Abstract
Objective
This study mainly aimed to investigate the association of ovarian cancer mortality with reproductive factors and body mass index among Japanese women aged 40-79 years.
Methods
The source of the data was the Japan Collaborative Cohort (JACC) study which covered the period of 1988 to 2009. A representative sample of 64,185 women was used. Cox model was used to estimate the relative risk (RR) and 95% confidence interval (CI).
Results
The total number of ovarian cancer deaths was 98, with a mortality rate of 9.30 per 100,000 person-years. Women with single marital status revealed significantly higher age-adjusted RR (RR, 4.11; 95% CI, 1.66 to 10.23; p=0.005) as compared to married women. The effect of single marital status was stronger among older women aged 50+ years (RR, 4.58; 95% CI, 1.65 to 12.72; p=0.003) than younger women. An elevated risk was found for both nulliparous and nullipregnant women. Similarly, an increased risk of ovarian cancer mortality was estimated among overweight among aged 50 years or less.
Conclusion
Out of many factors only single marital status indicated a higher risk for ovarian cancer mortality. All other factors provided inconclusive results, which imply further epidemiological investigations.
Keywords: Japan, Marital status, Ovarian cancer, Prospective cohort study, Reproductive history
INTRODUCTION
Globally overall cancer burden including the burden of ovarian cancer (OC) is increasing. The OC is the sixth and eighth leading cause of cancer mortality among women in developed and developing countries [1]. The worldwide estimated number of new OC cases increased from 137,600 in 1980 [2] to 225,000 in 2008 [1]. This gynecologic cancer mainly results from the malignant transformation of the ovarian surface epithelium [3], which approximately accounts for 90% of the total OC and generally develops after the age of 40 years [4].
As compared to the European and other developed countries, the OC is less dominant in Japan [5,6]. However, an increasing trend of OC has been observed in this country since 1975 [5-8]. For example, the age-standardized incidence of OC per 100,000 women increased from 6.4 in 2002 to 7.6 in 2008 in Japan [6,8]. The crude incidence rate per 100,000 women increased from 4.2 to 8.4 during the period of 1975-1998, whereas the age-standardized incidence rate increased from 4.0 to 5.4 per 100,000 women during the same period [7]. Several factors such as increased notification of OC from the concerned authorities and institutions due to better diagnostic facilities, changing dietary patterns and adoption of westernised lifestyles may contribute to the rising trend of OC [1,9].
Risk or protective factors for OC can broadly be grouped as socio-demographic (e.g., age, race, marital status) [10,11]; reproductive (e.g., number of pregnancy, parity, age at first birth, age at menarche) [10-14]; family history of cancer [14-17]; past history of diabetes [17]; dietary habits [17]; anthropometric measures (height, overweight/obesity) [14,17,18]; menopausal status and use of hormonal drugs [13,14,19-21]; use of oral contraceptives [11-13]; lifestyle factors such as smoking [5,22,23], drinking [14,22,24-26], physical activity [14,22,27-29], and walking [28].
Smoking is reported as a risk [5,23], protective [22] or independent factor for OC [14]. Similarly, alcohol drinking revealed increased [24], decreased [25] and no risk for OC [14,22,26]. Inconsistencies are also seen for other lifestyle factors (e.g., physical activity), anthropometric measures, a family history of cancer, dietary habits, menopausal status and hormonal use. These inconsistencies may arise from the variation of the study design, sample size and settings of the study. Most of the studies used a case-control design, which may suffer from recall and selection bias. Only few studies used cohort design. Moreover, interpretations of results are hampered by inadequate control for potential confounding factors, small sample sizes, and differences in reference groups [13]. All these inconsistencies underscore the necessities of further epidemiological studies based on a large sample of a cohort study.
Our study is an important attempt in this regard. Here we report the association of OC with various factors except dietary habits and use of oral contraceptives. However, attentions were given only to those factors which showed an elevated risk of mortality in the age-adjusted Cox model. We utilised the final data (ended in 2009) of the Japan Collaborative Cohort (JACC) study, which is one of the biggest prospective cohort studies for evaluating the cancer risk in Japan. Briefly, some characteristics of this study such as the long follow-up period and generation of reliable data made it unique in Japan. As the selected characteristics of study participants were similar to those of the Japanese general population, this study could also be regarded as a representative study of the Japanese population [30].
MATERIALS AND METHODS
Relevant data for this article were extracted from the JACC study, which was established in the late 1980s to evaluate the risk impact of lifestyle factors and levels of serum components on human health. The Ethical Board at Nagoya University School of Medicine approved this study. As this study is a prospective cohort study for all cancer sites, the study protocol included potential risk factors not only for OC but also for other cancers. The detailed information concerning the study design was explained elsewhere [31,32]. Briefly, the JACC study is a multicenter-collaborative study in which 24 institutions participated voluntarily. Study subjects were recruited from 45 areas of Japan except Shikoku district. Baseline data was mostly collected from 1988 to 1990 [30]. Individual informed consent prior to participation in the study was obtained in 36 of the 45 study areas (written consent in 35 areas and oral consent in 1 area), while in the remaining 9 areas, group consent from the head of the area was obtained. The JACC study recruited an initial sample of 110,585 respondents (men, 46,398; women, 64,190) aged 40-79 years. In order to extract the final sample for the present study, several exclusion criteria were applied. First, we excluded all the male subjects as we only focused on OC mortality related to women. Later, we excluded all females who had a history of OC (International Classification of Diseases [ICD] 9, 183) at the time of baseline survey. Finally, we got a sample of 64,185 women for detailed analyses.
