Abstract
Providing an esthetic restoration in the anterior region of the mouth has been the basis of peri-implant esthetics. To achieve optimal esthetics, in implant supported restorations, various patient and tooth related factors have to be taken into consideration. Peri-implant plastic surgery has been adopted to improve the soft tissue and hard tissue profiles, during and after implant placement. The various factors and the procedures related to enhancement of peri-implant esthetics have been discussed in this review article.
Keywords: Dental esthetics, dental implant, gingiva/surgery
INTRODUCTION
Esthetics signifies “natural beauty”, a quality that comes from within. It can be defined as the science of beauty that is applied in nature and in art. Ever since implants have been used as a treatment option for replacement of missing natural teeth, its results have found to be successful both in term of stability and esthetic outcomes. However, when tooth loss is accompanied by soft tissue and bone loss, it often requires augmentation of the peri-implant soft tissue or bony site either before or after the placement of the implant. This forms the crux of peri-implant plastic surgery. Peri-implant plastic surgery focuses on harmonizing peri-implant structures by means of hard tissue engineering and soft tissue engineering.
IDEAL REQUIREMENTS FOR ESTHETIC TREATMENT OUTCOME
An esthetic implant restoration is one that resembles a natural tooth in all respects.[1] Both dental and gingival esthetics act together to provide a harmonious smile. The clinician must be aware of the parameters related to gingival morphology, form, dimension, characterization, surface texture and color. The predictability of an esthetic outcome for an implant restoration is dependent on many variables including but not limited to the following:
Patient's smile line
In an average smile, 75-100% of the maxillary incisors and the interproximal gingiva are displayed. A high smile line poses considerable challenges when planning for implant supported restorations in the esthetic zone because the restoration and gingival tissues are completely displayed. The low smile line is a less critical situation because the implant restoration interface will be hidden behind the upper lip.[2]
Tooth position
The tooth needs to be evaluated in three planes of space before it is extracted: Apico coronal, faciolingual and mesiodistal. If there is a tooth with hopeless prognosis positioned ideally or apically and this is extracted, the gingival margin is likely to migrate apically.[3] A tooth positioned too far facially, often results in very thin or non-existent labial bone. A tooth positioned more lingually would benefit from the presence of an increased amount of facial bone.
Root position of the adjacent teeth
Teeth with root proximity also possess very little interproximal bone; this thin bone creates a greater risk of lateral resorption which will decrease the vertical bone height after extraction or implant placement.[4]
Biotype of the periodontium and tooth shape
Two different periodontal biotypes have been described in relation to the morphology of the interdental papilla and the osseous architecture: The thin scalloped periodontium and the thick flat periodontium.[5] A thick soft tissue biotype is a desirable characteristic that will positively affect the esthetic outcome of an implant – supported restoration because since it is more resistant to mechanical and surgical insults, it is less susceptible to mucosal recession and has more volume for prosthetic manipulation.
The tooth morphology also appears to be correlated with the soft tissue quality.[6] The triangular tooth shape is associated with the scalloped and thin periodontium. The contact area is located in the coronal third of the crown underlining a long and thin papilla. The square anatomic crown shape combines with a thick and flat periodontium. The contact area is located at the middle third supporting a short and wide papilla. Loss of interproximal tissue in the presence of a triangular tooth form will display a wider black triangle than in a situation when a square tooth is present.
