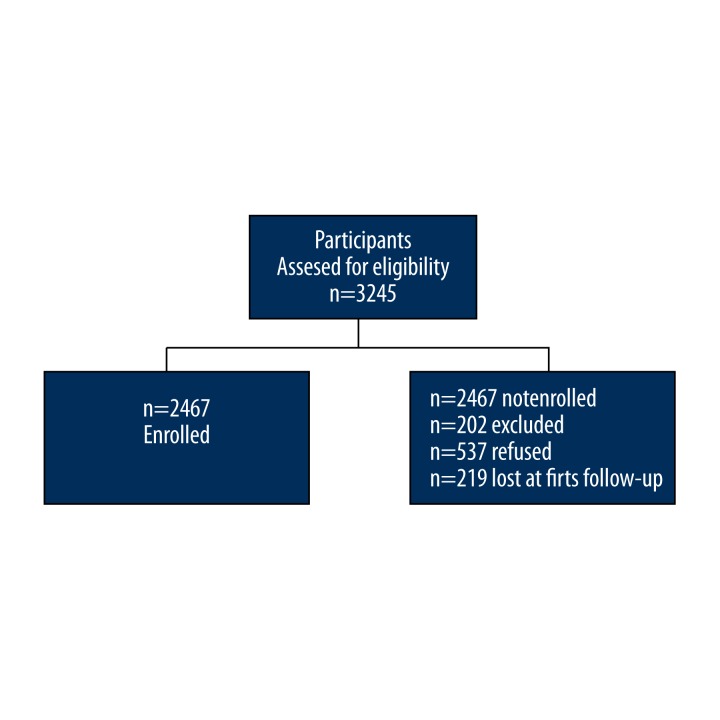
In the second stage, each GP chose a systematic, disproportionate sample of the first 55 patients who visited the practice for any reason from the day the study began, and who met the inclusion criteria and confirmed their consent by signing a written informed consent. All the participating GPs included the same number of patients (N=55), regardless of the total number of insured persons they have contracted with CIHI, and the total number of patients from the target population they examined. This was corrected by post-hoc weight factors prior to statistical analysis (Figure 1).
Figure 1.
Flow chart of patients including in the study.
Measurements and definition of metabolic syndrome
A standardized, validated CRISIC-fm questionnaire with 140 questions, designed for the study, was administered. Participants’ height and weight were measured twice (standardized, identical measuring scales) as well as their waist circumference (WC) and hip circumference (with plasticized inelastic tape measure), and their waist-hip ratio (WHR) was then calculated. Mean arterial pressure (mercury sphygmomanometer) and pulse frequency were assessed. A blood sample for the analysis of total cholesterol concentration, HDL and LDL cholesterol, triglycerides, fasting glucose (FG), and uric acid [20] was taken from each participant. The modified WHO, IDF, and NCEP definitions (Table 1) were used for the MetS analysis. Coronary disease was defined by previous myocardial infarction, angina pectoris, and/or revascularisation of coronary arteries, and cerebrovascular disease was defined by previous cerebral insult and/or transitory ischaemic attack. Peripheral artery disease (PAD) was defined by anamnestic data of intermittent claudication (fatigue, cramping and pain during walking) and <0.8 of ankle brachial index (ABI). Overweight was defined as BMI ≥25, and obesity was defined as BMI ≥30 kg/m2[21].
Table 1.
Definition of metabolic syndrome according to WHO, IDF, and NCEP ATP III.
| WHO (main criterion + two factors)* | IDF (main criterion + three factors) | NCEP ATP (combination of three factors) | |
|---|---|---|---|
| BMI (kg/m2) | >30 | – | – |
| Abdominal obesity (men/women) | WHR <0.9/0.85 | Waist ≥94/80 | Waist >102/88 |
| Triglycerides (mmol/l) | ≥1.7 | >1.7 | >1.7 |
| HDL cholesterol (mmol/l) (men/women) | <0.9/1.0 | <1.03/1.29 | <1.03/1.29 |
| Blood presure (mmHg) | ≥140/90 | >130/>85 or present | ≥130/≥85 |
| Type 2 diabetes** | Present | Present | – |
| Impaired tolerance test | 7.8–11.1 | – | – |
| Fasting glucose (mmol/l) | ≥6.1 | ≥5.6 | >5.6 |
| Urinary albumin excretion | ≥20 μg/min or ≥30 mg/g | – | – |
According to the WHO, either BMI or abdominal obesity represents one criterion;
according WHO, diabetes mellitus type 2, fasting glucose, impaired tolerance test are alternatives, fulfilling one criterion.
