Abstract
Background
Nurses in skilled nursing facilities (SNFs) play a key role in initiating/transitioning care for the >5 million patients who transition from hospitals-to-SNFs annually. Although hospital discharge processes are well studied, little is known about the SNF nursing processes or the SNF-based consequences of variation in transitional care quality.
Objective
To examine how SNF nurses transition the care of patients admitted from hospitals, the barriers they experience, and the outcomes associated with variation in the quality of transitions.
Design
Qualitative study using grounded dimensional analysis, focus groups and in-depth interviews.
Setting
5 Wisconsin SNFs.
Participants
27 registered nurses.
Results
SNF nurses rely heavily on written hospital discharge communication to effectively transition patients into the SNF. Nurses cited multiple inadequacies of hospital discharge information, including regular problems with medication orders (including the lack of opioid prescriptions for pain), little patient psychosocial/functional history, and inaccurate information regarding current health status. These communication inadequacies necessitated repeated phone clarifications, created care delays (including delays in pain control), increased SNF staff stress, frustrated patients/family members, directly contributed to negative SNF facility image, and increased a patient's rehospitalization risk. SNF nurses identified a specific list of information/components that they need to facilitate a safe, high-quality transition.
Conclusion
Nurses note multiple deficiencies in hospital-to-SNF transitions, with poor quality discharge communication being identified as the major barrier to safe and effective transitions. This information should be used to refine and support the dissemination of evidence-based interventions which support transitions of care, including the Interventions to Reduce Acute Care Transfers II (INTERACT) program.
Keywords: Care Transitions, Communication, Hospital to Skilled Nursing Facility
INTRODUCTION
Greater than 5 million patients transition from hospitals to skilled nursing facilities (SNFs) annually, and the nurses in these SNFs typically play the primary role in both receiving and initiating these patients’ care1. Although hospital discharge processes and hospital discharge communications to primary care physicians have been well described2,3 almost no prior work has focused on the nursing processes or on the SNF-based patient or system consequences of variation in transitional care quality. This is a critical oversight in the field of transitional care research, especially since discharge to a SNF is one of the strongest predictors for experiencing a 30-day rehospitalization4,5. In order to design effective hospital-SNF transitional care interventions to reduce these rehospitalizations, the primary processes at the receiving end of these transitions must be better understood.
The objective of this study was to examine how SNF nurses transition the care of patients admitted from hospitals, the barriers they experience, and the outcomes associated with variation in the quality of transitions. This was accomplished through a qualitative approach, which analyzed highly detailed information obtained via focus groups and interviews with practicing SNF nurses. This work suggests that high-quality, complete discharge communication is vital to safe and effective hospital-SNF transitions.
METHODS
Research Design
A qualitative study was conducted using Grounded Dimensional Analysis (GDA), an alternative to grounded theory methodology6-8. Both methodologies share a Symbolic Interactionist foundation which focuses on exploring social processes by understanding the actions of individuals in the context of social systems9. GDA utilizes a systematic analytic process to generate knowledge about conditions associated with variation in individuals’ socially-constructed understandings and actions in order to identify consequences of these variations7,10. GDA is not a consensus-building methodology, but rather focuses on the variation inherent in many real-world social processes, such as hospital-SNF transitions where clinical decision-making rarely follows a uniform pattern and may involve a wide variety of social/disciplinary groups (e.g., nursing, social work, medicine).
The end product of GDA is a conceptual model capable of explaining the primary components of the social process of interest. In this study, this was the process SNF nurses engage in when transitioning the care of patients from hospitals. The conceptual model elucidates how the components relate to one another and whether certain conditions and outcomes are associated with variation in the process. To construct a conceptual model with sufficient detail to inform clinical practice, GDA dictates the use of in-depth interviews and/or observations to facilitate the linking of conditions and outcomes with processes10.
Setting and Participants
Between June 2011 and February 2012, data were collected from 27 registered nurses representing 5 SNFs in 3 Wisconsin counties. Facility characteristics are described in Table 1.
Table 1.
Participating Skilled Nursing Facility Characteristics
| Facility | Ownership Type | Rural/Urban | Continuing Care Retirement Community | Resident Bed (#) | Nurses per Skilled Nursing Facility |
|---|---|---|---|---|---|
| 1 | Non-Profit Religious | Urban | Yes | 140 | 6 |
| 2 | Non-Profit Religious | Rural | No | 97 | 7 |
| 3 | Non-Profit Religious | Urban | Yes | 42 | 1 |
| 4 | Government | Rural | No | 104 | 4 |
| 5 | Non-Profit Religious | Urban | No | 184 | 9 |
aContinuing Care Retirement Community (CCRC) is an institution that offers independent living and skilled nursing facilities that accommodate an aging residents’ needs
Nurses were recruited in coordination with each facility's Director of Nursing through (1) announcements at facility staff meetings, (2) distribution of flyers on-site, and (3) e-mail announcements. In GDA, subject characteristics are driven exclusively by dimensions that are salient to the categories that emerge from the data. Therefore, this study did not systematically gather demographic characteristics on nurses. Interviews were conducted in a separate closed office space at the nurses’ places of work or at the University to maintain privacy. No interviews occurred during paid work time. Each participant received an honorarium of $30 per hour for interview participation. The study was approved by the University of Wisconsin-Madison Institutional Review Board.