The bone anatomy at the implant site
For successful esthetic restoration of implants, the bony housing must have a three dimensional configuration that permits placement of an implant in a restoratively ideal position. Two anatomic structures are important in determining predictability of soft tissues after implant placement. The first is the height and thickness of the facial bony wall and the second is the bone height of the alveolar crest in the interproximal areas.[7]
Height and thickness of facial bony wall
Kois et al.,[8] in a survey of 100 patients, classified patients as having high, normal or low crests. This was based on the vertical distance of the osseous crest to the free gingival margin. The greater the distance from the osseous crest to the free gingival margin the greater the risk of tissue loss after an invasive procedure. If the total vertical distance of the total dentogingival complex on the mid facial aspect is 3 mm, a slight apical loss of tissue up to 1 mm is anticipated after extraction and immediate implant placement.[8]
Height of bony crest in the interproximal area
The interproximal bony crest plays a critical role in the presence or absence of peri-implant papillae. When the contact point to the bone was 3-5 mm, papilla always filled the space. When the distance was 6 mm papilla was absent 45% of the time and with a distance of 7 mm, papilla did not fill the space 75% of the time. A difference of 1-2 mm is significant in obtaining soft tissue esthetics.[9]
Optimal implant positioning
The position, in which the implant is placed, is of utmost importance and the implant should be thought of as an extension of the clinical crown into the alveolar bone. When planning for an ideal three - dimensional implant position, it should be made sure that they are placed in the “comfort” zone. Comfort zones are defined in mesiodistal, faciolingual and apico coronal dimensions.[10]
Mesiodistally, it is recommended that an implant shoulder be placed at least 1 mm from an adjacent tooth. Faciolingually, it's been proposed that the implant shoulder margin should be at the ideal point of emergence i.e., 1 mm palatal to the point of emergence at adjacent teeth. The apico coronal location of the implant shoulder is dependent on a number of factors: 1. The cervical bone resorption morphology, 2. The diameter of the implant, 3. The size discrepancy between the root, 4. The diameter of the implant, 5. The thickness of the marginal gingiva and the proximal tissues. It is suggested that the implant collar be located 2 mm apical to the CEJ of the adjacent tooth if no gingival recession is present and 3 mm from the free gingival margin when it is.[11] Apico coronally, the position of the implant should be approximately 2 mm apical to the mid facial margin of the planned restoration.[12]
SITE EVALUATION
Before planning an implant therapy in an individual, a thorough knowledge about the health and bone morphology of the area is to be considered. Treatment planning must also address hard and soft tissue deficiencies in combination with precision in implant placement. In order to correct the soft and hard tissue deficiencies, understanding of the amount of loss of tissue is necessary and several classifications have been put forward by several authors.
Classification of tissue volume
The first classification of ridge deficiency was proposed by Seibert[13] in 1983 and later modified by Allen[14] in 1985.
Seibert[13] divided ridge deficiencies into three classes, with a Class I defect describing the apico coronal loss of ridge contour, Class II, buccolingual, and Class III, a combined loss of both apico coronal and bucco-lingual dimensions.
Allen[14] further quantified the loss of ridge dimension into mild (3 mm), moderate (3-6 mm) and severe (6 mm).
The Palacci-Ericsson[15] classification system divides implant sites into four classes according to the vertical and horizontal dimensions of tissue loss, respectively.
Vertical loss
Class I: Intact or slightly reduced papillae;
Class II: Limited loss of papillae (less than 50%);
Class III: Severe loss of papillae; and
Class IV: Absence of papillae (edentulous ridge).
Horizontal loss
Class A: Intact or slightly reduced buccal tissues;
Class B: Limited loss of buccal tissues;
Class C: Severe loss of buccal tissues; and
Class D: Extreme loss of buccal tissue, often with a limited amount of attached mucosa.
Classification of bone volume
Lekholm and Zarb[16] described the shape of the residual edentulous ridge in terms of remaining bone volume, with a 5-point classification system from A (intact ridge form) to E (severely deficient ridge form).
This classification lacks specific categorical ridge dimensions and has less detail within categories addressing vertical or horizontal ridge deficiency.
Misch and Judy[17] classified available bone into 4 divisions: abundant, barely sufficient, compromised, and deficient (A-D). Abundant bone is bone volume is greater than 5 mm in width, 10 to 13 mm in height, and 7 mm in length. Barely sufficient bone is 2.5 to 5 mm in width, greater than 10 to 13 mm in height, and greater than 12 mm in length. Compromised bone is less than 10 mm in height, or width (less than 2.5 mm). Deficient bone is generally not amenable to implant rehabilitation.
ESTHETIC ASSESSMENT
The success of a single tooth implant restoration in the esthetic zone depends not only on restored function but also on harmonious integration of the restoration into the patient's overall appearance, especially the peri-implant soft tissue.[18]
To date, no authoritative index has existed for the assessment of peri-implant soft tissue. Belser et al.,[19] indicated that esthetics of peri-implant soft tissues, including health, height, volume, color and contour, must be in harmony with the healthy surrounding dentition. Buser et al.,[20] indicated that patient satisfaction is a key factor in the success of implant therapy, especially in the anterior area.