WHO – World Health Organization; IDF – International Diabetes Federation; NCEP ATP III – National Cholesterol Education Program Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults.
Bias: We did not examine microalbuminuria, which is part of the WHO definition, due to its unavailability at primary healthcare level.
Statistical analysis
Descriptive statistics procedures were used to describe basic sample characteristics: continental/urban, continental/rural, coastal/urban, and coastal/rural, with differences examined using the χ2 test. An independent t-test was used to analyze the differences in quantitative values of participants’ characteristics between regions and population sizes. We used by binary logistic regression to analyze the relationship between MetS and CVD, as well the association between MetS according to NCEP and socio-behavioral settings. All values were interpreted at the significance level P<0.05. Statistical analysis was performed using SPSS for Windows (11.5, SPSS Inc., Chicago, IL, 2002).
Results
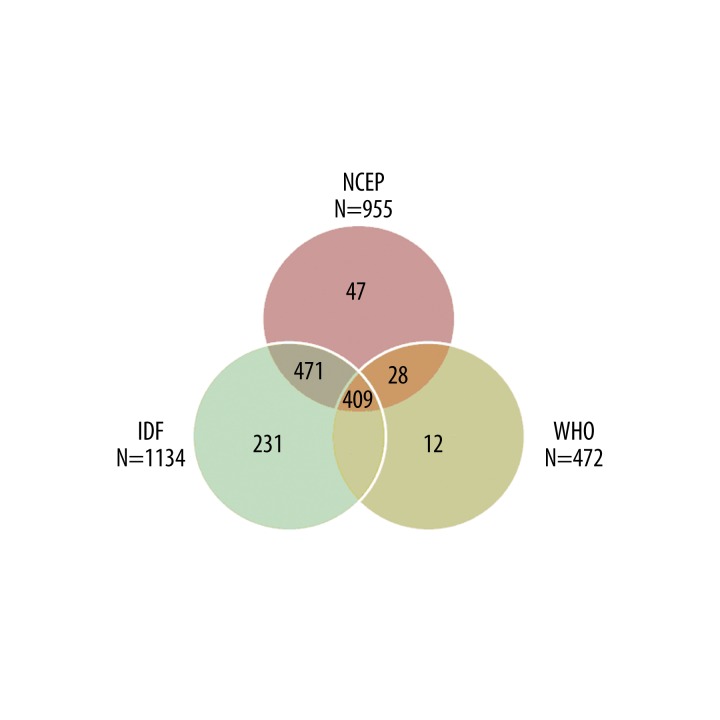
Fifty-nine family medicine doctors joined the study (response rate, 71%) with 2467 participants (38.1% men and 61.9% women) (response rate, 78%). In Figure 2 prevalence of MetS, according to the NCEP, IDF definitions was 38.7% (15.9% men and 22.7% women), 45.9% (18.6% men and 27.3% women); in the continental region 28.4%, 33.9%; in the coastal region 10.2%, 10.9%; in urban residents 26.2%, 31.5%; and in rural residents 12.4%, 14.4%. According to the NCEP criteria, there were significantly more obese people in rural areas (P=0.002) with elevated LDL cholesterol (P<0.001) and systolic pressure (P=0.029) compared to people in urban areas. Participants were older in the urban areas (P=0.022) of the continental region, and they were older (P=0.048) and had a higher waist circumference (P=0.035) in rural residents of the coastal region. Persons with MetS engaged in moderate physical activity more in continental rural than in urban s. The prevalence of prehypertension was significantly higher in urban residents of both coastal and continental regions. MetS was most prevalent in persons aged 50 to 59, except in coastal urban residents, in whom MetS was prevalent in older age (Tables 2 and 3). Association between MetS according to NCEP and socio-behavioural settings was significant (χ2=103.4; df=8; P<0.001) and correctly classified with 60% of subjects. Older age, male sex, and residence in the continental area were positively associated with MetS diagnosis according to NCEP, and current smoking and Mediterranean diet adherence were protective factors (Table 4). The association between MetS and cardiovascular disease was determined according to all 3 definitions, but the NCEP definition was the most sensitive (Table 5). Persons with MetS were, according to NCEP, at a 2.48 times higher risk of coronary disease. The association between MetS and cerebrovascular disease, according to the modified WHO definition, has not been supported by evidence, and according to NCEP and IDF definitions, it was equally significant. The association between MetS and peripheral vascular disease was strongest when expressed according to the modified WHO definition, a weaker association according to the NCEP definition, but the association was negligible according to the IDF definition. Age and sex also show a statistically significant correlation with CVD (Table 6).
