Abstract
Background
Little is known about the epidemiology of urogenital Chlamydia trachomatis infection (chlamydia) in Suriname. Suriname is a society composed of many ethnic groups, such as Creoles, Maroons, Hindustani, Javanese, Chinese, Caucasians, and indigenous Amerindians. We estimated determinants for chlamydia, including the role of ethnicity, and identified transmission patterns and ethnic sexual networks among clients of two clinics in Paramaribo, Suriname.
Methods
Participants were recruited at two sites a sexually transmitted infections (STI) clinic and a family planning (FP) clinic in Paramaribo. Urine samples from men and nurse-collected vaginal swabs were obtained for nucleic acid amplification testing. Logistic regression analysis was used to identify determinants of chlamydia. Multilocus sequence typing (MLST) was performed to genotype C. trachomatis. To identify transmission patterns and sexual networks, a minimum spanning tree was created, using full MLST profiles. Clusters in the minimum spanning tree were compared for ethnic composition.
Results
Between March 2008 and July 2010, 415 men and 274 women were included at the STI clinic and 819 women at the FP clinic. Overall chlamydia prevalence was 15% (224/1508). Age, ethnicity, and recruitment site were significantly associated with chlamydia in multivariable analysis. Participants of Creole and Javanese ethnicity were more frequently infected with urogenital chlamydia. Although sexual mixing with other ethnic groups did differ significantly per ethnicity, this mixing was not independently significantly associated with chlamydia. We typed 170 C. trachomatis-positive samples (76%) and identified three large C. trachomatis clusters. Although the proportion from various ethnic groups differed significantly between the clusters (P = 0.003), all five major ethnic groups were represented in all three clusters.
Conclusion
Chlamydia prevalence in Suriname is high and targeted prevention measures are required. Although ethnic sexual mixing differed between ethnic groups, differences in prevalence between ethnic groups could not be explained by sexual mixing.
Introduction
Urogenital Chlamydia trachomatis infection, or chlamydia, is the most prevalent bacterial sexually transmitted infection (STI) worldwide [1]. Left untreated, chlamydia can lead to complications like pelvic inflammatory disease, ectopic pregnancy, and infertility. To reduce complications and transmission of chlamydia, active case finding and early treatment are critical strategies [2], [3]. Suriname is on the South American continent, but as a consequence of a shared colonial past it is more socio-culturally connected to the Caribbean region. The prevalence of chlamydia in the general population in many countries of the Caribbean is unknown because testing facilities are lacking and routine screening is not available. A study in Guadeloupe among patients who were referred for a genital infection, showed a prevalence of 17% among men and 10% among women [4]. A study in Barbados among the general population showed a prevalence of 11% [5] and a study in Trinidad and Tobago among pregnant women showed a prevalence of 21% [6]. We previously found a prevalence of 21% among high-risk women and 9% among low-risk women in Suriname [7].
The variety of ethnicities is distinctive for Surinamese society. The Surinamese population consists of Creoles and Maroons (both descendants of African diaspora due to the slave trade), Hindustani, Javanese, and Chinese (all descendants of labor immigrants from the former British Indies, Dutch Indies, and China, respectively), Caucasians (descendants of European colonialists), indigenous Amerindians, and people of mixed race. The five major groups are Hindustani (27.4%), Creole (17.7%), Maroon (14.7%), Javanese (14.6%), and mixed race (12.5%). These groups cannot be considered a ‘minority’ since they are comparable in size and integrated parts of the total population [8]. Previous Surinamese studies on sexuality, however, have mainly focused on the Creoles, and rarely on other ethnicities [9], [10].
The structure of sexual networks is important for STI transmission, but elucidating these transmission networks based on epidemiological and behavioral data alone is challenging. Combining epidemiological and behavioral data with molecular microbial genotyping techniques can provide more insight into the transmission patterns of C. trachomatis. Molecular typing can reveal the relatedness of bacterial strains that circulate among the population and may identify transmission networks at the pathogen level. Because of the low genetic variability of C. trachomatis, a typing tool with a high discriminatory resolution between strains is necessary to reveal network associations of C. trachomatis. Whereas suitable molecular techniques for Neisseria gonorrhoeae have been available for some time [11], high-resolution typing methods for C. trachomatis, such as multilocus sequence typing (MLST), have only been developed recently [12], [13]. Studies using high-resolution typing of C. trachomatis strains have examined the relation between clinical symptoms [14], geographic location [15], and sexual risk group [16], [17]. The relation between ethno-demographic characteristics and C. trachomatis strains in sexual transmission networks of heterosexual populations has not yet been analyzed using high-resolution molecular pathogen typing.
Earlier we reported a high chlamydia prevalence among both low- and high-risk women [7]. Here we report on the chlamydia prevalence among women as well as men. The aim of our study among men and women at two clinics in Paramaribo, Suriname was to elucidate determinants for chlamydia, notably the role of ethnicity and ethnic sexual mixing, and to identify transmission patterns and sexual networks using molecular epidemiological network analyses.
Methods
Ethics Statement
The study was approved by the ethics committee of the Ministry of Health of the Republic of Suriname (VG010-2007) and the ethics committee of the Academic Medical Center, University of Amsterdam, the Netherlands (MEC07/127). Patients participated anonymously and gave written informed consent.
Recruitment Sites and Population
Participants were recruited at two sites in Paramaribo, Suriname:
The Dermatological Service, an integrated outpatient STI clinic, frequented by men and women, that offers free-of-charge examination and treatment of STIs and infectious skin diseases such as leprosy and leishmaniasis,. All individuals who visited for an STI check-up were invited to participate in the study. These participants were considered to be a ‘high-risk’ population for chlamydia.
The Lobi Foundation, a family planning (FP) clinic frequented by women only. All consecutive women visiting the clinic were invited to participate in the study. As women do not primarily visit this clinic to be checked for STIs, these participants were considered to be a ‘low-risk’ population for chlamydia.