Data Collection, Analysis
In-depth interviews were conducted either individually in focus groups (n=26) or individually (n=1). Interviews were audiotaped and transcribed verbatim. During GDA, data collection and analysis are both cyclic and concurrent. Following each interview/focus group, data were analyzed by the research team, and subsequent interview questions were developed. Concurrent data analysis also occurred during interviews through the modification of interview questions in order to maximize comparisons, an important analytic strategy of GDA. Analysis progressed through three phases: open coding, axial coding, and selective coding. Open coding involved line-by-line coding of data to examine how nurses understood hospital-to-SNF transitions, the actions they undertook as a result of their understandings, and whether conditions influenced their actions. Axial coding and selective coding developed the interrelationships among conditions and consequences associated with different components of the transition process. Throughout all phases of data collection and analysis, conceptual diagrams explicating the transition process underwent constant revision.
Analysis also occurred during interview sessions to facilitate ongoing constant comparative analysis, a fundamental analytic procedure of GDA10,11. Constant comparative analysis involves the pursuit of variability and complexity in the social process, and is often accomplished by exploring how nurses would respond to similar situations, provided different key variables. In this study, comparative analysis was accomplished by (1) identifying nurses with relevant experience, (2) constructing a social situation (the focus group) that allowed for dynamic comparisons between different social roles, (3) probing for variations in experiences and events within single nurses, and (4) modifying interview questions.
Several factors were considered in determining the appropriate sample size including: (1) the extent of saturation in the core social process, and (2) key data elements including the scope, quality, and complexity of the data12. Data generated in this study were rich, descriptive, complex, and somewhat broad in scope. Methodological strategies undertaken to maintain rigor and ensure accuracy of the conceptual model included the use of a multidisciplinary research team, member checking, and maintenance of memos.
RESULTS
Overall Quality of Hospital-to-SNF Transitions
From the perspective of SNF nurses, difficult hospital-to-SNF transitions were the norm, and when asked to recall the details of a good transition, none were able to do so. Nurses noted multiple deficiencies, with poor quality discharge communication being identified as the major barrier to safe and effective transitions. To facilitate a safe transition, SNF nurses needed specific, up-to-date information including descriptions of remarkable hospital events; written orders for medications, treatments, activity level and diet; recent and pending laboratory test results; accurate descriptions of functional and cognitive status; and pertinent social information such as preferences and unique needs (See Table 2 for a comprehensive list). Transition information came from three sources—the patient, the family and the hospital, with written hospital discharge information serving as the primary source. This study focused primarily on the process SNF nurses used to implement the medical, rather than social, plan of care, although nurses described both as important.
Table 2.
Hospital Discharge Information Needed by SNF Nurses to Develop and Implement a Safe Plan of Care
| Contact Information |
| Discharging unit & phone number |
| Attending MD & phone number |
| Other providers who will manage specific conditions (i.e., infections disease, anticoagulation) and contact information |
| RN who cared for patient & phone number |
| Spouse or partner & phone number |
| Family member(s) involved in care & phone number |
| Power of attorney - if activated & phone number |
| Past Medical History and Hospital Stay |
| Remarkable medical history |
| Remarkable events during hospital stay |
| Comorbidities |
| Code status |
| Medications |
| Discharge medication list |
| Drug name |
| Dose |
| Diagnosis/rationale for every medication |
| Start & stop dates/last dose administered |
| Opioid prescriptions (signed hard copy) |
| Significant medication changes |
| Change in psychiatric medications during stay |
| Change in opioid medication at discharge |
| Withdrawal of medication due to side effects |
| Allergies and Intolerances |
| Medications |
| Food |
| Latex |
| Functional Status |
| Ability and assistance required for ADLs |
| Sensory Aids (i.e., dentures, glasses, hearing aids) |
| Mobility status |
| Level of assistance needed |
| Equipment requirements |
| Fall risk |
| Psychosocial and Behavioral Concerns |