Figure 2.
Venn diagran- patients with MetS according to NCEP, IDF and WHO.
Table 2.
Patients with MetS (NCEP, IDF, WHO and combinations).
| Valid | Frequency | Percent | Valid Percent | CumulativePercent |
|---|---|---|---|---|
| Only WHO | 12 | 1.0 | 1.0 | 1.0 |
| Only NCEP | 47 | 3.8 | 3.8 | 4.8 |
| WHO + NCEP | 28 | 2.3 | 2.3 | 7.1 |
| Only IDF | 231 | 18.9 | 18.9 | 26.0 |
| WHO + IDF | 23 | 1.9 | 1.9 | 27.9 |
| NCEP + IDF | 471 | 38.6 | 38.6 | 66.5 |
| WHO+IDF+NCEP | 409 | 33.5 | 33.5 | 100.0 |
| Total | 1221 | 100.0 | 100.0 |
Table 3.
Study sample description (N=955 Croatian adults with metabolic syndrome) according to region (continental/coastal) and settlements (urban/rural) using NCEP ATP III definition: chi square test.
| Continental | Coastal | |||||
|---|---|---|---|---|---|---|
| Urban (N=459) % (N) | Rural (N=242) % (N) | P | Urban (N=189) % (N) | Rural (N=65) % (N) | P | |
| Gender | ||||||
| Men | 41.0 (188) | 38.8 (94) | 0.587 | 47.1 (89) | 35.4 (23) | 0.101 |
| Women | 59.0 (271) | 61.2 (148) | 52.9 (100) | 64.6 (42) | ||
| Age | ||||||
| ≤49 | 12.5 (81) | 30.6 (74) | 0.867 | 13.2 (25) | 4.6 (3) | 0.735 |
| 50–59 | 33.2 (215) | 38.4 (93) | 32.8 (62) | 35.4 (23) | ||
| 60–69 | 29.8 (193) | 30.6 (74) | 33.3 (63) | 27.7 (18) | ||
| ≥70 | 24.2 (157) | 0.4 (1) | 20.6 (39) | 32.3 (21) | ||
| No data | 0.3 (2) | 0,3 (1) | 0 (0) | 0 (0) | ||
| Physical activity intensity* | ||||||
| Low 6 | 44.2 (203) | 31.8 (77) | 0.001 | 50.8 (96) | 36.9 (24) | 0.099 |
| Moderate | 48.1 (221) | 52.5 (127) | 38.6 (73) | 55.4 (36) | ||
| Excessive | 2.2 (10) | 6.2 (15) | 2.1 (4) | 3.1 (2) | ||
| No data | 5,4 (25) | 9.5 (23) | 8.5 (16) | 4.6 (3) | ||
| Smoking | 19.0 (87) | 12.8 (31) | 0.088 | 14.8 (28) | 7.7 (5) | 0.141 |
| No data | 0.2 (1) | – | – | – | ||
| Hypertension | 73.6 (338) | 83.9 (203) | 0.003 | 56.6 (107) | 47.7 (31) | 0.272 |
| Prehypertension | 17.2 (79) | 11.2 (12) | 0.008 | 31.7 (60) | 20.0 (13) | <0.001 |
| Diabetes mellitus type 2 | 17.6 (81) | 16.1 (39) | 0.692 | 18.5 (35) | 10.8 (7) | 0.212 |
| Pre diabetes | 44.4 (204) | 44.2 (107) | 0.841 | 28.0 (53) | 32.3 (21) | 0.338 |
| Dyslipidaemia | 34.9 (160) | 31.0 (75) | 0.339 | 25.9 (49) | 20.0 (13) | 0.430 |
| Mediterranean diet | 13.7 (63) | 9.9 (24) | 0.213 | 30.2 (57) | 35.4 (23) | 0.084 |
| No data | 6.1 (28) | 4.5 (11) | 3.2 (6) | 3.1 (2) | ||
According to American College of Sports Medicine and the American Heart Association.
