Abstract
STUDY DESIGN
Multivariate analysis of prospectively collected registry data
OBJECTIVE
To determine the affect of payor status on complication rates after spine surgery.
SUMMARY OF BACKGROUND DATA
Understanding the risk of perioperative complications is an essential aspect in improving patient outcomes. Previous studies have looked at complication rates after spine surgery and factors related to increased perioperative complications. In other areas of medicine, there has been a growing body of evidence gathered to evaluate the role of payor status on outcomes and complications. Several studies have found increased complication rates and inferior outcomes in the uninsured and Medicaid insured.
METHODS
The XX Registry (XX-XX) is a collection of prospectively collected data on all patients who underwent spine surgery at our two institutions. Extensive demographic data, including payor status, and medical information were prospectively recorded as described previously by Mirza et al. Medical complications were defined in detail a priori and were prospectively recorded for at least 2 years after surgery. Using univariate and multivariate analysis, we determined risk of postoperative medical complications dependent on payor status.
RESULTS
1591 patients underwent spine surgery in 2003 and 2004 that met our criteria and were included in our analysis. With the multivariate analysis and by controlling for age, patients whose insurer was Medicaid had a 1.68 odds ratio (95% CI: 1.23, 2.29, p=0.001) of having any adverse event when compared to the privately insured.
CONCLUSION
After univariate and multivariate analyses, Medicaid insurance status was found to be a risk factor for postoperative complications. This corresponds to an ever-growing body of medical literature that has shown similar trends and raises the concern of underinsurance.
Keywords: spine surgery, perioperative complications, complication rates, payor status, underinsurance, Medicaid, public insurance
INTRODUCTION
Understanding the risk of perioperative complications is an essential aspect in improving patient outcomes. Enhanced knowledge of the risks associated with increased complications in spine surgery has been an area of increased interest. Numerous studies employing various study design methods have examined complications after spine surgery.1–14 More recent work has focused on the importance of data collected in a prospective manner to most accurately determine rate of perioperative complications and risk factors most associated with perioperative complications.3,4,10 Validating the Spine Adverse Events Severity system first described by Rampersaud et al.15, Street et al. used prospectively collected data on 942 patients and have shown that major spine surgery is associated with “…a very high rate of previously unrecognized postoperative complications.”10 Other studies have previously reported a multivariate analysis on prospectively collected data to show medical comorbidities and other factors most associated with perioperative complications.3,4
The Spine End Results Registry (2003–2004) is a registry of prospectively collected data of all patients undergoing spinal surgery at the University of XXXX Medical Center and XXXX Medical Center. Detailed information regarding patient demographics, insurance status, medical comorbidity, surgical invasiveness, and adverse occurrences were followed for up to two years and obtained prospectively using earlier published methods.16,17 Although insurance data were prospectively collected, this factor was not initially considered in determining risk and was not used in the multivariate analysis of previous studies in determining risk of perioperative complications.3,4
Payor status and its role in patient complications and outcomes are gaining increasing attention in the medical literature. Extensive evidence reports inferior outcomes and increased complications in uninsured patients compared to the privately insured.18–43 Similarly, mounting evidence suggests that patients with public insurance, particularly Medicaid may have increased complications and inferior outcomes when compared to commercially insured patients.19,21,22,24,26–34,40–42,44–53 Ranging from increased peri-operative complications28 to increased mortality for common medical conditions,42 studies spanning multiple medical fields have corroborated these findings in the Medicaid population.
With the growing body of literature analyzing the role of payor status in patient outcomes, we examined payor status and risk of perioperative complications following spine surgery for patients in our Spine End Results Registry (2003–2004). We hypothesized that Medicaid payer status was significantly associated with higher likelihood of medical complications than non-Medicaid payer status.
METHODS
Data Source
The Spine End Results Registry (2003–2004) is a registry of prospectively collected data of all patients undergoing spinal surgery at the XXXX Medical Center and XXXX Medical Center. Detailed information regarding patient demographics, insurance status, medical comorbidity, surgical invasiveness, and adverse occurrences were followed for up to two years and obtained prospectively using earlier published methods.16 This registry included patients undergoing any type of spinal surgery between January 1st 2003 and December 31st 2004 at two academic hospitals: a university based medical center, and a county hospital serving as the only Level I trauma center in a large multi-state area. All patients were prospectively followed for the occurrence of medical complication for at least two years after their surgery. The XXXX institutional review board approved the study and an informed consent was obtained from participants. Although insurance data were prospectively collected, this factor was not initially considered in determining risk and was not used in the multivariate analysis of our previous studies in determining risk of perioperative complications.3,4 Insurance data were provided by the XXXX Medical Center’s (XXMC) quality improvement database, which prospectively records and reports payor information in accordance with the Centers for Medicare and Medicaid Services (CMS) reporting criteria.
