Abstract
Human motor activity has a robust, intrinsic fractal structure with similar patterns from minutes to hours. The fractal activity patterns appear to be physiologically important because the patterns persist under different environmental conditions but are significantly altered/reduced with aging and Alzheimer's disease (AD). Here, we report that dementia patients, known to have disrupted circadian rhythmicity, also have disrupted fractal activity patterns and that the disruption is more pronounced in patients with more amyloid plaques (a marker of AD severity). Moreover, the degree of fractal activity disruption is strongly associated with vasopressinergic and neurotensinergic neurons (two major circadian neurotransmitters) in postmortem suprachiasmatic nucleus (SCN), and can better predict changes of the two neurotransmitters than traditional circadian measures. These findings suggest that the SCN impacts human activity regulation at multiple time scales and that disrupted fractal activity may serve as a non-invasive biomarker of SCN neurodegeneration in dementia.
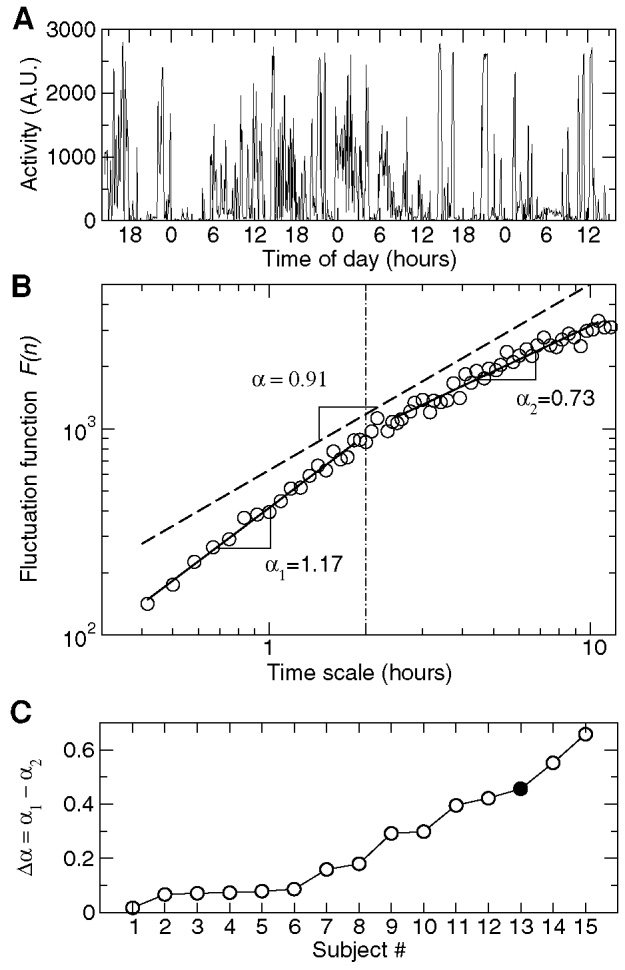
Aging and dementia are associated with disturbances in sleep and daily activity rhythms1,2,3 that are the main reason for the institutionalization of elderly dementia patients. Pathological mechanisms underlying these behavioral disturbances are not fully understood. One possible mechanism involves neurodegenerative changes in the central circadian pacemaker (suprachiasmatic nucleus: SCN) as supported by both human and animal studies4,5,6,7. SCN dysfunction can disrupt circadian rhythms of behavior and physiology and their synchrony with day-night/light-dark cycles8. Non-invasive and reliable assessment of SCN dysfunction is still a challenge in human studies. Traditional approaches based on circadian rhythmicity of behavior and core body temperature can be significantly complicated by many environmental influences such as from housing and light conditions, nursing home schedules for feeding and sleep, and interactions between patients and caregivers. New approaches that that are not confounded by these masking effects are needed to define the role of SCN dysfunction in the progression of dementia.
Fractal fluctuations — similar temporal structures at different time scales — are observed in many neurophysiological signals, including motor and brain activity9,10. Such dynamic patterns are robust in healthy physiological systems but are significantly altered/reduced with aging and disease11. Based on experimental and theoretical physics research, fractal patterns emerge as an integrated behavior on a system level, reflecting networks of elaborate feedback processes that interact across multiple control components and across a wide range of temporal scales12. From lesion studies in rats, we previously found that an intact SCN is necessary for the maintenance of fractal activity patterns13. In humans we showed fractal activity regulation is reduced with aging and Alzheimer's disease (AD)14,15 that are also accompanied by neuroanatomical changes in the SCN4,16. Thus, we hypothesized that SCN degeneration is responsible for the disrupted fractal activity regulation and that the disruption increases as AD progresses. To test these hypotheses, we analyzed existing antemortem actigraphy records (Fig. 1A) of 20 dementia patients (15 AD) and related these results to the number of vasopressinergic and neurotensinergic neurons in postmortem SCN tissue, and to occipital cortical amyloid plaque burden (a marker of AD severity) that were all taken from these same patients17. Moreover, we examined whether the use of a measure of fractal disruption can improve the prediction of the changes in the SCN.