| Personal interests/communication preferences |
| Cognitive status |
| Behavioral symptoms related to dementia |
| Type and severity |
| Need for personal safety attendant during stay |
| Effective comforting/reorientation strategies |
| Treatments |
| Wound care |
| Dressing type |
| Dressing schedule |
| PICC line care |
| Dressing type |
| Dressing schedule |
| Flushing schedule |
| Elimination Status |
| Bladder or bowel incontinence |
| Use of absorbent pads |
| Perineal skin concerns |
| Last bowel movement |
| Type and amount of medication administered for bowel-related problems prior to discharge |
| Use of indwelling urinary catheter if and when discontinued |
| Nutritional Status |
| Swallowing or feeding concerns |
| Special eating devices |
| Appetite |
| Weight |
| Dentures |
| Follow Up Care |
| Scheduled appointments |
| Who |
| When |
| Where |
| Phone number |
| Laboratory tests |
| Pending results |
| Follow-up laboratory tests that need to be done |
| Insurance Information |
| Name & number of policy |
a Skilled Nursing Facility (SNF)
b Activities of Daily Living (ADLs)
c Peripherally Inserted Central Catheter (PICC)
Much of the information nurses needed from hospitals to design the medical plan of care was routinely missing/incomplete, conflicting, or discovered to be inaccurate upon the patient's arrival. As a result, nurses emphasized the importance of contact information of the discharging physician, nurses and therapists. Yet, this information was rarely provided. Attempts to contact hospital staff for clarification were described as frustrating and time-consuming, as hospital staff were often reluctant to reconcile discrepancies, could no longer access the patient's medical record, or were unable to locate a staff person with personal knowledge of the patient.
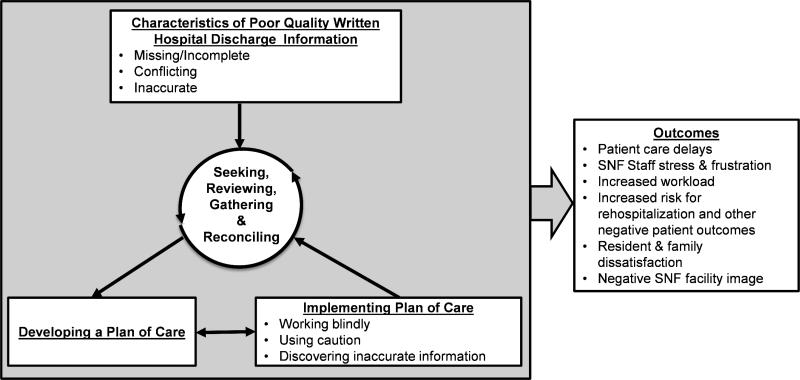
A conceptual model (Figure 1) was developed to illustrate the processes SNF nurses engage in when transitioning patients from hospitals. The model describes how characteristics of hospital discharge information drove the transition process (seeking, reviewing, gathering and reconciling information) and the consequences that missing/incomplete, conflicting and inaccurate information had on care delivery and patient outcomes. In describing the transition process nurses generally did not differentiate between returning SNF residents and residents who were new to the facility. When nurses had longitudinal knowledge of a resident however, they were sometimes able to identify inaccurate or missing information earlier in the transition process.
Figure 1.
A conceptual model of the process and outcomes associated with hospital to SNF transitions. A conceptual model developed to illustrate the processes SNF nurses engage in when transitioning patients from hospitals. The model describes how characteristics of hospital discharge information drove the transition process and the consequences that information had on care delivery and patient outcomes. Abbreviation: Skilled Nursing Facility (SNF).
Seeking, Reviewing, Gathering and Reconciling Hospital Information
Initial steps in the transition process were seeking and reviewing medical information from the hospital. Upon a patient's arrival, SNF nurses often received ‘reams’ of paper, which commonly exceeded 80 pages. Although much of this information was not relevant to designing the patient's plan of care (e.g., surgical flow sheets), SNF nurses usually had no other resource available to search for needed information. Nurses described spending hours sifting through masses of records and sometimes through the entire printed electronic health record (EHR) to piece together the hospital events. The tediousness of this process was exacerbated by variation in the amount, type and order of written information provided by hospitals.
In addition, nurses actively sought out information about prospective patients prior to their admission. This seeking was done to identify patients with “red flags,” which nurses defined as complex and demanding clinical needs, such as mechanical ventilation or challenging, dementia-related behavioral symptoms, which may not be a safe fit for their facility. Nurses stated that in their experience, red flags were often not communicated or under-emphasized by hospital staff because patients with such flags were difficult to place.
Inadequacies in hospital discharge information prompted a cyclic process of gathering and reconciling additional information in order to implement a safe and appropriate plan of care. Gathering and reconciling involved returning to the written discharge information sent by the hospital, or calling the primary care physician or a physician or nurse on the discharging hospital team. When called, primary care physicians were often unfamiliar with the patient's hospital stay and usually directed nurses back to hospital providers.