Exclusion Criteria
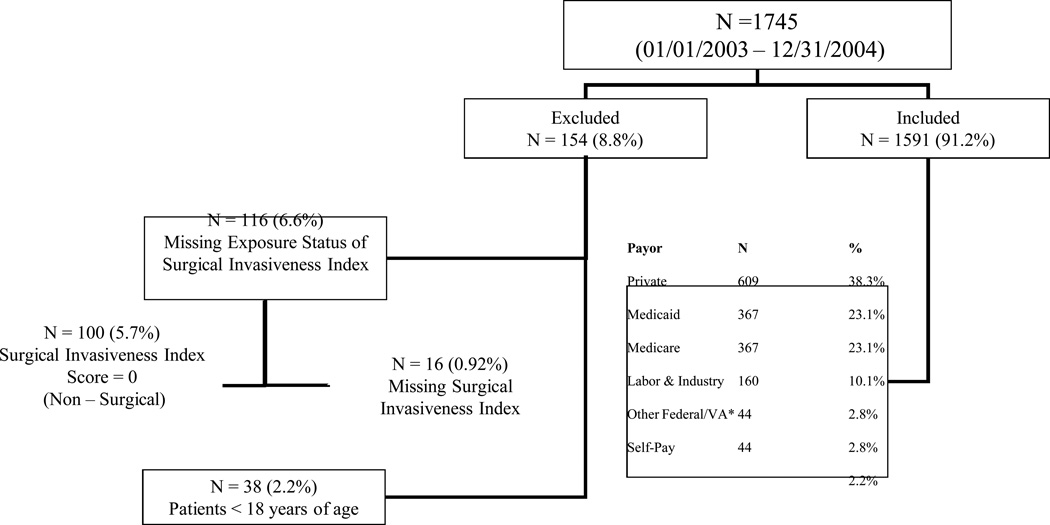
We excluded patients younger than 18 years of age, those with missing surgical invasiveness data and those with a surgical invasiveness index that was equal to zero, as this included patients who did not actually have surgery (Figure 1).
Figure 1.
Participant Flow Diagram
Any Adverse Event and Risk Factor Definitions
Medical complications examined in our study were combined into one outcome of “any adverse event”. A patient experienced “any adverse event”, a binary variable, if they had one or more coded adverse event in any one of six different organ system categories (cardiac, pulmonary, gastrointestinal (GI), neurological, hematological and urological) (see Supplemental Digital Conent) (Table 3).
Table 3.
Distribution of Demographics and Risk Factors across Payor Mix
| PAYOR | ||||||
|---|---|---|---|---|---|---|
| Private | Medicaid | Medicare | L&I | Fed&VA | SelfPay | |
| N | 611 | 367 | 369 | 161 | 42 | 44 |
| Row % | 38% | 23% | 23% | 10% | 3% | 3% |
| Age | ||||||
| 18 – 25 | 192 | 134 | 9 | 52 | 16 | 30 |
| 44% | 31% | 2% | 12% | 4% | 7% | |
| 40 – 64 | 408 | 223 | 87 | 106 | 21 | 14 |
| 48% | 26% | 10% | 12% | 2% | 2% | |
| >=65 | 11 | 10 | 273 | 3 | 5 | 0 |
| 4% | 3% | 90% | 1% | 2% | . | |
| Gender | ||||||
| Male | 315 | 226 | 190 | 119 | 32 | 34 |
| 34% | 25% | 21% | 13% | 3% | 4% | |
| Female | 296 | 141 | 179 | 42 | 10 | 10 |
| 44% | 21% | 26% | 6% | 1% | 1% | |
| Adverse Events | ||||||
| No | 508 | 272 | 240 | 130 | 34 | 39 |
| 42% | 22% | 20% | 11% | 3% | 3% | |
| Yes | 103 | 95 | 129 | 31 | 8 | 5 |
| 28% | 26% | 35% | 8% | 2% | 1% | |
| Anemia | ||||||
| No | 571 | 339 | 324 | 155 | 39 | 43 |
| 39% | 23% | 22% | 11% | 3% | 3% | |
| Yes | 40 | 28 | 45 | 6 | 3 | 1 |
| 33% | 23% | 37% | 5% | 2% | 0.1% | |
| Cancer History | ||||||
| No | 538 | 337 | 291 | 154 | 34 | 44 |
| 38% | 24% | 21% | 11% | 2% | 3% | |
| Yes | 73 | 30 | 78 | 7 | 8 | 0 |
| 37% | 15% | 40% | 4% | 4% | 0% | |
| Cardiac History | ||||||
| No | 575 | 342 | 292 | 156 | 39 | 43 |
| 40% | 24% | 20% | 11% | 3% | 3% | |
| Yes | 36 | 25 | 77 | 5 | 3 | 1 |
| 24% | 17% | 52% | 3% | 2% | 1% | |
| COPD | ||||||
| No | 582 | 339 | 328 | 151 | 39 | 43 |
| 39% | 23% | 22% | 10% | 3% | 3% | |
| Yes | 29 | 28 | 41 | 10 | 3 | 1 |
| 26% | 25% | 37% | 9% | 3% | 1% | |
| CVD | ||||||
| No | 590 | 350 | 323 | 159 | 40 | 44 |
| 39% | 23% | 21% | 11% | 3% | 3% | |
| Yes | 21 | 17 | 46 | 2 | 2 | 0 |
| 24% | 19% | 52% | 2% | 2% | 0% | |
| Drug Use | ||||||
| No | 579 | 279 | 352 | 143 | 40 | 33 |
| 41% | 20% | 25% | 10% | 3% | 2% | |
| Yes | 32 | 88 | 17 | 18 | 2 | 11 |
| 19% | 52% | 10% | 11% | 1% | 7% | |
| Hypertension | ||||||
| No | 473 | 268 | 176 | 121 | 30 | 42 |
| 43% | 24% | 16% | 11% | 3% | 4% | |
| Yes | 138 | 99 | 193 | 40 | 12 | 2 |
| 29% | 20% | 40% | 8% | 2% | 0% | |
| Liver Disease | ||||||