Furhauser et al.,[21] introduced an index termed the pink esthetic score (PES) to rate the appearance of the soft tissue in anterior implant restorations. They identified seven distinct soft tissue parameters: 1. The presence or absence of mesial papillae, 2. The presence or absence of distal papillae, 3. The level of emergence of the implant restoration from the mucosa at the facial aspect, 4. Curvature of the line of emergence of the implant restoration from the mucosa at the facial aspect, 5. Facial soft tissue convexity, 6. Color and 7. Texture of the facial marginal peri-implant mucosa. Each of these parameters was rated 2, 1 or 0 with the maximum possible score of 14, indicating the most esthetic result. The PES allows for more objective appraisal of the short and long term esthetic results of various surgical and prosthetic implant procedures.
MANAGEMENT OF PERI-IMPLANT ESTHETICS
Peri-implant plastic surgery
A large number of soft and hard tissue procedures have been described to facilitate edentulous ridge augmentation prior to implant placement. A straightforward implant placement can be performed without any additional surgeries; however, at the time of implant placement, minor hard tissue augmentation may be needed to add support to the peri-implant mucosa. In other situations, soft tissue must be added to enhance the final result and thus facilitate soft tissue handling at second stage surgery.
Surgical considerations
Planning and execution
Implant therapy in the anterior maxilla is considered an advanced or complex procedure and requires comprehensive preoperative planning and precise surgical execution based on a restoration driven approach.[19]
Patient selection
It is essential in achieving esthetic treatment outcomes. During treatment of high risk patients, a general risk assessment (medical status, periodontal susceptibility, smoking and other risks) should be undertaken with caution.[19]
Implant selection
Implant type and size should be based on site anatomy and the planned restoration. Inappropriate choice of implant body and shoulder dimensions may result in hard and/or soft tissue complications such as exposure of metal collar at the implant shoulder junction. To overcome this, the platform switching technique has been developed to preserve or regenerate the inter-implant soft tissue and impede an unsightly metal display. Platform switching can preserve soft and hard tissues and may provide better biological, mechanical, and esthetic outcomes.[22]
Clinical considerations
Single tooth replacement
For anterior single tooth replacement in sites without tissue deficiencies, predictable treatment outcomes, including esthetics, can be achieved because tissue support is provided by adjacent teeth.[19]
Multiple tooth replacement
The replacement of multiple adjacent missing teeth in the anterior maxilla with fixed implant restorations is poorly documented.[19] In this context, esthetic corrections is not predictable particularly regarding the contours of the inter-implant soft tissue.
PRE PLACEMENT PROCEDURES
A large number of soft and hard tissue procedures have been described to facilitate edentulous ridge augmentation prior to implant placement. Soft tissue modification before implant placement is advantageous in that proper tissue contours before first stage surgery, increasing the predictability of a satisfying treatment outcome.[23]
Ridge (socket) preservation
About 3 to 4 mm of resorption can occur during the first 6 months after extraction in the absence of intervention.[24,25] The ideal solution to successful ridge preservation is the flapless, atraumatic removal of the hopeless tooth, leaving much of the bony architecture, including thin buccal cortical plate, intact. After extraction socket is curetted, a decision is made regarding the grafting material from an absorbable collagen matrix, autogenous bone, demineralized freeze-dried bone allograft, combinations of growth factors, to a variety of synthetic grafting materials.[23]
Forced orthodontic eruption
The use of orthodontics in erupting hopeless teeth before extraction has been used successfully to augment bone and soft tissue support at future implant sites.[26]
Controlled tissue expansion
This technique was proposed by Bahat et al,[27] that exploited the elastic properties of the gingival epithelium, the tissue is expanded using an inflatable silicon balloon expander to gain adequate soft tissue for primary coverage of subsequent osseous grafts.