“The primary states... ‘I didn't know what happened at the hospital so I can't give you any orders...You need to call the hospitalist or whoever worked with them’.”
Reviewing written records often resulted in the discovery of additional information gaps and contradictions. These discoveries invariably led to additional information gathering to fill in the gaps and to reconcile conflicting information. As a result, the gathering and reconciling process typically took hours on the day of admission, and discrepancies/questions were often not reconciled for several days.
While nurses sometimes attempted to glean additional information by asking patients/families, this approach was problematic for several reasons: (1) patients/families were often not sufficiently informed to contribute useful information, (2) many patients had dementia and weren't able to provide information about their hospital stay or care needs, (3) asking patients/families to “fill in the gaps” created a poor first impression of SNF staff and the facility, and (4) since medical orders are legally binding, discrepancies within orders must be reconciled by a physician, nurse practitioner or physician assistant.
Nurses described instances when they did not have the information they needed as “working blindly.” Nurses also employed a strategy of “using caution” when care was perceived as potentially unsafe or informational sources appeared inaccurate. Nurses commonly discussed these situations as dangerous for patients and staff, especially in the case of “aggressive” behavioral symptoms.
Quality of Medical Information Sent from Hospitals
Missing and Incomplete Information
Basic information needed to transition patients into SNFs was consistent across patients/settings, yet such components (Table 2) were frequently absent in hospital discharge information. Missing/incomplete information resulted in care delays, which threatened patient safety and produced patient/family dissatisfaction with the transition process (See Table 3).
Table 3.
Characteristics of Hospital Discharge Information
| Categories | Description | Examples | Quotations |
|---|---|---|---|
| Missing/Incomplete | Necessary information that is omitted from discharge paperwork received by SNF nurses | • No wound care instructions provided for post-surgical patient • Medication orders missing important details • No signed prescription for controlled substances, especially opioids • No plans for medical follow-up |
“...there was nothing about the femur fractures we had no idea how, what, you know, if she was weight bearing or not weight bearing where-what we were supposed to be doing with them” |
| Conflicting | Discrepancies among written discharge documents | • Multiple medication lists and order sets which vary in content | “...we have three discharge summaries with all these different medications list, it just like, how are we safely supposed to take care of this patient...” |
| Inaccurate | Mismatch between the verbal or written report of the patient's condition from hospital and the SNF nurses assessment of patient's clinical presentation | • Mismatch between reported cognitive status and cognitive status • Activity orders reflect a different level of assistance than needed by resident • Resident presents as physiologically unstable |
“... a lot of the times we find when the person actually comes here they are a completely different picture than what we got in the pre-admission assessment.” (Focus Group 2, Subject 1) |
Conflicting Information
SNF nurses regularly discovered conflicting information, especially in medication lists. Conflicting information was identified when discrepancies were noted within and/or among the following sources: discharge paperwork/orders, hospital records, initial phone conversations and pre-existing medical orders.
Inaccurate Information
Inaccurate information was often in the form of a mismatch between the verbal report of the patient's condition from hospital staff and the patient's status on arrival. Most inaccuracies were in cognitive (i.e., agitation, dementia) or physical/physiological (i.e., functional status, muscle weakness, low blood pressure, high pulse, fever) status.
Consequences of Poor Quality Discharge Communication
Inadequate hospital discharge information/communication had a serious negative impact on patients/families, SNF staff and the SNF facility (Table 4).
Table 4.
Consequences of Poor Quality Discharge Communication for Patients/Families, Staff, and the Skilled Nursing Facility
| Group | Consequences | Example | Quotation |
|---|---|---|---|
| Patient and Family | • Care delays resulting from gathering/reconciling process and “working blindly” • Dissatisfaction with care quality and transition • Inappropriate care delivery • Increased rehospitalization risk • Increased risk for being untreated/undertreated for pain at time of transition • Patient safety compromised |
• Providing treatments such as wound care without specific orders • Delaying pain medications for several hours due to lack of signed opioid prescription • Not having necessary equipment for patient care on admission • Inappropriate care delivered leading to medication errors |
“We didn't know what her mobility...and we didn't know if she was weight bearing'... so we left her in bed, for probably a week” |
| SNF Staff | • Increased work- stress, frustration, feelings of inadequacy • Feeling unsafe in care delivery while “working blindly” • Feelings of guilt associated with patient harm • Additional work effort |
• Delivering care “blindly” while missing crucial information such as medication /activity orders • Unsuccessful attempts to clarify orders with multiple providers over the course of hours to days • Feeling guilt as a result of patient harm due to missing information regarding aggressive behavior |
“And as nurses you just feel like you're just asked to take care of this person with blinders on“ “I had to talk to like three people just to find out who the doctor was... Well then I called that office, he wasn't in. Nobody at the office could help me; it was like a week before we got some good information” |
| Facility | • Additional costs in staff time • Additional costs due to wasted resources • Decreased work satisfaction which may contribute to high turnover rates • Patient/family dissatisfaction with care, perpetuating a negative facility image |
• Paying a pharmacist overtime to drive from their home to fill an opioid prescription after hours • Ordering medications for a patient that are later discontinued without notification prior to transfer • Family feel that facility is unorganized and ill-equipped |
“It sends a terrible message to the patient and their family that we are ill prepared or that we are not capable of handling the acuity.” |
Consequences for Patients and Families
Missing/incomplete, conflicting and inaccurate information produced significant care delays due to the time-consuming process of gathering and reconciling information required to implement a safe plan of care. These delays were exacerbated by limitations inherent in the SNF environment, such as the lack of an on-site pharmacy and the need to special order equipment (e.g., specialty bed) days in advance.