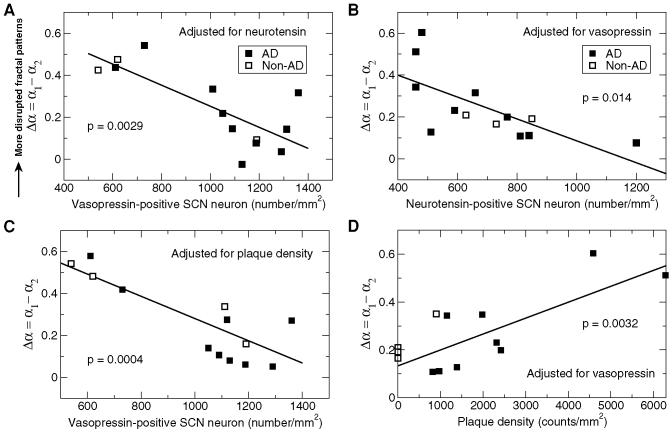
Figure 1. Alterations of fractal correlations in motor activity fluctuations in dementia patients.
(A) 72-hour activity recording of a representative dementia patient. (B) Detrended fluctuation function F(n) of the activity signal shown in (a). F(n) displayed different power-law behavior with different scaling exponent, α1 and α2, at time scales smaller than and larger than ~ 2 hours (indicated by dotted dashed line). For comparison, F(n) of young adults as observed in a previous study13 was also plotted (dashed black line). (C) Difference between α1 and α2 for all subjects (except for 5 individuals with no α2 due to many missing data points in their recordings). The subject # 13 (filled circle) is the patient whose data are shown in (A) and (B).
Results
Altered fractal activity patterns in dementia
To assess fractal patterns in activity fluctuations, we performed detrended fluctuation analysis (DFA)18 which quantifies fluctuation amplitudes F(n) across different time scales n. Using the DFA, we previously found that activity fluctuations of healthy young individuals possess robust fractal correlations as characterized by a power-law function F(n) ~ nα, with the scaling exponent α ~ 0.9 (Fig. 1B)15. Here we found that the fluctuation function of dementia patients generally deviated from a simple power-law form, displaying different patterns in two time-scale regions (Fig. 1B). At time scales n < ~ 2 hours, the fluctuation function showed a power-law form with the exponent α1 = 1.13 ± 0.03 (SE). At time scales n > ~ 2 hours, the fluctuation function also showed a power-law behavior but the exponent α2 (the exponent α at time scales > ~ 2 hours) was smaller than α1 (the exponent α at time scales < ~ 2 hours) (Fig. 1 B to C). The difference in fractal correlations between the two regions indicates an overall reduction of fractal regulation. Thus, we used the difference between the two exponents (Δα = α1 − α2; mean ± SE: 0.25 ± 0.05) to quantify the degree of disturbed fractal regulation: a larger Δα indicates more disrupted fractal regulation.
Associations between fractal activity disruption and circadian neurotransmitters
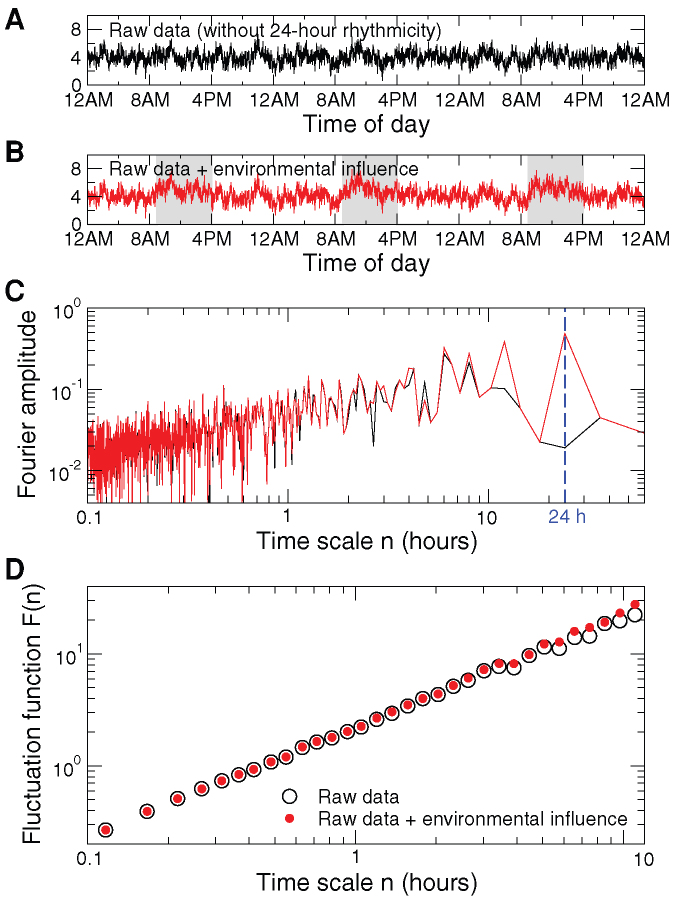
Next, we tested whether the disturbed fractal activity regulation in these dementia patients reflected SCN dysfunction. We quantified SCN neurons containing vasopressin or neurotensin that were obtained from postmortem hypothalamic tissue samples of these patients17. We found that Δα was negatively correlated with the number of neurons containing the two major SCN neurotransmitters (vasopressin: p = 0.0029; neurotensin: p = 0.014) (Fig. 2A, B; Model 1 in Table 1). Together, the two circadian neurotransmitters accounted for 72% of variation in Δα. These relationships between disrupted fractal activity and SCN neurotransmitters remained after adjusting for age, latency between behavioral activity recording and time of death (mean ± SE: 0.57 ± 0.13 years), and daily rhythm of neurotransmitter content (see Methods).