Table 4.
Study sample description (N=955 Croatian adults with metabolic syndrome) according to region (continental/coastal) and settlements (urban/rural) using NCEP definition: independent t-test.
| nnn | Settlement | Continental | Coastal | ||||
|---|---|---|---|---|---|---|---|
| N | Mean ±SD | P | N | Mean ±SD | P | ||
| Age (years) | Rural | 241 | 59.82±9.62 | 0.022 | 65 | 63.31±9.90 | 0.048 |
| Urban | 456 | 61.61±9.98 | 189 | 60.49±9.87 | |||
| BMI | Rural | 242 | 31.63±4.89 | 0.011 | 65 | 30.94±3.85 | 0.162 |
| Urban | 458 | 30.69±4.54 | 189 | 30.19±3.62 | |||
| WC (cm) | Rural | 242 | 104.5±10.94 | 0.007 | 65 | 99.82±9.90 | 0.035 |
| Urban | 459 | 102.05±11.69 | 189 | 103.08±11.06 | |||
| WHR | Rural | 242 | 0.95±0.09 | 0.007 | 65 | 0.91±0.08 | 0.079 |
| Urban | 459 | 0.93±0.08 | 189 | 0.93±0.08 | |||
| TC (mmol/L) | Rural | 242 | 5.87±1.28 | 0.523 | 65 | 5.79±1.19 | 0.890 |
| Urban | 459 | 5.94±1.40 | 189 | 5.76±1.29 | |||
| LDL-C (mmol/L) | Rural | 210 | 3.77±1.19 | 0.003 | 43 | 3.52±0.99 | 0.336 |
| Urban | 387 | 3.48±1.14 | 157 | 3.35±1.04 | |||
| HDL-C (mmol/L) | Rural | 242 | 1.4±0.44 | 0.738 | 65 | 1.44±0.38 | 0.296 |
| Urban | 459 | 1.39±0.52 | 189 | 1.38±0.40 | |||
| FBG (mmol/L) | Rural | 242 | 6.67±3.31 | 0.666 | 65 | 6.15±1.41 | 0.117 |
| Urban | 459 | 6.59±1.87 | 189 | 6.55±1.85 | |||
| Triglycerides (mmol/L) | Rural | 242 | 2.46±2.33 | 0.384 | 65 | 2.20±0.94 | 0.193 |
| Grad | 459 | 2.34±1.46 | 189 | 2.53±1.99 | |||
| Systolic BP (mmHg) | Rural | 242 | 138.54±15.93 | 0.09 | 65 | 138.14±16.63 | 0.203 |
| Urban | 459 | 136.41±15.73 | 189 | 135.26±15.40 | |||
| Diastolic BP (mmHg) | Rural | 242 | 83.05±7.17 | 0.380 | 65 | 83.49±10.49 | 0.686 |
| Urban | 459 | 82.49±8.38 | 189 | 82.94±9.10 | |||
| Uric acid (mmol/L) | Rural | 217 | 315.73±116.92 | 0.999 | 60 | 301.72±103.59 | 0.648 |
| Urban | 407 | 315.72±100.00 | 150 | 308.55±95.63 | |||
BMI – body mass index; WC – waist circumference; WHR – waist hip ratio; TC – total cholesterol; HDL-C – high density lipoproteins cholesterol; LDL-C – low density lipoproteins cholesterol; FBG – fasting blood glucose; BP – blood pressure.
