Abstract
Objective:
To determine whether early toxic effects from hydroxychloroquine (HCQ) could be detected by spectral-domain optical coherence tomography (SD-OCT) before symtomatic visual loss occured.
Materials and Methods:
Fifteen subjects with a history of the chronic use of hydroxychloroquine monotherapy for less than five years without fundus changes (group 1) and 15 visually normal healthy subjects (group 2) were enrolled in this study. All participants underwent systemic and ocular examination, visual field testing, and macular scan imaging using SD-OCT.
Results:
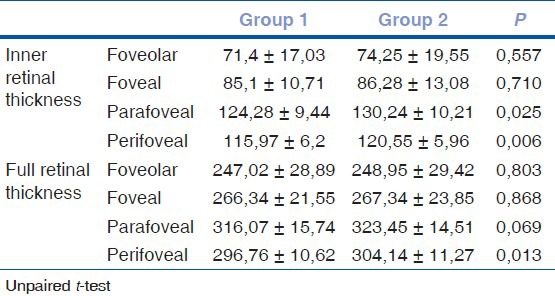
There were no significant differences in sex and ages between the groups (P > 0.05). Mean duration of HCQ usage in group 1 was 2.5 ± 1.34 (range:1-5) years. Visual field testing with central 10-2 threshold program was normal in all subjects. Inner retinal thickness in parafoveal and perifoveal area were found to be significantly lower in group 1 compared to group 2 (P < 0.01 for perifoveal, P < 0.05 for parafoveal retinal measurements). However, significant thinning was demonstrated only in full retinal thickness of perifoveal area in group 1 compared to group 2 (P: 0.013). Parafoveal and perifoveal inner retinal thickness measurements of inferior quadrants were significantly reduced in group 1 compared to group 2 (P < 0.01).
Conclusion:
Significant thinning of inner retinal layer especially in parafoveal and perifoveal areas in the absence of clinical fundus changes was observed in our study. We consider that SD-OCT may determine when inner retinal thinning starts in these patients and may contribute a quantitative approach to the early diagnosis and progression of retinal changes.
Keywords: Hydroxychloroquine, optical coherence tomography, retinal toxicity, retinal thickness
Hydroxychloroquine (HCQ) is an effective drug used in the treatment of various connective tissue disorders. Retinal toxicity is the major and most serious irreversible side effect of HCQ.[1] Risk of toxicity increases to 1% after five to seven years of use or cumulative dose of 1000 g of HCQ.[2] Although the risk of retinal degeneration increases with the duration of treatment, recent findings show that many patients may take HCQ for many years without problems, whereas, few patients develop retinal photoreceptor dysfunction at very low cumulative doses.[3,4] While additional risk factors for toxicity or idiosyncratic mechanisms are suggested, the reason for this variability remains to be established.[5]
The exact pathophysiologic mechanism of HCQ retinal toxicity is still uncertain. In animal studies it was shown that the earliest pathological changes were seen in retinal ganglion cells, but at later stages degeneration of photoreceptor and retina pigment epithelial cells was subsequently observed.[6,7] Besides it was concluded that the retinotoxic effect of chloroquine was not the result of its affinity to melanin-containing tissues.[8] The triggering event for retinopathy was proposed to be accumulation of lipid complexes in both neuronal (ganglion and bipolar) and glial cells in the retina.[9] Accordingly involvement of retinal ganglion cells and retinal nerve fiber layer (RNFL) is suggested in early retinal toxicity. In recent years, highly accurate structural representation of the retina has been possible with the invention of higher resolution spectral domain optic coherence tomography (SD-OCT) and significant alterations have been reported before the development of visible retinopathy. These changes may represent a potential preclinical state of HCQ toxicity.[10]
In our study, we aimed to determine whether early toxic effects from HCQ could be detected by SD-OCT before the onset of clinically appearent retinal toxicity. For this reason the patients receiving HCQ less than five years and without clinically appearent retinal toxicity were included in this study. In addition, we assessed macular region in quadrants to identify which areas of the macula were more selectively affected in this early period.
