Abstract
Background:
Routine use of gloves, masks and spectacles are important in infection control. Aim of this study was to assess the knowledge and attitudes of infection control measures among the patients attending clinics of Riyadh Colleges of Dentistry and Pharmacy (RCsDP) in Saudi Arabia.
Material and Methods:
It was a cross-sectional descriptive study of a convenient sample of dental patients attending dental clinics of RCsDP. A structured, close ended, self-administered questionnaire was distributed to 350 patients and a response rate of 86% was obtained. Questionnaireconsisted of series of queries related to knowledge and attitudes of patients towards infection control measures. Data analysis included frequency distribution tables, Mann-Whitney and Kruskal-Wallis tests. Level of significance was set at P < 0.05.
Results:
Final study sample included 301 patients (147 males and 154 females). Almost 99%, 93.7% and 82.7% of the patients agreed that dentist should wear gloves, face mask and spectacles while providing treatment. However, 60.1%, 30% of the patients said that HIV and hepatitis-B infections can spread in dental clinics. Half of the patients felt that they were likely to contract AIDS and 77.7% refused to attend clinics if they knew that AIDS and Hepatitis-B patients treated there. Only 25.2% said that autoclave is the best method of sterilization. A significantly higher knowledge of infection control was observed among the previous dental visitors compared to the first time visitors to the dental clinics (P < 0.05).
Conclusions:
Patients revealed adequate knowledge towards the use of gloves, face mask and spectacles by dentist. However, their knowledge regarding the spread of Hepatitis-B, HIV infection and use of autoclave was poor. Previous visitor of dental clinics showed higher knowledge of infection control as compared to the first time visitors. Many patients expressed their negative attitudes towards dental care due to AIDS and Hepatitis-B concerns.
Keywords: Attitude, dental patients, infection control measures, knowledge
INTRODUCTION
Individuals seeking dental care may be healthy or suffering from various infectious diseases or may be carriers of infectious diseases that cannot be easily identified. There is enough evidence to suggest that many infected patients are unaware of their status because of long incubation periods and post-infection window period during which antibodies cannot be detected.[1] Moreover, such patients may act as a source for spreading infection among dental health care workers and other patients in dental clinics.
Cross infection can be defined as the transmission of infectious agents between patients and staff within a clinical environment. The infective agent can be transmitted through blood, droplets of saliva and contaminated instruments by way of direct contact, inhalation or inoculation. The major route of cross infection in dental surgery is via infection through intact skin or mucosa due to accidents involving sharps or direct inoculation onto cuts and abrasions in the skin.[2,3]
The average overall prevalence of HBsAg in Saudi Arabia is estimated to be 8.3%[4] and the total number of HIV-positive Saudis on early 2010 was reported to be 4,019 persons.[5] With the presence of people infected with hepatitis B and the HIV viruses, cross infection has become a major concern to the dental health care workers and the patient. The increasing incidence of infections with human immunodeficiency virus (HIV) and hepatitis B virus (HBV) with their associated morbidity and mortality has led to a worldwide increased awareness of the risks of infection between patients, dentists and their staff.[6]
Dental treatment procedures frequently cause bleeding and exposure to infected blood, saliva and aerosol which are known means of infectious disease transmission. Routine use of barrier techniques such as gloves, masks, spectacles has been reported to be important in preventing the three routes of transmission (dentist to patient, patient to dentist, patient to patient) in dental clinic.[7]
Dilemma remains to be answered whether particular groups differ in their knowledge and attitude of infection control in dentistry; whether there is any difference in knowledge of infection control measures between previous and first time dental attenders; and whether some patients avoided or delayed seeking care because of such concerns. This study intended to clarify these issues and provide data on knowledge and attitudes of infection control measures among the dental patients. The aim of present study was to assess the knowledge and attitudes of infection control measures among the patients attending dental clinics of Riyadh Colleges of Dentistry and Pharmacy (RCsDP), Riyadh Saudi Arabia.
MATERIALS AND METHODS
Ethical review committee of the RCsDP formally approved the study. A Convenience sampling methodology was employed to select the patients seeking dental care in different clinics (An-Namuthajiya, Al-Munasiya and Al-Olaya) of RCsDP. Only those patients aged 17 years and above who could able to read and comprehend the Arabic language were considered in the study.