Table 5.
Association between metabolic syndrome according to NCEP and socio-behavioural settings: binary logistic regression.
| Socio-behavioural settings | Metabolic syndrome according NCEP – ATP III criteria | |||
|---|---|---|---|---|
| OR | 95% CI | P | ||
| Lower | Upper | |||
| Age (years) | 1.04 | 1.03 | 1.05 | <0.001 |
| Gender | ||||
| Female (Ref.) | 1.00 | |||
| Male | 1.24 | 1.01 | 1.53 | 0.049 |
| Residence | ||||
| Rural (Ref.) | 1.00 | |||
| Urban | 0.92 | 0.75 | 1.13 | 0.424 |
| Geographical area | ||||
| Coastal region (Ref.) | 1.00 | |||
| Continental region | 1.43 | 1.15 | 1.78 | 0.001 |
| Predominant diet type | ||||
| Continental | 1.00 | |||
| Mediterranean | 0.77 | 0.60 | 0.98 | 0.036 |
| Alcohol intake | 1.01 | 0.79 | 1.28 | 0.940 |
| Excessive physical activity | 1.21 | 0.72 | 2.03 | 0.480 |
| Current smoking | 0.78 | 0.61 | 1.00 | 0.046 |
OR – odds ratio; CI – confidence interval; Ref. – referent group.
Table 6.
Association of cardiovascular disease and metabolic syndrome with regard to WHO, NCEP, IDF definition, age and gender.
| Definition of MetS | Coronary disease | Cerebrovascular disease | Peripheral artery disease | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| WHO | 2.34 | 1.69–3.23 | <0.001 | 1.55 | 0.84–2.84 | 0.159 | 1.82 | 1.19–2.78 | 0.006 |
| Age | 1.07 | 1.05–1.09 | <0.001 | 1.05 | 1.02–1.07 | 0.002 | 1.04 | 1.02.1.06 | <0.001 |
| Male | 2.11 | 1.53–2.91 | <0.001 | 1.83 | 1.01–3.32 | 0.046 | 1.62 | 1.07–2.46 | 0.021 |
| NCEP | 2.48 | 1.80–3.42 | <0.001 | 2.14 | 1.19–3.86 | 0.011 | 1.55 | 1.04–2.32 | 0.032 |
| Age | 1.07 | 1.05–1.09 | <0.001 | 1.05 | 1.02–1.08 | <0.001 | 1.04 | 1.02–1.06 | 0.000 |
| Male | 2.34 | 1.73–3.16 | <0.001 | 1.75 | 1.01–3.00 | 0.004 | 1.78 | 1.20–2.63 | 0.004 |
| IDF | 2.05 | 1.47–2.85 | <0.001 | 1.99 | 1.07–3.69 | 0.030 | 1.02 | 0.69–1.53 | 0.910 |
| Age | 1.07 | 1.05–1.09 | <0.001 | 1.05 | 1.02–1.08 | <0.001 | 1.04 | 1.02–1.06 | <0.001 |
| Male | 2.34 | 1.73–3.17 | <0.001 | 1.76 | 1.03–3.03 | 0.040 | 1.80 | 1.22–2.65 | 0.003 |
WHO – World Health Organization; NCEP-ATP III – National Cholesterol Education Program Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults; IDF – International Diabetes Federation.