Materials and Methods
Fifteen patients who had systemic lupus erythematosus disease and treated with HCQ for less than five years (group 1) and 15 visually normal healthy subjects (group 2) were included in this study. Both eyes were studied. Inclusion criteria for patients was usage of HCQ less than five years without steroid or other immunosupresive treatment. Exclusion criteria included glaucoma or ocular hypertension, optic nerve and retinal diseases, uveitis, previous intraocular and refractive surgery, refractive error of more than ± 6 D sphere or ± 3 D cylinder, and media opacity that inhibited OCT examination. Patients with renal and liver dysfunction were excluded from the study. This clinical trial followed the tenets of the Declaration of Helsinki, and was approved by the institutional review board. Informed consent was obtained from all participants.
All subjects underwent a comprehensive ophthalmologic examination, visual field (VF) testing with central 10-2 programme (Zeiss Humphrey Systems, Dublin, CA,USA). Macular scan imaging was carried out on all subjects using the SD-OCT (Optovue RTVue Fourier domain OCT, Model RT 100, 2007, version 5.1; Optovue Inc, Fremont, CA, USA). All OCT scans were performed centred on the fovea for each person by the same examiner. Throughout scanning, the subject kept each eye constantly fixed on an internal target provided by the equipment. The axial resolution is approximately 5 μm. MM5 scan protocol measure the macular retinal thickness map with a 5 × 5 mm square grid centered on fixation. The grid spacing was 0.25 mm in the inner 3 × 3 mm area and 0.5 mm in the outer area (17 horizontal then 17 vertical line scans). Number of A-scans was 668 in long horizontal line, 400 in short horizontal line. The map of macular thickness was composed of three concentric circles: a central circle (fovea), an inner circle (parafovea), and an outer circle (perifovea) with radii of 1 mm, 3 mm, and 5 mm, respectively. Fourier- domain OCT with its higher resolution and better delineation of the retinal sublayers, allows us to precisely map the loss of retinal sublayers in retinal degeneration. A software programme segments the retina into inner and outer portions by delineating the boundary between the inner nuclear layer and the outer plexiform layer. Thickness of the inner retinal layer (encompasses the ganglion cell layer, inner plexiform layer and the inner nuclear layer)and full-thickness retina of the posterior pole were analyzed automatically. Thicknesses in perifoveal and parafoveal area of the macula were also analyzed automatically in four quadrants (nasal, temporal, superior, and inferior).
NCSS (Number Cruncher Statistical System) 2007 Statistical Software (Utah, USA) programme was used for statistical analysis. Besides standard descriptive statistical calculations (mean and standard deviation), unpaired sample test was used in the comparison of groups and Chi-square test was performed during the evaluation of qualitative data. Pearson correlation analysis was performed in determination of relationship between parameters. P value of less than 0.05 was considered to be statistically significant.
Results
There were no significant differences in sex and ages between the groups (P > 0.05) [Table 1]. Mean ages of group 1 and 2 were 49.0 (range: 35-67) and 48.93 (range: 34-66) years, respectively. Mean duration of HCQ usage in group 1 was 2.5 ± 1.34 (range:1-5) years. Average maintenance dosage was 200 mg/day. Every patients had normal or near- normal body mass indices. All of the patients were asymptomatic on presentation. Anterior segment and fundoscopy were normal in all subjects. VF testing was normal in all patients of group 1. Best corrected visual acuity was 20/20 using Snellen chart and intraocular pressure ranged from 12 to 18 mmHg. Average measurements of inner and full-thickness retina for each macular area (foveolar, foveal, parafoveal, perifoveal area) between 2 groups were compared [Table 2]. Inner retinal thickness in the parafoveal and perifoveal area was found to be significantly lower in group 1 compared to group 2 (P < 0.01 for perifoveal, P < 0.05 for parafoveal retinal measurements). However significant thinning was demonstrated only in full retinal thickness of perifoveal area in group 1 compared to control group (P: 0.013).
