Abstract
OBJECTIVE:
The aim of this study was to assess the cognitive and behavioral development of preterm and low birth weight newborns living in a disadvantageous socioeconomic environment at school age.
METHODS:
This cross-sectional study included children aged 6-7 from a historical birth cohort of preterm (gestational age <37 weeks) and low birth weight (<2,500 g) infants. The Wechsler Intelligence Scale for Children III (WISC-III) was administered by a psychologist while the parents completed the Child Behavior Checklist. The results were compared to the test's reference. The perinatal information and follow-up data were collected from the hospital files. The demographic data were collected from the parents. The current performance was compared with the results from the Denver II and Bayley II tests, which were administered during the first years of life.
RESULTS:
The total intelligence quotient varied from 70 to 140 (mean 98.7±15.8). The borderline intelligence quotient was observed in 9.3% of the children. The Child Behavior Checklist indicated a predominance of social competence problems (27.8%, CI 19.2 to 37.9) compared with behavioral problems (15.5%, CI 8.9 to 24.2). Both the Child Behavior Checklist domains, such as schooling, social and attention problems, and the cognitive scores were significantly associated with maternal education and family income. The results of the Denver and Bayley tests were associated with the cognitive performance (p<0.001) and the Child Behavior Checklist social profile, including aggressive and externalizing behavior (p<0.001).
CONCLUSIONS:
Our data suggest that even low-risk preterm newborns are at risk for developing disturbances in early school age, such as mild cognitive deficits and behavioral disorders. This risk might increase under unfavorable socioeconomic conditions.
Keywords: Cognition; Behavior, Outcome Assessment; Preterm Infants; Low Birth Weight
INTRODUCTION
There is an increasing worldwide survival rate of children who are born very preterm, and this outcome is an emerging public health problem because specialized outpatients clinics to follow up these infants are not fully available, at least in developing countries. The higher survival rates create a population with exceptional needs; numerous studies of the follow up of preterm and very low birth weight infants have demonstrated that these infants have an increased risk for cerebral palsy, cognitive and language delays and emotional/behavioral adjustment problems (1,2). These factors will influence academic achievement at school age because executive deficits might affect school performance and social and adaptative behavior (3-10). The degree of risk increases with decreased gestational age (2,11,12).
The school setting requires the interaction of different attributes, such as cognitive ability, social and emotional competence. Entering the formal educational process requires a child to have complex social abilities and effective functioning. The majority of academic achievement deficits are evident in the early school years, which indicates that neuropsychological assessment at this age is an essential tool for preventing difficulties. The problems diagnosed at this time represent indicators of mental disorders (13,14).
The data concerning the medium or long-term outcomes of preterm newborns in developing South American countries remain inadequate, and specific follow-up programs are difficult to maintain in public institutions. After discharge from a neonatal intensive care unit (NICU), the majority of these infants are followed at primary care facilities. In exceptional cases, a number of university hospitals offer specific programs for follow-up.
The aim of this study was to assess the cognitive and behavioral development of preterm and low birth weight newborns from disadvantaged social and economic environments in southern Brazil once they reach school age.
METHODS
This cross-sectional study included children aged 6-7 years old from a historical birth cohort of preterm (gestational age <37 weeks) and low birth weight (<2,500 g) infants. The infants were born between January 1999 and December 2000, admitted to the NICU of the University Hospital São Lucas of the Pontifícia Universidade Católica do Rio Grande do Sul (HSL/PUCRS) and followed at the neonatal outpatient clinic of the hospital. All patients under current follow-up were invited to participate in this study.
During 1999 and 2000, 520 children were born preterm and with low birth weight and were admitted to the neonatal unit. During the neonatal period, 59 died, and 64 were diagnosed with neonatal neurological disorders. For this study, the sample size was calculated using PEPI program version 4.0 (Abramson and Paul Gahlinger, Salt Lake city, UTAH, USA), based on 15 points of standard deviation and 3 points of error in the WISC scale III, with a confidence interval of 95%. After the sample size was calculated, the first 97 children whose parents answered the invitation, fulfilled the inclusion criteria and concluded the entire evaluation procedure were included in the study (49 girls and 48 boys).
The children included were low-risk preterm neonates who were attending preschool or elementary school and had a stable clinical condition that allowed testing. The exclusion criteria were a previous history of neonatal disorders such as the use of mechanical ventilation for more than 2 weeks, an intracranial hemorrhage grade III or IV, a congenital defect, neonatal seizures, bacterial meningitis, clinical evidence of perinatal asphyxia or the presence of periventricular leukomalacia. The children whose parents did not authorize the evaluation or who had a condition that would preclude testing were excluded.
Information related to pregnancy, delivery, neonatal disorders, previous visits to the outpatient follow-up clinic and the results of the developmental tests were obtained from the hospital files. All children included in the study were evaluated at 12-36 months of life with the Bayley Scale of Infant development version II administered by a psychologist immediately after the follow-up visit). A total of 93 subjects had the Denver II results available (this test was administered by a pediatric neurology fellow during the regular neurological follow-up visit). A number of children included in this study were previously evaluated for language acquisition at 3 years and for behavioral disorders at 4-5 years (15,16).