| No | 596 | 321 | 335 | 154 | 38 | 41 |
| 40% | 22% | 23% | 10% | 3% | 3% | |
| Yes | 15 | 46 | 34 | 7 | 4 | 3 |
| 14% | 42% | 31% | 6% | 4% | 3% | |
| Rheumatoid Arthristis | ||||||
| No | 595 | 349 | 345 | 159 | 40 | 44 |
| 39% | 23% | 23% | 10% | 3% | 3% | |
| Yes | 16 | 18 | 24 | 2 | 2 | 0 |
| 26% | 29% | 39% | 3% | 3% | 0% | |
| Renal Disease | ||||||
| No | 577 | 338 | 327 | 152 | 40 | 44 |
| 39% | 23% | 22% | 10% | 3% | 3% | |
| Yes | 34 | 29 | 42 | 9 | 2 | 0 |
| 29% | 25% | 36% | 8% | 2% | 0% | |
| Diagnosis | ||||||
| Degenerative | 379 | 210 | 240 | 127 | 24 | 11 |
| 38% | 21% | 24% | 13% | 2% | 1% | |
| Trauma | 138 | 101 | 73 | 28 | 6 | 27 |
| 37% | 27% | 20% | 8% | 2% | 7% | |
| Neoplasm | 67 | 17 | 24 | 1 | 7 | 2 |
| 57% | 14% | 20% | 1% | 6% | 2% | |
| Infection | 7 | 33 | 15 | 0 | 3 | 2 |
| 12% | 55% | 25% | 0% | 5% | 3% | |
| Complication | 10 | 3 | 16 | 5 | 1 | 2 |
| 27% | 8% | 43% | 14% | 3% | 5% | |
| Other | 10 | 3 | 1 | 0 | 1 | 0 |
| 67% | 20% | 7% | 0% | 7% | 0% | |
| Surgical Invasiveness Score | ||||||
| Mean | 7.86 | 7.32 | 11.40 | 7.64 | 8.26 | 6.27 |
| SD | 7.24 | 5.90 | 9.45 | 6.04 | 6.62 | 3.97 |
We assessed the odds ratio of several risk factors using univariate (Table 1) and multivariate analysis (Table 2). The exposure of interest was payor of surgical procedure and associated hospital stay. Risk factors assessed for confounding or effect modification included: age, gender, smoking status, alcohol use, drug use, diabetes, body mass index (BMI), medical co-morbidity (myocardial infarction, history of non-MI cardiac disease (valve disease, prolapse, abnormal EKG), congestive heart failure, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), asthma, hypertension, rheumatoid arthritis, renal conditions, pre-existing neoplasm, history of syncope or seizure, anemia, bleeding disorder), previous spinal surgery, primary diagnosis (degenerative, trauma, neoplasm, infection, and other), level of surgery (cervical, thoracic, lumbosacral), surgical approach (anterior, posterior, combined), and surgical invasiveness. Surgical invasiveness (SI) was defined using methods described in previously published works of the same cohort.
Table 1.
Univariate Analysis of Odds Ratio for Any Medical Complication (N=1591)
| Payor | NO Adverse Event 1,145 (77%) |
Any Adverse Event 446 (28%) |
OR of Adverse Event |
95% CI | p-value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Private | 482 (79%) | 127 (21%) | 1.00 | - | - | |
| Medicaid | 260 (71%) | 107 (29%) | 1.56 | 1.15 | 2.13 | 0.003 |
| Medicare | 209 (57%) | 158 (43%) | 2.87 | 2.14 | 3.85 | <0.001 |
| Labor & Industry | 122 (76%) | 38 (24%) | 1.18 | 0.759 | 1.81 | 0.427 |
| Other Federal/VA* | 34 (77%) | 10 (23%) | 1.12 | 0.479 | 2.39 | 0.768 |
| Self-Pay | 38 (86%) | 6 (14%) | 0.599 | 0.203 | 1.47 | 0.251 |
Veteran’s Administration
Table 2.
