Abstract
OBJECTIVE:
The acetabular buttress-plate has been widely used in treating difficult cases with satisfying clinical results. However, the biomechanical properties of a postoperative acetabular fracture fixed by the buttress-plate are not clear. The purpose of this study was to evaluate the biomechanical properties of stability after the anterior tube buttress-plate fixation of complex acetabular fractures in the quadrilateral area.
METHODS:
A construct was proposed based on anterior construct plate - 1/3 tube buttress plate fixation for acetabular both-column fractures. Two groups of six formalin-preserved cadaveric pelvises were analyzed: (1) group A, the normal pelvis and (2) group B, anterior construct plate-1/3 tube buttress plate with quadrilateral area fixation. The displacements were measured, and cyclical loads were applied in both standing and sitting simulations.
RESULTS:
As the load was added, the displacements were A<B, increasing in line. In the 600 N physiological loading, the differences were significant (standing position: p = 0.013; sitting position: p = 0.009) between groups A and B.
CONCLUSION:
The anterior construct plate - 1/3 tube buttress plate fixation provided a better stable construct for early sitting. The standing mode yielded more significant differences between the groups. Placing a 1/3 tube buttress-plate via an anterior approach is a novel method of providing quadrilateral area support in this setting.
Keywords: Acetabular Fractures, Quadrilateral Area, Articular Comminution, Internal Fixation, Biomechanics
INTRODUCTION
Treating acetabular fractures in the quadrilateral area is one of the most challenging problems in the orthopedic trauma department because such fractures often belong to the group of articular comminuted fractures. The bone in the quadrilateral area is thin, and the anatomical site is deep. The most difficult part of these bony deficits is that the screw can easily penetrate into the hip 1. Acetabular both-column fractures are the most common fracture in the quadrilateral area 1,2. We often select a multi-approach 3 or modified ilioinguinal approach 1 to expose this fracture during the operation. Due to the presence of many postoperative complications, the reduction and internal fixation of acetabular both-column fractures though a single anterior approach has been a direction sought by many orthopedic doctors 4,5.
The main problem is the difficulty involved in fixing the posterior column fracture block (quadrilateral area) through a single anterior approach. The lag screw through the anterior column to the posterior column would produce a certain clinical result 1,6, but its fixation is eccentric (partial posterior) and requires the fracture blocks of the anterior and posterior columns to not be crushed 6,7. The cerclage wires also produce some good results 8. However, more complex hardware combinations necessitate larger exposures, which are often associated with higher rates of infection and overall complications 9.
Given these issues, the fixation technology of the bone surface (buttress-plate) was used to fix the posterior column fracture block. A titanium plate combined with 1/3 tube buttress-plate has been widely used and produces a better therapeutic effect 3,4. The stability of elastic fixation to the quadrilateral area by the tube buttress-plate has always been controversial 3,8. Stability is essential because an ingrowth component can only be successful if it is adequately stabilized against the host bone to allow host bone ingrowth to occur 9. There are currently no biomechanical evaluations in the literature comparing buttress-plate for the treatment of complex acetabular fractures. Therefore, this study evaluated the biomechanics of a tube buttress-plate in both standing 1 and sitting 10 simulations.
METHODS
Specimens
We selected six formalin-preserved cadaveric pelvises for this investigation. Six normal human specimens that included the fourth lumbar vertebra and proximal 1/3 of the femoral shaft were obtained from the Department of Anatomy of Southern Medical University. These specimens had no known metabolic bone disease or tumors. The trabecular appearance and bony quality were examined, and bone abnormalities were ruled out by a standard anteroposterior X-ray. The soft tissue was removed, except the sacrum, sacroiliac joint, hip joint capsule, ligaments of the sacral spine, sacral tubercle and obturator internus (Figure 1). Only one hip was used for testing for each hip surgery. We selected the reconstruction plate, 1/3 tube and titanium screws (3.5 mm) of AO, and ZWICKZ100 material machine (Germany ZWICKZ, a precision of 0.1%, Department of Mechanical Room of the Wuhan University of Technology).