Figure 2. More disrupted fractal activity correlations in dementia patients with more reduced neurotransmitter in the SCN.
(A) Δα = α1 − α2 was negatively correlated with the number of vasopressin-positive SCN neurons after adjusting for the effect of the number of neurotensin-positive SCN neurons. (B) Δα was correlated with the number of neurotensin-positive SCN neurons after adjusting for the effect of the number of vasopressin-positive SCN neurons. Results in (A) and (B) were obtained from 13 subjects with dementia (10 with AD) using a regression model in which the two SCN neurotransmitters (vasopressin and neurotensin) were included as two factors (See Model 1 in Table 1). (C) α1-α2 was correlated with the number of vasopressin-positive SCN neurons after adjusting for the effect of AD severity as characterized by the plaque density from occipital Bielschowsky stain. (D) α1-α2 was correlated with the AD severity after adjusted for the effect of the number of vasopressin-positive SCN neurons. Results in (C) and (D) were obtained from 13 subjects with dementia (9 with AD) using a regression model in which vasopressin neuronal density and plaque density were included as two factors (see Model 2 in Table 1).
Table 1. Specification of regression models for prediction of disrupted fractal activity regulation (Models 1 and 2) and SCN neurotransmitters (Models 3 and 4). p1: p values for models; p2:p values for independent factors; AICc: corrected Akaike's information criterion value; ACBTR: amplitude of core body temperature rhythm, AMAR: amplitude of motor activity rhythm, IV: intraday variability.
| Response | DFtotal | DFmodel | R2 | p1 | AICc | Fixed Effects | t Ratio | p2 | |
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Δα | 12 | 2 | 0.72 | 0.0018 | −7.1 | vasopressin | −3.92 | 0.0029 |
| neurotensin | −2.97 | 0.014 | |||||||
| Model 2 | Δα | 12 | 2 | 0.78 | 0.0005 | −11.6 | vasopressin | −5.19 | 0.0004 |
| plaque density | 3.86 | 0.0032 | |||||||
| Model 3a | vasopressin | 18 | 3 | 0.38 | 0.058 | 90.8 | ACBTR | −0.78 | 0.45 |
| AMAR | −1.60 | 0.13 | |||||||
| IV | −2.76 | 0.015 | |||||||
| Model 3b | vasopressin | 13 | 4 | 0.66 | 0.032 | 75.1 | ACBTR | −0.78 | 0.45 |
| AMAR | −1.26 | 0.24 | |||||||
| IV | −1.9 | 0.09 | |||||||
| Δα | −2.42 | 0.039 | |||||||
| Model 4a | neurotensin | 16 | 3 | 0.18 | 0.45 | 85.3 | ACBTR | 1.28 | 0.22 |
| AMAR | 0.89 | 0.39 | |||||||
| IV | 0.58 | 0.57 | |||||||
| Model 4b | neurotensin | 11 | 4 | 0.77 | 0.023 | 63.1 | ACBTR | 0.40 | 0.70 |
| AMAR | 2.79 | 0.027 | |||||||
| IV | 2.96 | 0.021 | |||||||
| Δα | −3.88 | 0.0061 |
Effect of severity of Alzheimer's disease
We then tested whether disturbed fractal activity regulation was specifically related to neurodegenerative changes in the SCN associated with dementia, independent of AD severity per se. To estimate AD severity, we measured amyloid plaque density in the occipital cortex19. After adjusting for the effect of plaque density, we found an even more significant association between fractal disruption and vasopressin cell number in the SCN (Fig. 2C, Model 2 in Table 1). This result indicates that the association between vasopressin and fractal disruption is independent of AD severity. However, the association between neurotensin and fractal activity control was related to AD severity because this association became not significant (p > 0.3) after controlling for plaque density and vasopressin. Furthermore, after accounting for the effect of vasopressin, we also observed a positive correlation between Δα and plaque density (p = 0.0032) (Fig. 2D), suggesting that patients with more severe AD had more disrupted fractal regulation.