The neuropsychological assessment consisted of the administration of 2 tests, the Wechsler Intelligence Scale for Children – III (WISC-III) and the Child Behavior Checklist inventory (CBCL), which have been translated into and validated in Portuguese (17,18).
The subjects were tested with the WISC-III and CBCL by a psychologist (RGF) in a specific room that was adequately lit and with low noise, i.e., an appropriate location for cognitive assessment. While the child performed the tasks for the WISC-III, the parents/guardian answered the CBCL questionnaire in the same room. The parents/guardian were told not to interfere with the testing of the child. The results were compared with the test references and the results of the Bayley Scales II and Denver Test II, which were previously administered during follow-up visits.
The WISC scale is used worldwide to assess intelligence/cognition in children aged 6 to 16 years, and the results are expressed as the intelligence quotient (IQ). The mean IQ varies from 80 to 119 points, 79 to 70 is considered borderline and scores below 70 suggest mental retardation. The revised edition (III) enables assessment of intelligence, attention, visual-constructive ability, executive function, language, memory and four indexes derived from factor analyses: the verbal comprehension index, the perceptual organization index, the freedom from distractibility index and the processing speed index. The four indexes show the relevant dimension of the cognitive skills of the subjects (17).
The CBCL is a widely used questionnaire to assess emotional and behavioral problems in children and adolescents. The behavioral scale is composed of 118 items, and the normative data indicate problems (i.e., abnormal results) in patients who score higher than 67 points. Scores over the cut-off point for normality indicate symptomatic patients with clinical expression of behavioral problems. The social scale has 20 items, and its cut-off point is 40. Thus, children with scores over 40 are considered to have normal functioning in social competence/abilities (18).
The data concerning maternal education, occupation and family income (19) were collected in an interview with the parents/guardians.
The majority of the group was evaluated at 7 years of age (n = 88, 98.7%) and attended the first grade of elementary school (n = 87, 89.7%); the remaining children were evaluated at 6 years of age and attended pre-school.
Statistical analysis
The categorical variables were described as percentages. For the continuous variables, we used mean, standard deviation, median and minimum and maximum values. We used the Z test to compare the mean values obtained in the sample with the WISC-III reference. Binomial confidence intervals were used to describe the percentages of the clinical categories for the CBCL. The data were analyzed using SPSS for Windows, v. 15.0.
This project was approved by the Ethics Committee of PUCRS (07/03746), and all parents signed an informed consent.
RESULTS
The characteristics of the sample regarding the perinatal conditions showed a mean gestational age of 33.6±2.0 weeks and a mean birth weight of 1890±4.9 g. Of the births, 65% were by Cesarean section, and the mean Apgar scores at the 1st minute and 5th minute were 7.08±1.8 and 8.52±0.9, respectively. All children presented neonatal disorders, with breathing dysfunction (86.6%) and jaundice (66.0%) being the most prevalent conditions.
Table 1 presents the educational and socioeconomic status of the mothers. In this sample, the majority of the mothers were housewives without personal income. The mean family income was low (2.71±1.2) and varied from 1 to 4 times the Brazilian minimum wage.
Table 1.
Socioeconomic characteristics of the sample.
| Variables | n = 97 (49 girls and 48 boys) |
| Maternal age in years (mean ± standard deviation) | 25.2±6.5 |
| Maternal education n (%) | |
| Did not complete elementary school | 21 (21.6) |
| Completed elementary school | 40 (41.2) |
| Completed high school | 31 (32.0) |
| Graduated | 5 (5.25) |
| Maternal occupation n (%)* | |
| Teacher in an elementary school | 8 (8.2) |
| Worker (self-employed) | 23 (23.9) |
| Non-worker (housewives) | 41 (42.3) |
| Family income (mean±standard deviation)** | 2.71±1.2 |
OBS: *3 mothers died before this study; **income was measured as Brazilian minimum wage.
The results for the WISC-III test in the studied sample showed a mean full scale IQ of 98.7±15.8, a verbal scale IQ of 99.5±13.7, a performance scale IQ of 98.5±16.7, a verbal comprehension index of 98.6±12.9, a perceptual organization index of 98.8±16.4, a freedom from distractibility index of 98.4±15.1 and a processing speed index of 94.4±12.8. The total IQ score varied from 70 to 140. Borderline results (70 to 80) were observed in 9.3% of children for the full scale IQ, 5.2% on the verbal scale, 11.3% on the performance scale, 6.2% on the verbal comprehension index, 12.4% on the perceptual organization index, 13.4% on the freedom from distractibility index and 12.4% on the processing speed index. Between these tests and the reference standard, only the processing speed index showed a significant difference (p<0.001).