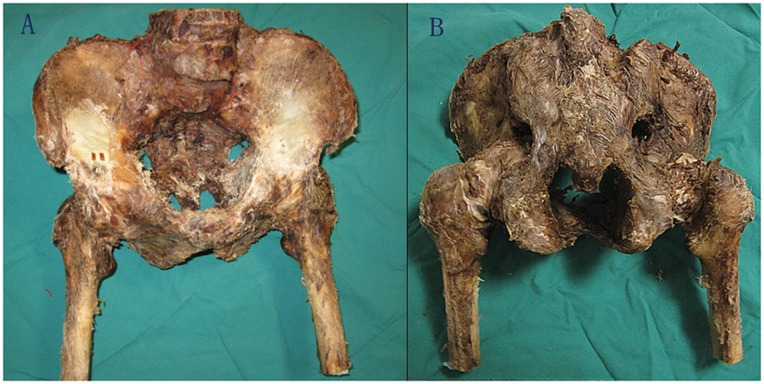
Figure 1.
Normal specimens (A. front, B. back).
Displacement measurement
The specimen was fixed in the position of standing or sitting (Figure 2) on the pelvis as previously described by Pierannunzii L 1 and Gao YC 10. Then, the specimen was treated repeatedly with loads from 400 to 700 Newtons. In the standing position, the lateral displacement of the posterior column fracture in the inner wall and the longitudinal displacement of the anterior inferior iliac spine were measured with a multifunctional digital dial gauge (Beijing Deli love Monitoring Technology, Beijing, China). In the sitting position, the lateral displacement of the posterior column fracture in the inner wall was measured with a multifunctional digital dial gauge, and the overall axial displacement of the pelvis was measured with the beam sensor of the ZwickZ100 electronic universal testing machine. The stiffness of the specimens was calculated. First, we tested the six normal human pelvises in both the standing and sitting simulations as the control group. Then, we produced high both-column fractures using a wire saw on one hip (Figure 3) and fixed the fracture using anterior construct plate -1/3 tube buttress-plate fixation (group B, Figure 4). We tested the fractured pelvic again in the standing and sitting positions consecutively.
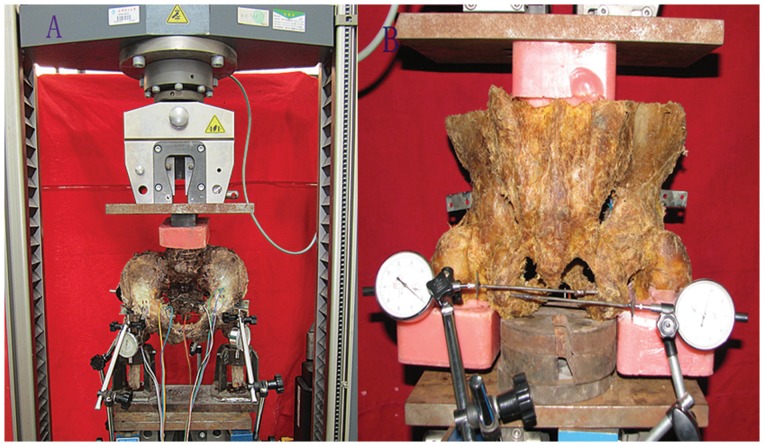
Figure 2.
Tests in the pelvis. (A. front, B. back).
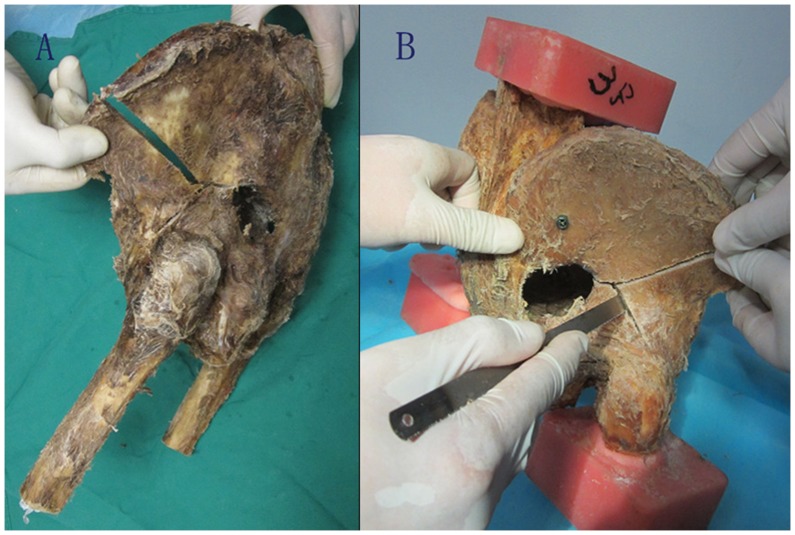
Figure 3.