Prediction for changes of neurotransmitters in the SCN
We further examined how the altered fractal activity patterns can help to predict changes in circadian neurotransmitters and how such a fractal marker compares to more traditional markers. We considered three traditional circadian measures: (1) the circadian amplitude of core body temperature: 0.32 ± 0.03 (SE) °C, range: 0.11 – 0.72°C; (2) the circadian amplitude of motor activity: 116 ± 25, range: 1.7 – 427; and (3) intraday variability in motor activity: 1.15 ± 0.08, range: 0.42 – 1.82. The regression model with the three circadian measures accounted for 38% of variation in vasopressin (Model 3a in Table 1: R2 = 0.38, p = 0.058, AICc = 90.8). Adding Δα to the model significantly improved the prediction to 66% (Model 3b in Table 1: R2 = 0.66, p = 0.032, AICc = 75.1). The reduced AICc indicated a better model fit when Δα was added to the model (adjusting for the number of factors in the model). The effect of Δα on a model in predicting neurotensin was even larger. Without including Δα, the three circadian measures together could account for only 18% of variation in neurotensin (Model 4a in Table 1). With Δα, 77% of variation in neurotensin could be explained (Model 4b in Table 1). In both models (for vasopressin and neurotensin, respectively), Δα was the single most significant predicting factor.
In addition, the nadir of cosinor fit of temperature was at 7:55AM ± 0.6 hours (SE) in these dementia patients, delayed for ~ 5 hours as compared to the elderly controls (nadir at ~ 3AM) as previously reported20,21,22,23. However, adding the temperature nadir did not improve the fits of the models for vasopressin and neurotensin in these patients because this circadian phase measure was not associated with the two neurontransmitters (both p > 0.65).
Discussion
Fractal patterns are a robust, intrinsic characteristic of motor activity regulation in healthy young humans14,15. Similar to disrupted circadian rhythmicity, disrupted fractal activity patterns in dementia reflect behavioral disturbances in these patients. The positive association between the fractal disruption and AD severity indicates that complex behavioral organization deteriorates as AD progresses. The effect of AD severity on fractal regulation may be partially mediated through its influence on neurotensin because: (i) senile plaque formation associated with AD severity is thought to contribute to neurodegeneration and neurotransmitter changes in the SCN (and not the other way around); (ii) plaque density was correlated with neurotensin content (p = 0.016) (Fig. 3); and (iii) the effect of neurotensin on Δα became not significant (p > 0.3) after controlling plaque density and vasopressin. Moreover, the strong correlation between the disrupted fractal activity and SCN neurotransmitters provides evidence that the SCN dysfunction underlies disturbed fractal regulation in dementia. It is worth noting that fractal activity patterns reveal a unique aspect of behavioral control at multiple time scales (i.e., dynamic properties of activity fluctuations from minutes to hours) that is different from and complementary to circadian rhythmicty24. Thus, the impact of the SCN dysfunction on fractal activity patterns also suggests a multiscale regulatory function of the human SCN.
Figure 3. Association between neurotransmitter content in the SCN and amyloid plaque density in the occipital cortex.
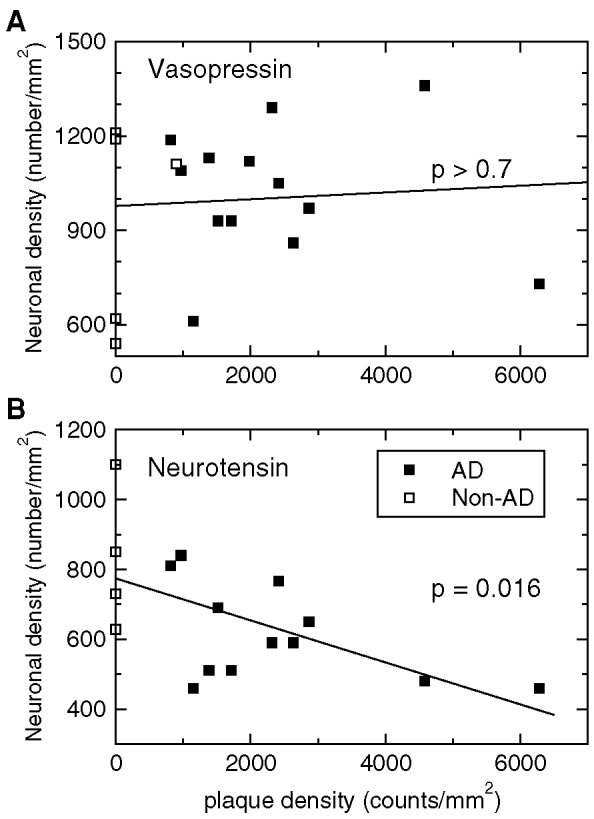
Only neurotensin neuronal density (not assessed in 1 AD and 1 frontotemporal dementia patients) was significantly associated with plaque density (R2 = 0.35, p = 0.016), i.e., patients with more plaques had fewer neurotensin-positive SCN neurons.