Recruitment took place between March 2008 and July 2010. Exclusion criteria were: age younger than 18 years and previous participation in the study. A nurse interviewed participants about demographic characteristics (including self-reported ethnicity) and sexual behavior.
Specimen Collection and Testing Procedures
Urine samples from males and nurse-collected vaginal swabs from females were obtained for nucleic acid amplification test (NAAT) testing with the monospecific Aptima Chlamydia assay for the detection of C. trachomatis rRNA (Hologic Gen-Probe Inc., San Diego, USA). Nurses were trained to collect the swabs before routine speculum examination was performed, as described before [7]. The samples were collected according to the manufacturer’s instructions, stored in a fridge (at temperature between 2° and 7°C) and packed according to IATA rules for transport by plane to the Public Health Laboratory in Amsterdam for NAAT testing. Technicians performing NAAT did not receive any information about the participant. NAAT test results were forwarded to the two clinics in Suriname, where the chlamydia positive participants were treated within 1 to 8 weeks after the clinic visit with doxycycline (100 mg bid for 7 days at the FP clinic and 100 mg bid for 10 days at the STI clinic) or, in case of (probable) pregnancy, with a single 1000 mg oral dose of azithromycin. Participants who tested positive for urogenital chlamydia also received treatment to be used by their partner(s).
MLST
Multilocus sequence typing (MLST) was used to genotype C. trachomatis. Details of this method were described previously [13]. In brief, DNA was extracted at the Public Health Laboratory Amsterdam from transport medium in which the swab or urine had been put, using isopropanol precipitation. All DNA isolates were tested for the presence of chlamydial DNA with the in-house pmpH qPCR as described previously [18], [19]. The DNA isolates were amplified by a nested PCR and sequenced for the regions ompA, CT046 (hctB), CT058, CT144, CT172 and CT682 (pbpB). The sequences were checked against an in-house library and against the Chlamydia trachomatis MLST database (mlst.bmc.uu.se), and were given an allele number for each region. Only samples of which all alleles were successfully amplified, sequenced and identified, and therefore had obtained a full MLST profile (sequence type, ST), were included in the analyses. As ompA is part of the MLST scheme, genovars could be assigned for all included samples. A minimum spanning tree was generated using MLST profiles. Cluster analysis was performed allowing single locus variance using BioNumerics 7 (Applied Maths, Sint-Martens-Latem, Belgium). A cluster was defined as a group of STs differing by not more than one locus from another ST within that group, and had to include at least 10% of the total number of samples (i.e. at least 17 samples). Typing data of the study population are also reported in a paper comparing the distributions of C. trachomatis strains among residents of Paramaribo and residents of Amsterdam (Bom et al., submitted).
Statistical Analysis
The study population consisted of high-risk men and women recruited at the STI clinic and low-risk women recruited at the FP clinic. To examine whether epidemiological characteristics differed between these three study groups the χ2-test for independence was used. Prevalence was calculated as the number of positive tests in the study period divided by the total number of individuals tested in the study period [20]. To assess determinants of chlamydia, we performed univariable logistic regression analysis and examined the effect of the following variables: age, education, ethnicity, different ethnic group of sexual partners (i.e. ethnic sexual mixing), study group (including sex and recruitment site), condom use, number of partners in the preceding month, number of partners in the preceding 12 months, having had sex in exchange for money or goods, and (for men) having had sex with men (MSM). Age was divided into four categories. Because of small numbers we grouped Caucasian, Chinese, and Indigenous Amerindian ethnicities together in univariable and multivariable analyses. Ethnic sexual mixing was defined as having had sex with at least one partner of another ethnicity in the preceding 12 months. Variables that were associated with chlamydia at P≤0.1 in the univariable analysis were entered into a multivariable model. Higher chlamydia prevalence at younger age and, with a higher number of sexual partners has been established by various other studies [21] and therefore these determinants were forced into the multivariable model. Ethnicity and ethnic group of the partner(s) were variables of specific interest and were also forced into the model. To avoid multicollinearity, we only included the variable ‘number of partners in the preceding 12 months’ in the model and not the variable ‘number of partners in the preceding month’. We considered P<0.05 as statistically significant. We checked for interactions between study group and all other variables in the final model and also checked for interactions between the number of partners in the preceding 12 months and ethnic sexual mixing.
To examine whether ethnic group was a determinant for ethnic sexual mixing, we performed a multivariable logistic regression analysis. Variables that were associated with ethnic sexual mixing at P≤0.1 in univariable analysis were entered into a multivariable model. The final model included number of partners in the preceding 12 months, sex in exchange for money or goods, and study group.
We compared the observed frequency of people who had sexual partners from their own ethnicity with the expected frequency (if partner selection from the population would have occurred at random with respect to ethnic background) by using the χ2 goodness-of-fit test [22]. The expected number of people with sexual partners from their own ethnicity was calculated by multiplying the total number of reported partners of an ethnicity by the proportion of individuals from each ethnicity in the study. In order to identify transmission patterns and sexual networks, a minimum spanning tree was made with different colors for different ethnicities and C. trachomatis clusters were compared in terms of ethnic composition using χ2-tests for independence. Analyses were performed with SPSS package version 19.0 (SPSS Inc., Chicago, IL).
Results
Study Population
A total of, 415 men and 1093 women were included in the study. The response rate among men was 78.3%, among women visiting the STI clinic 83.0% and among women visiting the FP clinic 99.8%. The included and excluded men did not differ by age (P = 0.303) and ethnicity (P = 0.329). The included and excluded women visiting the STI clinic had a comparable age (P = 0.238) but ethnicity did differ (P = 0.020). Demographics and sexual behavior of study participants are shown in Table 1. All epidemiological characteristics differed significantly between the three study groups. The overall median age was 29 years (IQR 25–37) and the majority had a low (40.5%) or medium (42.9%) level of education. In total, 444 (29.4%) were of Creole ethnicity, 289 (19.2%) of Hindustani ethnicity, 177 (11.7%) of Javanese ethnicity, 277 (18.4%) were mixed race, and 258 (17.1%) were of Maroon ethnicity. Women visiting the STI clinic were younger compared with men from the same site and women visiting the FP clinic (P<0.001). Women visiting the STI clinic reported higher risk behavior, such as >2 partners in the previous year (23.0%), and more frequently reported sex in exchange for money or goods (16.7%), compared with women visiting the FP clinic (6.1% and 0.7%, respectively).