Cadaver fracture model of high column fracture. (A. lateral, B. making fracture).
Figure 4.
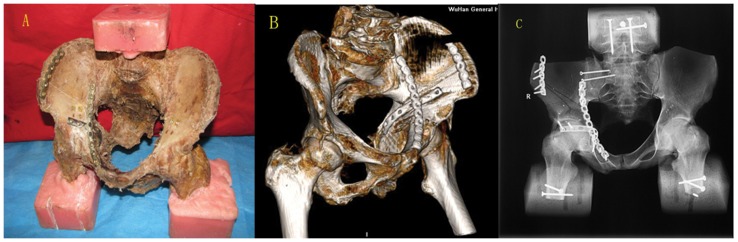
The anterior construct plate-1/3 tube buttress-plate fixed the specimen. (A. General view, B. CT reconstruction, C. X-rays scan).
Analysis
According to the matta standard 2, the displacement of a fracture after internal fixation of less than 1 mm indicated anatomic reduction; if the lateral displacement of the posterior column wall was greater than 1 mm, the femoral head would appear central dislocation; and if the longitudinal displacement of the anterior inferior iliac spine was greater than 1 mm, the femoral head would appear upward dislocation.
The “Paired-Sample T Test” was used to assess the significance of the differences between the groups for each index of measurement. Initially, all conditions were considered together; subsequently, the tests were conducted separately for each position by the “2-Repeating Factor of ANOVA”. An alpha-level of 0.05 was used for each test to test the differences between the simulations.
All data were expressed as the means±SE unless otherwise stated, and the statistical analysis was performed with SPSS 13.0 statistics software for Windows (SPSS, Chicago, IL).
RESULTS
The fracture blocks of the anterior and posterior columns in the specimens after internal fixation were firmly fixed immediately, resulting in anatomic reduction. The soft tissue (the sacrotuberous ligament, sacrospinous ligament and obturator internus) was taut. The screws and plates did not crack during the testing process. The maximum separation was less than 2 mm. After the removal of the load, the acetabular plate and fixation returned to their initial form or state.
The relationship between load and displacement
As the load was added, the displacements were A<B, increasing in line. In the standing position, the displacement of the specimens in group B under the 400 N load was greater than 1 mm, indicating that the dislocation of the femoral head began to appear under the 400 N load. In the inner wall, horizontal displacement of more than 1 mm appeared at the following loads: 400 N in 1 case, 500 N in 1 case, 600 N in 1 case, and 700 N in 2 cases. In the anterior wall, longitudinal displacement of more than 1 mm appeared at the following loads: 400 N in 1 case, 500 N in 2 cases, 600 N in 3 cases, and 700 N in 3 cases. The statistical analysis showed that there was a significant difference between the horizontal and vertical displacements (p<0.05) in group A to group B (Tables 1 and 2).
Table 1.
Different loading-lateral displacement of the posterior column inner wall in the standing position (x ± s mm).
| Different loads (N) | |||||||
| Group | 400 | 500 | 600 | 700 | |||
| A | 0.14±0.04 | 0.15±0.07 | 0.19±0.06 | 0.24±0.06 | |||
| B | 0.65±0.29 | 0.72±0.29 | 0.76±0.30 | 0.82±0.32 | |||
Paired-Sample T Test: group A - group B (p<0.012).
Table 2.
Different loading-lateral displacement of the anterior inferior iliac spine in the standing position (x ± s mm).
| Different loads (N) | ||||||
| Group | 400 | 500 | 600 | 700 | ||
| A | 0.14±0.05 | 0.18±0.07 | 0.26±0.10 | 0.31±0.12 | ||
| B | 0.24±0.18 | 0.29±0.19 | 0.36±0.18 | 0.40±0.16 | ||
Paired-Sample T Test: group A - group B (p<0.032).