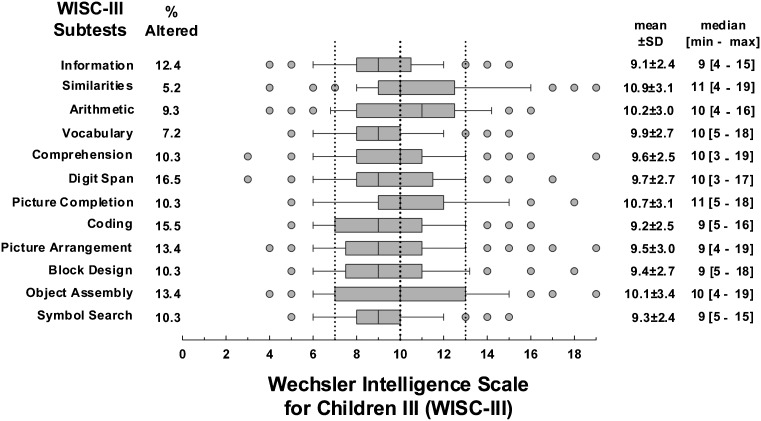
Figure 1 shows the results obtained in the study sample for the WISC-III. The subtests that comprised the verbal and the executive IQ and had the lowest scores, when compared with the mean standard scores of the scale, were digit span, coding, picture arrangement, object assembly and information, on which 16.5%, 15.5%, 13.4%, 13.4% and 12.4% of the children, respectively did not achieve the cut-off point of 7 (minimum value for normality).
Figure 1.
Boxplot graphic for scores on the WISC-III subtests obtained in the study sample. The first six subtests comprise the verbal IQ, and the others comprise the executive IQ The data are presented as the mean ± standard deviation (SD), median, minimum (min), maximum (max) and percentage of observations below the cut-off point 7 (minimum value for normality).
The performance on WISC-III and its associations with birth weight, maternal education and family income are shown in Table 2. We had not observed an association between lower birth weight and WISC performance; however, most of our sample had a birth weight between 1,500 and 2,500 g. A significant association was observed between maternal education/family income and WISC scores.
Table 2.
Performance on the WISC-III scale and its association with birth weight, maternal education and family income (n = 97).
| WISC-III Scale | Low birth weigh (<2500 g) n = 77 | Very low birth weight (1500-2500 g) n = 12 | Extremely low birth weight (<1500 g) n = 8 | Maternal education (rs) | Family income (rs) |
| mean±SD | mean±SD | mean±SD | |||
| IQF | 99.1±15.6a | 96.4±18.7 a | 98.8±14.4 a | 0.385c | 0.399 c |
| IQV | 100.3±13.5a | 93.9±15.1 a | 100±14.4 a | 0.375 c | 0.376 c |
| IQP | 98.3±16.6 a | 100±20.3 a | 98.0±13.4 a | 0.372 c | 0.397 c |
| VCI | 99.3±12.5 a | 94.3±14.8 a | 98.1±14.4 a | 0.344b | 0.357 c |
| POI | 98.4±16.3 a | 101.3±19.8 a | 98.0±13.5 a | 0.375 c | 0.399 c |
| FDI | 98.9±15.1 a | 93.3±16.6 a | 101.5±13.7 a | 0.403 c | 0.366 c |
| PSI | 95.0±12.8 a | 90.9±15.6 a | 94.4±6.80 a | 0.377 c | 0.396 c |
OBS: WISC-III: Wechsler Intelligence Scale for Children – III; IQF: full scale; IQV: verbal scale; IQP: performance scale; VCI: verbal comprehension index; POI: perceptual organization index; FDI: freedom from distractibility index; PSI: processing speed index. aOne-way ANOVA, results not significant (p>0.005). rs = correlation coefficient, bp<0.01, cp<0.001.
The distribution of CBCL scores indicated a predominance of social competence problems (27.8%, CI 19.2 to 37.9) compared with behavioral problems (15.5%, CI 8.9 to 24.2).
Table 3 shows the comparison between the results on WISC-III and CBCL. Full intelligence quotient (IQF), verbal intelligence quotient (IQV) and performance intelligence scale (IQP) were significantly associated with schooling (p<0.001), among the social competence domain and with the total behavior profile (p<0.001), attention (p = 0.001, p = 0.002, p = 0.001) and social problems (p = 0.04, p = 0.017, p = 0.002), respectively.
Table 3.