Table 1. Epidemiological characteristics of the study population by study group in Paramaribo, Suriname, 2008–2010.
| Men recruitedat STI clinic | Women recruitedat STI clinic | Womenrecruitedat familyplanningclinic | P value | Total studypopulation | ||
| (N = 415) | (N = 274) | (N = 819) | (N = 1508) | |||
| n (%) | n (%) | n (%) | n (%) | |||
| Demographic characteristics | ||||||
| Median age in years (IQR) | 29 (25–38) | 28 (23–33) | 31 (25–37) | <0.001 | 29 (25–37) | |
| Age in years | <25 | 109 (26.3) | 105 (38.3) | 184 (22.5) | <0.001 | 398 (26.4) |
| 25–29 | 116 (28.0) | 67 (24.5) | 198 (24.2) | 381 (25.3) | ||
| 30–34 | 59 (14.2) | 47 (17.2) | 173 (21.2) | 279 (18.5) | ||
| > = 35 | 131 (31.6) | 55 (20.1) | 264 (32.2) | 450 (29.8) | ||
| Education | Low | 235 (56.6) | 99 (36.1) | 277 (33.8) | <0.001 | 611 (40.5) |
| Medium | 111 (26.7) | 109 (39.8) | 427 (52.1) | 647 (42.9) | ||
| High | 40 (9.6) | 46 (16.8) | 111 (13.6) | 197 (13.1) | ||
| Unknown | 29 (7.0) | 20 (7.3) | 4 (0.5) | 53 (3.5) | ||
| Ethnic groupa | Caucasian | 2 (0.5) | 11 (4.0) | 6 (0.7) | <0.001 | 19 (1.3) |
| Chinese | 1 (0.2) | 6 (2.2) | 6 (0.7) | 13 (0.9) | ||
| Creole | 166 (40.0) | 79 (28.8) | 199 (24.3) | 444 (29.4) | ||
| Hindustani | 33 (8.0) | 30 (10.9) | 226 (27.6) | 289 (19.2) | ||
| Indigenous | 6 (1.4) | 9 (3.3) | 10 (1.2) | 25 (1.7) | ||
| Javanese | 14 (3.4) | 17 (6.2) | 148 (17.9) | 177 (11.7) | ||
| Maroon | 120 (28.9) | 53 (19.3) | 85 (10.4) | 258 (17.1) | ||
| Mixed | 72 (17.3) | 67 (24.5) | 138 (16.8) | 277 (18.4) | ||
| Sexual behavior | ||||||
| Ethnic sexual mixinga | Had only sexual partnersfrom same ethnic group | 162 (40.5) | 120 (48.0) | 508 (64.9) | <0.001 | 790 (55.1) |
| Had at least one sexual partnerfrom another ethnic group | 238 (59.5) | 130 (52.0) | 275 (35.1) | 643 (44.9) | ||
| Condom usea | Always | 126 (30.7) | 76 (28.0) | 79 (9.8) | <0.001 | 281 (18.8) |
| Never or inconsistent | 285 (69.3) | 195 (72.0) | 731 (90.2) | 1211 (81.2) | ||
| Number of partners preceding montha | 0 | 22 (5.3) | 16 (6.3) | 34 (4.2) | <0.001 | 72 (4.9) |
| 1 | 228 (55.1) | 185 (73.4) | 741 (91.7) | 1154 (78.3) | ||
| >1 | 164 (39.6) | 51 (20.2) | 33 (4.1) | 248 (16.8) | ||
| Median number of partners in thepreceding 12 months (IQR) | 2 (1–4) | 1 (1–2) | 1 (1–1) | <0.001 | 1 (1–2) | |
| Mean number of partners in thepreceding 12 months | 7 | 16 | 1 | |||
| Number of partners in thepreceding 12 months | 0 | 2 (0.5) | 11 (4.0) | 11 (1.3) | <0.001 | 24 (1.6) |
| 1 | 109 (26.3) | 136 (49.6) | 649 (79.2) | 894 (59.3) | ||
| 2 | 114 (27.5) | 64 (23.4) | 108 (13.2) | 286 (19.0) | ||
| >2 | 190 (45.8) | 63 (23.0) | 51 (6.1) | 304 (20.2) | ||
| Sex in exchange for money or goodsa | 11 (2.7) | 45 (16.7) | 6 (0.7) | <0.001 | 62 (4.2) | |
| Men having sex with mena | 7 (1.7) | NA | NA | 7 (1.7) | ||
| Chlamydia prevalence | ||||||
| Chlamydia trachomatis infectiondiagnosis by NAAT | 95 (22.9) | 51 (18.6) | 78 (9.5) | <0.001 | 224 (14.9) |
Numbers do not add up to the column total due to missing data, percentages do add up to 100%.
Missing data: ethnic group n = 6, ethnic sexual mixing n = 75, condom use n = 16, number of partners in the preceding month n = 34, sex in exchange for money or goods n = 22, men having sex with men n = 3.
IQR, interquartile range; NA, not available; NAAT, nucleic acid amplification test; p-values based on men attending the STI clinic, women attending the STI clinic and women attending the family planning clinic.