In the sitting position, the lateral displacement of the posterior column-inner wall in group B was absolutely within 0.5(mm and thus was without dislocation. The statistical analysis showed that although the numerical value of the lateral displacement of the posterior column-inner wall in group B was greater than that in group A, there was no significant difference (p>0.05) (Table 3). The axial stiffness of the pelvis in group A was significantly larger than that in group B (p<0.01) (Table 4).
Table 3.
Different loading-lateral displacement of the posterior column inner wall in the sitting position (x ± s mm).
| Different loads ( N ) | ||||
| Group | 400 | 500 | 600 | 700 |
| A | 0.18±0.07 | 0.20±0.06 | 0.21±0.05 | 0.22±0.06 |
| B | 0.26±0.17 | 0.28±0.18 | 0.32±0.18 | 0.35±0.20 |
Paired-Sample T Test :group A - group B (p>0.16).
Table 4.
Different loading-axial stiffness of the pelvis in the sitting position (x ± s N/mm).
| Different loads (N) | ||||
| Group | 400 | 500 | 600 | 700 |
| A | 208.5±54.3 | 213.0±50.6 | 221.5±59.4 | 222.0±40.3 |
| B | 118.2±10.5 | 125.6±8.9 | 129.9±7.5 | 132.5±7.1 |
Paired-Sample T Test: group A - group B (p<0.01).
Quantitative analysis of the test results on the physiological load (600 N)
In the standing position, the longitudinal stiffness of the anterior wall was 2883.9±1901.2 N/mm in group A and 1015.5±365.3 N/mm in group B. We analyzed the two measuring indices (the lateral displacement of the inner wall and the longitudinal stiffness of the anterior) comprehensively using the statistical method of "2 Repeating Factor Of ANOVA ", which showed a significant difference (F = 14.3, p = 0.013) between groups A and B. In the sitting position, we analyzed the two measuring indices (the lateral displacement of the inner wall and the axial stiffness of the pelvis) comprehensively, which showed a significant difference (F = 16.9, p = 0.009) between groups A and B.
DISCUSSION
The acetabulum represents a basin-like anatomic structure that bears the body's weight, receives the resultant force from the ground, and accommodates ambulatory activity and hip joint mobility 11. Open anatomic reduction of the articular surface combined with rigid internal fixation and early mobilization is the standard current treatment for injuries to this region 11,12. Maintaining stability of the joint is very important 9. The stability of the hip mainly depends on the blocking effect of the acetabular bone. The quadrilateral area (square area) is located in the inner side of the acetabular posterior column. Comminuted fractures are likely caused by strong violence to the longitudinal femoral neck. The femoral head with the fracture blocks would transpose to the intrapelvic direction 8,13. The bone in the quadrilateral area and the iliopectineal bulge of the anterior column are thin and close to the joint 3, limiting the types of fixation that can be used in this area. The blocking effect of the bone block in the quadrilateral area is often neglected. The existing classification of acetabular fractures does not list quadrilateral area fractures separately, although except for simple fractures, all other fractures involve this area according to the classification of Letournel and Judet. As society ages, the number of osteoporosis fractures of the quadrilateral area is increasing. Effectively fixing such fractures is becoming an urgent issue. To avoid the risk area, the current treatment basically only involves no fixation or indirect fixation. When the screw is away from the acetabular fracture, the reliable degree of fixation decreases by approximately 50% 14, and the stability of the acetabulum decreases 15,16. In general, only the anterior reconstruction titanium plate-screw system shows difficulty in fully achieving reliable fixation 8,14,16. The plate of the anterior column or posterior column only played a supporting role. Palliative care is only a prelude to joint replacement.
Historically, hip biomechanics suggested that the bearing force of the acetabulum could be divided into two components in the horizontal and vertical directions of the coronal plane 16,17. The shear stress in the horizontal direction often promoted the fracture block to emerge as a transverse separation 8,13,18,19. We should emphasize the reduction and stability of the quadrilateral area in the operation, not only paying attention to reducing and fixing the surface fracture of the posterior column 16. The lag screw fixation was eccentric and could play a certain role in fixation. However, not all acetabular fractures are amenable to the placement of an interfragmentary lag screw 6,7,20, and the fracture may be displaced during tightening of the interfragmentary lag screw 20.