Table 1.
Demographic characteristics of the patients
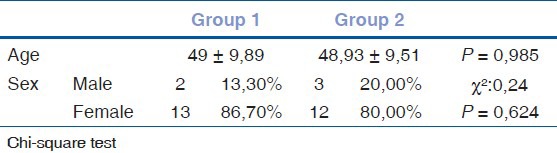
Table 2.
Mean retinal thickness of each macular areas in group 1 and 2
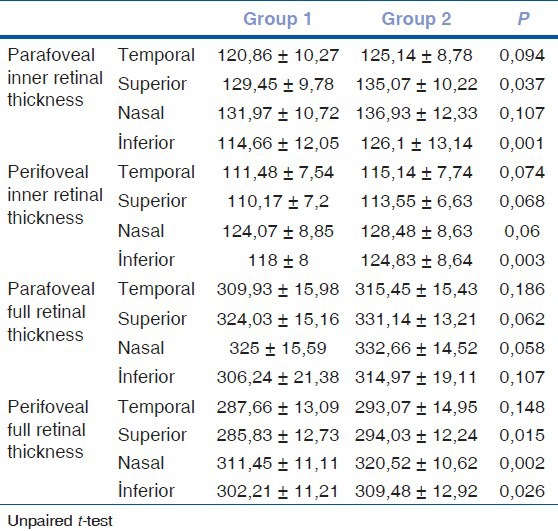
Retinal thickness measurements in macular areas were analyzed by segmentation into four quadrants (temporal, nasal, superior, inferior) [Table 3]. Parafoveal and perifoveal inner retinal thickness measurements of inferior quadrants were significantly reduced in group 1 compared to group 2 (P < 0.01). Perifoveal full retinal thickness measurements were also significantly lower in superior, nasal and inferior quadrants (P < 0.05).
Table 3.
Mean retinal thickness measurements of each quadrants of macular areas in group 1 and 2
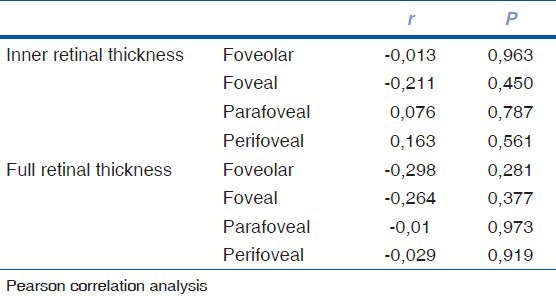
No significant correlation was found between duration of therapy and OCT parameters (P > 0.05). Table 4 lists the correlation analyses between the duration of therapy and retinal thickness parameters.
Table 4.
Correlation analysis between duration of therapy and retinal thickness parameters
Discussion
Retinal toxicity from HCQ has a low incidence, but it can have devastating effects on vision. Even after cessation of the drugs, progression of retinal degeneration can be seen.[11] There's no firm definition of early toxicity and no established criteria for diagnosing HCQ toxicity before a stage where some minor permanent visual loss is likely. Furthermore, retinal changes can be subtle and tend to be a late finding. Therefore, ophthalmic screening is recommended to recognize earliest functional and anatomical changes, before the retinal toxic damage is well developed. Recently, Marmor and associates have reported revised recommendation on screening for HCQ retinopathy. According to these recommendations annual screening should begin after five years or sooner, if there are unusual risk factors VF should be supplemented with sensitive objective test, such as multifocal electroretinogram (mfERG), SD-OCT, and fundus autofluorescence. However, relative sensitivity and specificity of these tests has not been established yet.[12] Recently, SD-OCT imaging exhibited abnormalities in areas that appeared unaffected on VF 10-2 and clinical fundoscopic examination.[10] These changes may represent potential early retinal HCQ toxicity.