1. Follow-up
The whole study including the follow-up period in most areas was ended at the end of 2009 [30]. In some areas the follow-up was ended even early: at the end of 1999 (4 areas), 2003 (4 areas) and 2008 (2 areas). The main reason for different follow-up periods was the retirement of major researchers in different years from their study areas. During the follow-up period, statuses of subjects (namely deaths, lost-to follow-up, and alive) were ascertained annually or biannually by the investigators. The investigators reviewed the population registry of cohort members to determine the causes of deaths with the permission of the director-general of the Prime Minister's Office (Ministry of Public Management, Home Affairs, Post and Telecommunications) and/or the Ministry of Health, Labor and Welfare, Japan. The date of move-out of cohort members from the study areas were also annually or biannually verified by the investigator in cooperation with key members of the local governmental office [33]. For the present study, the event of interest was the survival time from enrollment to death due to OC. Here censored cases meant all (1) drop/move out cases during follow-up, (2) deaths except OC death, and (3) cases who survived until the end of the follow-up. It should be noted that this article utilised only a part of the whole study findings. Many articles have already been published on different cancers [30] including OC [5,33,34] since the inception of the JACC study.
2. Baseline information
A lot of information at baseline survey e.g., demographic information; schooling; past history of 7 acute infectious and 11 chronic diseases; health check-up including screening; lifestyles (e.g., smoking, alcohol drinking and physical activity); anthropometric measures; reproductive history; food habits and blood samples (partly) were collected using self-administered questionnaire. However, only few of them were considered for analyses.
3. Adjusted variables
Some of the evaluated factors used as adjusted variables in the Cox model are listed in Table 1. The composite variable for family history of cancer was based on the histories of various cancers either in father or mother or siblings, which included breast (ICD9, 174), endometrial (ICD9, 182) and ovarian (ICD9, 183) cancers for mother and sister, and prostate cancer (ICD9, 185) for father and brother.
Table 1.
Information of adjusted variables
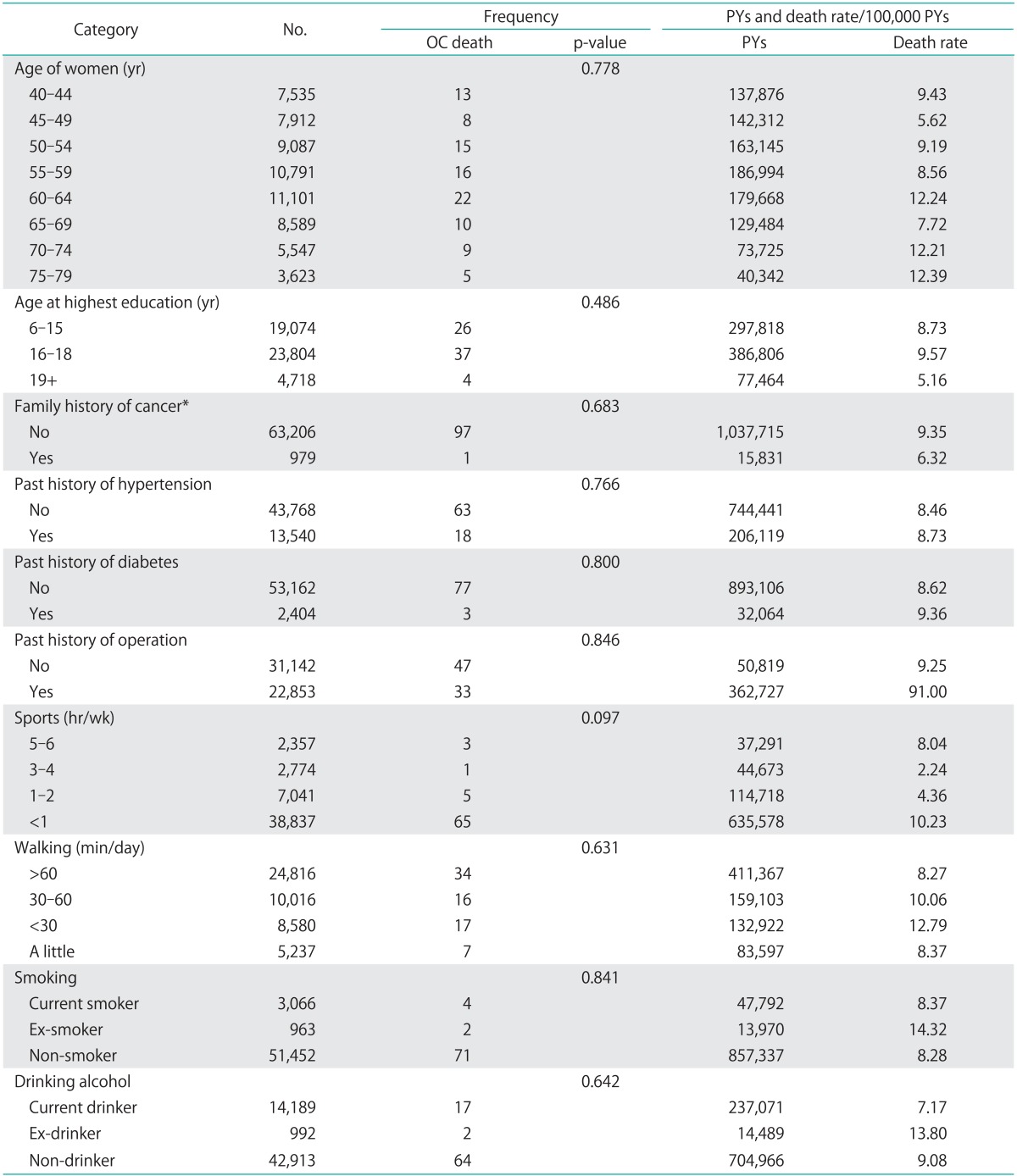
Total sample varied due to missing information.