“...we don't have a big central supply where we can just pick up the phone and say we need a bariatric bed... we have to rely on a rental company [causing] delays in care.”
Nurses noted that missing/incomplete or inaccurate information on activity level or orthopedic device care produced delays which put patients at increased risk for mobility issues and rehospitalization. Nurses described several occurrences when bed rest was enforced purely due to missing activity orders, because they did not know if the patient should ambulate. In one example a patient who had bilateral lower extremity casts was left in bed for one week as the SNF nurses repeatedly requested and waited for clarification of physical activity orders and cast care.
A very common and problematic care delay cited by nurses was the lack of signed, hard-copy opioid prescriptions, which are legally required to dispense controlled substances. It often took hours to obtain opioid prescription orders. Delays in pain treatment sometimes resulted in severe pain, especially for patients who did not receive a scheduled pain medication prior to leaving the hospital.
Another common challenge was the discovery of conflicting medication orders upon patient arrival. Nurses sometimes received discharge orders via fax prior to admission in order to prepare for the transition, but many medications changed immediately prior to discharge and these changes were not communicated before transferring the patient. As many SNFs did not have an on-site pharmacy, the new medications/treatments were often not readily available, thus, resulting in additional treatment delays. This was particularly problematic for late-in-the-day or weekend transfers as fewer resources were available.
Care delays and implementation of an inappropriate plan of care resulting from inaccurate information produced significant patient and family dissatisfaction and also made the SNF facility appear unorganized and ill-equipped to care for patients. This experience produced substantial stress and frustration among SNF nurses.
Consequences for SNF Staff and Facility
Nurses described feeling overwhelmed by the constant need to gather and reconcile information received from hospitals. This process is cyclic, inefficient, and extremely time-consuming. SNF nurses had little ability to influence what they perceived to be the primary driver of this process—inadequate discharge communication. Nurses described feeling that attempts to “demand” that hospitals supply discharge orders early in the day and communicate changes would not be productive and feared that hospitals would refer fewer patients to the facility.
“We used to demand... the discharge summaries from the hospitals the night before. And now hospitals are saying, ‘No, we refuse to do that. They'll come when we want them to come’.”
This process produced stress and frustration within other departments, such as Physical Therapy, because these groups also relied on timely and accurate discharge information to implement their care plans. SNF nurses assumed the primary responsibility and workload for obtaining, reviewing and reconciling all necessary information and for relaying the information to appropriate departments. This work spread across shifts as information needs were sequentially passed on while waiting for a clarifying call from the hospital or primary care provider to be returned.
Constant shifting of care strategies and the high level of vigilance necessitated by unclear care needs produced workflow disruptions and inefficiencies. These frustrations were exacerbated by the unresponsiveness, and sometimes hostile responses, from hospital staff. Nurses described hospital staff as often abandoning responsibility for discharged patients regardless of the urgency of the nurse's concern. Nurses commonly described calling multiple providers and “begging” for clarifications for discharge orders, which contributed to SNF nurse's feelings of inadequacy.
SNF nurses indicated that patients and family members interpret the consequences of poor quality discharge information as evidence that SNF staff “don't know what they are doing.” Continually revising the plan of care or being unable to respond to patient needs in a timely manner undermined trust and confidence of patients/families. This added to the stress and workload of all SNF staff, who then had to work even harder to re-establish trust and rapport with patients/families.
Suggestions for Improving Transitions
SNF nurses had several suggestions for improving transitions. First, they stated that hospitals need to communicate medical information at least 24 hours prior to SNF admission to ensure that needed medications and special equipment are available. Any changes to the plan also need to be immediately communicated at the time the change is made. Secondly, SNF nurses wanted to have immediate access to a prescribing provider with up-to-date knowledge of the patient as the patient is admitted to the SNF. Ideally, this provider would be able to clarify missing, inaccurate or conflicting information. Nurses from one participating SNF stated that their local community hospital provided phone access directly to the discharging hospitalist physician for 24 hours post-discharge, and that this arrangement greatly expedited the communication/clarification process. Finally, SNF nurses highlighted the need for more focused, standardized and complete communication of medical information as outlined in Table 2.