Discussion
This study shows the relationship between MetS and CVD according to all examined definitions, but the most consistent association was shown according to the NCEP definition. Although criteria in the IDF definition are slightly stricter [10], which resulted in lower sensitivity in the association with CVD, the NCEP definition, with its increased sensitivity, was superior. A similar association was shown in a 2007 Swedish study [22]. The NCEP definition was also found to be superior to definitions by the IDF, Joint Interim Statement (JIS), and American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) in a Greek study [23]. The IDF definition is the most appropriate one for practical use [22,23]. The WHO definition includes most elements and is the only definition that uses BMI as a general obesity standard and WHR as a standard for abdominal obesity, but the WHO definition also includes the measurement of insulin resistance, which is not routinely determined in primary healthcare. All other definitions use only waist circumference, which is not a sufficient indicator of general obesity. Although, according to the definition, MetS includes a combination of risk factors, in some studies, the predictive value of such combinations is similar (in Framingham, the MetS definition alone predicted about 25% of all new-onset cardiovascular disease) [3] or even weaker than the value of any of the single risk factors [25]. In our study, a less consistent relationship was seen with stroke (only evident by the NCEP and IDF definitions), thus suggesting that single risk factors, especially systolic blood pressure, were stronger predictors of stroke [26]. Hypertension, as well as hyperlipoproteinemia, proved to be well regulated, so it was not possible to determine the significance of the association between hypertension as a single risk factor and the brain insult. But, the fact that the prevalence of prehypertension was significantly increased in the urban residents of both Croatian regions may be explained by the fact that lifestyle is different from that of rural residents, which in turn contributes to the development of hypertension and its higher prevalence. Therefore, it is not surprising that a controversy exists over whether or not a diagnosis of MetS provides more useful information about CVD risk than its individual components do.
To conduct a proper analysis of the relationship between MetS and CVD, regardless of the diagnostic criteria used, it was necessary to analyze the prevalence of MetS in continental and coastal regions and in urban and rural residents in Croatia due to the significantly different lifestyles of the participants [14,15].
The results of our study show that, according to both definitions, MetS was more prevalent in women aged 50–59, which is inconsistent with studies conducted in some Mediterranean countries [27] where it was more prevalent in men. The reason for the higher prevalence of MetS in these women may be because, in postmenopausal women, height decreases and waist circumference increases. It is important to recognize MetS in older women (>65 years of age) because the association of MetS with all-cause mortality has already been proven in these women, but, in men, such an association has not been proved [28]. Still, in continental Europe, (e.g., Germany), research showed a higher prevalence in men, mostly between 60 and 79 years of age [29]. Our study showed a higher prevalence of MetS in the continental region (due to diet), and in urban vs. rural residents (more physical activity). Similar results were shown by a study in Portugal, where a higher prevalence was found in older women in the continental region [30]. The prevalence of MetS, according to the NCEP definition, in the sample of 9 Dalmatian islands in 2006, was 34%, even reaching 47.2% on the island of Vis [17]. The results of our study of the prevalence of MetS in the coastal region, with 26.6% (NCEP) and 26.1% (IDF), are very similar to the results shown by the study of MetS on the island of Hvar in 2007–8, where it was 25% and 38.5%, based on NCEP and IDF definitions, respectively [19].
Data on the prevalence of MetS among the mainland Croatian populations is limited. A study conducted in a region of continental Croatia (Baranja) showed that the prevalence of MetS, assessed by the NCEP criteria, was 40% (35% in males and 42% in females) [18]. The prevalence of MetS was much higher than in our study, but it is necessary to emphasize that our study was conducted in the whole territory of the Republic of Croatia. The main study limitation is the inability to meet the exact WHO criteria, due to difficulties in establishing microalbuminuria diagnosis in family medicine. Furthermore, GP’s engagement in the intervention group could not be completely controlled, and therefore possibly was not equal among all physicians randomized in that group.
Limitations
There are 2 main limitations to this study. The sample’s subjects were patients registered by GPs, which does not entirely correspond to the general population sample. In addition, we did not examine microalbuminuria, which is part of the WHO definition, due to its unavailability at the primary health care level in Croatia.
Conclusions
Although all 3 definitions of MetS were associated with a higher risk for CHD, association was the greatest and most consistent when using the NCEP definition. According to that definition, the prevalence of MetS is higher in the continental region (possibly due to different diet type) and in urban residents (probably due to less physical activity and more sedentary lifestyle), in older people, and in males.
Acknowledgements
We are grateful to the patients and physicians who participated in the study.