OC, ovarian cancer; PYs, person-years.
*Breast, endometrial, and ovarian cancer for mother and sister and prostate cancer for father and brother.
It should be noted that the accessibility to screening program for cancer in Japan is fairly good. However, there is no national screening programme which is directly provided by the Japanese Government. Only several screening programs for cancer are indirectly supported by the government. Moreover, insurance does not cover screening programs [35,36].
4. Target variables
Several reproductive variables namely marital status (married, widowed, divorced, single), age at marriage in years (11-19, 20-25, 26+), number of pregnancy (0, 1-2, 3-4, 5+), number of live birth (0, 1-2, 3-4, 5+), age at first delivery in years (11-22, 23-26, 27+), age at menarche in years (below 14, 15-16, 17+), age at menopause in years (<50, 50+), and history of hormonal drug use (yes, no) including body mass index (BMI; underweight, normal, overweight) were considered as target variables.
5. Statistical analyses
All statistical analyses were performed using IBM SPSS ver. 19.0 (IBM Inc., Armonk, NY, USA). Firstly, we presented the distribution of women, OC deaths, person-years (PYs) and death rate per 100,000 PYs for each category of the adjusted and target variables (Tables 1, 2). Using Cox-proportional hazard model, we estimated the age-adjusted (model I) and multivariable-adjusted (model II) relative risk (RR) and 95% confidence interval (95% CI) for all target variables (Table 2). Before entering target and adjusted variables into the multivariable model, we checked the multicollinearity using variance inflation factor (VIF) statistic. None of the variables suffered from the multicollinearity as all VIFs were less than 3. We also checked the interaction effect of marital status, pregnancy and delivery on OC death, which was highly insignificant. Therefore, we did not report this finding. Lastly, we calculated age-adjusted (continuous) RR and 95% CI for two mutually exclusive groups of women using the cut-off age of 50 at baseline (Table 3). We excluded all women with single marital status while analyzing three variables namely age at marriage, number of pregnancy and number of live birth. We used this exclusion criterion, as more than 90% of the women were nullipregnant or nulliparous. Similarly, all nulliparous women were excluded from the variable age at first delivery. Any result with a p-value of 0.05 was considered as statistically significant.
Table 2.
Adjusted relative risk for ovarian cancer mortality in relation to reproductive and other factors in Japan
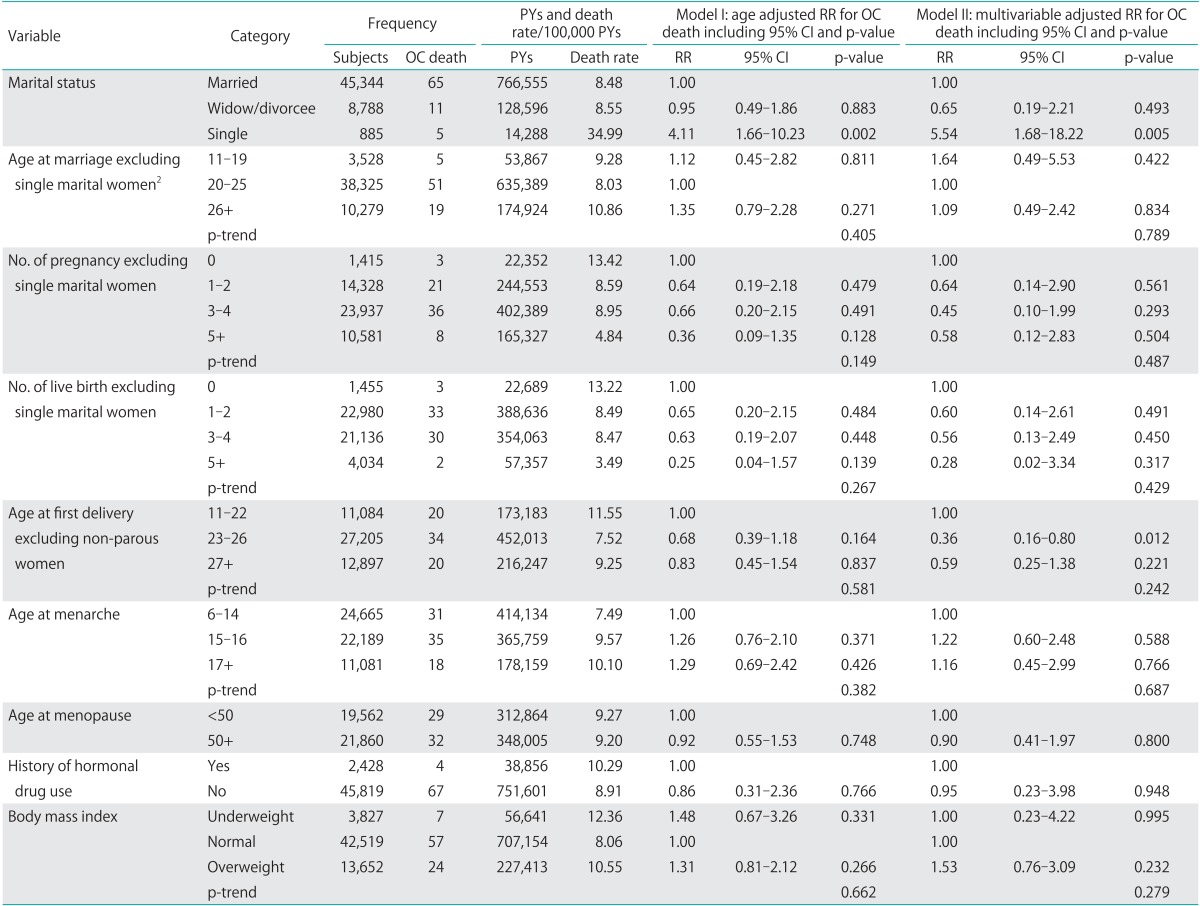
OC, ovarian cancer; PYs, person-years; RR, relative risk.