Questionnaire design
A self-administered, close ended questionnaire was prepared in Arabic language and the content authenticity was pretested on a sample of dental patients attending RCsDP to ascertain practicability, cogency and rendition of responses. After modification of few questions a final version of questionnaire was prepared and distributed among the 350 patients. Patients were interviewed at main waiting area of clinics of RCsDP (An-Namuthajiya, Al-Munasiya and Al-Olaya). Three hundred one patients responded positively by returning the filled questionnaire and a response rate of 86% was obtained. Each patient took 5 min to complete the questionnaire.
The questionnaire consisted of three parts, first part included socio-demographic data (age, gender, income, occupation, education and visit to the dentist). Second part included fifteen questions to assess the knowledge about the infection spread and control methods in dental operatory. Third part had five questions to assess the perceived attitudes of patients towards infection control measures. The knowledge responses (Yes, No and Do not know) and attitude responses (Strongly agree, Disagree and Strongly disagree) obtained from the questionnaires were coded and entered into the SPSS software package version 19. Frequency distribution tables were obtained for demographic data, knowledge and attitude responses. Mann-Whitney tests were performed to compare the mean ranks of knowledge and attitudes between different genders, education, visit to dental clinics and occupational groups. Kruskal-Wallis tests were performed to compare the mean ranks of knowledge and attitudes among different age groups and household income of the patients. Level of significance was set at P < 0.05.
RESULTS
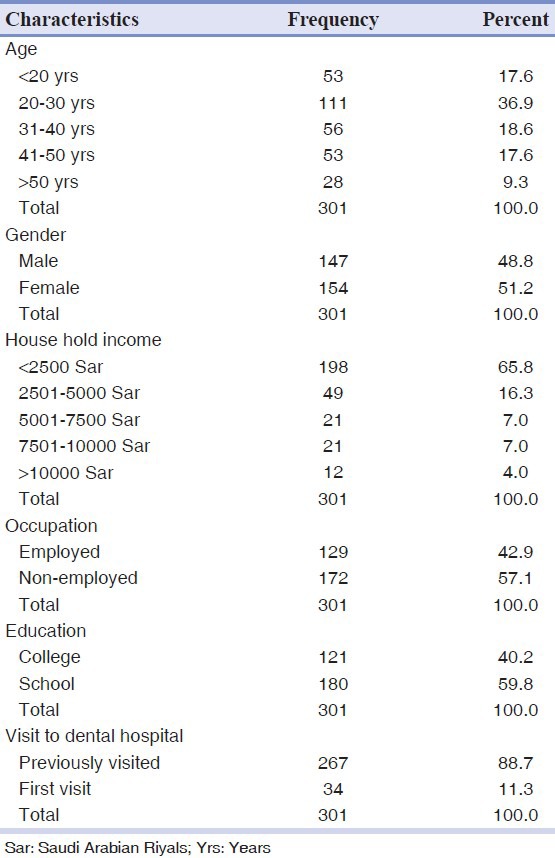
Table 1 shows the distribution of study subjects. Most of the patients were belonged to the 20-30 years and less than 2,500 Sar monthly income. More than half of the patients were employed.
Table 1.
Distribution of study subjects
In the present study more than 80% of the study subjects were knowledgeable about the meaning of infection, spread of infection through contaminated and unsterilized instruments, dentist using barrier methods (wearing gloves, mouth mask, spectacles and gowns) to prevent spread of infection, wearing gloves provide protection to dentist and patients, use of new gloves for every new patient.
Fifty to eighty percent of the patients know about the spread of infection in dental hospital through blood and saliva and dentist acquiring infection from patient and vice versa during dental treatment. Almost 60.1% agreed that AIDS can spread in dental clinic during treatment of affected person and 30% of the patients know about the hepatitis B spread in dental clinic. Only 25.2% know that autoclave is the best method of sterilizing dental instruments.
More than 92% of the study subjects would like their dentist to wear gloves, face mask and spectacle while providing dental treatment. Seventy two percentage of respondents felt that dentist should change the gloves after every patient. Seventy four percentages refused to undergo dental treatment if dentist does not use barrier methods of infection control.
More than 47% of the subjects felt that they were likely to contract AIDS from dentist suffering with AIDS during treatment. Nearly 77.7% said that they will refuse to attend dental clinics if they knew that the AIDS and hepatitis B patients being treated here.
