Abstract
Background:
Cancer of the uterine cervix is the most common malignancy amongst women in India. Identification of its pre-cancerous lesions and prevention by HPV vaccine may go a long way in decreasing the incidence.
Aim:
The aim was to study the awareness about the various aspects of the HPV infection and vaccine among medical students.
Settings and Design:
It was a cross-sectional study conducted in a tertiary care hospital of Delhi.
Materials and Methods:
150 medical students aged between 18-25 years were requested to complete a 35 point questionnaire regarding cervical malignancy, HPV infection, HPV vaccine and the answers were then analyzed.
Results:
None of the students knew the correct incidence of cervical cancer in India and 18% of them did not know that the HPV vaccination prevents cervical cancer and 50% thought that vaccination induces false sense of security. Fifty percent were unaware of HPV infection and its association with other STD's and cervical cancer. The information regarding the mechanism of action, dosage, schedule and cost of the HPV vaccine was lacking in majority of them. The limitation of this study is that it does not reflect the knowledge or awareness of a layman or full-fledged medical doctor.
Conclusions:
To conclude gaps in knowledge regarding HPV infection and vaccination existed amongst the medical students and a more integrated teaching regarding HPV carcinogenesis, vaccination and cervical cancer needs to be introduced.
Keywords: Awareness, human papillomavirus infection, human papillomavirus vaccine
Introduction
Cancer of the cervix is a major health problem in India and accounts for 26.1-43.8% of all cancers in Indian women.(1,2) Majority of risk factors of cervical cancer are related with the sexual behavior and exposure to Human papillomavirus (HPV) which has been established as a causative agent for development of cervical cancer in 70-80%.(3) The campaign of HPV vaccination is a boon to the society and this has got the virus the importance, it deserves. The pharmaceutical companies are making aggressive efforts in promoting their product, but this is associated with myths and misconceptions regarding the virus and vaccine among people.
Materials and Methods
Study setting
A cross-sectional study was conducted in March 2011 to know the level of awareness about various aspects of HPV infection and vaccine among medical students.
Participant recruitment
There were 150 medical students between 18-25 years who participated in the study, out of which 90 were males and 60 were females. The participants were assured of anonymity and confidentiality and were requested to complete a 35 point questionnaire regarding cervical malignancy, HPV infection and HPVvaccine.
The questionnaire developed for the study consisted of:
Incidence of cervical cancer in India.
HPV infection and its treatment.
Relationship between HPV and cervical and other cancers.
Pharmacology of HPV vaccine.
Spectrum of HPV vaccine and its efficacy.
Myths and beliefs associated with the vaccine.
Results
Socio-demographic features
The survey sample consisted of 150 medical students aged between 18-25 years with a mean age of 21.5 ± 1.2 years. There were 90 males and 60 females studying in second or third year of M.B.B.S and all of them were unmarried.
HPV knowledge
The answers were analyzed by the senior faculty members conducting the study. None of the students knew the correct incidence of cervical cancer in India and answers varied from 1-80%. Ninety six percent implicated HPV as a causative agent of cervical cancer but majority (32%) did not know about its association with other cancers. Forty four percent of the students answered that HPV causes vulval, penile, oral and vaginal cancers while 12% students gave weird answers like leiomyoma of uterus, seminoma and hepatocellular malignancy.
According to 55% students, HPV infection spreads by sexual as well as non-sexual route but 38% said that it only spreads sexually. Sixty nine percent felt that infection could occur in a monogamous relationship and 64% thought that HPV has a vertical transmission. Eighty five percent of them answered that all cases of HPV infections progress to cervical cancer but none knew the time of progression and 80% were of the opinion that condoms prevent HPV infection and they did not know whether HPV infection is treatable or not.
Knowledge about HPV vaccination
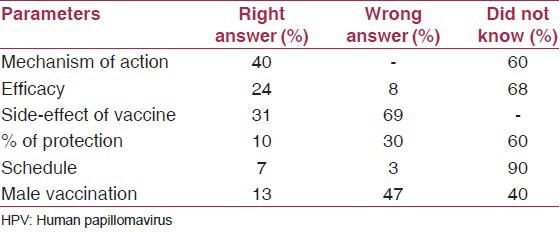
Eighteen percent of the medical students did not know that HPV vaccination prevents cervical cancer. Thirty four percent thought that it could protect against other cancers also and 17.3% expressed that HPV vaccine could protect against other sexually transmitted diseases. Fifty percent knew the correct age for initiation of vaccination. The vaccination schedule was not known to 90% of them. Sixty percent of the medical students were not aware of the mechanism of action of the vaccine and when the immunity developed after the last dose. Sixty eight percent did not know the duration of efficacy, while wild guesses were made by 24% and 69% did not have any idea about the side-effects of the vaccine. Forty percent students answered that the vaccine was approved for men [Table 1].
Table 1.