Prevalence and Determinants of Chlamydia
The prevalence of chlamydia was 18.6% (95% CI, 14.3–23.6%) among women visiting the STI clinic, 9.5% (95% CI, 7.7–11.7%) among women visiting the FP clinic [7] and 22.9% (95% CI, 19.0–27.1%) among male STI clinic visitors. The highest prevalence of chlamydia was found among Creole men visiting the STI clinic (30.1%) but this was not significantly higher than the prevalence among men from other ethnic groups which ranged between 15.2% and 21.4% (P = 0.123). Hindustani women had a slightly lower prevalence (6.3%) compared with women from other ethnic groups, which ranged between 10.9% and 15.3% (P = 0.054). Univariable associations between epidemiological characteristics and chlamydia are shown in Table 2. Age, ethnic group, ethnic sexual mixing, study group and number of partners in the preceding 12 months were significantly associated with chlamydia in univariable analysis. In multivariable analysis, chlamydia was significantly associated with ethnic group (OR, 1.76; 95% CI, 1.03–3.00 for Creoles, OR, 2.05; 95% CI, 1.09–3.84 for Javanese, both compared with Hindustani); age (OR, 3.01; 95% CI, 1.93–4.71 for those aged <25 years, compared with those aged ≥35); and study group (OR, 2.30; 95% CI, 1.52–3.49 for men visiting the STI clinic and OR, 1.91; 95% CI 1.24–2.94 for women visiting the STI clinic, both compared with women visiting the FP clinic), but not with ethnic sexual mixing (OR, 1.33; 95% CI, 0.96–1.85) and number of partners in the preceding 12 months (OR, 1.39; 95% CI, 0.92–2.11 for having >2 partners compared with having ≤1 partner) (Table 2).
Table 2. Univariable and multivariable logistic regression analyses of determinants associated with chlamydia among the study population included at two sites in Paramaribo, Suriname, 2008–2010.
| NAATpositive | UnivariableOR (95%CI) | P value | MultivariableAdjusted OR(95%CI)* | P value | ||
| 224/1508 (14.9) | ||||||
| n/N (%) | ||||||
| Study group | Family planning clinic – women | 78/819 (9.5) | 1 | <0.001 | 1 | <0.001 |
| STI clinic – women | 51/274 (18.6) | 2.17 (1.48–3.19) | 1.91 (1.24–2.94) | |||
| STI clinic – men | 95/415 (22.9) | 2.82 (2.03–3.91) | 2.30 (1.52–3.49) | |||
| Age in years | <25 | 90/398 (22.6) | 3.36 (2.22–5.08) | <0.001 | 3.01 (1.93–4.71) | <0.001 |
| 25–29 | 71/381 (18.6) | 2.63 (1.72–4.04) | 2.60 (1.65–4.09) | |||
| 30–34 | 27/279 (9.7) | 1.23 (0.73–2.08) | 1.26 (0.73–2.18) | |||
| > = 35 | 36/450 (8.0) | 1 | 1 | |||
| Education | Low | 96/611 (15.7) | 1 | 0.878 | ||
| Medium | 93/647 (14.4) | 0.90 (0.66–1.23) | ||||
| High | 27/197 (13.7) | 0.85 (0.54–1.35) | ||||
| Unknown | 8/53 (15.1) | 0.95 (0.44–2.09) | ||||
| Ethnic group | Creole | 87/444 (19.6) | 3.11 (1.88–5.14) | 0.001 | 1.76 (1.03–3.00) | 0.027 |
| Hindustani | 21/289 (7.3) | 1 | 1 | |||
| Javanese | 28/177 (15.8) | 2.40 (1.32–4.37) | 2.05 (1.09–3.84) | |||
| Maroon | 36/258 (14.0) | 2.07 (1.17–3.65) | 0.96 (0.52–1.78) | |||
| Mixed | 44/277 (15.9) | 2.41 (1.39–4.17) | 1.33 (0.72–2.35) | |||
| Othera | 7/57 (12.3) | 1.79 (0.72–4.43) | 1.01 (0.38–2.67) | |||
| Ethnic sexual mixing | Had only sexual partnersfrom same ethnic group | 88/790 (11.1) | 1 | <0.001 | 1 | 0.090 |
| Had at least one sexual partnerfrom another ethnic group | 125/643 (19.4) | 1.93 (1.43–2.59) | 1.33 (0.96–1.85) | |||
| Condom use | Always | 45/281 (16.0) | 1 | 0.529 | ||
| Never or inconsistent | 176/1211 (14.5) | 0.89 (0.62–1.27) | ||||
| Number of partners in thepreceding month | 0 | 8/72 (11.1) | 1 | <0.001 | ||
| 1 | 152/1154 (13.2) | 1.21 (0.57–2.58) | ||||
| >1 | 58/248 (23.4) | 2.44 (1.11–5.39) | ||||
| Number of partners in thepreceding 12 months | ≤1 | 104/918 (11.3) | 1 | <0.001 | 1 | 0.225 |
| 2 | 49/286 (17.1) | 1.62 (1.12–2.34) | 1.33 (0.88–2.01) | |||
| >2 | 71/304 (23.4) | 2.39 (1.71–3.33) | 1.39 (0.92–2.11) | |||
| Sex in exchange formoney or goods | No | 207/1424 (14.5) | 1 | 0.166 | ||
| Yes | 13/62 (21.0) | 1.56 (0.83–2.93) |
ORs in the multivariable model are adjusted for all factors for which adjusted ORs are shown.
Other: Caucasian, Chinese, Indigenous.
NAAT, nucleic acid amplification test; OR, odds ratio; 95%CI, 95% confidence interval.
The interactions between study group and all other variables in the final model and the interaction between the number of partners in the preceding 12 months and ethnic sexual mixing were not significant.
Sexual Mixing among Ethnic Groups
A total of 643 participants (43.6%) reported sexual mixing with other ethnic groups, and 790 (52.4%) did not report any sexual mixing. Ethnic sexual mixing differed between ethnic groups. Of the Hindustani 65 (23.5%) reported sexual mixing. This was higher for individuals with Creole (n = 191; 44.3%), Javanese (n = 85; 49.4%), Maroon (n = 95; 38.6%), or mixed race (n = 170; 65.9%) ethnicity (P<0.001). In multivariable analysis, adjusting for number of partners in the preceding 12 months, sex in exchange for money or goods, and study group, ethnic sexual mixing was significantly associated with ethnic group (OR, 1.87; 95% CI, 1.30–2.70 for Creoles; OR, 3.34; 95% CI, 2.18–5.11 for Javanese; OR, 1.15; 95% CI, 0.75–1.76 for Maroon; OR, 4.88; 95% CI, 3.26–7.30 for mixed race; all compared with Hindustani).