Correlation between the Wechsler intelligence scale for children (WISC-III) and the various domains of the Child Behavior Checklist (CBCL).
| Domains of the CBCL | rs (IQF) | p | rs (IQV) | p | rs (IQP) | p |
| Total Score Social Competence | -0.21 | 0.042 | -0.20 | 0.052 | -0.20 | 0.049 |
| Activities | 0.20 | 0.056 | 0.17 | 0.098 | 0.20 | 0.051 |
| Sociability | 0.25 | 0.015 | 0.21 | 0.044 | 0.28 | 0.006 |
| Schooling | 0.56 | <0.001 | 0.58 | <0.001 | 0.50 | <0.001 |
| Total Score Behavior Profile | 0.43 | <0.001 | 0.41 | <0.001 | 0.42 | <0.001 |
| Isolation | -0.019 | 0.851 | 0.027 | 0.796 | -0.052 | 0.611 |
| Somatic Complaints | 0.24 | 0.019 | 0.24 | 0.020 | 0.20 | 0.049 |
| Anxiety/Depression | -0.13 | 0.191 | -0.10 | 0.348 | -0.17 | 0.095 |
| Social Problems | -0.29 | 0.004 | -0.24 | 0.017 | -0.31 | 0.002 |
| Thought Problems | 0.05 | 0.645 | 0.07 | 0.492 | 0.05 | 0.604 |
| Attention Problems | -0.33 | 0.001 | -0.31 | 0.002 | -0.33 | 0.001 |
| Delinquent Behavior | -0.034 | 0.742 | -0.06 | 0.582 | -0.01 | 0.888 |
| Aggressive Behavior | -0.18 | 0.087 | -0.19 | 0.067 | -0.14 | 0.166 |
| Internalizing | -0.08 | 0.457 | -0.04 | 0.696 | -0.12 | 0.259 |
| Externalizing | -0.15 | 0.156 | -0.15 | 0.132 | -0.12 | 0.250 |
OBS: Spearman's rank correlation coefficient (rs); significance (p); IQF: full intelligence quotient; IQV: verbal intelligence quotient; IQP: performance intelligence scale.
An attempt to correlate the different domains of the CBCL and the socioeconomic profile of the sample showed significant associations with maternal education and family income (Table 4). No significant correlations were found between CBCL and maternal age.
Table 4.
Correlation between the different domains of the Child Behavior Checklist (CBCL) and socioeconomic profile of the sample.
| CBCL | rs | p | rs | p | rs | p |
| Maternal education | Maternal age | Family income | ||||
| Total Score | -0.32 | 0.001 | 0.07 | 0.529 | -0.13 | 0.214 |
| Social Profile | ||||||
| Activities | 0.22 | 0.034 | -0.22 | 0.032 | 0.02 | 0.849 |
| Sociability | 0.20 | 0.050 | 0.12 | 0.256 | 0.12 | 0.225 |
| Schooling | 0.48 | <0.001 | -0.02 | 0.826 | 0.35 | <0.001 |
| Behavior Profile | ||||||
| Isolation | -0.09 | 0.380 | 0.04 | 0.681 | 0.19 | 0.068 |
| Somatic Complaints | -0.05 | 0.598 | 0.14 | 0.172 | 0.05 | 0.664 |
| Anxiety/Depression | -0.22 | 0.003 | -0.10 | 0.352 | -0.14 | 0.179 |
| Social Problems | -0.34 | 0.001 | -0.03 | 0.812 | -0.24 | 0.020 |
| Thought Problems | -0.10 | 0.350 | 0.14 | 0.185 | 0.01 | 0.950 |
| Attention Problems | -0.38 | <0.001 | -0.01 | 0.973 | -0.31 | 0.002 |
| Delinquent Behavior | -0.10 | 0.352 | 0.10 | 0.346 | 0.03 | 0.768 |
| Aggressive Behavior | -0.24 | 0.017 | 0.12 | 0.230 | -0.08 | 0.431 |
| Internalizing | -0.24 | 0.020 | 0.01 | 0.913 | -0.05 | 0.646 |
| Externalizing | -0.23 | 0.026 | 0.12 | 0.249 | -0.07 | 0.473 |
OBS: Spearman's rank correlation coefficient (rs); significant at p<0.005.
The retrospective data related to the developmental screening applied during follow-up (up to 3 years) showed abnormal Denver test results in 9 subjects. The Bayley mental scale was abnormal in 16 patients, the motor scale was abnormal in 17 patients and the behavioral scale was abnormal in 14 patients. The results of the Denver and Bayley scales were compared with the WISC-III and CBCL. A significant association with all the WISC subtests and the results of the Denver and Bayley (p<0.001) scales was observed. The CBCL total scores significantly correlated with the results of the Bayley and Denver tests (p<0.001) in all social profile domains (p<0.001) and with social, aggressive and externalizing behavior (p<0.001) (Table 5).
Table 5.