DISCUSSION
This study represents the first in-depth examination of SNF nurses’ work processes, perceived barriers and outcomes associated with variation in the quality of hospital-to-SNF transitions. Nurses described numerous safety concerns, inefficiencies and adverse patient and staff outcomes that commonly result from hospital-to-SNF transitions, with poor quality discharge communication identified as the major barrier to safe and effective transitions. The information nurses received from hospitals was virtually always described as being inadequate due to missing/incomplete, conflicting and inaccurate information. Poor quality discharge communication produced a cyclical, inefficient process of gathering and reconciling information. These attempts often took the form of repeated call backs to discharging hospitals, were time-consuming and led to delays in patient care, patient/family dissatisfaction, increased rehospitalization risk, increased staff stress/frustration, and perpetuation of a negative SNF facility image. Occasionally, poor quality discharge information directly led to inappropriate care, which compromised patient safety.
A lack of transitional care training among health professionals might contribute to poor quality discharge communication, and to some extent, might explain the limited responsiveness SNF nurses receive in attempts to reconcile inadequate information. Accreditation guidelines for physician and nursing training programs are vague in terms of the type or extent of transitional care training that they must provide13-15. Considering the lack of focus in these guidelines, nation-wide transitional care training is likely variable, and crucial topics, such as understanding the needs and resource limitations of non-hospital settings, may not be consistently addressed. A review of curricular interventions focused on transitional care found that only 32% included “introduction to care settings” as a learning objective16. This suggests that more detailed accreditation guidelines are needed to ensure that a minimum level of transitional care training and experience is included within all health professional training programs.
These findings also suggest that poor quality discharge communication might be directly related to patient outcomes such as rehospitalization. Discharge summaries are the primary (and sometimes only) document accompanying patients between care facilities and are the regular source for SNF admission orders2, 17-20. The frequent omissions of recommended components in discharge summaries found within prior research are consistent with the findings of this qualitative study2, 21, 22.
Although it is clear from this study that an overwhelming amount of written discharge data interferes with effective communication, SNF nurses felt that a minimum standard set of components (Table 2) would be necessary to ensure high-quality patient safety and care for newly admitted SNF patients. Hospital providers may view the SNF nurses’ requested component list as overly extensive or burdensome. However, these discharge communications can dictate SNF care for up to 30 days for some patients, especially those who do not see a prescribing provider until their 30-day Medicare SNF benefit recertification22 so their quality and completeness is critical. Also, with the advent of new EMR capabilities and the restructuring of health systems to focus on episodic care and population health (e.g., Accountable Care Organizations), innovative technologies and programs may soon be available to ease this burden on the discharging hospital provider, while generating a higher quality discharge communication which takes the needs of the end-user (e.g., SNF nurse) into account. The requested content list provided here can be utilized in the design of such innovative programs.
A number of existing interventions to improve care transitions could help to address this communication problem. Many of these transitional care interventions utilize nurse practitioners to bridge the gap between care settings soon after hospital discharge,23, 24 but these programs are not available in many areas and often exclude patients with dementia, an important SNF population. There is work being done at the national level to standardize information sharing across health systems, including the Continuity of Care Document (CCD),25 but the currently proposed document omits many of the informational components deemed as critical by SNF nurses and leaves issues of communication timing and clarification unaddressed. The Institute for Healthcare Improvement (IHI) and others have made important recommendations for improving care transitions,26 including direct nurse-to-nurse communication (i.e., “warm handoff”), but per the SNF nurses in this study, the quality and content of these handoffs is often poor. The Interventions to Reduce Acute Care Transfers II (INTERACT) program27 is a nursing home-based intervention which shows considerable promise for addressing this inter-setting communication problem, especially if the program were more widely disseminated. The most recent version of INTERACT includes multiple tools to help improve collaboration between hospitals and nursing homes, and the information offered within this study may inform further evolution of the program. The SNF nurses in this study offered a number of interventions that they thought would be helpful, but more work is needed to design, refine and disseminate nursing home-focused transitional care interventions. With the advent of payment penalties for hospitals with higher than average recidivism rates, there may be additional incentives for hospital systems to engage in partnerships with SNFs to improve the quality of transitional care.