Table 3 shows the ethnic groups of the participants included in the study and the observed and expected ethnic background of their partners. Of the Creole, Hindustani, Javanese and Maroon participants between 60.5% and 77.9% reported to have had sex with a partner of their own ethnicity; for mixed race individuals this was 44.4%. Maroon individuals were more likely to have a partner with a Creole ethnicity (29.8%) compared with a partner with a Hindustani (3.1%) or Javanese ethnicity (3.9%). Likewise, only 1% of the Hindustani and Javanese individuals reported sex with a Maroon partner. The observed frequencies of only having sexual partners from participants’ own ethnicity were significantly higher than expected frequencies if partners had been selected from the population at random with respect to ethnicity (P<0.001 for all 5 major ethnic groups).
Table 3. Ethnic sexual mixing patterns of men and women, Paramaribo, Suriname, 2008 to 2010.
| Ethnic group of sexual partner | ||||||||||
| Creole partner | Hindustani partner | Javanese partner | Maroon partner | Mixed race partner | ||||||
| O | E | O | E | O | E | O | E | O | E | |
| n (%) | n (%) | n (%) | n (%) | n (%) | ||||||
| Ethnic group of study participants | ||||||||||
| Creole (n = 444) | 314 (70.7) | 157 | 26 (5.9) | 104 | 29 (6.5) | 60 | 51 (11.5) | 80 | 99 (22.3) | 99 |
| Hindustani (n = 289) | 20 (6.9) | 103 | 225 (77.9) | 68 | 14 (4.8) | 39 | 3 (1.0) | 52 | 32 (11.1) | 65 |
| Javanese (n = 177) | 12 (6.8) | 63 | 28 (15.9) | 41 | 107 (60.5) | 24 | 1 (0.6) | 32 | 43 (24.3) | 40 |
| Maroon (n = 258) | 77 (29.8) | 91 | 8 (3.1) | 60 | 10 (3.9) | 35 | 196 (76.0) | 47 | 25 (9.7) | 58 |
| Mixed (n = 277) | 93 (33.6) | 98 | 53 (19.1) | 65 | 39 (14.1) | 37 | 17 (6.1) | 50 | 123 (44.4) | 62 |
| Other (n = 63)a | 19 (30.2) | 22 | 13 (20.6) | 15 | 4 (6.3) | 9 | 4 (6.3) | 11 | 16 (25.3) | 14 |
| Total | 535 | 534 | 353 | 353 | 203 | 204 | 272 | 272 | 338 | 338 |
| O/E | 2.0 | 3.3 | 4.5 | 4.2 | 2.0 | |||||
| ?2 = 268, p<0.001 | ?2 = 472, p<0.001 | ?2 = 339, p<0.001 | ?2 = 585, p<0.001 | ?2 = 96, p<0.001 | ||||||
Percentages in row totals can exceed 100% as participants may have partners from various ethnicities.
O = observed; E = expected. χ2 based on goodness of fit.
The expected number of people with sexual partners from their own ethnicity was calculated by multiplying the total number of reported partners of an ethnicity (e.g. n = 353 for Hindustani) by the proportion of individuals from each ethnicity in the study (e.g. 19% for Hindustani). O/E is the ratio of the observed number of partners (e.g. n = 225 for Hindustani) divided by the expected number of partners from that ethnic group (e.g. n = 68 for Hindustani).
Other; Caucasian, Chinese, Indigenous (n = 57), unknown (n = 6).
Genovar Typing and MLST
We were able to type 170 samples of the 224 C. trachomatis positive samples (75.9%). The strains belonged to nine ompA genovars, predominantly E (32.4%), F (19.4%), D (18.2%) and I (12.9%). Furthermore, J (5.9%), G (5.3%), K (2.9%), B (1.8%), and H (1.2%) were found.
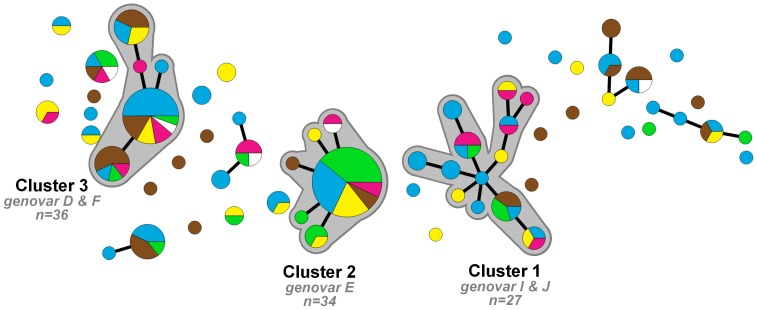
Among the 170 fully typed samples, we identified 65 different MLST profiles of which 32 (49%) were novel when checked against the MLST database on January 8, 2013. These novel MLST profiles were found in 52 (31%) of 170 samples. A minimum spanning tree was generated using MLST profiles (Figure 1) in which three large distinct clusters of C. trachomatis strains could be identified. Cluster 1 consisted of 27 samples (genovars I (81.5%) and J (18.5%)), cluster 2 consisted of 34 samples (all genovar E) and cluster 3 consisted of 36 samples (genovars D (23.5%) and F (76.5%)). There were 13 smaller clusters (containing 2–10 samples) and 20 singletons.
Figure 1. Minimum spanning tree of 170 Chlamydia trachomatis positive samples in Paramaribo, Suriname 2008–2010.