Table 3.
Results of age-adjusted Cox models for two mutually exclusive groups of women based on the cut-off of age 50 at baseline
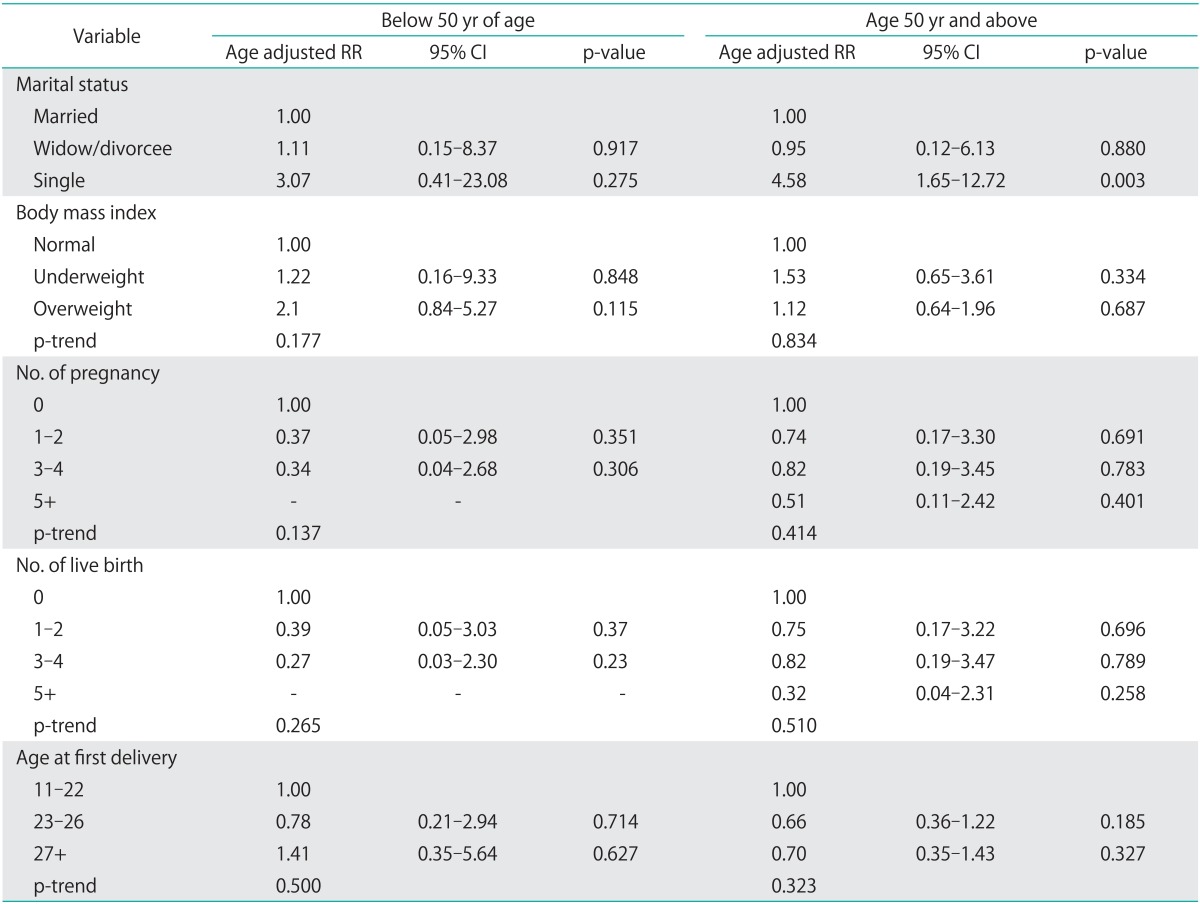
Not estimated due to insufficient number of ovarian cancer death.
CI, confidence interval; RR, relative risk.
RESULTS
1. Descriptive characteristics
The total number of OC deaths was 98 during the average follow-up period of 16.41 PYs. The mortality rate was 9.30 per 100,000 PYs. The average age of women at baseline survey was about 58 years with a standard deviation of 10.1 years. According to Table 1, the highest percentage of women was non-smoker (92.7%) and non-drinker (73.9%). A majority of women belonged to the category of normal BMI (70.9%), followed by overweight (22.8%) and underweight (6.4%), respectively.