Soft tissue grafting
These procedures have been used successfully for many years in periodontics and oral surgery in resolving recession defects around natural teeth and augmenting alveolar ridge contours.[28,29,30] The following procedures are designed for use in augmentation of edentulous ridge defects: The roll technique, pouch procedures, interpositional grafts, onlay grafts and combination grafts.[31,32,33]
IMPLANT STAGE 1 AND 2 PROCEDURES
Papilla regeneration technique
This technique was developed to correct deficient interproximal papillae contours between multiple implants at stage 2 surgery and is primarily an esthetically driven procedure. The procedure involves elevating a full thickness mucoperiosteal flap at the palatal or lingual extent of the implant cover screws. Vertical releasing incisions are used to aid in flap elevation, and the incisions are made so as to exclude the papillary tissue of adjacent natural teeth. Semilunar, beveled incisions are then created in the buccal flap extending toward each abutment, beginning with the distal aspect of the most mesially located implant. The pedicles are secured between the abutments using tension-free suturing and are allowed to heal for 4 to 6 weeks before final restoration[34] [Figures 1a–c].
Figure 1a.
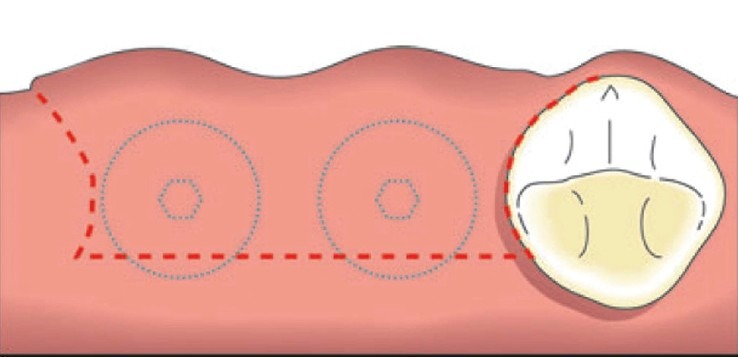
A full-thickness flap is elevated and reflected buccally[34]
Figure 1c.
The pedicles are rotated to fill the inter-abutment and abutment-tooth spaces[34]
Figure 1b.
Semilunar bevel incisions are made, recreating a scalloped shape similar to that of tissues around natural teeth[34]
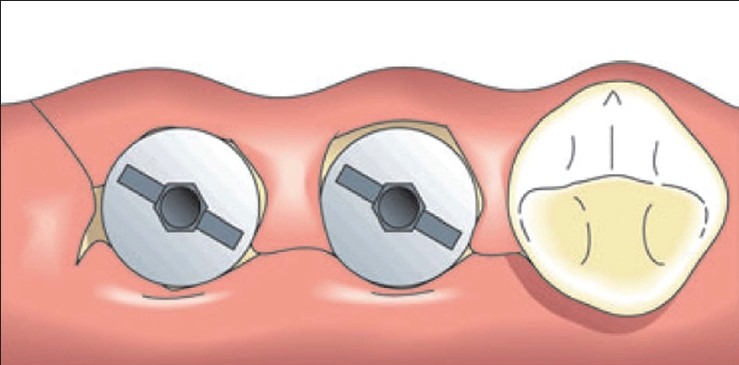
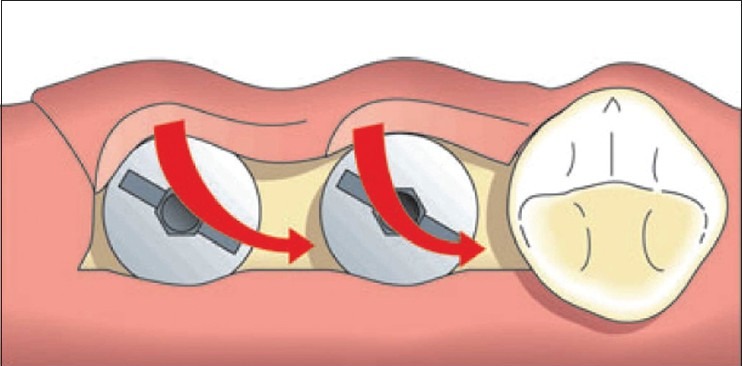
Tissue punch (Flapless) technique[35] and titanium papillary inserts[36] have also been considered during the second stage of implant placement [Figures 2a-d].[37]
Figure 2a.