Each circle represents one MLST type. Size of the circles is proportional to the number of identical MLST profiles. Bold lines connect types that differ by one single locus. Halos indicate the three large distinct clusters (≥27 samples). Colors indicate ethnicity; blue – Creole, brown – mixed race, green – Javanese, yellow – Maroon, pink – Hindustani, white – Indigenous Amerindian, Caucasian and unknown.
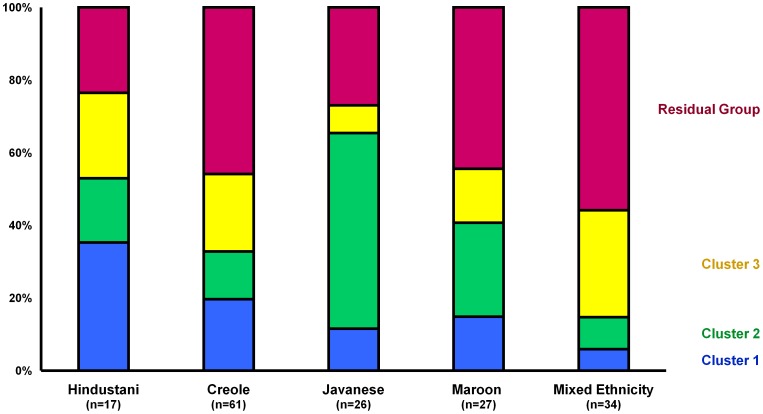
Although all five major ethnic groups were represented in all three clusters, the proportion from various ethnic groups differed significantly between the three clusters (P = 0.003). Figure 2 shows the distribution of individuals in each cluster for each ethnic group. Individuals with Javanese ethnicity were mainly found in cluster 2 (53.8%). Of the Hindustani, 35.1% belonged to cluster 1. Of the Creole and mixed race individuals 45.9% and 55.9%, respectively, were found outside the three main clusters of C. trachomatis strains.
Figure 2. Distribution of individuals in Chlamydia trachomatis clusters within ethnic groups in Paramaribo, Suriname, 2008–2010.
Colors indicate cluster: Blue – cluster 1; Green – cluster 2; Yellow – cluster 3; Pink – residual group.
Discussion
Prevalence of Chlamydia in Suriname
This is the first report on epidemiology of chlamydia in Suriname in both a high-risk and a low-risk population. Previously, we described the high prevalence of 9% and 21% respectively among low-risk and high-risk Surinamese women [7]; here we report a very high prevalence of 23% among high-risk Surinamese men. The high prevalence found in Suriname in our study can partly be attributed to the current lack of screening facilities in Suriname. The prevalence among women visiting the FP clinic was comparable to that reported by a recent study in the Caribbean region among women in the general population [5]. Another study in the region among women who were referred for a genital infection, presumably a high-risk group for chlamydia, reported a prevalence of 11% [4], and among pregnant women a prevalence of 21% was found [6]. Studies among STI clinic visitors in the Caribbean region are scarce, but a study in Jamaica from 1999, in which chlamydia was tested by direct fluorescence assay and culture (which are now considered obsolete diagnostics), reported a prevalence of 55% [23]. The high prevalence found in low- or middle-income countries indicates the urgent need for reliable and affordable diagnostics, preferably a point-of-care test. The prevalence found among the STI clinic visitors is likely to be higher than the prevalence in the Surinamese general population. Furthermore, despite the high response rate, the included and excluded women visiting the STI clinic differed by ethnicity and the reported prevalence should be interpreted as the prevalence among those who were tested and might not reflect the ‘true’ prevalence. The response rate among the population attending the FP clinic was very high and the prevalence may be a reasonable reflection of the sexually active Surinamese population. The higher prevalence indicates that preventive measures focused on the sexually active population in general are urgently necessary. Our study showed that the younger age group was disproportionately affected by chlamydia, so targeting prevention at this group seems most cost-effective, especially since safe sex messages probably will be more effective at sexual debut [9].
Prevalence of Chlamydia among Ethnic Groups
The Creole and Javanese groups seemed more affected by chlamydia compared with the Hindustani. A study from Trinidad and Tobago performed in 2004 compared three ethnic groups (African, East Indian and mixed race) using univariable analysis and found that individuals of East Indian descent were less likely to be infected with chlamydia compared with those of African descent [6]. Compared with Trinidad and Tobago, a society characterized by two dominant ethnic groups, Surinamese society is much more ethnically diverse. Since the prevalence in all but one ethnic group was above 12%, testing and treatment of all groups is required. The distribution of ethnic groups included in our study was approximating a correct representation of the actual Surinamese population according to the 2004 population census [8], although our study included more Creole and mixed race individuals and less people with Hindustani ethnicity.
Chlamydia and Sexual Mixing among Ethnic Groups
Previously it was found that sexual mixing patterns could be important for dynamics of the spread of STI [24]. Here we show that the frequency of having only sexual partners from participants’ own ethnicity was higher than expected if partners would have been selected regardless of ethnicity (i.e. assortative mixing). On the other hand, almost half of the study population reported ethnic sexual mixing, which showed that bridges between the ethnic groups do exist. Ethnic sexual mixing differed per ethnic group and was highest for mixed race individuals followed by Javanese and Creoles. Nevertheless, this sexual mixing was not associated with chlamydia, which is in line with a study among immigrants in the Netherlands where ethnic sexual mixing was not associated with self-reported STI [25]. One study on ethnic mixing of Surinamese immigrants in the Netherlands showed that Hindu-Surinamese individuals were more likely to mix than Afro-Surinamese individuals [26], which is in contrast to our data derived from Suriname. In the Dutch study among Surinamese migrants, eight times more Afro-Surinamese individuals were included than Hindu-Surinamese individuals [26]. Population size and the size of the ethnic group are of importance for the likelihood of ethnic sexual mixing and might explain the difference between the studies. Hindu-Surinamese migrants in the Netherlands might be more likely to meet individuals from different ethnicities, and therefore more likely engage in ethnic sexual mixing.