According to Table 2, slightly over 80% of the women (82.4%) were married and only few of them were single. Most of the married women (83.8%) got married between 20 to 25 years of age with an average of 23.4 years. The average number of pregnancy per woman was 3.4, with the highest percentage in the category of 3 to 4 children, followed by the category of 1 to 2 children. Only few women reported no pregnancy. In contrast, the average number of live births was 2.7 per woman, with the highest percentage in the group of 1 to 2 births, followed by the group of 3 to 4 births. The average age of first delivery for parous women was 24.9 years and the highest percentage occurred between 23 and 26 years of age, followed by 27 years and more. Age at menarche ranged between 11 to 22 years for the majority women (average, 15.0). Almost 50% of the women experienced menopause at the age of 50 years (average, 48.5).
Marital status was significantly associated with OC mortality in both age-adjusted and multivariable-adjusted models (Table 2). For instance, single marital women revealed a significantly higher RR of OC mortality in age-adjusted (RR, 4.11; 95% CI, 1.66 to 10.23; p=0.002) and multivariable-adjusted (RR, 5.54; 95% CI, 1.68 to 18.22; p=0.005) models as compared to married women. Although overweight women revealed an elevated risk of OC mortality as compared to normal BMI in both models, they were statistically insignificant.
The age-adjusted Cox-model revealed reduced but insignificant association of OC mortality with higher number of pregnancy and higher number of live birth as compared to the null category. For example, the age-adjusted RR for the category of 1-2, 3-4, and 5+ pregnancies were 0.64 (95% CI, 0.19 to 2.18), 0.66 (95% CI, 0.20 to 2.15), and 0.36 (95% CI, 0.09 to 1.34) when compared with the category of nullipregnancy (Table 2). Later age at menarche was also found to be associated with an elevated risk of OC mortality (Table 2).
Group-specific analyses based on the baseline age (Table 3) showed a strong and significant association between single marital status and OC mortality among the women of 50+ years of age at baseline (RR, 4.58; 95% CI, 1.65 to 12.72; p=0.003). In contrast, the association was insignificant among the younger women aged less than 50 years (RR, 3.07; 95% CI, 0.41 to 23.08; p=0.275).
DISCUSSION
According to our results, only marital status was strongly associated with OC mortality, with a four-time higher risk among women with single marital status. The effect of single marital status was stronger among older (aged 50+ years at baseline) than younger women. Nulliparous and nullipregnant women also experienced elevated risks of OC mortality. Lower risks of OC mortality due to higher pregnancies or a higher risk due to nulliparity were reported in other studies [13,19,21]. A lower number of birth/pregnancy is obviously associated with a prolonged birth spacing or time to pregnancy, which may act as risk factors. For instance, a higher risk of OC was found among those women who gave last birth before 10 years as compared to women who gave last birth within five years of diagnosis [16]. Similarly, an increased ovarian cancer risk with a prolonged time to pregnancy was found by Braem et al. [13]. The average age at marriage at baseline (23.4 years) seems to be low according to the present situation. However, it is not surprising because the data reflected the situation of the period of 1988 to 1991.
Although additional research is recommended to elucidate the different biologic pathways of OC [13], according to present knowledge, reproductive factors such as pregnancies or some components of the child bearing process can protect OC by several mechanisms [13,21]. The two commonly suggested etiologic mechanisms for OC are (1) that suppression of ovulation reduces risk and (2) that suppression of pituitary gonadotropins reduces risk. Parity might reduce OC risk by increasing the circulation of progesterone levels [13]. A pregnancy may lead to anovulation, thereby can reduce gonadotropin secretion and increase endogenous estrogen and progesterone levels. An increasing progesterone level can protect the OC development by suppressing the epithelial proliferation, promoting cellular differentiation and apoptosis. Moreover, pregnancies and apoptosis resulting from the high progesterone levels during pregnancy or from exogenous hormone can clear malignantly transformed cells from the ovaries [13,21].
Other reproductive factors provided mixed results. For instance, our study failed to show any significant association between age at delivery and OC mortality, although some studies reported that higher age at first birth is positively associated with OC [16,19]. Similarly, several epidemiological studies which examined the impact of age at menarche and age at menopause on epithelial OC provided inconclusive results [13,16]. Although some studies provided the evidence of higher risk in relation to age at menarche and menopause [19,37], the JACC study failed to provide such evidence. Results are also inconsistent for hormonal drug use as our study revealed no association with OC, whereas others reported higher risks [19,21]. It is explained that an excessive stimulation of ovarian tissue by hormones may increase the OC risk [13].
Being underweight and overweight also showed age-adjusted elevated risks for OC mortality. Results connecting the obesity and OC are also mixed. Many studies suggested that excess body weight is a risk factor for many cancers [18,22,38,39]. The association was heterogeneous and stronger in case-control studies than in prospective studies [18]. For instance, height (≥170 cm) and BMI were found to be associated with an increased risk of OC in premenopausal women [18]. Overweight women showed significantly increased risk of OC mortality in Denmark [40]. Several interacting metabolic and hormonal pathways of insulin-resistance could be responsible for the underlying association between excess body weight and cancer [38]. However, no association was also reported by other studies [39].
Briefly, other investigated factors such as education [16], smoking [5,14,19,22,23], alcohol drinking [14,22,24-26], physical activity (sports, walking) [14,22,27-29], and family history of cancer [15,16,21,40] are still inconsistent.
Despite of many strengths mentioned in the introduction, this study has also several limitations. Some of the important factors mentioned by others are not studied, because of data unavailability. For instance, we did not study the association of oral contraceptives and OC mortality, although this factor found as a protective factor by other studies [13,16,37]. Hysterectomy, tubal ligation [13], higher number of abortions [16] and breastfeeding [21] were also found to be protective. Our analyses are based on baseline data and hence we did not consider any changes in investigated factors (e.g., smoking, and drinking). This also may limit our findings as subjects can change their behaviors any time during the long follow-up period. Finally, missing information for different variables which vary from 6.5% (BMI) to 35.5% (age at menopause) may affect the power of the study.