Correlation between the results previously obtained on the Bayley Scales and Denver Test II and the different domains of the Child Behavior Checklist (CBCL) and WISC III.
| CBCL | rs (Bayley mental) | p | rs (Bayley motor) | p | rs (Bailey) | p (behavioral) | rs (Denver) | p |
| CBCL Total Score | 0.42 | <0.001 | 0.45 | <0.001 | 0.49 | <0.001 | 0.42 | <0.001 |
| Social Profile | ||||||||
| Activities | -0.27 | 0.008 | -0.32 | 0.002 | -0.30 | 0.003 | -0.21 | 0.043 |
| Social | -0.29 | 0.005 | -0.31 | 0.002 | -0.35 | 0.001 | -0.20 | 0.050 |
| School | -0.61 | <0.001 | -0.62 | <0.001 | -0.60 | <0.001 | -0.58 | <0.001 |
| Total Score | -0.49 | <0.001 | -0.54 | <0.001 | -0.54 | <0.001 | -0.41 | <0.001 |
| Behavior Profile | ||||||||
| Withdrawn | 0.09 | 0.379 | 0.10 | 0.317 | 0.13 | 0.219 | 0.09 | 0.409 |
| Somatic Complaints | -0.07 | 0.498 | -0.02 | 0.860 | -0.5 | 0.648 | -0.13 | 0.227 |
| Anxious/Depressed | 0.20 | 0.049 | 0.21 | 0.040 | 0.30 | 0.004 | 0.18 | 0.080 |
| Social Problems | 0.48 | <0.001 | 0.51 | <0.001 | 0.51 | <0.001 | 0.40 | <0.001 |
| Thought Problems | 0.08 | 0.434 | 0.08 | 0.434 | 0.06 | 0.563 | 0.02 | 0.823 |
| Attention Problems | 0.40 | <0.001 | 0.45 | <0.001 | 0.46 | <0.001 | 0.40 | <0.001 |
| Delinquent Behavior | 0.14 | 0.191 | 0.17 | 0.095 | 0.18 | 0.076 | 0.16 | 0.130 |
| Aggressive Behavior | 0.38 | <0.001 | 0.40 | <0.001 | 0.43 | <0.001 | 0.44 | <0.001 |
| Internalizing | 0.21 | 0.048 | 0.22 | 0.031 | 0.28 | 0.006 | 0.15 | 0.141 |
| Externalizing | 0.35 | 0.001 | 0.38 | <0.001 | 0.40 | <0.001 | 0.41 | <0.001 |
| WISC III | ||||||||
| IQF | -0.711 | <0.001 | -0.688 | <0.001 | -0.670 | <0.001 | -0.631 | <0.001 |
| IQV | -0.699 | <0.001 | -0.663 | <0.001 | -0.640 | <0.001 | -0.637 | <0.001 |
| IQP | -0.656 | <0.001 | -0.651 | <0.001 | -0.640 | <0.001 | -0.567 | <0.001 |
| VCI | -0.678 | <0.001 | -0.649 | <0.001 | -0.620 | <0.001 | -0.626 | <0.001 |
| POI | -0.638 | <0.001 | -0.629 | <0.001 | -0.617 | <0.001 | -0.554 | <0.001 |
| FDI | -0.682 | <0.001 | -0.633 | <0.001 | -0.636 | <0.001 | -0.575 | <0.001 |
| PSI | -0.568 | <0.001 | -0.592 | <0.001 | -0.581 | <0.001 | -0.497 | <0.001 |
OBS: Spearman's rank correlation coefficient (rs); significance was set at p<0.005. IQF: full scale, IQV: verbal scale, IQP: performance scale, VCI: verbal comprehension index, POI: perceptual organization index, FDI: freedom from distractibility index, PSI: processing speed index.
DISCUSSION
Despite the technological and scientific improvements that have largely contributed to the decrease in neonatal mortality, prematurity and low birth weight remain the major causes of neonatal mortality and morbidity, constituting a high risk factor and promoting a significant clinical and epidemiological effect (1,20,21). Specific follow-up facilities to assess the short- and long-term outcomes of preterm newborns have been established in many tertiary centers worldwide, and an extensive amount of data has been published in the last years concerning this subject (20).
In developing countries and specifically in Brazil, the percentage of survivors who are discharged from NICU care has also increased because of improvement in the accessibility of high technological procedures in tertiary and university hospitals (22). Few programs for the long-term follow-up of survivors are available, and the majority of them are concentrated in specific university hospitals in the southern, southeast or northeast regions of the country (15,16),.
In this study, we have demonstrated that even a selected population of low neurological risk preterm newborns might face learning difficulties and behavioral problems when entering school. As previously suggested by Golden (32), IQ is a consequence of current intelligence plus environment and motivation, which indicates that intelligence is an interaction between the environment and biological skills. The assessment of high-risk children who are preterm, have a low birth weight and have been raised in unfavorable socioeconomic condition is justified because low social status is a predictor of poor cognitive outcome even in children raised in developed countries (33,34). One of the limitations of this study was being unable to include children who were born in the same institution at term and had comparable socioeconomic backgrounds as a control group to further explore our findings. This type of follow-up is very difficult to achieve because normal children are discharged from the hospital directly to primary care centers near their homes and do not retain contact with the tertiary care institution of their birth. Because the instruments applied in the neuropsychological evaluation were translated into and validated for the Brazilian population and have standard references of normality, the results obtained in our sample were compared to the reference values of the tests. The design (cross-sectional) might be another limitation of the study, and the ideal design for follow-up studies is birth cohorts or prospective studies. Although part of the information used in this study was collected from the database of the historical cohort, the neuropsychological evaluation was prospective.