Besides the epidemiological characterization of ethnic sexual mixing, we used MLST typing to identify pathogen-associated networks among participants with chlamydia. Previously ompA genovar typing has been used [27] but MLST was found to be more discriminative and provides more solid proof of independent circulation [17]. Furthermore MLST is less affected by intragenic recombination of C. trachomatis, than typing based on only the ompA gene is [28]. MLST revealed that all major ethnic groups were represented in all three clusters of C. trachomatis strains, which suggests that these strains circulate endemically among all ethnic groups. Although the distribution of clusters within each group varied, clear separate networks for C. trachomatis transmission by ethnicity could not be identified which can be explained by ethnic sexual mixing between the groups. The typing results were in agreement with the epidemiological data. In contrast, studies comparing non-mixing populations (heterosexuals and MSM) showed hardly any overlap in chlamydial strains [16], [17]. In our study we could not distinguish separate networks between MSM and heterosexuals as only 7 MSM were included of whom only one had chlamydia and the provided sample could not be typed by MLST.
By checking the MLST profiles in the international C. trachomatis database, 32 (49%) novel strains were found. This database has existed since 2007 and comprises 459 profiles to date. It is most likely that many novel strains will be found. The database will expand and include an increasingly wide variety of C. trachomatis strains from different parts of the world. Combining the molecular data with epidemiological characteristics will provide more insight into global C. trachomatis transmission networks.
Several potential limitations should be mentioned. In our study differences in prevalence of chlamydia between ethnic groups were found, but we were not able to elucidate why these differences exist between ethnic groups. Therefore, additional risk behavior data are necessary. For example, concurrency is an important factor in the spread of HIV/STI [29] and is not uncommon among Surinamese individuals [26], [30], [31]. Also, we did not have information on other partner characteristics besides ethnic group such as age, type of partner (regular or casual), or condom use with different partners. Mathematical transmission models could be of added value to better identify sexual networks. Participants were interviewed face to face by a research nurse. Therefore, they may have given socially desirable answers and response bias may have occurred. Such bias might have occurred for variables such as condom use and number of sexual partners and would probably have resulted in an underestimation of risk behavior. Furthermore, ethnicity of the partner was self-reported and misclassification cannot be excluded.
In conclusion, the prevalence of chlamydia in Suriname is very high, with 10% in a low-risk population and up to 23% in a high-risk population. This prevalence is high overall in all ethnic groups (>7%), but higher in the Creole and Javanese groups compared with the Hindustani population. Although a high degree of sexual mixing occurs between the ethnic groups, having sex with a partner of the same ethnic group was more common than would be expected if partner selection occurred regardless of ethnic group. Nevertheless, based on the MLST typing analysis there is no sound evidence for separate ethnic sexual transmission networks and differences in prevalence of chlamydia between ethnic groups could not be explained by ethnic sexual mixing patterns. Prevention activities must rather be targeted at the whole community at risk, with a focus on the younger age groups. Adequate testing facilities and subsequent treatment are needed to reduce the disease burden of chlamydia in Suriname.
Acknowledgments
The authors would like to thank all nurses and laboratory technicians of the Dermatological Service and the Lobi Foundation for data collection; Ronald Geskus for critically reading the manuscript, and Claire Buswell for editing the final manuscript.
Funding Statement
This work was supported by the Research and Development fund of the Public Health Service of Amsterdam (project no 2369 and 2371) and AGIS healthcare insurance (RVVZ no 1417000). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization (2001) Global prevalence and incidence of selected curable sexually transmitted infections: Overview and estimates. Geneva, Switzerland: World Health Organization.
- 2. Farley TA, Cohen DA, Elkins W (2003) Asymptomatic sexually transmitted diseases: the case for screening. Prev Med 36: 502–509. [DOI] [PubMed] [Google Scholar]
- 3. Land JA, van Bergen JE, Morre SA, Postma MJ (2010) Epidemiology of Chlamydia trachomatis infection in women and the cost-effectiveness of screening. Hum Reprod Update 16: 189–204. [DOI] [PubMed] [Google Scholar]
- 4. Weill FX, Le Hello S, Clerc M, Scribans C, de Barbeyrac B (2010) Serological reactivity and bacterial genotypes in Chlamydia trachomatis urogenital infections in Guadeloupe, French West Indies. Sex Transm Infect 86: 101–105. [DOI] [PubMed] [Google Scholar]
- 5. Adams OP, Carter AO, Prussia P, McIntyre G, Branch SL (2008) Risk behaviour, healthcare access and prevalence of infection with Chlamydia trachomatis and Neisseria gonorrhoeae in a population-based sample of adults in Barbados. Sex Transm Infect 84: 192–194. [DOI] [PubMed] [Google Scholar]
- 6. Rampersad J, Wang X, Gayadeen H, Ramsewak S, Ammons D (2007) In-house polymerase chain reaction for affordable and sustainable Chlamydia trachomatis detection in Trinidad and Tobago. Rev Panam Salud Publica 22: 317–322. [DOI] [PubMed] [Google Scholar]
- 7. van der Helm JJ, Sabajo LO, Grunberg AW, Morre SA, Speksnijder AG, et al. (2012) Point-of-Care Test for Detection of Urogenital Chlamydia in Women Shows Low Sensitivity. A Performance Evaluation Study in Two Clinics in Suriname. PLoS One 7: e32122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Website Government Suriname. Available: http://www.gov.sr/sr/over-suriname/demografie.aspx. Accessed 2013 Jun 6.
- 9.Botman M, Sanches P (2008) [From Punta Woi and John the Baptist to put those Boegroes in me! Sexuality and eroticism in Suriname. OSO Journal for Surinamistics and the Caribbean Region. 2008 volume 27.1]. Van Punta Woi en Johannes de Doper tot Boegroe ing gi mi! Sexualiteit en erotiek in Suriname. OSO Tijdschrift voor Surinamistiek en het Caraïbisch gebied, jaargang 27.1.