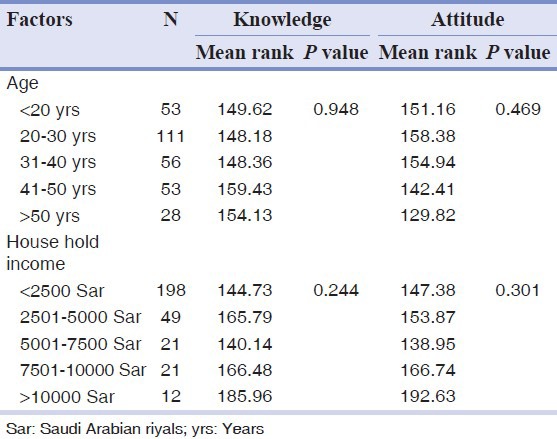
Study subjects who visited dental clinic previously showed higher mean ranks for knowledge as compared to the first time visitors and the difference was statistically significant (P < 0.05) [Table 2]. Age, gender, education, occupation and house-hold income did not show any significance towards knowledge and attitude of infection control measures [Tables 2 and 3].
Table 2.
Comparison of infection control knowledge and attitude among study subjects by Mann-Whitney test
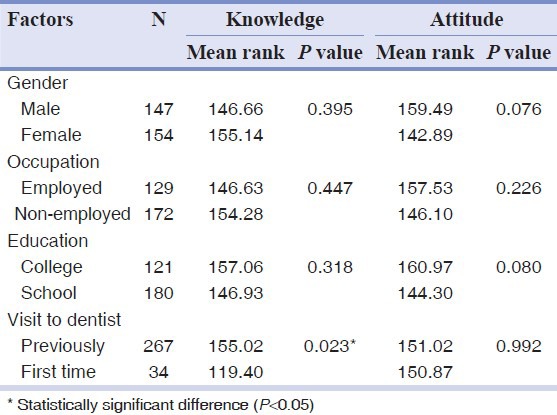
Table 3.
Comparison of infection control knowledge and attitude among the study subjects by Kruskal-Wallis test
DISCUSSION
This survey evaluated the knowledge and attitudes of dental patients towards infection control measures in dental clinics of a private dental college (RCsDP) in Saudi Arabia. Not all infection control procedures were investigated because of concerns that a larger number of items would reduce the response rate. Also, there is evidence that self-reports may overestimate compliance with recommended infection control procedures. The results presented indicate the opinions of Saudi dental patients attending clinics RCsDP in Riyadh. Whether such opinions would be widely held on a nationwide basis remains to be determined by conducting similar surveys in government and other newer private dental schools of Saudi Arabia. Our study revealed an overall adequate knowledge and attitudes of dental patients towards infection control measures.
Dentists, dental assistants and patients may be exposed to pathogenic microorganisms localized in oral cavity and respiratory tract including cytomegalovirus CMV, HBV, HCV, herpes simplex virus HSV type 1 and 2, HIV, Mycobacterium tuberculosis, staphylococci, streptococci and other viruses and bacteria.[8,9] These microorganisms could be transmitted to the dental health care professionals by direct contact with a patient's saliva, blood, skin and oral secretions or by indirect contact through injuries caused by sharp contaminated instruments or by droplet infection from aerosols or splatters.[3]
However, the individual responses to the use of barrier methods of infection control varied amongst different studies as compared to the present study. The wearing of gloves by dentists undertaking clinical procedures has been recommended as an essential element of dental surgery infection control.[10] The reason behind this is to prevent transmission of infection from the operator's hands to the patients and to prevent contact of blood and saliva to the operator's hands. In the present study, 98.7% of respondents knew that the dentist should wear protective gloves. This result was higher than the previously reported studies by Yorden KS[10] 87%, Burke, et al.,[6] 84%, Gerbert, et al.,[11] 76%, Bowden, et al.,[12] 70%, Samranayake and McDonald[13] 60%, Mousa, et al.,[7] 90%, Azodo, et al.,[14] 98.3%, Otuyemi, et al.,[15] 88.8% and Sofola[9] 98.6%.
When enquired about the protection provided by wearing of the gloves, 91% of study subjects said that gloves protect both dentist and the patient from transfer of infection. This result was lower, than reported by Azodo, et al.[14] 94.3%, and higher than reported by Otuyemi, et al.[15] 63%. Most patients in a study conducted by Mousa, et al. believed that gloves were for the patient's protection.[7]
Center for disease control recommended that a separate pair of gloves must be used for each patient to avoid contamination.[16] In the present study, more than 95% of the study subjects know that dentist should wear new gloves for each patient while providing care. Eighty one point three percentage felt that gloves should be changed after every patient in a study conducted by Otuyemi, et al. among university dental patients.[15]
The use of high speed air-driven dental hand pieces and ultrasonic scalers produce large amounts of aerosol and splatter in dentistry. Such aerosol can contain pathogenic disease causing organisms ranging from influenza, tuberculosis to severe acute respiratory distress.[17,18,19] Use of face masks in dentistry has been advocated to protect clinicians from inhaling aerosols. In the present study, 93.7% of study subjects were knowledgeable about the wearing of face masks by dentist while providing care. This response was higher than that reported by Porter, et al.[20] 73%, Bowden, et al.[12] 56% and Mousa, et al. 73%.[7]
Eighty two point seven percentages of respondents expected the dentist to wear protective spectacles routinely. This result is higher to that reported by Porter, et al. 37% for Hong Kong patients and 44% for British patients.[20] This response may reflect patients’ knowledge about the risk of infection transmission from dentist to patient via lachrymal secretions and awareness of the potential spread of infection via debris from the patients mouth to the eyes of dental staff and vice versa.