Previous studies have shown that the preterm status of a child per se may affect academic achievement and performance from school age to adolescence (1),. The data regarding Brazilian studies are controversial; some authors have reported cognitive impairment at school age in very low birth weight neonates (23-25), and others have not (27). In this study, no significant cognitive impairment was observed; however, our sample consisted of low neurological risk newborns, the majority of them with birth weight from 1500 to 2500 g.
Learning difficulty is typically understood in its functional aspect in the school setting, i.e., as a discrepant performance of the abilities measured by the IQ. Despite a normal global intellectual functioning according to standardized tests, premature children would be more likely to have disabilities in school performance (35). For each premature child, the mean IQ tends to decrease as the gestational age decreases, and there is a forecasted decrease of approximately 1.7 points for each week (13) of prematurity. In our study, the only IQ component that differed significantly from the reference scale was the processing speed index; a small percentage of the children (9.3%) achieved borderline results (from 70 to 80 points) for the full IQ scale. When we analyzed separately the subtests of the WISC III, lower significant scores were found in 2 domains of the verbal IQ and in 2 domains of the performance IQ. Clinically, the IQV is related to factors that are dependent on learning and previous acquisitions, and the IQP is related to maturational aspects. A low level of maternal education and lower family income were also associated with deficits on some subtests.
One of the reasons for the lower school achievement of preterm and low birth weight children is that they are more subject to emotional and behavioral problems that might influence school performance (5,36). We observed that our population was more vulnerable to behavioral and emotional problems because a number of the children were detected as having attention problems, anxiety, depression or aggressive behavior, which might influence academic performance. Co-morbidity between learning deficits and behavior problems has been reported by other authors, as we found in our sample (13,23), and possible explanations for these findings might be related to the maternal level of education and family income. Méio et al. studied a Brazilian sample and considered a low maternal level of education and low income as risk factors for developmental delay (23). Bradley and Corwyn showed that the educational level of the parents is the best socioeconomic predictor for school performance during adolescence (37).
In the social competence profile, the children in the sample group demonstrated altered scores on those scales, which are expected because of their decreased participation in social activities; this decreased participation causes peer integration problems that affect social life. The low income family factor prevents attendance at social activities. The decreased social activity of preterm and low birth weight children, which occurs as a consequence of exposure to unfavorable personal and social factors such as low income family income, low maternal education and a low stimulation home environment, was previously reported (14). Growing up in low-income households is considered as a risk for learning problems and deficits in executive functioning and is also a risk in children born extremely preterm (38).
In the behavior profile of the study population, the lowest behavior scores were obtained relative to attention problems, anxiety and depression and aggressive behavior. Co-morbidity between the learning deficits in the verbal and non-verbal subtype scores associated with behavior problems has been previously described (13,14). Our results showed that preterm and low birth weight children with verbal learning deficits have a greater probability of presenting clinical levels of behavioral problems and are more likely to have externalized behavioral problems (more anxiety and crying, attitude problems, hesitancy, low self-esteem, depressive features, oppositional behavior, tics, introversion and stereotypical behavior).
The comparison of the behavioral alterations shown by the CBCL to the results from the Bayley Scales and the Denver II administered during the follow-up showed that there is an association between the mental, motor and behavioral impairments indicated by the CBCL. Those results suggest that the altered results on the Denver and Bayley tests observed during the early follow-up might predict a number of behavioral symptoms. The predictive value of these tests has been reported in previous studies by our group (15,16). This finding indicates the importance of training health care personnel to apply those tests as a routine evaluation for children who are at risk of developmental problems.