Multivariate Analysis of Odds Ratio for Any Medical Complication
| Risk Factor | Odds Ratio | 95% C.I. | ||
|---|---|---|---|---|
| Lower | Upper | p-value | ||
| Age (18 – 39) | 1.00 | - | - | - |
| 40 – 64 | 2.09 | 1.47 | 2.96 | < 0.0001 |
| ≥65 | 4.40 | 2.90 | 6.68 | < 0.0001 |
| Medicaid Payor | 1.68 | 1.23 | 2.29 | 0.001 |
| Congestive Heart Failure | 3.65 | 2.00 | 6.65 | < 0.0001 |
| Bleeding Diagnosis or Blood Clots | 1.91 | 1.23 | 2.98 | 0.004 |
| Diagnosis (Degenerative) | 1.00 | - | - | - |
| Trauma | 3.45 | 2.54 | 4.68 | < 0.0001 |
| Infection | 2.40 | 1.26 | 4.56 | 0.008 |
| Surgical Invasiveness Group (1 – 5) | 1.00 | - | - | - |
| 6 – 10 | 1.60 | 1.15 | 2.23 | 0.005 |
| 11 – 15 | 2.95 | 2.06 | 4.24 | < 0.0001 |
| 16 – 20 | 4.30 | 2.62 | 7.03 | < 0.0001 |
| 21 – 25 | 7.09 | 3.62 | 13.89 | < 0.0001 |
| > 25 | 11.0 | 6.11 | 19.71 | < 0.0001 |
CI = confidence intervals
Analysis
Categorical data are presented as the number of cases and percentages. For categorical values, Pearson’s Chi-square or Fisher’s exact tests (where cell counts were low) were used to assess the univariate effect of various risk factors, including the exposure of interest, payor status, on the outcome. Odds Ratio (OR) and 95% confidence intervals (95% CI) were calculated for each of the categorical variables using univariate and multivariate backwards, stepwise logistic regression analysisto examine the association between payor status and medical complication, adjusting for confounding factors of comorbidity and the effect- modifying interaction between age and the exposure of interest, payor status. In the model we included risk factors that were deemed of clinical importance by the study investigators to contribute to medical complication, were a known confounder, or had a univariate association of p < 0.10. Because surgical approach and the number of vertebral levels operated on are a component of the invasiveness index they were not included in the multivariate model.
Statistical analysis was performed using SAS Enterprise Guide 4.3 software (SAS Inc., Cary, NC) and STATA 12.1 (StataCorp, College Station, TX) with hypothesis testing using a 2-tailed test of significance and an alpha level of p< 0.05
RESULTS
There were 1745 patients who underwent spine surgery from Jan 1st 2003 to Dec 31st 2004. Of these, 154 were excluded for reasons outlined in Figure 1, leaving 1591 patients who were analyzed in this study.
The United States Government was the majority payor (N=778/1594, 48.8%) in our study, with almost half of patients received either Medicare (N=367/1594, 23.1%), Medicaid (N=367/1594, 23.1%) or some other federally funded program, including the Veterans’ Administration (N=44/1594, 2.8%). This was followed by private insurers (N=609/1594, 38.3%), and self-pay (N=44/1594, 2.8%).
Other studies have previously reported univariate analysis of risk factors for medical complications in greater detail3, we did not present the complete results of the univariate analysis in this manuscript as those risk factors are not the focus of our study question (Table 1). However, we did incorporate the results of the univariate analysis into our multivariate analysis and do present the significantly associated risk factors along with the payor data (Table 2).
The risk for any adverse event was highest among those patients receiving the most invasive surgical treatment (surgical invasiveness > 25). The odds of any adverse event following the most invasiveness spinal surgeries (SI>25) was more than 10-fold higher than those who received the least invasive (SI≤ 5) spine surgeries (OR=11.0, 95% CI: 6.11, 19.7, p<0.0001). In the univariate analysis, patients whose payor was Medicare had a 2.87 odds (95% CI: 2.14, 3.85, p<0.0001) of any adverse event occurring compared to those with private insurance. However, when controlling for age as a risk factor in the multivariate, Medicare was not statistically, significantly associated with any adverse event. However after controlling for confounders and effect modifiers in the multivariate analysis, those patients whose insurer was Medicaid had a 1.68 odds (95% CI: 1.23, 2.29, p=0.001) of having any adverse event when compared to the privately insured (Tables 1 & 2).