The rate of annual incidence of HIV-infection in Saudis was ranging 229-505 cases per year during 2001-2009. Between 2001 and 2009 the mean annual incidence of HIV-infection in Saudis was 342 cases per year. The total number of HIV-positive Saudis on early 2010 was reported to be 4,019 persons[5] similarly the average overall prevalence of HBsAg in Saudi Arabia is estimated to be 8.3%, a figure that ranks this country amongst the highly endemic areas of HBV infection in the world.[4] With such incidence of HIV and hepatitis B, dental health care workers are known to be at increased risk of hepatitis and human immunodeficiency virus (HIV) infections. The knowledge of spread of HIV and hepatitis B infection during dental treatment was known to 60.1% and 30% subjects, respectively.
Sterilization and disinfection of instrument is of utmost significance in dental offices as it assists in preventing the transmission of infection from patient to patient and from instrument to patient. One third of the total populations were ignorant about sterilization methods used in dentistry.[13] In the present study, lower than 26% of the respondents said that autoclaving of the instrument is the best method of sterilization of instruments, this response is lower as compared to the 43.7% reported by Azodo, et al.[14]
The responses to the attitudinal questions varied among the study subjects 92.7% would like their dentist to wear gloves and face mask while providing dental care for them and only less than 17% expressed that they would like to attend dentist who is not going to use gloves, face and spectacles while providing dental care. Seventy one point eight percentages would like their dentist to wear new gloves for every patient. Less than 48% of the study subjects felt that they are likely to get AIDS if dentist treating suffers with AIDS. However, 77.7% respondents would not like to attend the dental hospital if they come to know that AIDS and hepatitis B patient being treated here. Sofola, et al. reported that, 54% study subjects felt that they could contact an infection in the dental clinic and 43% of them identified HIV as a risk and 61.4% would not attend a clinic if they knew that HIV patients were treated there.[9] Similarly, Mousa, et al. reported that just over 50% of patients believed that they could contact HIV from an HIV-infected dentist.[7] Two third of the respondents believed that transmission of AIDS in the dental clinic is unlikely, one half of the general practice patients were unwilling to visit the dentist if the later was known to treat patients with AIDS.[13]
Knowledge of cross infection control measures was higher among the patients who have visited the dental clinic previously as compared to the first time visitors. This may be due to their familiarity and first hand experiences to infection control procedures employed by the dentist while providing care. Previous studies reported that the age[15] gender[9] educational attainment[7,9] geographic location[7] language and dental visiting pattern[21] were the factors affected knowledge and attitude of dental patients towards infection control measures in dentistry. However, except for visit to dentist no other factors showed significant difference in the present study.