This study has several limitations. The sample represents nurses working in geographically similar areas with a limited number of hospitals. Although these hospitals represent a variety of urban, rural, academic and community practice settings, they may not be representative of all hospitals nationwide. Furthermore, this study did not include for-profit nursing homes. Negative outcomes described by our nurses may be exaggerated in for-profit sites, which generally have lower staffing ratios28. This study examined transitions to SNFs only, and findings may not be generalizable to patients discharged to inpatient rehabilitation or other outpatient settings. No demographic information was collected on participating nurses, which limits our ability to interpret whether differences in work process might be related to educational training/background or past work experiences. Because no direct participant observation took place it is impossible to affirm, with certainty, how often nurses encounter deficiencies in the quality of information and how they respond to those situations. Future studies in this area are needed.
CONCLUSION
Nurses note multiple deficiencies in hospital-to-SNF transitions, with poor quality discharge communication being identified as the major barrier to safe and effective transitions. This information should be used to refine and support the dissemination of evidence-based interventions which support transitions of care, including INTERACT. Future research is needed to quantify the impact of poor discharge communication on patient outcomes.
ACKNOWLEDGMENTS
For “yes” x mark(s): give brief explanation below:
| Elements of Financial/Personal Conflicts | BJK | ALGB | RRR | BEP | BJB | AJHK | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | X | X | ||||||
| Grants/Funds | X | X | X | X | X | X | ||||||
| Honoraria | X | X | X | X | X | X | ||||||
| Speaker Forum | X | X | X | X | X | X | ||||||
| Consultant | X | X | X | X | X | X | ||||||
| Stocks | X | X | X | X | X | X | ||||||
| Royalties | X | X | X | X | X | X | ||||||
| Expert Testimony | X | X | X | X | X | X | ||||||
| Board Member | X | X | X | X | X | X | ||||||
| Patents | X | X | X | X | X | X | ||||||
| Personal Relationship | X | X | X | X | X | X | ||||||
*Authors can be listed by abbreviations of their names.
Funding Sources and Related Paper Presentations
This project was supported by the National Institute on Aging Paul B. Beeson Patient-Oriented Research Career Development Award (K23AG034551 [PI Kind]), in partnership with the American Federation for Aging Research, the John A. Hartford Foundation, the Atlantic Philanthropies, and the Starr Foundation and the Madison VA Geriatrics Research, Education and Clinical Center (GRECC-Manuscript #2013-05). Authors Roiland and Gilmore-Bykovskyi acknowledge the John A. Hartford Foundation Building Academic Geriatric Nursing Capacity Program for support. Author Roiland's contributions were supported by an F31 NRSA Award from the National Institute of Nursing Research (F31NR013097-01). Additional support was provided by the University of Wisconsin School of Medicine and Public Health's Health Innovation Program; the Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research; and the Clinical and Translational Science Award program of the National Center for Research Resources, National Institutes of Health (1UL1RR025011).The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The findings of this study have been selected for poster presentation at the annual meetings for the American Geriatrics Society, Gerontological Society of America, and Midwest Nursing Research Society.
Sponsor's Role: None.
Footnotes
Author Contributions: Barbara J. King made contributions to the design, acquisition, analysis and interpretation of data, drafting the article, and final approval of the version to be published. Andrea L. Gilmore-Bykovskyi made contributions to the design, analysis and interpretation of data, drafting and critical revision of the article, and final approval of the version to be published. Rachel R. Roiland made contributions to the acquisition, analysis and interpretation of data, drafting of the article, and final approval of the version to be published. Brock E Polnaszek made contributions to the acquisition and interpretation of data, critical revision of the article, and final approval of the version to be published. Barbara J. Bowers made contributions to the design, analysis and interpretation of data, critical revision of the article and approval of final version to be published. Amy J.H. Kind made contributions to the conception, design, analysis and interpretation of data, drafting and critical revision of the article and final approval of the version to be published. The authors would also like to acknowledge Peggy Munson for IRB assistance, Melissa Hovanes for project management and support, Kristen Pecanac for assistance with data analysis. The authors have obtained written consent from all contributors who are not authors and are named in this section.