Based on concepts of modern statistical physics and nonlinear dynamic theory, fractal activity patterns are more resilient to external influences (e.g., scheduled behavior and environmental conditions) that can significantly impact traditional measures such as mean, variation and rhythmicity of motor activity14,15,25. For instance, dementia patients in a nursing home may have regular daily schedule of interactions with caregivers. These scheduled events can induce apparent 24-hour rhythmicity in activity fluctuations even thought patients themselves may have abolished endogenous circadian control (Figure 4). In contrast, scheduled events have less impact on fractal patterns in activity fluctuations. Thus, fractal measures may better reflect intrinsic alterations in the circadian control network. Consistently, this study showed that fractal activity patterns are very sensitive to neuronal changes in the SCN. The single fractal measure increased the combined predictive power of three traditional circadian measures by ~ 1.7 times for vasopressin, and by ~ 4.2 times for neurotensin. These results do not refute the value of traditional circadian measures for the assessment of SCN dysfunction. Indeed both fractal and circadian measures clearly showed altered behavioral control in dementia and/or AD patients14,15,17
Figure 4. Effects of scheduled daily events on assessments of circadian rhythmicity and fractal patterns.
(A) Simulated 72-hour activity recording that possesses fractal correlations but no 24-h rhythm. (B) The same signal as shown in A except for an increased activity level between 9AM and 4PM that was used to simulate the environmental influence due scheduled daily events. (C) Fourier amplitudes of the signals shown in (A) and (B). (D) Detrended fluctuation function F(n) of the signals shown in (A) and (B). Daily events led to a significant 24-hour rhythm (C) but barely affected fractal patterns as revealed by detrended fluctuation analysis (D).
Identifying and monitoring the SCN dysfunction and its associated behavioral disturbances are particularly important for dementia care. With an identified target (i.e., neuronal degeneration in the SCN), more efficient therapies and treatments may be designed to improve the quality of life of people with the disease. For instance, light and/or melatonin can be used to restore perturbed circadian rhythms of physiological functions (e.g., disrupted sleep, daily behavioral cycles, and cognition) that are associated with the SCN dysfunction26,27. Our results suggest that disrupted fractal activity may server as a non-invasive, sensitive biomarker for SCN deterioration in dementia. However, without a comprehensive mechanistic understanding of fractal regulation and its degradation in dementia, interventions/treatments targeted at restoring the regulation in dementia patients are still not feasible at the current stage. Despite the relevance of the SCN to fractal activity patterns as indicated by this and previous studies4,5,6,7, the neurophysiological basis for fractal regulation is still elusive. One possible theory is related to the interactions between different physiological functions. To achieve an ideal system performance, maintaining circadian rhythmicity in behavior and physiology is important but may not be sufficient. An appropriate orchestration of circadian rhythms in different physiological processes (their phase relationship) is demanding and is believed to be the important functional role of the master circadian clock28. Can the involvement of the SCN in fractal regulation reflect the dynamic process of the SCN-enabled orchestration among many physiological functions? If confirmed, the theory should provide a specific neurophysiological basis for the widely accepted belief that fractal patterns in physiology indicates system integrity and flexibility11. Further studies are warranted to test this hypothesis and to determine the neural circuitry for fractal regulation.
This is a pilot study with a small sample size. In this study we only considered two major circadian neurotransmitters in humans, i.e., vasopressin and neutotensin. Another important circadian neurotransmitter in mammals is vasoactive intestinal peptide (VIP) that was not assessed in the human study. How the change in VIP affects fractal activity regulation should be examined in further studies. Furthermore, large-scale longitudinal studies are needed to determine the time course of fractal activity disruptions during the progression of dementia and to test whether fractal disruptions can serve as a diagnostic marker for the early onset of the disease process.
Methods
Subjects
We utilized existing data from 20 male, dementia patients (62–80 years) including 15 with Alzheimer's Disease (AD), 4 with frontotemporal dementia, and 1 with dementia with Lewy bodies who were residing at the E. N. Rogers Memorial (ENRM) Veterans Administration (VA) Hospital Geriatric Research, Education and Clinical Center (GRECC) in Bedford, MA. All subjects were admitted with a diagnosis of possible or probable dementia disease17. Dementia (or AD) was confirmed after postmortem neuropathological diagnosis (see below). Among the 15 AD patients, there were three subjects with Braak stage 3–4 and eleven subjects with Braak stage 5–6 (Braak stage for one subject missing). The Institutional Review Boards of the McLean and ENRM VA Hospitals approved the protocol and informed consent for this study. Informed consent was obtained from the subject's next-of-kin in accordance with the VA's human subjects' research policies on surrogate consent.