Given the characteristics of the anatomy and acetabulum biomechanics, a reconstruction titanium plate-1/3 tube type elastic buttress-plate, which is typically used as the fixation technology of the bone surface, is an ideal internal fixation. It has the advantage of a simple application during the operation. The routine method is almost unable to achieve fixation to the acetabular fossa and quadrilateral area as well as the 1/3 tube 3,4,12.
Cole 19 first reported the use of elastic buttress-plate fixation to resist the shear stress of the inner wall. The proximal end of the plate was fixed to the iliac bone. He highlighted that an excessive correction plate, which is similar to a spring, was used to hold the pieces of a medial wall fracture downward in the pelvic side wall. A recent clinical study showed that elastic plate stability was reduced by postoperative turning during nursing care and that the plate was remodeled easily, resulting in the loss of its fixation role after fatigue. It also has the potential to cut pelvic organs. Farid 8 made some improvements with the addition of cerclage wire in the elastic steel plate to strengthen the fixation. To provide adequate pressure, the wire needed to be thread through the greater sciatic notch, and stripping during the operation was significant. All of these factors can easily injure the sciatic nerve and peripheral vascular system. Pan 3 added the 1/3 tubular plate under the anterior column reconstruction titanium plate and attempted to rely on the extrusion of the titanium plate to reinforce the elastomeric tube, thereby fixing the bone block. Laflamme 13 performed a follow-up study over 4.2 years in elderly people using a buttress-plate to fix fracture blocks in the quadrilateral area and found that the anatomical reduction rate was 90.5%. There are currently no biomechanical evaluations in the literature comparing buttress-plate for the treatment of complex acetabular fractures. Therefore, this study evaluated the tube buttress-plate.
The horizontal displacement in the posterior column wall reflects the shear resistance of the internal fixator after the operation. Upward or slip displacements, which are produced by the push of the femoral head-acetabular roof, reflect the overall standing stability of the hip. The longitudinal displacement of the sacroiliac joint mainly comprises the longitudinal stiffness of the complete pelvis. However, the stiffness of the entire pelvis is not equivalent to the stiffness of the sacroiliac joint 21. The stability of the hip also produces axial stiffness in the pelvis. In the same pelvis, the difference in the axial stiffness reflects the stability of the fixation. We selected cadaveric specimens to create a high both-column fracture model. According to the stress distribution of the hip after loading in the coronal plane, the results showed the following: 1. as the load increased from 400 N to 700 N, the displacement increased, which was consistent with the law of conventional dynamics; and 2. in the standing position, the displacements in group B were larger. When the load exceeded 400 N, dislocation of the femoral head began to appear. Compared with the normal acetabulum, there was a significant difference in group B (Tables 1 and 2). In the sitting position, the overall axial stiffness of the pelvis was reduced (Tables 3 and 4). The lateral displacement of the inner wall in the posterior column was within 0.5 mm, with no dislocation, which was not significantly different (Table 3).
The patients are in a wheelchair for 2-6 weeks after the operation. This stage is the critical period for fracture repair and creation of the articular surface as well as for further functional exercise. Standing early is vital to reduce the long-term complications of bed rest and recover the patient's confidence. However, if functional exercises are started too early, the loss outweighs the gain. At home and abroad, there are few reports that note that patients need to take care of the physiological conditions of fracture reduction after the operation 10. We tested the positions of sitting and standing in this experiment, retaining portions of the soft tissue. We also fully simulated the postoperative physiological status of the patients, which was close to the clinical status. In group B, the experimental results showed that the hip was prone to instability in the standing position. The shear force of the 1/3 tube type titanium plate was poor. Although the axial stiffness of the pelvis in the sitting position was poorer than that of the normal pelvis, acetabulum fractures showed a satisfactory reduction on physiological load. Thus, sitting early is safe.
In general, as long as the patient's condition allows it, the operation of the acetabular fracture should be performed 3-7 days and no more than 2 weeks after the injury. Otherwise, the difficulty of the operation would increase 22. Thus, because the healing rate of acetabular fractures is very rapid, the fractures will tend to be stable after 2 or 3 weeks because they can easily form a localized scab. Along with the process of fracture healing, the fixation stability of an acetabular fracture will be enhanced, that is, the inner fixation would bear weight-stress for a short time only. Its main contribution of share the weight is going on in the initial 2 weeks. All of these factors may explain why single-point elasticity fixation (1/3 tube type titanium plate) can obtain satisfactory results in the fixing portion of the posterior column fracture.
