Cystic fibrosis–related diabetes (CFRD) is the most common comorbidity in patients with cystic fibrosis (CF) (1). Consensus guidelines state that all patients above the age of 10 years should be screened annually for CFRD with a 2-h 75-g oral glucose tolerance test (OGTT) (2). There are four categories of glucose tolerance based on OGTT fasting and 75-g 2-h glucose levels: normal glucose tolerance, impaired glucose tolerance (IGT) with 2 h level 7.8–11.1 mmol/L, CFRD without fasting hyperglycemia (CFRD FH−) with 2-h level > 11.1 mmol/L, and CFRD with fasting hyperglycemia (CFRD FH+) (2).
At our institution in 2011, there were 167 pre–lung transplant adult CF patients, of whom 46 had preexisting CFRD. Of the remaining, 28 agreed to the test; 3 were found to have CFRD FH−, 1 was found to have CFRD FH+, and 1 had an incomplete test. Of the remaining 23, 7 had IGT.
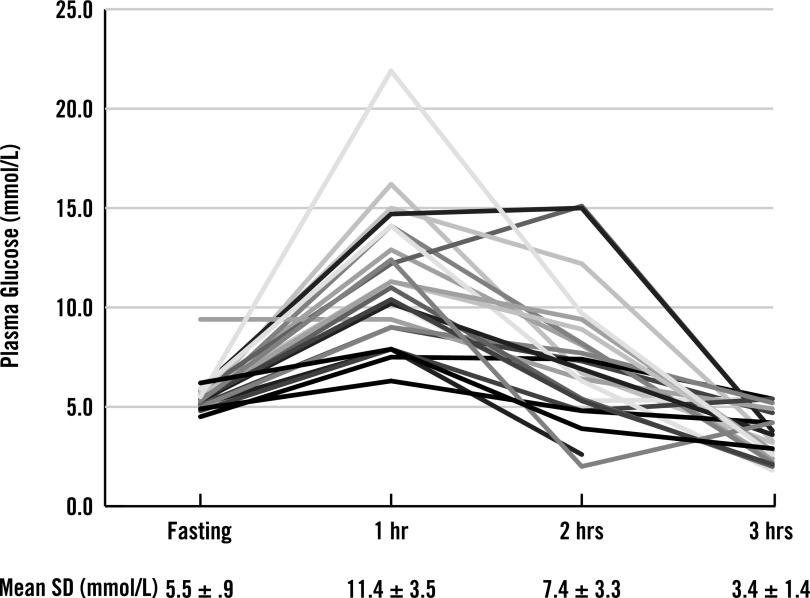
For the 28 who agreed to testing, age, sex, and BMI were 27.2 ± 5.9 years of age, 61% male, and 22.2 ± 2.7 kg/m2. For the 23 without CFRD, fasting and 1-, 2-, and 3-h glucose levels were 5.5 ± 0.9 mmol/L, 11.4 ± 3.5 mmol/L, 7.4 ± 3.3 mmol/L, and 3.4 ± 1.2 mmol/L, respectively (Fig. 1). At 2 h, one patient with symptomatic hypoglycemia at 2.4 mmol/L did not continue. At 3 h, 13 of the remaining 22 (59%) were found to have blood glucose levels <3.9 mmol/L, 10 (45%) had levels <3.3 mmol/L, 6 (27%) had levels <2.8 mmol/L, and 3 (14%) had levels <2.2 mmol/L.
Figure 1.
Serum glucose of 23 CF patients undergoing an OGTT over a 3-h time period. There can be marked hypoglycemia at both the 2-h and 3-h time point. hr, hour.
The benefit of identification of CFRD and IGT in CF is supported by a small improvement in BMI (0.39 BMI units) in patients with CFRD FH− treated with insulin in a 1-year randomized multicenter study (3). Epidemiological studies have shown that higher BMI is an independent predictor of improved survival in CF.
Hyperglycemia in CF appears to be primarily due to β-cell failure over time (4). What is not as well understood are the dynamics of islet hormones in an adult CF population, particularly glucagon secretion with meals or hypoglycemia. In our patients, we saw frequent hypoglycemia 3 h after a 75-g oral glucose load and occasionally at the 2-h time point. While 3-h OGTT glucose levels have not been measured before, fasting hypoglycemia has been described in a pediatric and adult CF population (5).
Our patients were symptomatic, and although no one required assistance for treatment, glucose levels <2.2 mmol/L in patients represents islet pathology. While glucagon deficiency in the context of a delayed insulin response is an attractive possibility for etiology, further study is required to answer this question.
In conclusion, 3-h testing for CFRD in adults with an OGTT can result in 3-h hypoglycemia; patients should be cautioned regarding the symptoms of hypoglycemia after a 2-h test along with measures to treat those symptoms. The etiology and long-term significance of the CF abnormal glucose response warrants further study.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
I.B.H. drafted the manuscript. M.M.J. reviewed the manuscript and provided comments and assisted in data collection. C.H.G. reviewed the manuscript and provided comments. M.L.A. drafted the manuscript. I.B.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank Lori Menalia, RN, and Deanne Berg-Jurkovich, RN, both of the University of Washington Medical Center, for assistance in the collection of data.
References
- 1.Moran A, Dunitz J, Nathan B, Saeed A, Holme B, Thomas W. Cystic fibrosis-related diabetes: current trends in prevalence, incidence, and mortality. Diabetes Care 2009;32:1626–1631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moran A, Brunzell C, Cohen RC, et al. CFRD Guidelines Committee Clinical care guidelines for cystic fibrosis-related diabetes: a position statement of the American Diabetes Association and a clinical practice guideline of the Cystic Fibrosis Foundation, endorsed by the Pediatric Endocrine Society. Diabetes Care 2010;33:2697–2708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moran A, Pekow P, Grover P, et al. Cystic Fibrosis Related Diabetes Therapy Study Group Insulin therapy to improve BMI in cystic fibrosis-related diabetes without fasting hyperglycemia: results of the cystic fibrosis related diabetes therapy trial. Diabetes Care 2009;32:1783–1788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Battezzati A, Mari A, Zazzron L, et al. Identification of insulin secretory defects and insulin resistance during oral glucose tolerance test in a cohort of cystic fibrosis patients. Eur J Endocrinol 2011;165:69–76 [DOI] [PubMed] [Google Scholar]
- 5.Battezzati A, Battezzati PM, Costantini D, et al. Spontaneous hypoglycemia in patients with cystic fibrosis. Eur J Endocrinol 2007;156:369–376 [DOI] [PubMed] [Google Scholar]