Study procedure
Details of the procedure were published previously17. Briefly, following provision of informed consent, physiological recordings were obtained every 6 months for the duration of the 3-year data collection portion of the study using a 72 hour data-collection protocol. All subjects were free from significant intercurrent illness and were taking no antipyretic medication for at least 24 hour prior to the time of physiological recording. Subjects were studied in their accustomed environment on the GRECC unit following standard ward routines. No effort was made to control light, food, nursing care, the patient's sleep schedule or any other masking influences during data collection. The age of patients at time of last study was 69.5 ± 1.5 (SE) years. Upon death of the subjects, consent was obtained from the subjects' next-of-kin for autopsy and subsequent donation of their brains to the Alzheimer's Disease Research Center Brain Bank at the ENRM VA Hospital. Consent for this portion of the study was obtained independently without any linkage to the prior, physiological data collection. At time of death subjects' mean age was 70.1 ± 1.4 (SE) years with a mean latency from last physiological recording to death of 0.57 ± 0.13 (SE) years (the maximum latency ~ 2 years). Only 6 subjects survived to undergo the protocol more than once.
Data acquisition
During each 72-hour data collection protocol, locomotor activity data were recorded continuously collected by an ambulatory activity monitor (AM-16, Ambulatory Monitoring Inc., Ardsley, NY) featuring a piezoelectric bender sensitive to accelerations of 0.01 g. Activity counts were accumulated over 5 minute epochs and written to memory. Core body temperature was recorded simultaneously by a rectal thermistor (YSI, series 400, Yellow Springs, OH) that sampled the temperature data every 6 minutes throughout the 72-hour data-collection period. All activity and temperature recordings except for one AD patient have been previously published17 and were used for a secondary analysis in this study.
Neuropathological examination
Brains were coronally sectioned after being fixed in neutral buffered formalin for > 4 weeks. Then the hypothalamus was dissected from the brains for the examination of the suprachiasmatic nucleus (SCN). Fourteen different brain areas were then sampled to determine the diagnosis of Alzheimer's disease, dementia with Lewy bodies and other neurodegenerative dementias in accordance with standardized criteria4,29. To quantify the severity of AD, the amyloid plaque density was measured in the occipital cortex using Bielschowsky silver stain (not available in 2 AD patients)19. Neuropathologic diagnoses were confirmed independently by two board-certified neuropathologists.
SCN immunohistochemistry
Utilizing stereological sampling methods17 in accordance with the principles described by Weibel30, the degeneration and function of the SCN were quantified by glia/neuron ratio and by counts of SCN-neurons containing vasopressin or neurotensin, respectively. Hypothalami were blocked, embedded in paraffin and serially sectioned at 8 microns in the coronal plane; the dorsal subdivision of the SCN was identified by examining the Nissl-stain; nuclear diameter and cell density were used to localize the centre of the nucleus; sections from 200 microns on either side of the centre of the dorsal SCN were stained sequentially with Nissl, Bielschowsky silver, Nissl combined with glial fibrillary acidic protein (GFAP), vasopressin and neurotensin; the area of greatest cell density on each slide was selected for analysis. For all cell-counting protocols (glia/neuron ratio, neurotensin and vasopressin) only cells with complete cytoplasmic borders and a clearly visible nucleus were recorded, and the counts obtained from ten separate random 0.1 × 0.1 mm2 fields were averaged. Neurotensin content was not assessed in 2 subjects (1 AD and 1 frontotemporal dementia patients). Glia to neuron ratio was determined by examination of GFAP/Nissl-stained sections. Cells were identified by their respective astrocytic or neuronal staining patterns. The neuroanatomical data except for one AD patient have been previously published17 and were used for a secondary analysis in this study.
Circadian/daily rhythms
To assess circadian/daily rhythmicity, we quantified the amplitude of core body temperature (CBT) rhythm, the amplitude of motor activity rhythm, and intraday variability in motor activity — a measure characterizing fragmentation of the activity rhythm31. To estimate the amplitudes of CBT and activity rhythms, we performed cosinor analyses to fit data using a single harmonic cosine function (24 hours). We calculated the intraday variability by measuring the hour-to-hour variance in the activity data.
Adjustment for daily rhythm in neurotransmitter content
It has been shown that vasopressin synthesis of the human SCN exhibits a circadian or diurnal rhythm32. Due to this rhythmicity, time of death could influence the estimated vasopressin neuronal density. By pooling data from all subjects, we confirmed a significant 24-hour rhythm in vasopressin-containing SCN neurons (p = 0.03)17. Based on the group averaged rhythm, we adjusted the number of vasopressin-containing SCN neurons using cosinor analysis. The analysis based on the adjusted measure (i.e., residue from cosinor fitting) confirmed but did not significantly improve the identified relationship between vasopressin neuronal density and fractal regulation. Given that the postmortem technique only allowed assessment of neurotransmitter content at a single time point per person, any individual differences in the day/night rhythm in vasopressin could not be established. Therefore, the adjustment based on the group average may not reliably account for the effect of time of day on neurotransmitter content for each individual, especially for these dementia patients with disrupted circadian/daily rhythms. In addition, the observed 24-hour rhythm of vasopressin, that was published before17, suggests that the SCNs in some subjects remained rhythmic to a certain degree. No significant dependence of neurotensin neuronal density on time of death was observed in these patients.