DISCUSSION
Significant evidence in the medical literature has shown clearly inferior outcomes and increased complications in uninsured patients compared to the privately insured.18–43 While this association to the uninsured population may be intuitive, there is increasing evidence of similarly inferior outcomes and increased complications in patients with public insurance, particularly Medicaid, when compared to privately insured patients.19,21,22,24,26–34,40–42,44–53 In addition, multiple studies have even found Medicaid status to be a significant factor for increased in-hospital mortality when compared to privately insured patients.19,24,27,28,34,42,46 Disparities in the care of children on public insurance also exist, ranging from cleft palate repair, otitis media treatment, and complications associated with spinal fusions for scoliosis.45,48,52 Alosh et al. have also published in the spine literature to show an increased risk of perioperative mortality in patients covered by Medicaid undergoing anterior cervical spine surgery.32
With our results corroborating multiple previous studies regarding Medicaid status and inferior patient outcomes, the essential follow up question is “Why?” Much attention, and justifiably so, is given to the blight of the uninsured. However, what is often neglected is the concept of underinsurance. Underinsurance is considered to be present when the health insurance benefits are in some way inadequate. Bashsur et al. defined it in general terms as “coverage that fails to provide adequate protection against health care expenditures.”58 More specifically, three main indicators of underinsurance have been specified as: “lack of needed benefits or services, limited access to providers, or out-of-pocket costs that are considered to be unreasonable.”44,59 Two decades ago, Bodenheimer discussed the importance of addressing the problem of underinsurance and stated that “…it reduces access to health care, especially for lower-income people, creates and inequitable method of financing care, and…can contribute to substandard clinical outcomes.”60 Kogan et al. showed that similar to uninsured children, underinsured children have suboptimal access to health care and quality of health care.44 In response to these findings, Perrin wrote that “the Affordable Care Act may leave chronically ill children…and newly insured Medicaid populations underinsured.”59 A recent study by Link et al. found that underinsured patients were less healthy and had lower health related quality of life than uninsured patients and that their study results may be generalizable to the U.S. population.61 From their findings, they concluded that underinsurance at the very least is as big of a challenge to public health and health policy as non-insured status. With their study mentioned previously, Lidor et al. concluded that the “lack of adequate health insurance is a…powerful predictor of disease severity…and mortality.”30
In addition to inadequate access, a component of underinsurance is when the coverage does not adequately protect the patient against healthcare expenditures. Thus, patients with Medicaid insurance may be faced with higher medical payments than they can afford and as a result avoid recommended treatment. Furthermore, lacking resources may prevent the patients from following physician recommendations. If socioeconomic disparities are an underlying cause for the differences in patient outcomes of Medicaid versus private insurance, then it is possible that level of education and understanding of medical conditions and treatment could be a factor. This helps explain the finding by Dasenbrock et al. who found Medicaid patients presented with a higher acuity of disease than private insurance patients.19 Therefore, rather than being a risk factor on its own, insurance status more likely serves as a proxy for other variables.
The results of our study further support the growing body of literature that Medicaid patients have higher rates of complications. One study previously reported risk factors for medical complications using this data registry, however in one previous report, we did not include payor status as a covariate.3 In this study we specifically examine the role of payor status in the context of previously defined risk factors. In the univariate analysis, both Medicare and Medicaid insurance status had increased rates of perioperative medical complications. However, with the multivariate analysis controlling for other significant risk factors, especially age, Medicaid but not Medicare, insurance status remained a significant risk factor for perioperative medical complications. Because our patient population is very heterogeneous with our academic institution seeing a broad spectrum of patients, we feel that our findings are generalizable to the overall spine surgery community. Therefore, just as medical and surgical co-morbidity factors should be taken into account when considering the safety of surgery and likelihood of complication, Medicaid status should be considered as well as our study clearly suggests an association.
The implication of this finding is significant, particularly as we progress into an era of quality metrics being linked to reimbursement. The occurrence of a complication is increasingly being regarded as an indicator of ‘poor quality’. Metrics such as surgical site infection or readmission within 30 days of discharge already are subject to ‘quality adjustment payments’ to medical centers. However, these metrics are not risk adjusted to account for patient risk factors. Inherently, patients will have different risks for complications based on their medical co-morbidities and other socioeconomic risk factors. It goes without saying that sicker patients are more likely to have complications from treatment when compared to a healthy patient undergoing the same treatment. Thus, medical centers that treat a disproportionate number of patients with co-morbidities and risk factors may find their ‘quality’ rating to be lower than other facilities that treat healthier patients. Without sufficient risk adjustment to account for patient morbidity and known risk factors, these quality metrics not only inaccurately assign quality grades but also can financially penalize medical institutions that treat patients with these known risk factors. As hospital reimbursement becomes directly related to various non-risk-adjusted outcome measures, it is possible that higher risk patients may encounter additional challenges in access to health care. As our study and others before it have demonstrated an association of payor status and complications, it is entirely possible that this may have unintended consequences in limiting access of care for these patients. Further investigation is essential to fully understand the etiology of this finding and more importantly, to remedy this disparity in health care.
Supplementary Material
KEY POINTS.
-
-
This study identifies the role of payor status in the risk for perioperative medical complications following spine surgery.
-
-
Medicaid insurance status is a risk factor for perioperative complications
-
-
Underinsurance of patients is an often unacknowledged problem
Acknowledgments
We would like to acknowledge Dr. Sohail Mirza (Dartmouth Medical Center) for his tremendous contribution to the registry utilized in this manuscript.