Our data suggest that even low-risk preterm newborns are at risk for developing disturbances such as mild cognitive deficits and behavioral disorders in early childhood or early school age. This risk might increase under unfavorable socioeconomic conditions. Abnormal results on the Denver and Bayley scales during early follow-up might predict a number of behavioral symptoms, although the use of these tests should be stressed as part of the neuropsychological assessment of this unique population to identify early on the risk of later complications and to enable a specific intervention.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Allen MC. Neurodevelopmental outcomes of preterm infants. Curr Opin Neurol. 2008;21(2):123–8. doi: 10.1097/WCO.0b013e3282f88bb4. [DOI] [PubMed] [Google Scholar]
- 2.Larroque B, Ancel PY, Marret S, Marchand L, André M, Arnauld C, et al. Neurodevelopmental disabilities and special care of 5-year-old children born before 33 weeks of gestation (the EPIPAGE study): a longitudinal cohort study. Lancet. 2008;371(9615):813–20. doi: 10.1016/S0140-6736(08)60380-3. [DOI] [PubMed] [Google Scholar]
- 3.Lundequist A, Böhm B, Smedler AC. Individual neuropsychological profiles at age 51\2 years born preterm in relation to medical risk factors. Child Neuropsychol. 2013;19(3):313–31. doi: 10.1080/09297049.2011.653331. [DOI] [PubMed] [Google Scholar]
- 4.Jongbloed –Pereboom M, Janssen AJ, Steenbergen B, Nijhuis-van der Sander MW. Motor learning and working memory in children born preterm: a systematic review. Neurosci Biobehav Rev. 2012;36(4):1314–30. doi: 10.1016/j.neubiorev.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 5.Scott MN, Taylor HG, Fristad MA, Klein N, Espy KA, Minich N, et al. Berhavior disorders in extremely preterm\extremely low birth weight children in kindergarten. J Dev Behav Pediatr. 2012;33(3):202–13. doi: 10.1097/DBP.0b013e3182475287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aarnoudse-Moens CS, Duivenvoorden HJ, Weisglas –Kuperus N, Van Goudoever JB, Oosterlaa J. The profile of executive function in very preterm children at 4 to 12 years. Dev Med Child Neurol. 2012;54(3):247–53. doi: 10.1111/j.1469-8749.2011.04150.x. [DOI] [PubMed] [Google Scholar]
- 7.Mulder H, Pitchford NJ, Marlow N. Inattentive behavior is associated with poor working memory and slow processing speed in very pre-term children in middle childhood. Br J Educ Psychol. 2011;81(Pt 1):147–60. doi: 10.1348/000709910X505527. [DOI] [PubMed] [Google Scholar]
- 8.Guellec I, Lapillone A, Renolleau S, Charlaluk ML, Roze JC, Marret S, et al. Neurologic outcomes at school age in very preterm infants born with severe or mild growth restriction. 2011;127(4):e883–91. doi: 10.1542/peds.2010-2442. [DOI] [PubMed] [Google Scholar]
- 9.Aarnoudse-Moens CS, Weisglas –Kuperus N, Van Goudoever JB, Oosterlaan J. Meta-analysis of neurobehavioral outcomes in very preterm and\or very low birth weight children. Pediatrics. 2009;124(2):717–28. doi: 10.1542/peds.2008-2816. [DOI] [PubMed] [Google Scholar]
- 10.Pritchard VE, Clark CA, Liberty K, Champion PR, Wilson K, Woodward LJ. Early school-based learning difficulties in children born very preterm. Early Hum Dev. 2009;85(4):215–24. doi: 10.1016/j.earlhumdev.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Woodward LJ, Moor S, Hood KM, Champion PR, Foster-Cohen S, Inder TE, et al. Very preterm children show impairments across multiple neurodevelopmental domains at age 4 years. Arch Dis Child Fetal Neonatal Ed. 2009;94(5):F339–44. doi: 10.1136/adc.2008.146282. [DOI] [PubMed] [Google Scholar]
- 12.Mu SC, Lin CH, Chen YL, Chang CH, Tsou KI. Relationship between perinatal and neonatal indices and intelligence quotient in very low birth weight infants at the age of 6 or 8 years. Pediatr Neonatol. 2008;49(2):13–8. doi: 10.1016/S1875-9572(08)60005-4. [DOI] [PubMed] [Google Scholar]
- 13.Anderson PJ, Doyle LW. Cognitive and educational deficits in children born extremely preterm. Semin Perinatol. 2008;32(1):51–8. doi: 10.1053/j.semperi.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 14.Yu JW, Buka SL, Cormick MC, Fitzmaurice GM, Indurkhya A. Behavioral problems and the effects of early intervention on eight-year-old children with learning disabilities. 2006;10(4):329–38. doi: 10.1007/s10995-005-0066-7. [DOI] [PubMed] [Google Scholar]
- 15.Schirmer CR, Portuguez MW, Nunes M L. Clinical assessment of language development in children at age 3 years that were born preterm. Arq Neuropsiquiatr. 2006;64(4):926–31. doi: 10.1590/s0004-282x2006000600007. [DOI] [PubMed] [Google Scholar]
- 16.Do Espírito Santo JL, Portuguez MW, Nunes ML. Cognitive and behavioral status of low birthweight preterm children raised in a developing country at preschool age. J Pediatr (Rio J) 2009;85(1):35–41. doi: 10.2223/JPED.1859. [DOI] [PubMed] [Google Scholar]
- 17.Nascimento E, Figueiredo VLM. WISC-III and WAIS-III: alterations in the current American original version of the adaptations for use in Brazil. Psicol. Reflex. Crit. 2002;15(3):603–12. [Google Scholar]
- 18.Bordin IAS, Mari JJ, Caeiro MF. Validation of the Brazilian version of the Child Behavior Checklist (CBCL) Rev. ABP-APAL. 1995;17(2):55–66. [Google Scholar]
- 19.Associação Nacional de Empresas de Pesquisa. Critério de classificação econômica Brasil. http://www.abep.org/novo/Content.aspx?ContentID=301 (september 20th, 2012)
- 20.Bhutta AT, Cleves MA, Casey PH. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA. 2002;288(6):728–37. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]
- 21.Fawke J. Neurological outcomes following preterm birth. Semin. Fetal Neonatal Med. 2007;12(5):374–82. doi: 10.1016/j.siny.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Ministério da Saúde. http://portal.saude.gov.br/portal/arquivos/pdf/Manual_Infantil_Fetal.pdf (september 20th, 2012).