Our significant findings may indicate several implications. For instance, the rate of women remaining single is increasing in Japan, which may cause an increased burden for OC in the future. Similarly, decreasing number of pregnancies and births per woman can also contribute to the higher burden of OC in Japan [10,17]. Likewise, population ageing can contribute to the increasing burden of OC in Japan.
In conclusion, our study revealed both consistent and inconclusive results. Only women with single marital status experienced a significantly higher risk of OC mortality. Although many studies reported higher risks for nulliparous and nullipregnant women, these results are still inclusive in Japan. Other factors also provided inconsistent results when compared with other studies. Despite of these inconsistencies, our findings could still be taken as an important reference because of its strengths in terms of large and representative sample, reliability, and long follow-up.
ACKNOWLEDGMENTS
This work was supported by Grants-in-Aid for Scientific Research from the Ministry of Education, Science, Sports and Culture of Japan (Monbusho), and Grants-in-Aid for Scientific Research on Priority Areas of Cancer, as well as Grants-in-Aid for Scientific Research on Priority Areas of Cancer Epidemiology from the Japanese Ministry of Education, Culture, Sports, Science and Technology (Monbu-Kagaku-sho) (Nos. 61010076, 62010074, 63010074, 1010068, 2151065, 3151064, 4151063, 5151069, 6279102, 11181101, 17015022, 18014011, 20014026 and 20390156).
We like to express our sincere thanks to all participants and researchers related to the JACC study, and all funding bodies which supported our study. Particularly we wish to express our sincere thanks to Drs. Kunio Aoki and Yoshiyuki Ohno, Professors Emeritus of the Nagoya University School of Medicine and former chairpersons of the JACC study. We are also greatly indebted to Dr. Haruo Sugano, former Director of the Cancer Institute, Tokyo, who contributed greatly to the initiation of the JACC study, to Dr. Tomoyuki Kitagawa, Director Emeritus of the Cancer Institute of the Japanese Foundation for Cancer Research and former project leader of the Grant-in-Aid for Scientific Research on Priority Area 'Cancer', and to Dr. Kazao Tajima, Aichi Cancer Center and previous project leader of the Grant-in Aid for Scientific Research on Priority Area of Cancer Epidemiology, for their encouragement and support during this study.
Footnotes
No potential conflict of interest relevant to this article was reported.
Members of the JACC Study Group: The present members of the JACC Study Group who co-authored this paper are: Dr. Akiko Tamakoshi (present chairperson of the study group), Hokkaido University Graduate School of Medicine; Drs. Mitsuru Mori & Fumio Sakauchi, Sapporo Medical University School of Medicine; Dr. Yutaka Motohashi, Akita University School of Medicine; Dr. Ichiro Tsuji, Tohoku University Graduate School of Medicine; Dr. Yosikazu Nakamura, Jichi Medical School; Dr. Hiroyasu Iso, Osaka University School of Medicine; Dr. Haruo Mikami, Chiba Cancer Center; Dr. Michiko Kurosawa, Juntendo University School of Medicine; Dr. Yoshiharu Hoshiyama, Yokohama Soei University; Dr. Naohito Tanabe, University of Niigata Prefecture; Dr. Koji Tamakoshi, Nagoya University Graduate School of Health Science; Dr. Kenji Wakai, Nagoya University Graduate School of Medicine; Dr. Shinkan Tokudome, National Institute of Health and Nutrition; Dr. Koji Suzuki, Fujita Health University School of Health Sciences; Dr. Shuji Hashimoto, Fujita Health University School of Medicine; Dr. Shogo Kikuchi, Aichi Medical University School of Medicine; Dr. Yasuhiko Wada, Faculty of Nutrition, University of Kochi; Dr. Takashi Kawamura, Kyoto University Center for Student Health; Dr. Yoshiyuki Watanabe, Kyoto Prefectural University of Medicine Graduate School of Medical Science; Dr. Kotaro Ozasa, Radiation Effects Research Foundation; Dr. Tsuneharu Miki, Kyoto Prefectural University of Medicine Graduate School of Medical Science; Dr. Chigusa Date, School of Human Science and Environment, University of Hyogo; Dr. Kiyomi Sakata, Iwate Medical University; Dr. Yoichi Kurozawa, Tottori University Faculty of Medicine; Drs. Takesumi Yoshimura & Yoshihisa Fujino, University of Occupational and Environmental Health; Dr. Akira Shibata, Kurume University; Dr. Naoyuki Okamoto, Kanagawa Cancer Center; and Dr. Hideo Shio, Moriyama Municipal Hospital.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Parkin DM, Laara E, Muir CS. Estimates of the worldwide frequency of sixteen major cancers in 1980. Int J Cancer. 1988;41:184–197. doi: 10.1002/ijc.2910410205. [DOI] [PubMed] [Google Scholar]