CONCLUSIONS
Patients attending dental clinics of RCsDP have adequate knowledge of wearing gloves, face mask and spectacles by dentist during the dental treatment to control infection. However, their knowledge regarding the spread of hepatitis B, HIV infection in dental clinics and use of autoclave for sterilizing dental instrument was poor. Dental patients who visited dental clinics previously showed higher knowledge of infection control measures as compared to the first time visitors.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Samaranayake L. Rules of infection control. Int Dent J. 1993;43:578–84. [PubMed] [Google Scholar]
- 2.Girdler NM, Matthews RW, Scully C. Use and acceptability of rubber gloves for outpatient dental treatment. J Dent. 1987;15:209–12. doi: 10.1016/0300-5712(87)90111-4. [DOI] [PubMed] [Google Scholar]
- 3.Verrusio AC, Neidle EA, Nash KD, Silverman S, Jr, Horowitz AM, Wagner KS. The dentist and infectious diseases: A national survey of attitudes and behavior. J Am Dent Assoc. 1989;118:553–62. doi: 10.14219/jada.archive.1989.0082. [DOI] [PubMed] [Google Scholar]
- 4.Paul T, Maktabi A, Almas K, Saeed S. Hepatitis-B awareness and attitudes amongst dental health care workers in Riyadh, Saudi Arabia. Odontostomatol Trop. 1999;86:9–12. [PubMed] [Google Scholar]
- 5.Alothman AF, Muhajer K, Balkhy H. Prevalence of HIV-infection in Saudi Arabia. BMC Proceedings. 2011;5:252. [Google Scholar]
- 6.Burke FJ. Use of non-sterile gloves in clinical practice. J Dent. 1990;18:79–89. doi: 10.1016/0300-5712(90)90089-w. [DOI] [PubMed] [Google Scholar]
- 7.Adel AM, Nadia MM, Azza MT. Knowledge and attitudes of dental patients towards cross-infection control measures in dental practice. East Mediterr Health J. 1997;3:263–73. [Google Scholar]
- 8.Hospital Infection Control Practices Advisory Committee. Guideline for infection control in health care personnel. Am J Infect Control. 1998;26:289–354. [Google Scholar]
- 9.Sofola OO, Uti OG, Onigbinde OO. Public perception of cross-infection control in dentistry in Nigeria. Int Dent J. 2005;55:383–7. doi: 10.1111/j.1875-595x.2005.tb00051.x. [DOI] [PubMed] [Google Scholar]
- 10.Yorden KS. Patients’ attitudes towards the routine use of rubber gloves in a dental office. J Indiana Dent Assoc. 1985;64:25–8. [PubMed] [Google Scholar]
- 11.Gerbert B, Maguire BT, Spitzer S. Patients› attitudes toward dentistry and AIDS. J Am Dent Assoc. 1989:16S–21. doi: 10.14219/jada.archive.1989.0278. [DOI] [PubMed] [Google Scholar]
- 12.Bowden JR, Scully C, Bell CJ, Levers H. Cross infection control, attitudes of patients toward wearing of gloves and masks by the dentist in the United Kingdom in 1987. Oral Surg Oral Pathol Oral Med. 1989;67:45–8. doi: 10.1016/0030-4220(89)90301-0. [DOI] [PubMed] [Google Scholar]
- 13.Samaranayake LP, McDonald KC. Patient perception of cross infection prevention in dentistry. Oral Surg Oral Med Oral Pathol. 1990;69:457–60. doi: 10.1016/0030-4220(90)90379-7. [DOI] [PubMed] [Google Scholar]
- 14.Azodo CC, Umoh A, Ehizele Nigerian patients’ perception of infection control measures in dentistry. Int J Biomed Hlth Sci. 2010;6:173–9. [Google Scholar]
- 15.Otuyemi OD, Oginni AO, Ogunbodede EO, Oginni FO, Olusile AO. Patients’ attitudes to wearing of gloves by dentists in Nigeria. East East African Med J. 2001;78:220–2. doi: 10.4314/eamj.v78i4.9068. [DOI] [PubMed] [Google Scholar]
- 16.Harte JA. Standard and Transmission-based Precautions: An update for Dentistry. J Am Dent Assoc. 2010;141:572–81. doi: 10.14219/jada.archive.2010.0232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holbrook WP, Muir KF, Macphee IT, Ross PW. Bacteriological investigation of the aerosol from ultrasonic scalers. Br Dent J. 1978;144:245–7. doi: 10.1038/sj.bdj.4804072. [DOI] [PubMed] [Google Scholar]
- 18.Micik RE, Miller RL, Mazzerella MA, Ryge G. Studies on dental aerobiology I: Bacterial aerosols generated during dental procedures. J Dent Res. 1969;48:49–56. doi: 10.1177/00220345690480012401. [DOI] [PubMed] [Google Scholar]
- 19.Miller RL, Micik RE, Abel C, Ryge G. Studies of dental aerobiology, II: Microbial splatter discharged from the oral cavity of dental patients. J Dent Res. 1971;50:621–5. doi: 10.1177/00220345710500031701. [DOI] [PubMed] [Google Scholar]
- 20.Porter SR, Peake G, Scully C, Samaranayake LP. Attitude to cross infection measures of UK and Hong Kong patients. Br Dent J. 1993;175:245–57. doi: 10.1038/sj.bdj.4808292. [DOI] [PubMed] [Google Scholar]
- 21.Thompson MW, Stewart JF, Carter KD, Spencer AJ. Public perception of cross infection control in dentistry. Aust Dent J. 1997;42:291–6. doi: 10.1111/j.1834-7819.1997.tb00132.x. [DOI] [PubMed] [Google Scholar]