- 23.Méio MDBB, Lopes CS, Morsch DS. Prognostic factors for cognitive development of very low birth weight premature children. Rev Saúde Publica. 2003;37(3):311–8. doi: 10.1590/s0034-89102003000300008. [DOI] [PubMed] [Google Scholar]
- 24.Méio MDBB, Lopes CS, Morsch DS, Monteiro APG, Rocha SB, Borges RA, et al. Desenvolvimento cognitivo de crianças prematuras de muito baixo peso na idade pré-escolar. J Pediatr (Rio J) 2004;80(6):495–502. [PubMed] [Google Scholar]
- 25.Rodrigues MCC, Mello RR, Fonseca SC. Learning difficulties in schoolchildren born with very low birth weight. J. Pediatr (Rio J.) 2006;82(1):6–14. doi: 10.2223/JPED.1429. [DOI] [PubMed] [Google Scholar]
- 26.Mello RR, Silva KS, Rodrigues MCC, Chalfun G, Ferreira RC, Delamonica JVR. Predictive factors for neuromotor abnormalities at the corrected age of 12 months in very low birth weight premature infants. 2009;67(2A):235–41. doi: 10.1590/s0004-282x2009000200012. [DOI] [PubMed] [Google Scholar]
- 27.Oliveira GE, Magalhães LC, Salmela LFT. Relationship between very low birth weight, environmental factors, and motor and cognitive development of children of 5 and 6 years old. Rev Bras Fisioter. 2011;15(2):138–45. doi: 10.1590/s1413-35552011000200009. [DOI] [PubMed] [Google Scholar]
- 28.Vieira ME, Linhares MB. Developmental outcomes and quality of life in children born preterm at preschool- and school-age. J Pediatr (Rio J) 2011;87(4):281–91. doi: 10.2223/JPED.2096. [DOI] [PubMed] [Google Scholar]
- 29.Procianoy RS, Koch MS, Silveira RC. Neurodevelopmental outcome of appropriate and small for gestational age very low birth weight infants. 2009;24(7):788–94. doi: 10.1177/0883073808331087. [DOI] [PubMed] [Google Scholar]
- 30.Eickman SH, Lira PIC, Lima MC. Desenvolvimento mental e motor aos 24 meses de crianças nascidas a termo com baixo peso. Arq Neuropsiquiatr. 2002;60(3-B):748–54. [PubMed] [Google Scholar]
- 31.Emond AM, Lira PIC, Lima MC, Grantahm- Mc Gregor SM, Ashworth A. Development and behavior of low- birthweight term infants at 8 years in northeast Brazil: a longitudinal study. Acta Paediatr. 2006;95(10):1249–57. doi: 10.1080/08035250600615127. [DOI] [PubMed] [Google Scholar]
- 32.Golden CJ. Clinical interpretation of objective psychological tests 2 ed. Massachusetts, USA: Allyn and Bacon; 1990. [Google Scholar]
- 33.Beaino G, Khoshnood B, Kaminski M, Marret S, Pierrat V, Vieux R, et al. EPIPAGE Study Group. Predictors of the risk of cognitive deficiency in very preterm infants: the EPIPAGE prospective cohort. Acta Paediatr. 2011;100(3):370–8. doi: 10.1111/j.1651-2227.2010.02064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ford RM, Neulinger K, O' Callaghan M, Mohay H, Gary P, Shum D. Executive function in 7-9 –year-old children born extremely preterm or with extremely low birth weight: effects of biomedical history, age at assessment and socioeconomic status. Arch Clin Neuropsychol. 2011;26(7):632–44. doi: 10.1093/arclin/acr061. [DOI] [PubMed] [Google Scholar]
- 35.Lind A, Korkman M, Lehtonen L, Lapinleimu H, Parkkola R, Matomäki J, et al. Cognitive and neuropsychological outcomes at 5 years of age in preterm children born in the 2000s. Dev Med Child Neurol. 2011;53(3):256–62. doi: 10.1111/j.1469-8749.2010.03828.x. [DOI] [PubMed] [Google Scholar]
- 36.Narberhaus A, Pueyo-Benito R, Segarra-Castells MD, Perapoch-López J, Botet-Mussons F, Junqué C. Long-term cognitive dysfunctions related to prematurity. Rev Neurol. 2007;45(4):224–8. [PubMed] [Google Scholar]
- 37.Bradley RH, Corwyn RF. Socioeconomic status and child development. Annual Rev Psychology. 2002;53:317–99. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- 38.Taylor HG, Klein N, Anselmo MG, Minich N, Espy KA, Hack M. Learning problems among kindergarten students with extremely preterm birth. Arch Pediatr Adolesc Med. 2011;165(9):819–25. doi: 10.1001/archpediatrics.2011.137. [DOI] [PMC free article] [PubMed] [Google Scholar]