In addition, the proper selection of the operation approach will reduce the degree of difficulty and improve the quality of the reduction 23. In the reduction of both column acetabular fractures, we often adopt the combination approach, which needs a wide range of stripping and a long operation time. Postoperative heterotopic ossification also occurs at a high rate. We selected a single ilioinguinal approach in the fixation of an anterior construct plate-1/3 tube buttress plate, fully utilizing the advantages of the anterior approach, which are essential to maximize the union rates and minimize the complications in these difficult cases 24. The ilioinguinal approach also could be able to fix most complex fractures of the acetabulum25. Therefore, the reduction and internal fixation of both-column fractures using a single anterior approach has been the direction taken by many orthopedic doctors 4,5. However, the main problem is that the block posterior column and the quadrilateral area are difficult to fix. The 1/3 tube plate had better results than palliative care (no fixation or indirect fixation) in weakening the shear stress on the inner wall but is poorer to prevent separation of the distal bone block. More work is needed to search for a suitable fixator.
A few points should be noted. First, we only used six specimens as representatives because human pelvis specimens are very precious. Second, we elected to pursue a repeated measures design rather than a matched pair design for this investigation. Six specimens were tested four successive times. To reduce the effect of the repeated test impacts, the experiments were performed randomly in the simulated positions. At the same time, the maximum load (700 N) was within the yielding point of the pelvises 26. The mechanical strength had no obvious effect on the elastic deformation. Third, although there are individual differences among the experimental samples, the experimental load was selected based on the characteristics of each specimen 16,20. Therefore, we selected a large observation range, from 400 to 700 N, and did not perform the analysis one by one, but rather only focused on the analysis of the 600 N physiological weight 10,16. In addition, Vailas 27 highlighted that the function of the soft tissue could not be ignored. The integrity of the articular capsule determined the stability of the hip joint. To be close to the actual clinical state, we retained the important ligaments and muscles for convenient measurements in this experiment, which was different from previous studies 9,20.
ACKNOWLEDGMENTS
The authors wish to thank Zhu Jian (Department of Thoracic Cardiovascular Surgery, Wuhan General Hospital of Guangzhou Command, Wuhan, People's Republic of China) for his careful revision of the manuscript and excellent technical assistance.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Pierannunzii L, Fischer F, Tagliabue L, Calori GM, d'Imporzano M. Acetabular both-column fractures: essentials of operative management. Injury. 2010;41(11):1145–9. doi: 10.1016/j.injury.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 2.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–45. [PubMed] [Google Scholar]
- 3.Pan ZJ, Chen HX. Clinical department of orthopedics trauma diseases. Beijing: Scientific And Technical Documentation Press; 2010. pp. 345–7. [Google Scholar]
- 4.El-khadrawe TA, Hammad AS, Hassaan AE. Indicators of outcome after internal fixation of complex acetabular fractures. Alexandria Journal of Medicine. 2012;2(48):99–107. [Google Scholar]
- 5.Jeffcoat DM, Carroll EA, Huber FG, Goldman AT, Miller AN, Lorich DG, et al. Operative treatment of acetabular fractures in an older population through a limited ilioinguinal approach. J Orthop Trauma. 2012;26(5):284–9. doi: 10.1097/BOT.0b013e31821e10a2. [DOI] [PubMed] [Google Scholar]