UWMC IRB-approved
The Manuscript submitted does not contain information about medical device(s)/drug(s). Supported by grants from the NIH/NIAMS 5K23AR48979 and 5P60-AR48093 and supported in part by the Spine End-Results Research Fund at the University of Washington Medical Center through a gift from Synthes Spine (Paoli, PA). Relevant financial activities outside the submitted work: board membership, consultancy, expert testimony, grants/grants pending, and payment for lectures.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cassinelli EH, et al. Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis: an analysis of 166 patients. Spine. 2007;32:230–235. doi: 10.1097/01.brs.0000251918.19508.b3. [DOI] [PubMed] [Google Scholar]
- 2.Lee DY, Lee S-H, Jang J-S. Risk factors for perioperative cardiac complications after lumbar fusion surgery. Neurol. Med. Chir. (Tokyo) 2007;47:495–500. doi: 10.2176/nmc.47.495. [DOI] [PubMed] [Google Scholar]
- 3.Lee MJ, et al. Risk factors for medical complication after spine surgery: a multivariate analysis of 1,591 patients. Spine J. 2012;12:197–206. doi: 10.1016/j.spinee.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee MJ, et al. Risk Factors for Medical Complication After Lumbar Spine Surgery. Spine. 2011;36:1801–1806. doi: 10.1097/brs.0b013e318219d28d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schoenfeld AJ, Ochoa LM, Bader JO, Belmont PJ., Jr Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am. 2011;93:1577–1582. doi: 10.2106/JBJS.J.01048. [DOI] [PubMed] [Google Scholar]
- 6.Weiss H-R, Goodall D. Rate of complications in scoliosis surgery – a systematic review of the Pub Med literature. Scoliosis. 2008;3:9. doi: 10.1186/1748-7161-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85-A:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Whitmore RG, et al. Patient Comorbidities and Complications following Spinal Surgery: A Societal-based Cost Analysis. Spine. 2011 doi: 10.1097/BRS.0b013e31823da22d. [DOI] [PubMed] [Google Scholar]
- 9.Patel N, et al. Obesity and spine surgery: relation to perioperative complications. Journal of Neurosurgery: Spine. 2007;6:291–297. doi: 10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- 10.Street JT, et al. Morbidity and mortality of major adult spinal surgery. A prospective cohort analysis of 942 consecutive patients. Spine J. 2012;12:22–34. doi: 10.1016/j.spinee.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Fu K-MG, et al. Morbidity and mortality in the surgical treatment of 10,329 adults with degenerative lumbar stenosis. Journal of Neurosurgery: Spine. 2010;12:443–446. doi: 10.3171/2009.11.SPINE09531. [DOI] [PubMed] [Google Scholar]
- 12.Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA. Morbidity and mortality in association with operations on the lumbar spine. The influence of, age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74:536–543. [PubMed] [Google Scholar]
- 13.Nasser R, et al. Complications in spine surgery. J Neurosurg Spine. 2010;13:144–157. doi: 10.3171/2010.3.SPINE09369. [DOI] [PubMed] [Google Scholar]
- 14.Wang MC, Chan L, Maiman DJ, Kreuter W, Deyo RA. Complications and Mortality Associated With Cervical Spine Surgery for Degenerative Disease in the United States. Spine. 2007;32:342–347. doi: 10.1097/01.brs.0000254120.25411.ae. [DOI] [PubMed] [Google Scholar]
- 15.Rampersaud YR, Neary MA, White K. Spine adverse events severity system: content validation and interobserver reliability assessment. Spine. 2010;35:790–795. doi: 10.1097/BRS.0b013e3181bf25a3. [DOI] [PubMed] [Google Scholar]
- 16.Mirza SK, et al. Development of an index to characterize the ‘invasiveness’ of spine surgery: validation by comparison to blood loss and operative time. Spine. 2008;33:2651–2661. doi: 10.1097/BRS.0b013e31818dad07. discussion 2662. [DOI] [PubMed] [Google Scholar]
- 17.Romano PS, Chan BK, Schembri ME, Rainwater JA. Can administrative data be used to compare postoperative complication rates across hospitals? Med Care. 2002;40:856–867. doi: 10.1097/00005650-200210000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Sabik LM, Dahman BA. Trends in Care for Uninsured Adults and Disparities in Care by Insurance Status. Med Care Res Rev. 2011 doi: 10.1177/1077558711418519. [DOI] [PubMed] [Google Scholar]
- 19.Dasenbrock HH, et al. The impact of insurance status on outcomes after surgery for spinal metastases. Cancer. 2012 doi: 10.1002/cncr.27388. [DOI] [PubMed] [Google Scholar]
- 20.Downing SR, et al. The impact of insurance status on actuarial survival in hospitalized trauma patients: when do they die? J Trauma. 2011;70:130–134. doi: 10.1097/TA.0b013e3182032b34. discussion 134–135. [DOI] [PubMed] [Google Scholar]