- 3.Hennessy BT, Coleman RL, Markman M. Ovarian cancer. Lancet. 2009;374:1371–1382. doi: 10.1016/S0140-6736(09)61338-6. [DOI] [PubMed] [Google Scholar]
- 4.Romero I, Bast RC., Jr Minireview: human ovarian cancer: biology, current management, and paths to personalizing therapy. Endocrinology. 2012;153:1593–1602. doi: 10.1210/en.2011-2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Niwa Y, Wakai K, Suzuki S, Tamakoshi K, Lin Y, Yatsuya H, et al. Cigarette smoking and the risk of ovarian cancer in the Japanese population: findings from the Japanese Collaborate Cohort study. J Obstet Gynaecol Res. 2005;31:144–151. doi: 10.1111/j.1447-0756.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- 6.Park B, Park S, Kim TJ, Ma SH, Kim BG, Kim YM, et al. Epidemiological characteristics of ovarian cancer in Korea. J Gynecol Oncol. 2010;21:241–247. doi: 10.3802/jgo.2010.21.4.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ioka A, Tsukuma H, Ajiki W, Oshima A. Ovarian cancer incidence and survival by histologic type in Osaka, Japan. Cancer Sci. 2003;94:292–296. doi: 10.1111/j.1349-7006.2003.tb01435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim K, Zang R, Choi SC, Ryu SY, Kim JW. Current status of gynecological cancer in China. J Gynecol Oncol. 2009;20:72–76. doi: 10.3802/jgo.2009.20.2.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kato I, Tominaga S, Kuroishi T. Relationship between westernization of dietary habits and mortality from breast and ovarian cancers in Japan. Jpn J Cancer Res. 1987;78:349–357. [PubMed] [Google Scholar]
- 10.Mori M, Harabuchi I, Miyake H, Casagrande JT, Henderson BE, Ross RK. Reproductive, genetic, and dietary risk factors for ovarian cancer. Am J Epidemiol. 1988;128:771–777. doi: 10.1093/oxfordjournals.aje.a115030. [DOI] [PubMed] [Google Scholar]
- 11.Edmondson RJ, Monaghan JM. The epidemiology of ovarian cancer. Int J Gynecol Cancer. 2001;11:423–429. doi: 10.1046/j.1525-1438.2001.01053.x. [DOI] [PubMed] [Google Scholar]
- 12.Moorman PG, Calingaert B, Palmieri RT, Iversen ES, Bentley RC, Halabi S, et al. Hormonal risk factors for ovarian cancer in premenopausal and postmenopausal women. Am J Epidemiol. 2008;167:1059–1069. doi: 10.1093/aje/kwn006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braem MG, Onland-Moret NC, van den Brandt PA, Goldbohm RA, Peeters PH, Kruitwagen RF, et al. Reproductive and hormonal factors in association with ovarian cancer in the Netherlands cohort study. Am J Epidemiol. 2010;172:1181–1189. doi: 10.1093/aje/kwq264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiderpass E, Sandin S, Inoue M, Shimazu T, Iwasaki M, Sasazuki S, et al. Risk factors for epithelial ovarian cancer in Japan - results from the Japan Public Health Center-based Prospective Study cohort. Int J Oncol. 2012;40:21–30. doi: 10.3892/ijo.2011.1194. [DOI] [PubMed] [Google Scholar]
- 15.Parazzini F, Negri E, La Vecchia C, Restelli C, Franceschi S. Family history of reproductive cancers and ovarian cancer risk: an Italian case-control study. Am J Epidemiol. 1992;135:35–40. doi: 10.1093/oxfordjournals.aje.a116199. [DOI] [PubMed] [Google Scholar]
- 16.Tavani A, Negri E, Franceschi S, Parazzini F, La Vecchia C. Risk factors for epithelial ovarian cancer in women under age 45. Eur J Cancer. 1993;29A:1297–1301. doi: 10.1016/0959-8049(93)90077-s. [DOI] [PubMed] [Google Scholar]
- 17.Mori M, Nishida T, Sugiyama T, Komai K, Yakushiji M, Fukuda K, et al. Anthropometric and other risk factors for ovarian cancer in a case-control study. Jpn J Cancer Res. 1998;89:246–253. doi: 10.1111/j.1349-7006.1998.tb00555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schouten LJ, Rivera C, Hunter DJ, Spiegelman D, Adami HO, Arslan A, et al. Height, body mass index, and ovarian cancer: a pooled analysis of 12 cohort studies. Cancer Epidemiol Biomarkers Prev. 2008;17:902–912. doi: 10.1158/1055-9965.EPI-07-2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Polychronopoulou A, Tzonou A, Hsieh CC, Kaprinis G, Rebelakos A, Toupadaki N, et al. Reproductive variables, tobacco, ethanol, coffee and somatometry as risk factors for ovarian cancer. Int J Cancer. 1993;55:402–407. doi: 10.1002/ijc.2910550312. [DOI] [PubMed] [Google Scholar]
- 20.Lacey JV, Jr, Brinton LA, Leitzmann MF, Mouw T, Hollenbeck A, Schatzkin A, et al. Menopausal hormone therapy and ovarian cancer risk in the National Institutes of Health-AARP Diet and Health Study Cohort. J Natl Cancer Inst. 2006;98:1397–1405. doi: 10.1093/jnci/djj375. [DOI] [PubMed] [Google Scholar]
- 21.Sueblinvong T, Carney ME. Current understanding of risk factors for ovarian cancer. Curr Treat Options Oncol. 2009;10:67–81. doi: 10.1007/s11864-009-0108-2. [DOI] [PubMed] [Google Scholar]