Even though central VF testing can be a sensitive test for early toxicity, its effectiveness depends on patient cooperation and physician sensitivity to early changes.[12] Moreover, assesment of VF might be difficult especially in early toxicity as some patients may have macular changes not associated with VF field defects.[13] Optimal test or combination of tests is still unknown. Recently, mfERG has been shown to provide objective documentation of paracentral functional loss in early HCQ retinopathy.[14,15] Nevertheless, mfERG is limited by clinical availability, patient cooperation, specialized training for administration and interpretation, and cost. Likewise, fundus autofluorescence has demonstrated areas of early photoreceptor damage and subtle retina pigment epithelial cell defects before visual field loss. The sensitivity of fundus autofluorescence relative to other tests is still being evaluated.[16]
In our study, significant inner retinal thinning was observed in HCQ treated patients without clinically apparent retinal toxicity. Correspondingly, Pasadhika et al., reported thinning of the perifoveal inner retinal layer, especially the inner plexiform and ganglion cell layer observed by SD-OCT in HCQ treated patients in the absence of clinically evident retinal toxicity. It's interesting that thinning of RNFL was not found in these patients. This finding may suggest that RNFL thinning follows significant retinal ganglion cell degeneration.[13] In another study designed to compare patients with retinal toxicity and the others without toxicity, selective thinning of the inner retina was detected in the absence of clinically apparent fundus changes, but significant thinning of the inner, outer, and full thickness retina was observed in patients with retinal toxicity.[14] The main difference of our study is inclusion of the patients receiving HCQ treatment less than five years, whereas, patients with a history of chronic exposure of HCQ more than five years were included in these studies. Besides, in literature, several reports demonstrated early decline in retinal function of patients receiving less than five years and serial mfERG assessment may be useful for early detection of retinal changes.[15,16,17] In other studies with the inclusion of patients under long-term HCQ treatment, abnormalities at the outer retinal layers were also shown.[10] In addition, alteration of the photoreceptor inner and outer segment junction and thinning of the outer nuclear layer was identified with high resolution OCT.[18] Even so outer retinal changes observed with OCT are unlikely to be the earliest sign of toxicity due to identification of patient who had significant VF defects without clinically apparent macular findings.[10]
HCQ retinopathy is characterized by relative sparing of foveal function in the presence of parafoveal dysfunction and subsequent degeneration.[19] This is in agreement with early paracentral scotoma also seen in these patients.[12] Besides, parafoveal loss of visual sensitivity with mfERG has been also described in early HCQ retinopathy.[20,21] Moreover, it has been speculated that the most severe damage corresponds to the area of the parafoveal vascular network and longer preservation of the avascular area of the fovea may be due to the lack of retinal vessels. According to this theory, CQ retinopathy starts with the distribution of drugs via the retinal vessels first affecting the retinal ganglion cells.[22] This pathophysiological mechanism seems to be corroborated by our findings in which significant inner retinal thinning occurs in the parafoveal and perifoveal area of the macula.
In our study, we further assessed the perifoveal and parafoveal areas in quadrants to identify which areas of the macula were more selectively affected in this early period. Inner retinal thickness measurements of the inferior quadrants in the parafoveal and perifoveal areas were significantly reduced in HCQ treated patients compared to the control group. Similarly, Marmor et al., reported the quadrants of earliest outer retinal damage included the inferior retina.[23] Also, previous case reports demonstrated retinal thinning mainly in the inferior quadrant of the parafoveal and perifoveal area.[24,25] Further studies are warranted to confirm these results.
The limitations of our study are that a greater number of patients should be included and the combined application of functional testing and retinal imaging should be done to determine the optimal screening regimen. Further studies are needed to understand the pathophysiological mechanism and to determine the additional risk factors underlying this retinal toxicity. There's also a theoretical possibility that the rheumatological diseases may independently affect the retinal structures. However we would not have expected inner retinal thinning exclusively from rheumatological diseases in the absence of glaucoma or retinal vascular diseaseses.