- 21.Kwok J, et al. The impact of health insurance status on the survival of patients with head and neck cancer. Cancer. 2010;116:476–485. doi: 10.1002/cncr.24774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stulberg DB, Zhang JX, Lindau ST. Socioeconomic disparities in ectopic pregnancy: predictors of adverse outcomes from Illinois hospital-based care 2000–2006. Matern Child Health J. 2011;15:234–241. doi: 10.1007/s10995-010-0579-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haider AH, et al. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 24.Nguyen GC, Bayless TM, Powe NR, Laveist TA, Brant SR. Race and health insurance are predictors of hospitalized Crohn’s disease patients undergoing bowel resection. Inflamm. Bowel Dis. 2007;13:1408–1416. doi: 10.1002/ibd.20200. [DOI] [PubMed] [Google Scholar]
- 25.Bjurlin MA, Zhao LC, Goble SM, Hollowell CMP. Race and Insurance Status are Risk Factors for Orchiectomy Due to Testicular Trauma. J. Urol. 2012;187:931–935. doi: 10.1016/j.juro.2011.10.152. [DOI] [PubMed] [Google Scholar]
- 26.Rosen H, Saleh F, Lipsitz SR, Meara JG, Rogers SO., Jr Lack of insurance negatively affects trauma mortality in US children. J. Pediatr. Surg. 2009;44:1952–1957. doi: 10.1016/j.jpedsurg.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 27.Kapoor JR, et al. Payment source, quality of care, and outcomes in patients hospitalized with heart failure. J. Am. Coll. Cardiol. 2011;58:1465–1471. doi: 10.1016/j.jacc.2011.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.LaPar DJ, et al. Primary payer status affects mortality for major surgical operations. Ann. Surg. 2010;252:544–550. doi: 10.1097/SLA.0b013e3181e8fd75. discussion 550–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boxer LK, et al. Payer status is related to differences in access and outcomes of abdominal aortic aneurysm repair in the United States. Surgery. 2003;134:142–145. doi: 10.1067/msy.2003.214. [DOI] [PubMed] [Google Scholar]
- 30.Lidor AO, Gearhart SL, Wu AW, Chang DC. Effect of race and insurance status on presentation, treatment, and mortality in patients undergoing surgery for diverticulitis. Arch Surg. 2008;143:1160–1165. doi: 10.1001/archsurg.143.12.1160. discussion 1165. [DOI] [PubMed] [Google Scholar]
- 31.Kelz RR, et al. Morbidity and mortality of colorectal carcinoma surgery differs by insurance status. Cancer. 2004;101:2187–2194. doi: 10.1002/cncr.20624. [DOI] [PubMed] [Google Scholar]
- 32.Alosh H, Riley LH, 3rd, Skolasky RL. Insurance status, geography, race, and ethnicity as predictors of anterior cervical spine surgery rates and in-hospital mortality: an examination of United States trends from 1992 to 2005. Spine. 2009;34:1956–1962. doi: 10.1097/BRS.0b013e3181ab930e. [DOI] [PubMed] [Google Scholar]
- 33.Robbins AS, Pavluck AL, Fedewa SA, Chen AY, Ward EM. Insurance status, comorbidity level, and survival among colorectal cancer patients age 18 to 64 years in the National Cancer Data Base from 2003 to 2005. J. Clin. Oncol. 2009;27:3627–3633. doi: 10.1200/JCO.2008.20.8025. [DOI] [PubMed] [Google Scholar]
- 34.Parikh PB, et al. Association of health insurance status with presentation and outcomes of coronary artery disease among nonelderly adults undergoing percutaneous coronary intervention. Am. Heart J. 2011;162:512–517. doi: 10.1016/j.ahj.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 35.Salim A, et al. Does insurance status matter at a public, level I trauma center? J Trauma. 2010;68:211–216. doi: 10.1097/TA.0b013e3181a0e659. [DOI] [PubMed] [Google Scholar]
- 36.Rosen H, Saleh F, Lipsitz S, Rogers SO, Jr, Gawande AA. Downwardly mobile: the accidental cost of being uninsured. Arch Surg. 2009;144:1006–1011. doi: 10.1001/archsurg.2009.195. [DOI] [PubMed] [Google Scholar]
- 37.Greene WR, et al. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. Am. J. Surg. 2010;199:554–557. doi: 10.1016/j.amjsurg.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 38.Sabatino SA, et al. Disparities in mammography use among US women aged 40–64 years, by race, ethnicity, income, and health insurance status 1993 and 2005. Med Care. 2008;46:692–700. doi: 10.1097/MLR.0b013e31817893b1. [DOI] [PubMed] [Google Scholar]
- 39.Freeman J, Boomer L, Fursevich D, Feliz A. Ethnicity and Insurance Status Affect Health Disparities in Patients with Gallstone Disease. J. Surg. Res. 2011 doi: 10.1016/j.jss.2011.06.064. [DOI] [PubMed] [Google Scholar]