- 10.Wekker G (2008) [Looking for Surinamese sexuality. During the day you hassle me, but at night you want sexual intimacy. OSO Journal for Surinamistics and the Caribbean Region. 2008 volume 27.1]. Op zoek naar Surinaamse seksualiteit. Overdag scheld je me schandalig uit, maar ‘s nachts wil je seksuele intimiteit. OSO Tijdschrift voor Surinamistiek en het Caraïbisch gebied, jaargang 27.1.
- 11. Choudhury B, Risley CL, Ghani AC, Bishop CJ, Ward H, et al. (2006) Identification of individuals with gonorrhoea within sexual networks: a population-based study. Lancet 368: 139–146. [DOI] [PubMed] [Google Scholar]
- 12. Klint M, Fuxelius HH, Goldkuhl RR, Skarin H, Rutemark C, et al. (2007) High-resolution genotyping of Chlamydia trachomatis strains by multilocus sequence analysis. J Clin Microbiol 45: 1410–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bom RJ, Christerson L, Schim van der Loeff MF, Coutinho RA, Herrmann B, et al. (2011) Evaluation of high-resolution typing methods for Chlamydia trachomatis in samples from heterosexual couples. J Clin Microbiol 49: 2844–2853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Christerson L, de Vries HJ, Klint M, Herrmann B, Morre SA (2011) Multilocus sequence typing of urogenital Chlamydia trachomatis from patients with different degrees of clinical symptoms. Sex Transm Dis 38: 490–494. [DOI] [PubMed] [Google Scholar]
- 15. Gravningen K, Christerson L, Furberg AS, Simonsen GS, Odman K, et al. (2012) Multilocus sequence typing of genital Chlamydia trachomatis in Norway reveals multiple new sequence types and a large genetic diversity. PLoS One 7: e34452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Christerson L, Bom RJ, Bruisten SM, Yass R, Hardick J, et al. (2012) Chlamydia trachomatis strains show specific clustering for men who have sex with men compared to heterosexual populations in Sweden, the Netherlands, and the United States. J Clin Microbiol 50: 3548–3555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bom RJ, van der Helm JJ, Schim van der Loeff MF, van Rooijen MS, Heijman T, et al. (2013) Distinct Transmission Networks of Chlamydia trachomatis in Men Who Have Sex with Men and Heterosexual Adults in Amsterdam, The Netherlands. PLoS One 8: e53869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Quint KD, Bom RJ, Bruisten SM, van Doorn LJ, Nassir HN, et al. (2010) Comparison of three genotyping methods to identify Chlamydia trachomatis genotypes in positive men and women. Mol Cell Probes 24: 266–270. [DOI] [PubMed] [Google Scholar]
- 19. Quint KD, Bom RJ, Quint WG, Bruisten SM, Schim van der Loeff MF, et al. (2011) Anal infections with concomitant Chlamydia trachomatis genotypes among men who have sex with men in Amsterdam, the Netherlands. BMC Infect Dis 11: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dicker LW, Mosure DJ, Levine WC (1998) Chlamydia positivity versus prevalence. What’s the difference? Sex Transm Dis 25: 251–253. [DOI] [PubMed] [Google Scholar]
- 21. Norman J (2002) Epidemiology of female genital Chlamydia trachomatis infections. Best Pract Res Clin Obstet Gynaecol 16: 775–787. [DOI] [PubMed] [Google Scholar]
- 22. Doerner R, McKeown E, Nelson S, Anderson J, Low N, et al. (2012) Sexual mixing and HIV risk among ethnic minority MSM in Britain. AIDS Behav 16: 2033–2041. [DOI] [PubMed] [Google Scholar]
- 23. Dowe G, Smikle M, King SD, Wynter H, Frederick J, et al. (1999) High prevalence of genital Chlamydia trachomatis infection in women presenting in different clinical settings in Jamaica: implications for control strategies. Sex Transm Infect 75: 412–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Aral SO, Hughes JP, Stoner B, Whittington W, Handsfield HH, et al. (1999) Sexual mixing patterns in the spread of gonococcal and chlamydial infections. Am J Public Health 89: 825–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. van Veen MG, Kramer MA, Op de Coul EL, van Leeuwen AP, de Zwart O, et al. (2009) Disassortative sexual mixing among migrant populations in The Netherlands: a potential for HIV/STI transmission? AIDS Care 21: 683–691. [DOI] [PubMed] [Google Scholar]
- 26. Gras MJ, Weide JF, Langendam MW, Coutinho RA, van den Hoek A (1999) HIV prevalence, sexual risk behaviour and sexual mixing patterns among migrants in Amsterdam, The Netherlands. AIDS 13: 1953–1962. [DOI] [PubMed] [Google Scholar]
- 27. Geisler WM, Suchland RJ, Stamm WE (2006) Association of Chlamydia trachomatis Serovar Ia infection with black race in a sexually transmitted diseases clinic patient population in Birmingham, Alabama. Sex Transm Dis 33: 621–624. [DOI] [PubMed] [Google Scholar]
- 28.Harris SR, Clarke IN, Seth-Smith HM, Solomon AW, Cutcliffe LT, et al.. (2012) Whole-genome analysis of diverse Chlamydia trachomatis strains identifies phylogenetic relationships masked by current clinical typing. Nat Genet 44: 413–9, S1. [DOI] [PMC free article] [PubMed]
- 29. Morris M, Kretzschmar M (1997) Concurrent partnerships and the spread of HIV. AIDS 11: 641–648. [DOI] [PubMed] [Google Scholar]
- 30.Terborg JRH (2001) Sexual behaviour and sexually transmitted diseases among the Saramaka and Ndjuka Maroons in the hinterland of Suriname. Paramaribo: ProHealth & Primary Health Care Suriname. 28–36.
- 31. van Veen MG, Schaalma H, van Leeuwen AP, Prins M, de Zwart O, et al. (2011) Concurrent partnerships and sexual risk taking among African and Caribbean migrant populations in the Netherlands. Int J STD AIDS 22: 245–250. [DOI] [PubMed] [Google Scholar]