Footnotes
Source of support: Departmental sources
Declaration
Funding: None.
Ethics approval: Ethics Committee, Zagreb University School of Medicine.
Conflicts of interest: None.
References
- 1.Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595–607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan NM. The deadly quartet and the insulin resistance syndrome: an historical overview. Hypertens Res. 1996;19(Suppl 1):S9–11. doi: 10.1291/hypres.19.supplementi_s9. [DOI] [PubMed] [Google Scholar]
- 3.Kahn R, Buse J, Ferrannini E, Stern M American Diabetes Association; European Association for the Study of Diabetes. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2005;28(9):2289–304. doi: 10.2337/diacare.28.9.2289. [DOI] [PubMed] [Google Scholar]
- 4.Rydén L, Standl E, Bartnik M, et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD) Eur Heart J. 2007;28(1):88–136. doi: 10.1093/eurheartj/ehl260. [DOI] [PubMed] [Google Scholar]
- 5.Hanefeld M, Köhler C. The metabolic syndrome and its epidemiologic dimensions in historical perspective. Z Arztl Fortbild Qualitatssich. 2002;96(3):183–88. [PubMed] [Google Scholar]
- 6.Grundy SM, Brewer HB, Jr, Cleeman JI, et al. Definition of the metabolic syndrome: Report of NHLBI/AHA conference on scientific issues related to definition. Circulation. 2004;109(3):433–38. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 7.de Simone G, Devereux RB, Chinali M, et al. Prognostic impact of metabolic syndrome by different definitions in a population with high prevalence of obesity and diabetes: the Strong Heart Study. Diabetes Care. 2007;30(7):1851–56. doi: 10.2337/dc06-2152. [DOI] [PubMed] [Google Scholar]
- 8.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. [PubMed] [Google Scholar]
- 9.World Health Organisation. Definition, diagnosis and clasification of diabetes mellitus and its complications: report of A WHO consultatio. Part 1: dignosis and clasification of diabetes mellitus. [Accessed Apr 03, 2013]. Available at. URL: http://whqlibdoc.who.int/hq/1999/who_ncd_ncs_99.2.pdf.
- 10.The IDF consensus worldwide definition of the metabolic syndrome. International Diabetes Federation; 2006. [Accessed Apr 03, 2013]. Available at. URL: http://www.idf.org/webdata/docs/IDF_Meta_def_final.pdf. [Google Scholar]
- 11.Einhorn D, Reaven GM, Cobin RH, et al. American College of Endocrinology position statement on the insulin resistance syndrome. Endocr Pract. 2003;9(3):237–52. [PubMed] [Google Scholar]
- 12.Balkau B, Charles MA. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR) Diabet Med. 1999;16(5):442–43. doi: 10.1046/j.1464-5491.1999.00059.x. [DOI] [PubMed] [Google Scholar]
- 13.Bergman Marković B, Kern J, Blažeković-Milaković S, et al. Metabolički sindrom u obiteljskoj medicini. Acta Med Croatica. 2007;61:245–51. [PubMed] [Google Scholar]
- 14.Bergman Marković B, Vrdoljak D, Kranjčević K, et al. Continental-Mediterranean and rural-urban differences in cardiovascular risk factors in Croatian population. Croat Med J. 2011;52(4):566–75. doi: 10.3325/cmj.2011.52.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vrdoljak D, Bergman Marković B, Kranjčević K, et al. How well do anthropometric indices correlate with cardiovascular risk factors? A cross-sectional study in Croatia. Med Sci Monit. 2012;18(2):PH6–11. doi: 10.12659/MSM.882451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rumboldt M, Rumboldt Z, Pesenti S. Association between the metabolic syndrome and parental history of premature cardiovascular disease. Eur Heart J. 2006;27(20):2481. doi: 10.1093/eurheartj/ehl262. [DOI] [PubMed] [Google Scholar]