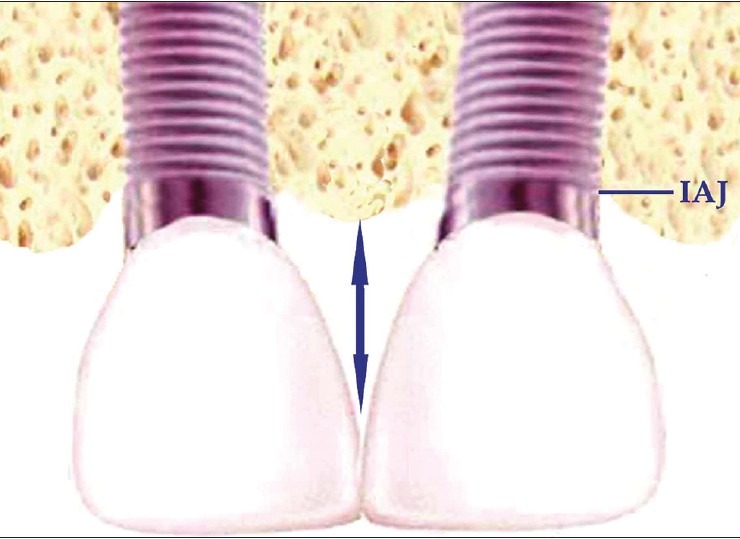
Loss of interproximal bone to the level of the implantabutment junction between two adjacent implants[37]
Figure 2d.
Titanium papillary insert supporting inter-implant papilla around two adjacent implants[37]
Figure 2b.

Loss of papilla between two adjacent implants[37]
Figure 2c.
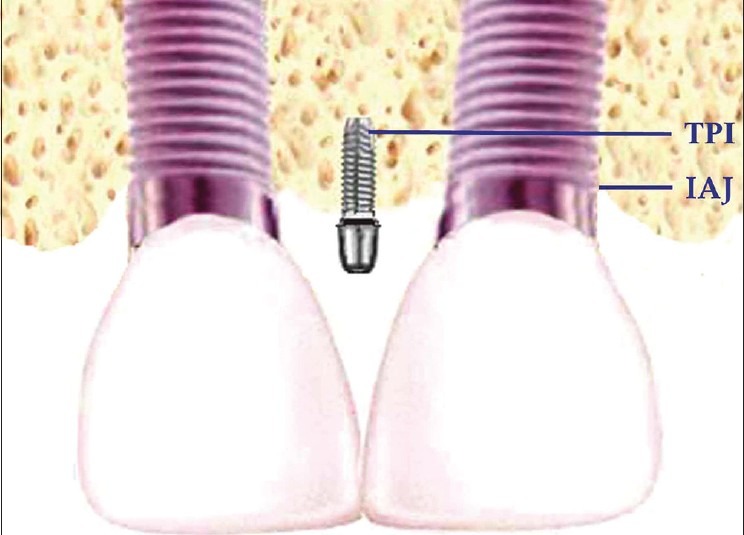
Titanium papillary insert is positioned in the interproximal bone between the adjacent implants[37]
POST PLACEMENT SOFT TISSUE MANAGEMENT
All esthetic tissue management should be completed before seating of the definitive restoration in as much post placement esthetic management is severely limited. Post-placement soft tissue modification in this context therefore, consists primarily of hard tissue regenerative procedures or hard or soft tissue respective procedures in an attempt to restore the health of peri-implant tissues.[38]
Vertical defects
If the extent of bone loss is less than 2 mm, the defect can be grafted with autogenous bone or it can be removed through osteoplasty, converting the defect into a horizontal deficiency.[23]
Horizontal defects
The most predictable method of treating horizontal implant defects is through reduction of the soft tissue thickness via apical repositioning. If the horizontal defect extends beyond one half of the implant body, it should be removed. Regenerative procedures using autogenous bone and a barrier membrane to gain height around the implant fixture is indicated only in single- or multiple-implant fixed restorations or when additional bone-to-implant interface is required to withstand the forces exerted on the prosthesis.[39]
MANAGEMENT TRIAD TO INCREASE SOFT TISSUE THICKNESS
In spite of the available surgical techniques, Fu et al.,[40] proposed a guideline that demonstrates possible ways to increase the soft tissue thickness around implants, i.e. the “PDP management triad”: implant position (P), implant design (D) and prosthetic design (P). First, the implant position, and angulation are key determinants in ensuring that an implant supported restoration has functional and esthetic success through an ideal emergence profile. Second, implant diameter and platform design can help prevent crestal bone resorption, which is a great asset in preserving esthetics. Third, the prosthetic design can provide the additional space for soft tissue in growth to create a fuller soft tissue profile.