Knowledge about HPV vaccination
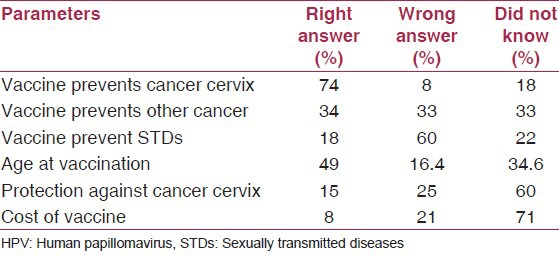
Attitude of the medical students towards vaccination
The questionnaire was designed so as know the attitude of our medical college-goers towards the vaccine. Nine percent said that vaccine would promote sexual promiscuity if given to 11-12 year olds and 50% thought that vaccination induces false sense of security. After vaccination, 51% thought that a person would test positive for HPV. 70% were not aware of the cost of the vaccine but the answers varied from Rs 500/- to 1 to 2 lacs. 65% boys thought it was expensive for routine use and would take if the cost comes down while 88% of girls would like to vaccinate themselves [Table 2].
Table 2.
Attitude of medical students towards HPV vaccination
Discussion
This is first time in the history of medicine that a cancer can be prevented by vaccination. The development of HPV vaccine represents a huge advancement in the fight against cervical cancer. The enthusiastic marketing of the vaccine by the pharmaceutical companies have brought the virus into spotlight by making the public aware of its association with cervical cancer without which the vaccine is useless. The quotient of awareness is still very low and has left many myths and misconceptions in the minds of the consumer.
The study looks at the awareness and attitude of our medical college students towards HPV and its vaccine. The medical students did not know the incidence of cervical cancer in India, but they could relate its association with cervical cancer. In our present study we have observed that the level of awareness about HPV and HPV vaccine was very low. The lack of knowledge may be due to the fact that the HPV infection is mainly asymptomatic and in 90% of cases the infection clears off without treatment. The study by Durusoy, et al., on HPV vaccine awareness and willingness of first-year students entering university in western Turkey revealed that the knowledge amongst them was remarkably poor and only 11.6% of females intended to be vaccinated vs 88% in our study.(4) The study by Naki, et al., on the awareness, knowledge and attitudes related to HPV infection and vaccine among non-obstetrician-gynecologist healthcare providers suggested that the HPV related knowledge in the physicians was significantly higher and were more willing to get vaccinated when compared to the non-physician staff.(5) The study by Zimet GD on the reasons for non-vaccination against HPV and future intentions among 19-26 year old women revealed that of the 185 non-vaccinated populations 48% were unlikely to do anything regarding the vaccination. The various reasons cited were that they were married or in a monogamous relationship, vaccine is too new, not having appropriate information, worried about side-effects or insurance coverage.(6) The attitude of students in our study was that it would induce false sense of security, test positive for HPV and was expensive for routine use.
The lack of knowledge among medical students is only tip of the iceberg. The misconceptions in the lay public would be even more and this could prove detrimental to the health of the society. Thus, widespread acceptance of HPV vaccines is likely to lend enormous health benefits by decreasing morbidity and mortality associated with cervical cancer. There exists a need to implement this fact by aggressive health education programs, group discussions and targeting mainly the adolescent population. Instead of a glamorous approach, we want the pharmaceutical companies to create awareness and educate on the various aspects of HPV, cervical cancer and its prevention. We should encourage medical students in group discussions, interactive sessions and forums where all the doubts and aspects of HPV and its association with cervical cancer can be highlighted and clarified.
To conclude, there exist gaps in knowledge regarding HPV infection and vaccination and a more integrated teaching regarding HPV carcinogenesis, vaccination and cervical cancer needs to be introduced.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Cervical cancer control in developing countries: Memorandum from a WHO meeting. Bulletin World Health Organ. 1996;74:345–51. [PMC free article] [PubMed] [Google Scholar]
- 2.Parkin DM, Bray F, Ferlay J. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94:153–6. doi: 10.1002/ijc.1440. [DOI] [PubMed] [Google Scholar]
- 3.Creasman WT. Preinvasive disease of the cervix. In: DiSaia PJ, Creasman WT, editors. Clinical Gynecology Oncology. 7th ed. Philadelphia: Elsevier; 2007. pp. 1–36. [Google Scholar]
- 4.Durusoy R, Yamazhan M, Taşbakan MI, Ergin I, Aysin M, Pullukçu H, et al. HPV vaccine awareness and willingness of first-year students entering university in western Turkey. Asian Pac J Cancer Prev. 2010;11:1695–701. [PubMed] [Google Scholar]
- 5.Naki MM, Celik H, Api O, Celik H, Kars B, Yasar E, et al. Awareness, knowledge and attitude related to HPV infection and vaccine among non-obstetrician-gynecologist healthcare providers. J Turkish-German Gynecol Assoc. 2010;11:16–21. [PMC free article] [PubMed] [Google Scholar]
- 6.Zimet GD, Weiss TW, Rosenthal SL, Good MB, Vichnin MD. Reasons for non-vaccination against HPV and future vaccination intentions among 19-26 year-old women. BMC Womens Health. 2010;10:27. doi: 10.1186/1472-6874-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]