- 17.Kolcić I, Vorko-Jović A, Salzer B, et al. Metabolic syndrome in a metapopulation of Croatian island isolates. Croat Med J. 2006;47(4):585–92. [PMC free article] [PubMed] [Google Scholar]
- 18.Vuletić S, Kern J, Ivanković D, et al. Metabolički sindrom u populaciji Hrvatske- kardiovaskularna multirizičnost. Acta Med Croatica. 2007;61(3):239–43. [in Croatian] [PubMed] [Google Scholar]
- 19.Graham I, Atar D, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary: Fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts) Eur Heart J. 2007;28(19):2375–414. doi: 10.1093/eurheartj/ehm316. [DOI] [PubMed] [Google Scholar]
- 20.WHO. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452. [PubMed] [Google Scholar]
- 21.Nilsson PM, Engström G, Hedblad B. The metabolic syndrome and incidence of cardiovascular disease in non-diabetic subjects – a population-based study comparing three different definitions. Diabet Med. 2007;24(5):464–72. doi: 10.1111/j.1464-5491.2007.02142.x. [DOI] [PubMed] [Google Scholar]
- 22.Athyros VG, Ganotakis ES, Elisaf MS, et al. Prevalence of vascular disease in metabolic syndrome using three proposed definitions. Int J Cardiol. 2007;117(2):204–10. doi: 10.1016/j.ijcard.2006.04.078. [DOI] [PubMed] [Google Scholar]
- 23.Moebus S, Balijepalli C, Lösch C, et al. Age- and sex-specific prevalence and ten-year risk for cardiovascular disease of all 16 risk factor combinations of the metabolic syndrome – A cross-sectional study. Cardiovasc Diabetol. 2010;9:34. doi: 10.1186/1475-2840-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lawlor DA, Smith GD, Ebrahim S. Does the new International Diabetes Federation definition of the metabolic syndrome predict CHD any more strongly than older definitions? Findings from the British Women’s Heart and Health Study. Diabetologia. 2006;49(1):41–48. doi: 10.1007/s00125-005-0040-3. [DOI] [PubMed] [Google Scholar]
- 25.Hadaegh F, Mohebi R, Cheraghi L, et al. Do different metabolic syndrome definitions predict cerebrovascular events and coronary heart disease independent of their components?: 9 years follow-up of the tehran lipid and glucose study. Stroke. 2012;43(6):1669–71. doi: 10.1161/STROKEAHA.112.650812. [DOI] [PubMed] [Google Scholar]
- 26.Lafortuna CL, Agosti F, De Col A, et al. Prevalence of the metabolic syndrome and its components among obese men and women in Italy. Obes Facts. 2012;5(1):127–37. doi: 10.1159/000336700. [DOI] [PubMed] [Google Scholar]
- 27.Forti P, Pirazzoli GL, Maltoni B, et al. Metabolic syndrome and all-cause mortality in older men and women. Eur J Clin Invest. 2012;42(9):1000–9. doi: 10.1111/j.1365-2362.2012.02688.x. [DOI] [PubMed] [Google Scholar]
- 28.Moebus S, Hanisch JU, Aidelsburger P, et al. Impact of 4 different definitions used for the assessment of the prevalence of the Metabolic Syndrome in primary healthcare: The German Metabolic and Cardiovascular Risk Project (GEMCAS) Cardiovasc Diabetol. 2007;6:22. doi: 10.1186/1475-2840-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fiuza M, Cortez-Dias N, Martins S, Belo A VALSIM study investigators. Metabolic syndrome in Portugal: prevalence and implications for cardiovascular risk – results from the VALSIM Study. Rev Port Cardiol. 2008;27(12):1495–529. [PubMed] [Google Scholar]
- 30.Deka R, Durakovic Z, Niu W, et al. Prevalence of metabolic syndrome and related metabolic traits in an island population of the Adriatic. Ann Hum Biol. 2012;39(1):46–53. doi: 10.3109/03014460.2011.637512. [DOI] [PubMed] [Google Scholar]
- 31.Tucak-Zorić S, Curcić IB, Mihalj H, et al. Prevalence of metabolic syndrome in the interior of Croatia: the Baranja region. Coll Antropol. 2008;32(3):659–65. [PubMed] [Google Scholar]