- 22.Riman T, Dickman PW, Nilsson S, Nordlinder H, Magnusson CM, Persson IR. Some life-style factors and the risk of invasive epithelial ovarian cancer in Swedish women. Eur J Epidemiol. 2004;19:1011–1019. doi: 10.1007/s10654-004-1633-8. [DOI] [PubMed] [Google Scholar]
- 23.Kjaerbye-Thygesen A, Frederiksen K, Hogdall EV, Glud E, Christensen L, Hogdall CK, et al. Smoking and overweight: negative prognostic factors in stage III epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2006;15:798–803. doi: 10.1158/1055-9965.EPI-05-0897. [DOI] [PubMed] [Google Scholar]
- 24.La Vecchia C, Negri E, Franceschi S, Parazzini F, Gentile A, Fasoli M. Alcohol and epithelial ovarian cancer. J Clin Epidemiol. 1992;45:1025–1030. doi: 10.1016/0895-4356(92)90119-8. [DOI] [PubMed] [Google Scholar]
- 25.Lagiou P, Ye W, Wedren S, Ekbom A, Nyren O, Trichopoulos D, et al. Incidence of ovarian cancer among alcoholic women: a cohort study in Sweden. Int J Cancer. 2001;91:264–266. doi: 10.1002/1097-0215(200002)9999:9999<::aid-ijc1027>3.3.co;2-b. [DOI] [PubMed] [Google Scholar]
- 26.Schouten LJ, Zeegers MP, Goldbohm RA, van den Brandt PA. Alcohol and ovarian cancer risk: results from the Netherlands Cohort Study. Cancer Causes Control. 2004;15:201–209. doi: 10.1023/B:CACO.0000019512.71560.2b. [DOI] [PubMed] [Google Scholar]
- 27.Leitzmann MF, Koebnick C, Moore SC, Danforth KN, Brinton LA, Hollenbeck AR, et al. Prospective study of physical activity and the risk of ovarian cancer. Cancer Causes Control. 2009;20:765–773. doi: 10.1007/s10552-008-9291-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chionh F, Baglietto L, Krishnan K, English DR, MacInnis RJ, Gertig DM, et al. Physical activity, body size and composition, and risk of ovarian cancer. Cancer Causes Control. 2010;21:2183–2194. doi: 10.1007/s10552-010-9638-y. [DOI] [PubMed] [Google Scholar]
- 29.Rossing MA, Cushing-Haugen KL, Wicklund KG, Doherty JA, Weiss NS. Recreational physical activity and risk of epithelial ovarian cancer. Cancer Causes Control. 2010;21:485–491. doi: 10.1007/s10552-009-9479-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tamakoshi A, Ozasa K, Fujino Y, Suzuki K, Sakata K, Mori M, et al. Cohort profile of the Japan Collaborative Cohort Study at final follow-up. J Epidemiol. 2013;23:227–232. doi: 10.2188/jea.JE20120161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ohno Y, Tamakoshi A JACC Study Group. Japan collaborative cohort study for evaluation of cancer risk sponsored by monbusho (JACC study) J Epidemiol. 2001;11:144–150. doi: 10.2188/jea.11.144. [DOI] [PubMed] [Google Scholar]
- 32.Tamakoshi A Japan Collaborative Cohort Study for Evaluation of Cancer. Overview of the Japan Collaborative Cohort Study for evaluation of cancer (JACC) Asian Pac J Cancer Prev. 2007;8(Suppl):1–8. [PubMed] [Google Scholar]
- 33.Sakauchi F, Khan MM, Mori M, Kubo T, Fujino Y, Suzuki S, et al. Dietary habits and risk of ovarian cancer death in a large-scale cohort study (JACC study) in Japan. Nutr Cancer. 2007;57:138–145. doi: 10.1080/01635580701274178. [DOI] [PubMed] [Google Scholar]
- 34.Niwa Y, Yatsuya H, Tamakoshi K, Nishio K, Kondo T, Lin Y, et al. Relationship between body mass index and the risk of ovarian cancer in the Japanese population: findings from the Japanese Collaborate Cohort (JACC) study. J Obstet Gynaecol Res. 2005;31:452–458. doi: 10.1111/j.1447-0756.2005.00319.x. [DOI] [PubMed] [Google Scholar]
- 35.Yoshida M, Kondo K, Tada T. The relation between the cancer screening rate and the cancer mortality rate in Japan. J Med Invest. 2010;57:251–259. doi: 10.2152/jmi.57.251. [DOI] [PubMed] [Google Scholar]
- 36.Machii R, Saika K, Higashi T, Aoki A, Hamashima C, Saito H. Evaluation of feedback interventions for improving the quality assurance of cancer screening in Japan: study design and report of the baseline survey. Jpn J Clin Oncol. 2012;42:96–104. doi: 10.1093/jjco/hyr185. [DOI] [PubMed] [Google Scholar]
- 37.Parazzini F, Franceschi S, La Vecchia C, Fasoli M. The epidemiology of ovarian cancer. Gynecol Oncol. 1991;43:9–23. doi: 10.1016/0090-8258(91)90003-n. [DOI] [PubMed] [Google Scholar]
- 38.Ceschi M, Gutzwiller F, Moch H, Eichholzer M, Probst-Hensch NM. Epidemiology and pathophysiology of obesity as cause of cancer. Swiss Med Wkly. 2007;137:50–56. doi: 10.4414/smw.2007.11435. [DOI] [PubMed] [Google Scholar]
- 39.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–578. doi: 10.1016/S0140-6736(08)60269-X. [DOI] [PubMed] [Google Scholar]
- 40.Kasprzak L, Foulkes WD, Shelling AN. Forth nightly review: hereditary ovarian carcinoma. BMJ. 1999;318:786–789. doi: 10.1136/bmj.318.7186.786. [DOI] [PMC free article] [PubMed] [Google Scholar]