REFERENCES
- 1.Mor V, Intrator O, Feng Z, et al. The revolving door of rehospitalization from skilled nursing facilities. Health Aff. 2010;29:57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: Implications for patient safety and continuity of care. J Am Med Assoc. 2007;297:831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 3.Schoenborn NL, Arbaje AI, Eubank KJ, et al. Clinician Roles and Responsibilities During Care Transitions of Older Adults. J Am Geriatr Soc. 2013 doi: 10.1111/jgs.12084. [DOI] [PubMed] [Google Scholar]
- 4.Kind AJ, Smith MA, Frytak JR, et al. Bouncing back: Patterns and predictors of complicated transitions 30 days after hospitalization for acute ischemic stroke. J Am Geriatr Soc. 2007;55:365–373. doi: 10.1111/j.1532-5415.2007.01091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kind AJ, Smith MA, Liou JI, et al. The price of bouncing back: one-year mortality and payments for acute stroke patients with 30-day bounce-backs. J Am Geriatr Soc. 2008;56:999–1005. doi: 10.1111/j.1532-5415.2008.01693.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bowers B, Schatzman L. Dimensional Analysis. In: Morse J, Stern P, Corbin J, et al., editors. Developing Grounded Theory: The Second Generation. Left Coast Press; 2008. [Google Scholar]
- 7.Kools S, McCarthy M, Durham R, et al. Dimensional Analysis: Broadening the Conception of Grounded Theory. Qualitative Health Research. 1996;6:312–330. [Google Scholar]
- 8.Schatzman L. Dimensional analysis: Notes on an alternative approach to grounding of theory in qualitative research. Aldine De Gruyter; New York: 1991. [Google Scholar]
- 9.Bowers B, Schatzman L. Developing Grounded Theory: The Second Generation. Left Coast Press; Walnut Creek, California: 2009. [Google Scholar]
- 10.Caron C, Bowers B. Methods and application of dimensional analysis: A contribution to concept and knowledge development in nursing. W.B. Saunders Co.; Philadelphia: 2000. [Google Scholar]
- 11.Strauss AL. Qualitative Analysis for Social Scientists. Cambridge University Press; Cambridge, UK: 1987. [Google Scholar]
- 12.Morse J. Determining sample size. Qualitative Health Research. 2000:3–5. [Google Scholar]
- 13.Liaison Committee on Medical Education [October 9, 2012];Function and Structure of a Medical School: Standards for Accrediting of Medical Education Programs Leading to the M.D. Degree. Available at: http://www.lcme.org/standard.htm.
- 14.American Association of Colleges of Nursing [October 9, 2012];The Essentials of Baccalaureate Education for Professional Nursing Practice. [Google Scholar]
- 15.Accreditation Council for Graduate Medical Education [October 9, 2012];Common Program Requirements. Available at: http://www.acgme-nas.org/assets/pdf/CPR-Categorization-TCC.pdf.
- 16.Buchanan IM, Besdine RW. A systematic review of curricular interventions teaching transitional care to physicians-in-training and physicians. Acad Med. 2011;86:628–639. doi: 10.1097/ACM.0b013e318212e36c. [DOI] [PubMed] [Google Scholar]
- 17.Kind A, Anderson P, Hind J, et al. Omission of dysphagia therapies in hospital discharge communications. Dysphagia. 2011;26:49–61. doi: 10.1007/s00455-009-9266-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kind A, Smith M. AHRQ Patient Safety: New Directions and Alternative Approaches. Agency for Healthcare Research and Quality; Rockville, MD: 2008. Documentation of Mandated Discharge Summary Components in Transitions from Acute to Sub-Acute Care. pp. 179–188. [PubMed] [Google Scholar]
- 19.Kind AJ, Thorpe CT, Sattin JA, et al. Provider characteristics, clinical-work processes and their relationship to discharge summary quality for sub-acute care patients. J Gen Intern Med. 2012;27:78–84. doi: 10.1007/s11606-011-1860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walz SE, Smith M, Cox E, et al. Pending laboratory tests and the hospital discharge summary in patients discharged to sub-acute care. J Gen Intern Med. 2011;26:393–398. doi: 10.1007/s11606-010-1583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Archives and Records Administration . Public Health -- Requirements for States and Long Term Care Facilities, 42 CFR 483. United States Government Printing Office; Washington, DC: 2012. [Google Scholar]
- 22.Dimant J. Roles and responsibilities of attending physicians in skilled nursing facilities. J Am Med Dir Assoc. 2003;4:231–243. doi: 10.1097/01.JAM.0000075915.15039.B1. [DOI] [PubMed] [Google Scholar]
- 23.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. J Am Med Assoc. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 24.Coleman EA, Smith JD, Frank JC, et al. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004;52:1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- 25.Agency for Healthcare Research and Quality [January 4, 2013];Prospects for care coordination measurement using electronic data sources: Challenges of measuring care coordination using electronic data and recommendations to address those challenges. Available at: http://www.ahrq.gov/qual/prospectscare/prospects1.htm.
- 26.Herndon L, Bones C, Kurapati S, et al. How-to Guide: Improving Transitions from the Hospital to Skilled Nursing Facilities to Reduce Avoidable Rehospitalizations. Institute for Healthcare Improvement; Cambridge, MA: 2012. [Google Scholar]
- 27.Florida Atlantic University [February 5, 2013];Interventions to Reduce Acute Care Transfers. Available at: https://www.interact2.net.
- 28.Harrington C, Olney B, Carrillo H, et al. Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies. Health Serv Res. 2012;47:106–128. doi: 10.1111/j.1475-6773.2011.01311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]