- 40.Shen JJ, Washington EL. Disparities in outcomes among patients with stroke associated with insurance status. Stroke. 2007;38:1010–1016. doi: 10.1161/01.STR.0000257312.12989.af. [DOI] [PubMed] [Google Scholar]
- 41.Fedewa SA, Lerro C, Chase D, Ward EM. Insurance status and racial differences in uterine cancer survival: a study of patients in the National Cancer Database. Gynecol. Oncol. 2011;122:63–68. doi: 10.1016/j.ygyno.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 42.Hasan O, Orav EJ, Hicks LS. Insurance status and hospital care for myocardial infarction, stroke, and pneumonia. J Hosp Med. 2010;5:452–459. doi: 10.1002/jhm.687. [DOI] [PubMed] [Google Scholar]
- 43.Halpern MT, Renaud JM, Vickrey BG. Impact of insurance status on access to care and out-of-pocket costs for U.S. individuals with epilepsy. Epilepsy Behav. 2011;22:483–489. doi: 10.1016/j.yebeh.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 44.Kogan MD, et al. Underinsurance among children in the United States. N. Engl. J. Med. 2010;363:841–851. doi: 10.1056/NEJMsa0909994. [DOI] [PubMed] [Google Scholar]
- 45.Abbott MM, Kokorowski PJ, Meara JG. Timeliness of surgical care in children with special health care needs: delayed palate repair for publicly insured and minority children with cleft palate. J. Pediatr. Surg. 2011;46:1319–1324. doi: 10.1016/j.jpedsurg.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 46.Lemaire A, Cook C, Tackett S, Mendes DM, Shortell CK. The impact of race and insurance type on the outcome of endovascular abdominal aortic aneurysm (AAA) repair. J. Vasc. Surg. 2008;47:1172–1180. doi: 10.1016/j.jvs.2008.01.033. [DOI] [PubMed] [Google Scholar]
- 47.Abdo A, et al. The effect of insurance status on outcomes after partial nephrectomy. Int Urol Nephrol. 2011 doi: 10.1007/s11255-011-0056-1. [DOI] [PubMed] [Google Scholar]
- 48.Vitale MA, et al. The contribution of hospital volume, payer status, and other factors on the surgical outcomes of scoliosis patients: a review of 3,606 cases in the State of California. J Pediatr Orthop. 2005;25:393–399. doi: 10.1097/01.bpo.0000153880.05314.be. [DOI] [PubMed] [Google Scholar]
- 49.Hakim RB, Benedict MB, Merrick NJ. Quality of care for women undergoing a hysterectomy: effects of insurance and race/ethnicity. Am J Public Health. 2004;94:1399–1405. doi: 10.2105/ajph.94.8.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Boomer L, Freeman J, Landrito E, Feliz A. Perforation in adults with acute appendicitis linked to insurance status, not ethnicity. J. Surg. Res. 2010;163:221–224. doi: 10.1016/j.jss.2010.04.041. [DOI] [PubMed] [Google Scholar]
- 51.Trinh Q-D, et al. Morbidity and mortality of radical prostatectomy differs by insurance status. Cancer. 2011 doi: 10.1002/cncr.26475. [DOI] [PubMed] [Google Scholar]
- 52.Patel S, Schroeder JW, Jr, et al. Disparities in children with otitis media: the effect of insurance status. Otolaryngol Head Neck Surg. 2011;144:73–77. doi: 10.1177/0194599810391428. [DOI] [PubMed] [Google Scholar]
- 53.Carter JE, Neff LP, Holmes JH. Adherence to Burn Center Referral Criteria: Are Patients Appropriately Being Referred? Journal of Burn Care & Research. 2010;31:26–30. doi: 10.1097/BCR.0b013e3181cb8efb. [DOI] [PubMed] [Google Scholar]
- 54.Income, Poverty, and Health Insurance Coverage in the United States: 2010. at < www.census.gov/prod/2011pubs/p60-239.pdf>.
- 55.Collins SR, Robertson R, Garber T, Doty MM. Tracking trends in health system performance: the income divide in health care: how the Affordable Care Act will help restore fairness to the U.S. health system. Issue Brief (Commonw Fund) 2012;3:1–24. [PubMed] [Google Scholar]
- 56.Key Features of the Law | HealthCare.gov. at < http://www.healthcare.gov/law/features/index.html>.
- 57.Ku L. Ready, set, plan, implement: executing the expansion of Medicaid. Health Aff (Millwood) 2010;29:1173–1177. doi: 10.1377/hlthaff.2010.0417. [DOI] [PubMed] [Google Scholar]
- 58.Bashshur R, Smith DG, Stiles RA. Defining underinsurance: a conceptual framework for policy and empirical analysis. Med Care Rev. 1993;50:199–218. doi: 10.1177/107755879305000204. [DOI] [PubMed] [Google Scholar]
- 59.Perrin JM. Treating underinsurance. N. Engl. J. Med. 2010;363:881–883. doi: 10.1056/NEJMe1007674. [DOI] [PubMed] [Google Scholar]
- 60.Bodenheimer T. Underinsurance in America. N. Engl. J. Med. 1992;327:274–278. doi: 10.1056/NEJM199207233270412. [DOI] [PubMed] [Google Scholar]
- 61.Link CL, McKinlay JB. Only half the problem is being addressed: underinsurance is as big a problem as uninsurance. Int J Health Serv. 2010;40:507–523. doi: 10.2190/HS.40.3.g. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.