In conclusion, our results show that thinning of the inner retinal layer of the parafoveal and perifoveal areas may be evidence of early HCQ toxicity. Although these data are not sufficient to demonstrate the sensitivity of SD-OCT for determining early subclinical retinal toxicity, we consider that SD-OCT may detect when inner retinal thinning starts in these patients and may contribute a quantitative approach to the early diagnosis and progression of retinal changes. For this reason, prospective evaluation of inner retinal layer thickness during HCQ treatment may be warranted to detect structural and functional changes early enough so that irreversible retinal damage can be avoided.
Footnotes
Source of Support: Nil.
Conflict of Interest: No.
References
- 1.Rynes RI. Antimalarial drugs in the treatment of rheumatological diseases. Br J Rheumatol. 1997;36:799–805. doi: 10.1093/rheumatology/36.7.799. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe F, Marmor MF. Rates and predictors of hydroxychloroquine retinal toxicity in patients with rheumatoid arthritis and systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2010;62:775–84. doi: 10.1002/acr.20133. [DOI] [PubMed] [Google Scholar]
- 3.Ruther K, Foerster J, Berndt S, Schroeter J. Chloroquine/hydroxychloroquine: Variability of retinotoxic cumulative doses. Ophthalmologe. 2007;104:875–9. doi: 10.1007/s00347-007-1560-7. [DOI] [PubMed] [Google Scholar]
- 4.Turgut B, Turkcuoglu P, Serdar Koca S, Aydemir O. Detection of the regression on hydroxychloroquine retinopathy in optical coherence tomography. Clin Rheumatol. 2009;28:607–9. doi: 10.1007/s10067-009-1108-0. [DOI] [PubMed] [Google Scholar]
- 5.Michaelides M, Stover NB, Francis PJ, Weleber RG. Retinal toxicity associated with hydroxychloroquine and chloroquine: Risk factors, screening, and progression despite cessation of therapy. Arch Ophthalmol. 2011;129:30–9. doi: 10.1001/archophthalmol.2010.321. [DOI] [PubMed] [Google Scholar]
- 6.Rosenthal AR, Kolb H, Bergsma D, Huxsoll D, Hopkins JL. Chloroquine retinopathy in the rhesus monkey. Invest ophthalmol Vis Sci. 1978;17:1158–75. [PubMed] [Google Scholar]
- 7.Hallberg A, Naeser P, Andersson A. Effects of long-term chloroquine exposure on the phospholipid metabolism in retina and pigment epithelium of the mouse. Acta Ophtalmol. 1990;68:125–30. doi: 10.1111/j.1755-3768.1990.tb01892.x. [DOI] [PubMed] [Google Scholar]
- 8.Kuhn H, Keller P, Kovács E, Steiger A. Lack of correlation between melanin affinity and retinopathy in mice and cats treated with chloroquine or flunitrazepam. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1981;216:177–90. doi: 10.1007/BF00408159. [DOI] [PubMed] [Google Scholar]
- 9.Duncker G, Bredehorn T. Chloroquine-induced lipidosis in the rat retina: Functional and morphological changes after withdrawal of the drug. Graefes Arch Clin Exp Ophthalmol. 1996;234:378–81. doi: 10.1007/BF00190714. [DOI] [PubMed] [Google Scholar]
- 10.Kimberly E, Han DP, Schell J, Godara P, Rha J, Carroll J. Spectral-domain optical coherence tomography and adaptive optics may detect hydroxychloroquine retinal toxicity before symptomatic vision loss. Trans Am Ophthalmol Soc. 2009;107:28–33. [PMC free article] [PubMed] [Google Scholar]
- 11.Easterbrook M. Long-term course of antimalarial maculopathy after cessation of treatment. Can J Ophthalmol. 1992;27:237–39. [PubMed] [Google Scholar]