Provisional and definitive restorations
To optimize esthetic treatment outcomes, the use of provisional restorations with adequate emergence profiles is recommended to guide and shape the peri-implant tissues prior to definitive restoration. It is preferable to place provisional restorations on the implant at the time the restorative procedure is started.[41,42,43] This process will establish a natural and esthetic soft tissue form that will determine guidelines for laboratory fabrication of an anatomically appropriate soft tissue model [Figures 3 and 4].
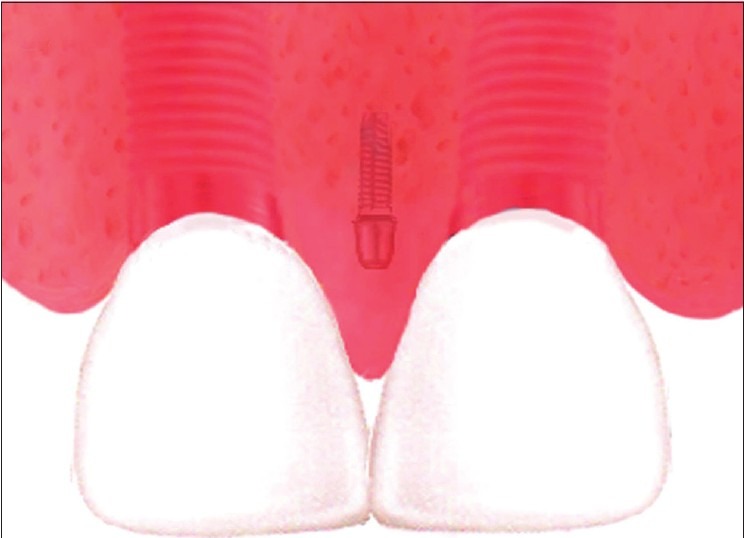
Figure 3.

Unaesthetic appearance due to loss of tooth in the anterior region
Figure 4.

Placement of provisional restoration after implant placement in maxillary left central incisor
CONCLUSION
The implantological rehabilitation of the esthetic zone is one of the most demanding and complex treatments due to the necessity to obtain an optimum esthetic result. From existent evidence concerning soft tissue modification around implants, implant plastic surgery should emerge as a distinct sub-discipline of that will continue to develop and expand as dental implants are accepted as a routine treatment for the restoration of function and esthetics. Though, osseointegration and restoration of function and soft tissue esthetics dictate implant success, the patient's satisfaction is a key element of the success of implant therapy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Higginbottom FL, Wilson TG. Three-dimensional templates for placement of root-form dental implants. Int J Oral Maxillofac Implants. 1996;6:787–95. [PubMed] [Google Scholar]
- 2.Tjan AH, Miller GD. The JG: Some aesthetic factors in a smile. J Prosthet Dent. 1984;51:24–8. doi: 10.1016/s0022-3913(84)80097-9. [DOI] [PubMed] [Google Scholar]
- 3.Kois JC. Aesthetic extraction site development: The biologic variables. Contem Aesthet Resto Pract. 1998;2:10–8. [Google Scholar]
- 4.Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71:546–9. doi: 10.1902/jop.2000.71.4.546. [DOI] [PubMed] [Google Scholar]
- 5.Becker W, Ochsenbein C, Tibbetts L, Becker BE. The alveolar bone anatomic profiles as measured from dry skulls. Clinical ramifications. J Clin Periodontol. 1997;24:727–731. doi: 10.1111/j.1600-051x.1997.tb00189.x. [DOI] [PubMed] [Google Scholar]
- 6.Jivraj S, Chee W. Treatment planning of implants in the aesthetic zone. Br Dent J. 2006;201:13–23. doi: 10.1038/sj.bdj.4813820. [DOI] [PubMed] [Google Scholar]
- 7.D’Addona A, Nowzari H. Intramembranous autogenous osseous transplants in aesthetic treatment of alveolar atrophy. J Periodontol 2000. 2001;(27):148–61. doi: 10.1034/j.1600-0757.2001.027001148.x. [DOI] [PubMed] [Google Scholar]
- 8.Kois JC. Altering gingival levels: The restorative connection part I: Biologic variables. J Esthet Dent. 1994;6:3–9. [Google Scholar]
- 9.Tarnow DP, Magner AW, Fletcher P. The effect of distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:886–995. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]
- 10.Spielman HP. Influence of the implant position on the aesthetics of the restoration. Pract Aesthet Dent. 1996;8:897–904. quiz 906. [PubMed] [Google Scholar]