- 6.Lin HH, Hung SH, Su YP, Chiu FY, Liu CL. Cerclage wiring in displaced associated anterior column and posterior hemi-transverse acetabular fractures. Injury. 2012;43(6):917–20. doi: 10.1016/j.injury.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Vanderschot P. Treatment options of pelvic and acetabular fractures in patients with osteoporotic bone. Injury. 2007;38(4):497–508. doi: 10.1016/j.injury.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 8.Farid YR. Cerclage wire-plate composite for fixation of quadrilateral plate fractures of the acetabulum:a checkrein and pulley technique. J Orthop Trauma. 2010;24(5):323–8. doi: 10.1097/BOT.0b013e3181c90bbe. [DOI] [PubMed] [Google Scholar]
- 9.Gililland JM, Anderson LA, Henninger HB, Kubiak EN, Peters CL. Biomechanical analysis of acetabular revision constructs: Is pelvic discontinuity best treated with bicolumnar or traditional unicolumnar fixation? J Arthroplasty. 2013;28(1):178–86. doi: 10.1016/j.arth.2012.04.031. [DOI] [PubMed] [Google Scholar]
- 10.Gao YC, Guo Z, Fu J, Tian WJ. Three-dimensional finite element analysis of the pelvis in sitting stance. Journal of Clinical Rehabilitative Tissue Engineering Research. 2011;22(15):3997–4001. [Google Scholar]
- 11.Kubota M, Uchida K, Kokubo Y, Shimada S, Matsuo H, Yayama T, et al. Changes in gait pattern and hip muscle strength after open reduction and internal fixation of acetabular fracture. Arch Phys Med Rehabil. 2012;93(11):2015–21. doi: 10.1016/j.apmr.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 12.Briffa N, Pearce R, Hill AM, Bircher M. Outcomes of acetabular fracture fixation with ten years' follow-up. J Bone Joint Surg Br. 2011;93(2):229–36. doi: 10.1302/0301-620X.93B2.24056. [DOI] [PubMed] [Google Scholar]
- 13.Laflamme GY, Hebert-Davies J, Rouleau D, Benoit B, Leduc S. Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury. 2011;42(10):1130–4. doi: 10.1016/j.injury.2010.11.060. [DOI] [PubMed] [Google Scholar]
- 14.Shazar N, Brumback RJ, Novak VP, Belkoff SM. Biomechanical evaluation of transverse acetabular fracture fixation. Clin Orthop Relat Res. 1998;(352):215–22. [PubMed] [Google Scholar]
- 15.Harnroongroj T, Asavamongkolkul A, Chareancholvanich K. Reconstruction of the pelvic brim and its role in the reduction accuracy of displaced T-shaped acetabular fracture. J Med Assoc Thai. 2000;83(5):483–93. [PubMed] [Google Scholar]
- 16.Wu XB, Zhang Q, Guo MK, Zhang YZ. Biomechanical comparison of 4 plateinternal fixation methods for simulated fractures of acetabular posterior column. Acta Acad Med Militaris Tertiae. 2010;7(32):665–8. [Google Scholar]
- 17.Mao BY. Biomechanical analysis of surgical revision in artificial hip joint. Orthopedic J China. 2003;11(10):700–2. [Google Scholar]
- 18.Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010;92(2):250–7. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 19.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;(305):112–23. [PubMed] [Google Scholar]
- 20.Mehin R, Jones B, Zhu Q, Broekhuyse H. A biomechanical study of conventional acetabular internal fracture versus locking plate fixation. Can J Surg. 2009;52(3):221–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Wang F, Liu R, Wang QG, Shi DF, Yang Q, Chen B, et al. Testing of axial stiffness of human pelvis under gradient vertical loads. J Med Biomechanics. 2011;1(26):57–61. [Google Scholar]
- 22.Cai XH, Chen ZH, Xu YN, Huang JF, Xu F, Liu XM, et al. Relevancy factor analysis on the choice of operative approaches for different acetabular fractures. Orthopedic J China. 2006;20(14):1526–8. [Google Scholar]
- 23.Yu LX, Wang L, Liu QP, Zhang H. Surgical therapy of displaced complex acetabular fractures and analysis of influence factors in 40 patients. Orthopedic J China. 2012;8(20):685–7. [Google Scholar]
- 24.Qin XD, Li X, LV TR, Song LJ, Zhang N, Fan WM. The subinguinal approach for treatment of acetabular fractures. Chin J Orthop Traumatol. 2010;10(12):936–9. [Google Scholar]
- 25.Ma WH, Xu RM, Xue B, Feng JX. Surgical treatment of severe comminuted acetabular fractures. J Bone Joint Injury. 2003;2(18):88–90. [Google Scholar]
- 26.Liu Y, Chen FZ, Mei HJ, You H, Yang Q, Wang Z, et al. Biomechanical studies of normal pelvis in static standing position . Clin Med Eng. 2010;17(6):7–12. [Google Scholar]
- 27.Vailas JC, Hurwitz S, Wiesel SW. Posterior acetabular fracture-dislocations: fragment size, joint capsule, and stability. J Trauma. 1989;29(11):1494–6. [PubMed] [Google Scholar]