Fractal analysis
To estimate fractal patterns in the activity fluctuations at different time scales, we used the detrended fluctuation analysis (DFA)18. Compared with traditional correlation analyses such as power spectral analysis and Hurst analysis, the DFA can accurately quantify correlations in signals that may be masked by underlying nonstationarities or trends33. This method quantifies the detrended fluctuation function, F(n), of activity fluctuations at different time scales n. The DFA algorithm includes four steps: (i) removing the global mean and integrating the time series of an activity signal; (ii) dividing the integrated signal into non-overlapping windows of the same chosen size n; (iii) detrending the integrated signal in each window using polynomial functions to obtain residuals; and (iv) calculating the root mean square of residuals in all windows as fluctuation amplitude F(n). The same four steps were repeated for different time scale n. To eliminate the effect of possible linear trends in original data, we applied the 2nd order DFA, i.e., the 2nd order of polynomial functions were used to detrend data34. A power-law form of F(n) indicates self-similarity (scale-invariance) in the fluctuations, yielding F(n) ~ nα. The parameter α, called the scaling exponent, quantifies the correlation properties in the signal as follows: if α = 0.5, there is no correlation in the fluctuations (“white noise”); if α > 0.5, there are positive correlations, where large activity values are more likely to be followed by large activity values (and vice versa for small activity values). The exponent α = 1.0 indicates highest complexity in the systems. Similar α values (close to 1.0) have been observed in many neurophysiological outputs under normal conditions, indicating complex feedback interactions9,10,11. A further increase in α (> 1) suggests more regular or predicted fluctuations. A special case is α = 1.5 as observed in Brownian motion which is the integral of a white noise signal, i.e., increments of fluctuations are white noise.
In 5 recordings (4 AD and 1 non-AD patients), F(n) could only be obtained at time scales < ~ 4 hours due to missing data in those recordings. Thus, the range of time scales for estimating the scaling exponent at n > 2 hours was too small to obtain reliable α2 for the 5 subjects.
Statistics
To determine effects of the SCN dysfunction on fractal activity regulation, a linear regression model was used to determine the relationships between antemortem fractal activity patterns and postmortem neuropathological measurements of neuronal counts (vasopressin and neurotensin) (Models 1–2 in Table 1). Similar regression models were used to examine how circadian and fractal measures can predict neurotransmitter content (Models 3a–4b).
Author Contributions
K.H., S.A.S. and F.A.J.L.S. conceived and designed the research. E.G.S. and D.G.H. carried out the experiment. K.H. and D.G.H. performed the data analysis. K.H. performed the statistical analysis. All authors wrote the manuscript.
Acknowledgments
The authors wish to thank C. Saper and J. Lu at Beth Israel Deaconess Medical Center for helpful discussions. This work was supported by grants from US National Institutes of Health K99-HL102241 and R00-HL102241 to K.H., R01-AG20654 to D.G.H., K24-HL76446 to S.A.S., P30-HL101299 and R01-HL094806 to F.A.J.L.S, and from National Science Council in Taiwan (ROC) NSC 101-2911-I-008-001 to K.H.
References
- Huang Y. L. et al. Age-associated difference in circadian sleep-wake and rest-activity rhythms. Physiol Behav. 76, 597–603 (2002). [DOI] [PubMed] [Google Scholar]
- Hatfield C. F., Herbert J., Van Someren E. J., Hodges J. R. & Hastings M. H. Disrupted daily activity/rest cycles in relation to daily cortisol rhythms of home-dwelling patients with early Alzheimer's dementia. Brain 127, 1061–1074 (2004). [DOI] [PubMed] [Google Scholar]
- Lim A. S. & Saper C. B. Sleep, circadian rhythms, and dementia. Ann. Neurol. 70, 677–679 (2011). [DOI] [PubMed] [Google Scholar]
- Stopa E. G. et al. Pathologic evaluation of the human suprachiasmatic nucleus in severe dementia. J. Neuropathol. Exp. Neurol. 58, 29–39 (1999). [DOI] [PubMed] [Google Scholar]
- Wu Y. H., Zhou J. N., van Heerikhuize J., Jockers R. & Swaab D. F. Decreased MT1 melatonin receptor expression in the suprachiasmatic nucleus in aging and Alzheimer's disease. Neurobiol. Aging 28, 1239–1247 (2007). [DOI] [PubMed] [Google Scholar]
- Nakamura T. J. et al. Age-related decline in circadian output. J. Neurosci. 31, 10201–10205 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farajnia S. et al. Evidence for neuronal desynchrony in the aged suprachiasmatic nucleus clock. J. Neurosci. 32, 5891–5899 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy J. F., Zeitzer J. M. & Czeisler C. A. Decreased sensitivity to phase-delaying effects of moderate intensity light in older subjects. Neurobiol. Aging 28, 799–807 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chialvo D. R. Emergent complex neural dynamics. Nature Physics 6, 744–750 (2010). [Google Scholar]
- Pittman-Polletta B., Scheer F. A., Butler M., Shea S. A. & Hu K. The role of the circadian system in fractal neurophysiological control. Biological Reviews (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberger A. L., Amaral L., Hausdorff J. M. & Ivanov P. Ch. Fractal dynamics in physiology: alterations with disease and aging. Proc Natl Acad Sci U S A 99, 2466–2472 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassingthwaighte J. B., Liebovitch L. S. & West B. J. Fractal physiology. Oxford university Press US, New York (1994).