- 11.Saadoun AP, LeGall M, Touati B. Selection and ideal tridimensional implant position for soft tissue aesthetics. Pract Periodontics Aesthet Dent. 1999;11:1063–72. quiz 1074. [PubMed] [Google Scholar]
- 12.Buser D, von Arx T. Surgical procedures in partially edentulous patients with ITI implants. Clin Oral Implants Res. 2000;11:83–100. doi: 10.1034/j.1600-0501.2000.011s1083.x. [DOI] [PubMed] [Google Scholar]
- 13.Seibert JS. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts. Part II. Prosthetic/periodontal interrelationships. Compend Contin Educ Dent. 1983;4:549–62. [PubMed] [Google Scholar]
- 14.Allen EP, Gainza CS, Farthing GG, Newbold DA. Improved technique for localized ridge augmentation: A report of 21 cases. J Periodontol. 1985;56:195–9. doi: 10.1902/jop.1985.56.4.195. [DOI] [PubMed] [Google Scholar]
- 15.Palacci P, Ericsson I. London: Quintessence Books; 2001. Esthetic implant dentistry soft and hard tissue management. [Google Scholar]
- 16.Lekholm U, Zarb G. Patient selection. In: Branemark PI, Zarb G, Albrektsson T, editors. Tissue Integrated Prostheses. Osseointegration in Clinical Dentistry. Chicago, Ill: Quintessence; 1985. pp. 199–209. [Google Scholar]
- 17.Misch CE, Judy KW. Classification of partially edentulous arches for implant dentistry. Int J Oral Implantol. 1987;4:7–13. [PubMed] [Google Scholar]
- 18.Doring K, Eisenmann E, Stiller M. Functional and esthetic considerations for single tooth Ankylos implant crown: 8 years of clinical performance. J Oral Implantol. 2004;30:198–209. doi: 10.1563/1548-1336(2004)30<198:FAECFS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Belser U, Martin W, Belser UC. Consensus statements and recommended clinical procedures regarding esthetics in implant dentistry. Int J Oral Maxillofac Implants. 2004;19:73–4. [PubMed] [Google Scholar]
- 20.Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19:43–61. [PubMed] [Google Scholar]
- 21.Fürhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G. Evaluation of soft tissue around single-tooth implant crowns: The pink esthetic score. Clin Oral Implants Res. 2005;16:639–44. doi: 10.1111/j.1600-0501.2005.01193.x. [DOI] [PubMed] [Google Scholar]
- 22.Salimi H, Savabi O, Nejatidanesh F. Current results and trends in platform switching. Dent Res J. 2011;8:S30–6. [PMC free article] [PubMed] [Google Scholar]
- 23.Kazor CE, Al-Shammari K, Sarment DP, Misch CE, Wang HL. Implant plastic surgery: A review and rationale. J Oral Implantol. 2004;4:240–54. doi: 10.1563/0.637.1. [DOI] [PubMed] [Google Scholar]
- 24.Juodzbalys G. Socket morphology-based treatment for implant esthetics: A pilot study. Int J Oral Maxillofac Implants. 2010;25:970–8. [PubMed] [Google Scholar]
- 25.Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants. 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990;1:33–40. doi: 10.1034/j.1600-0501.1990.010105.x. [DOI] [PubMed] [Google Scholar]
- 26.Salama H, Salama M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects. Int J Periodontics Restorative Dent. 1993;13:312–33. [PubMed] [Google Scholar]
- 27.Bahat O, Koplin LM. Pantographic lip expansion and bone grafting for ridge augmentation. Int J Periodontics Restorative Dent. 1989;9:344–53. [PubMed] [Google Scholar]