- 12.Marmor MF, Kellner U, Lai TY, Lyons JS, Mieler WF American Academy of Ophthalmology. Revised recommendations on screening for chloroquine and hydroxychloroquine retinopathy. Ophthalmology. 2011;118:415–22. doi: 10.1016/j.ophtha.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 13.Pasadhika S, Fishman GA, Choi D, Shahidi M. Selective thinning of the perifoveal inner retina as an early sign of hydroxychloroquine retinal toxicity. Eye (Lond) 2010;245:756–62. doi: 10.1038/eye.2010.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pasadhika S, Fishman GA. Effects of chronic exposure to hydroxychloroquine or chloroquine on inner retinal structures. Eye. 2010;24:340–46. doi: 10.1038/eye.2009.65. [DOI] [PubMed] [Google Scholar]
- 15.Lai TY, Chan WM, Li H, Lai RY, Lam DS. Multifocal electroretino-graphic changes in patients receiving hydroxychloroquine therapy. Am J Ophthalmol. 2005;1405:794–807. doi: 10.1016/j.ajo.2005.05.046. [DOI] [PubMed] [Google Scholar]
- 16.Maturi RK, Yu M, Weleber RG. Multifocal electroretinographic evaluation of long-term hydroxychloroquine users. Arch Ophthalmol. 2004;1227:973–81. doi: 10.1001/archopht.122.7.973. [DOI] [PubMed] [Google Scholar]
- 17.Moschos MN, Moschos MM, Apostolopoulos M, Mallias JA, Bouros C, Theodossiadis GP. Assessing hydroxychloroquine toxicity by the multifocal ERG. Doc Ophthalmol. 2004;1081:47–53. doi: 10.1023/b:doop.0000018385.99215.0d. [DOI] [PubMed] [Google Scholar]
- 18.Rodriguez-Padilla JA, Hedges TR, 3rd, Monson B, Srinivasan V, Wojtkowski M, Reichel E, et al. High-speed ultra-high-resolution optical coherence tomography findings in hydroxychloroquine retinopathy. Arch Ophthalmol. 2007;125:775–80. doi: 10.1001/archopht.125.6.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Browning DJ. Hydroxychloroquine and chloroquine retinopathy: Screening for drug toxicity. Am J Ophthalmol. 2002;1335:649–56. doi: 10.1016/s0002-9394(02)01392-2. [DOI] [PubMed] [Google Scholar]
- 20.Lyons JS, Severns ML. Detection of early hydroxychloroquine retinal toxicity enhanced by ring ratio analysis of multifocal electroretinography. Am J Ophthalmol. 2007;143:801–9. doi: 10.1016/j.ajo.2006.12.042. [DOI] [PubMed] [Google Scholar]
- 21.Lyons JS, Severns ML. Using multifocal ERG ring ratios to detect and follow Plaquenil retinal toxicity: A review: Review of mfERG ring ratios in Plaquenil toxicity. Doc Ophthalmol. 2009;118:29–36. doi: 10.1007/s10633-008-9130-0. [DOI] [PubMed] [Google Scholar]
- 22.Kellner U, Kellner S, Weinitz S. Chloroquine retinopathy: Lipofuscin- and melanin-related fundus autofluorescence, optical coherence tomography and multifocal electroretinography. Doc Ophthalmol. 2008;1162:119–27. doi: 10.1007/s10633-007-9105-6. [DOI] [PubMed] [Google Scholar]
- 23.Marmor MF. Comparison of screening procedures in hydroxychloroquine toxicity. Arch Ophthalmol. 2012;1304:461–9. doi: 10.1001/archophthalmol.2011.371. [DOI] [PubMed] [Google Scholar]
- 24.Korah S, Kuriakose T. Optical coherence tomography in a patient with chloroquine-induced maculopathy. Indian J Ophthalmol. 2008;566:511–3. doi: 10.4103/0301-4738.43379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kelmenson AT, Brar VS, Murthy RK, Chalam KV. Fundus autofluorescence and spectral domain optical coherence tomography in early detection of Plaquenil maculopathy. Eur J Ophthalmol. 2010;204:785–8. doi: 10.1177/112067211002000423. [DOI] [PubMed] [Google Scholar]