- Hu K., Scheer F. A., Ivanov P. C., Buijs R. M. & Shea S. A. The suprachiasmatic nucleus functions beyond circadian rhythm generation. Neuroscience 149, 508–517 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu K. et al. Non-random fluctuations and multi-scale dynamics regulation of human activity. Physica A 337, 307–318 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu K., Van Someren E. J., Shea S. A. & Scheer F. A. Reduction of scale invariance of activity fluctuations with aging and Alzheimer's disease: Involvement of the circadian pacemaker. Proc. Natl. Acad. Sci. U. S. A 106, 2490–2494 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofman M. A. & Swaab D. F. Living by the clock: the circadian pacemaker in older people. Ageing Res. Rev. 5, 33–51 (2006). [DOI] [PubMed] [Google Scholar]
- Harper D. G. et al. Dorsomedial SCN neuronal subpopulations subserve different functions in human dementia. Brain 131, 1609–1617 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng C. K. et al. Mosaic organization of DNA nucleotides. Phys. Rev. E. Stat. Phys. Plasmas. Fluids Relat Interdiscip. Topics. 49, 1685–1689 (1994). [DOI] [PubMed] [Google Scholar]
- Attems J., Jellinger K. A. & Lintner F. Alzheimer's disease pathology influences severity and topographical distribution of cerebral amyloid angiopathy. Acta Neuropathol. 110, 222–231 (2005). [DOI] [PubMed] [Google Scholar]
- Satlin A., Volicer L., Stopa E. G. & Harper D. Circadian locomotor activity and core-body temperature rhythms in Alzheimer's disease. Neurobiol. Aging 16, 765–771 (1995). [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel S. et al. Variations in circadian rhythms of activity, sleep, and light exposure related to dementia in nursing-home patients. Sleep 20, 18–23 (1997). [PubMed] [Google Scholar]
- Harper D. G. et al. Differential circadian rhythm disturbances in men with Alzheimer disease and frontotemporal degeneration. Arch. Gen. Psychiatry 58, 353–360 (2001). [DOI] [PubMed] [Google Scholar]
- Harper D. G. et al. Disturbance of endogenous circadian rhythm in aging and Alzheimer disease. Am. J. Geriatr. Psychiatry 13, 359–368 (2005). [DOI] [PubMed] [Google Scholar]
- Hu K. et al. Fractal Patterns of Neural Activity Exist within the Suprachiasmatic Nucleus and Require Extrinsic Network Interactions. PLoS. One. 7, e48927 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov P. C., Hu K., Hilton M. F., Shea S. A. & Stanley H. E. Endogenous circadian rhythm in human motor activity uncoupled from circadian influences on cardiac dynamics. Proc. Natl. Acad. Sci. U. S. A 104, 20702–20707 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satlin A., Volicer L., Ross V., Herz L. & Campbell S. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimer's disease. Am. J. Psychiatry 149, 1028–1032 (1992). [DOI] [PubMed] [Google Scholar]
- Riemersma-van der Lek R. F. et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 299, 2642–2655 (2008). [DOI] [PubMed] [Google Scholar]
- Reppert S. M. & Weaver D. R. Coordination of circadian timing in mammals. Nature 418, 935–941 (2002). [DOI] [PubMed] [Google Scholar]
- McKee A. C. Brain banking: basic science methods. Alzheimer Dis. Assoc. Disord. 13 Suppl 1, S39–S44 (1999). [PubMed] [Google Scholar]
- Weibel E. Sampling of tissue. pp. 63–100 (Academic Press, New York,1989).
- Witting W., Kwa I. H., Eikelenboom P., Mirmiran M. & Swaab D. F. Alterations in the circadian rest-activity rhythm in aging and Alzheimer's disease. Biol. Psychiatry 27, 563–572 (1990). [DOI] [PubMed] [Google Scholar]
- Hofman M. A. & Swaab D. F. Alterations in circadian rhythmicity of the vasopressin-producing neurons of the human suprachiasmatic nucleus (SCN) with aging. Brain Res. 651, 134–142 (1994). [DOI] [PubMed] [Google Scholar]
- Chen Z., Ivanov P. C., Hu K. & Stanley H. E. Effect of nonstationarities on detrended fluctuation analysis. Phys. Rev. E. Stat. Nonlin. Soft. Matter Phys. 65, 041107 (2002). [DOI] [PubMed] [Google Scholar]
- Hu K., Ivanov P. C., Chen Z., Carpena P. & Stanley H. E. Effect of trends on detrended fluctuation analysis. Phys. Rev. E. Stat. Nonlin. Soft. Matter Phys. 64, 011114 (2001). [DOI] [PubMed] [Google Scholar]