- 28.Guirado JL, Yuguero MR, Zamora G, Barrio E. Immediate provisionalization on a new implant design for esthetic restoration and preserving crestal bone. Implant Dent. 2007;16:155–64. doi: 10.1097/ID.0b013e31805816c9. [DOI] [PubMed] [Google Scholar]
- 29.Guirado JL, Ruiz AJ, Moreno G, Marí L. Immediate loading and immediate restoration in 105 expanded-platform implants via the Diem System after a 16-month follow-up period. Med Oral Patol Oral Cir Bucal. 2008;13:576–81. [PubMed] [Google Scholar]
- 30.Hermann F, Lerner H, Palti A. Factors influencing the preservation of the periimplant marginal bone. Implant Dent. 2007;16:165–75. doi: 10.1097/ID.0b013e318065aa81. [DOI] [PubMed] [Google Scholar]
- 31.Cohen ES. Ridge augmentation utilizing the subepithelial connective tissue graft: Case reports. Pract Perio Aesth Dent. 1994;6:47–53. [PubMed] [Google Scholar]
- 32.Kaldahl WB, Tussing GJ, Wentz FM, Walker JA. Achieving an esthetic appearance with a fixed prosthesis by submucosal grafts. J Am Dent Assoc. 1982;104:449–52. doi: 10.14219/jada.archive.1982.0209. [DOI] [PubMed] [Google Scholar]
- 33.Khoury F, Happe A. The palatal subepithelial connective tissue flap method for soft tissue management to cover maxillary defects: A clinical report. Int J Oral Maxillofac Implants. 2000;15:415–8. [PubMed] [Google Scholar]
- 34.Palacci P, Nowzari H. Soft tissue enhancement around dental implants. Periodontol 2000. 2008;(47):113–32. doi: 10.1111/j.1600-0757.2008.00256.x. [DOI] [PubMed] [Google Scholar]
- 35.Gomez-Roman G, Schulte W, d’Hoedt B, Axman-Krcmar D. The Frialit-2 implant system: Five-year clinical experience in single-tooth and immediately postextraction applications. Int J Oral Maxillofac Implants. 1997;123:299–309. [PubMed] [Google Scholar]
- 36.El Askary AS. Use of a titanium papillary insert for the construction of interimplant papillae. Implant Dent. 2000;9:358–62. doi: 10.1097/00008505-200009040-00013. [DOI] [PubMed] [Google Scholar]
- 37.Pradeep AR, Karthikeyan BV. Peri-implant papilla reconstruction: Realities and limitations. J Periodontol. 2006;77:534–44. doi: 10.1902/jop.2006.050068. [DOI] [PubMed] [Google Scholar]
- 38.Hurzeler MB, Weng D. Peri implant tissue management: optimal timing for an aesthetic result. Pract Periodontics Aesthet Dent. 1996;8:857–869. quiz 869. [PubMed] [Google Scholar]
- 39.Misch CE. Stage II surgery: Uncovery and treatment of healing complications. In: Misch CE, editor. Contemporary Implant Dentistry. 2nd ed. St Louis, Mo: CV Mosby; 1999. pp. 385–95. [Google Scholar]
- 40.Fu J, Lee A, Wang H. Influence of Tissue Biotype on Implant Esthetics. Int J Oral Maxillofac Implants. 2011;26:499–508. [PubMed] [Google Scholar]
- 41.Chee WW. Provisional restorations in soft tissue management around dental implants. Periodontol 2000. 2001;27:139–47. doi: 10.1034/j.1600-0757.2001.027001139.x. [DOI] [PubMed] [Google Scholar]
- 42.Kaiser DA, Jones JD. Provisionalization for a single cementable dental implant restoration. J Prosthet Dent. 1999;81:729–30. doi: 10.1016/s0022-3913(99)70114-9. [DOI] [PubMed] [Google Scholar]
- 43.Vogel RC. Enhancing implant esthetics with ideal provisionalization. J Indiana Dent Assoc. 2002;81:11–4. 43. [PubMed] [Google Scholar]


