Abstract
Background
The Commission on Social Determinants of Health has urged governments across the world to promote health equity by reducing the gap between the most and least deprived individuals in society. Some of this gap can be bridged by promoting healthy lifestyles through targeted public health policy and interventions.
Methods
Cross-sectional analyses of data on behavioural risk factors, individual socioeconomic factors, and neighbourhood deprivation score collected from 26,290 adults aged over 16 years who participated in the 2008 East of England Lifestyle Survey.
Results
After adjustment for individual socioeconomic factors, across quintiles of increasing neighbourhood deprivation, participants were more likely to smoke and less likely to consume five portions of fruit and vegetables on five or more days of the week (least deprived versus most deprived quintile- odds ratios for not smoking 0.45 [0.41 to 0.50]; and fruit and vegetable consumption 0.70 [0.64 to 0.76] p-trend <0.0001). Greater neighbourhood deprivation and lower occupational social class were independently associated with a lower summary healthy lifestyle score (both p-trend <0.0001).
Conclusions
Public health interventions aimed at reducing health inequalities by targeting behavioural risk factors may focus in particular on reducing smoking and increasing fruit and vegetable consumption in more deprived communities.
INTRODUCTION
The influences of individual level behavioural and socioeconomic factors (for example income, education, occupational social class) and health inequalities have been studied extensively. However, the association between behavioural risk factors and levels of neighbourhood deprivation is less clear1. Studies show that area level deprivation is associated with atherosclerosis and coronary heart disease but it is unclear how much of this association is mediated by behavioural risk factors2,3. Individuals achieving four healthy behaviours (not smoking, moderate alcohol intake- excluding non-drinkers, fruit and vegetable consumption and physical activity) on average have a 14 year higher life expectancy than individuals achieving no healthy behaviours4 and have a lower incidence of stroke5,6. Behavioural risk factors also explain some of the socio-economic inequalities in morbidity and mortality from other chronic diseases7-13.
The World Health Organisation Commission on Social Determinants of Health has called for national and global health-equity surveillance systems for monitoring of policy and action to reduce health inequity and create a more just and fairer society14. Since 1998, the UK government has tried to reduce health inequalities through various national and local initiatives15,16, and a recently commissioned review highlighted that individuals who live in the poorest areas die, on average, seven years earlier than people in the richest neighbourhoods17. A recent study suggested that population-wide best-practice interventions to reduce levels of classic Coronary Heart Disease (CHD) risk factors (blood pressure, cholesterol, blood glucose and smoking cessation) could reduce by 69%- 86% the difference in CHD mortality between high and low socio-economic groups with smoking cessation and reduction of cholesterol concentration accounting for the largest part of the change18.
While addressing behavioural risk factors can only be a part of the solution to reducing health inequity, it is important to understand the distribution of behavioural risk factors in relation to deprivation if scarce resources for public health interventions are to be used most efficiently to reduce the gap in life-expectancy between the most and least deprived communities. In this study we examined the relationship between area deprivation and the four healthy behaviours, and a summary behaviour score based on these behaviours. We also examined if the association was independent of occupational social class.
METHODS
Study population
The participants were 26,290 men and women aged over 16 years, living in the East of England (population approximately 5.6 million). The East of England Strategic Health Authority is one of 10 Strategic health Authorities in England and covers a wide socioeconomic, urban-rural and ethnic distribution. For the purposes of planning health services, the region is divided into 14 Primary Care Trusts (PCT), and quotas were set for sampling so that at least 1,250 participants were chosen from each PCT. One purpose of the East of England Lifestyle Survey was to compare the 20% most deprived to the 80% least deprived areas within each PCT, hence quotas were set for area deprivation (approximately 40% of the participants were from the most deprived quintile of each PCT in order to obtain sufficient number of participants from the most deprived neighbourhoods). Quotas were also set for age, gender, ethnicity, and working status to provide a representative sample for the entire region.
Procedures
Interviews were conducted by telephone (land-line), using random digit dialling, between 29/10/2008-21/12/2008. A survey questionnaire was developed by regional public health professionals using questions equivalent to previously validated questionnaires used in major national surveys like the Health Survey for England, General Household Survey and the International Physical Activity Questionnaire (IPAQ). Demographic data on age, gender, ethnicity, residential post-code, working status and occupational social class was collected. Health status was assessed by questions on general health (very good, good, fair, bad or very bad) and presence of long term limiting illness or disability. Self-reported height and weight were used to calculate body mass index (BMI= Weight in Kg/ Height in meters2).
Detailed questions on smoking (status- non smoker, past smoker, current smoker, age when first started to smoke, wanting to quit smoking, quit attempts, quantity, frequency and type), alcohol consumption (type, quantity, frequency), fruit and vegetable intake (number of portions eaten on the previous day, and frequency of consuming at least five portions a day over an average week), and physical activity (measured using the IPAQ-http://www.ipaq.ki.se/ipaq.htm) were included. Physical activity energy expenditure was quantified as metabolic equivalent of task (MET) -minutes/week by multiplying the amount of time spent doing an activity per day, number of days it was carried out per week, and metabolic equivalent (MET) score for that activity according to Ainsworth et al19. Participants were categorised as High (meeting any of the following criteria: vigorous-intensity activity on at least 3 days and accumulating at least 1500 MET- minutes/week OR 7 days of any combination of walking, moderate- or vigorous-intensity activities achieving at least 3000 MET- minutes/week), Moderate (meeting any of the following criteria: 3 or more days of vigorous activity of at least 20 minutes per day OR 5 or more days of moderate-intensity activity or walking at least 30 minutes per day OR 5 or more days of any combination of walking, moderate-intensity or vigorous intensity activities achieving at least 600 MET- minutes/week), Low (not meeting any of the above criteria) physical activity.
A healthy lifestyle score was calculated based on the number of four healthy behaviours achieved, as identified in previous studies4. Each of the following behaviours received a score of 1- not smoking, moderate alcohol consumption (1-14 units/week for women and 1-21 units/week for men), high or moderate levels of physical activity, and eating five or more portions of fruit or vegetables on at least 5 days/week. Hence each participant could get a minimum score of zero and maximum score of four.
The residential post-code of each participant was assigned a neighbourhood deprivation score based on the Index of Multiple Deprivation 2007 which combines a number of indicators, chosen to cover a range of economic, social and housing issues, into a single deprivation score for each small area (n= 32,482) in England20. Scores are used to rank small areas, with a high score indicating greater deprivation. Nationally the lowest score is 0.37 (least deprived) and the highest score in 85.46 (most deprived). The lowest score in the East of England is 0.67 (second most affluent nationally) and the highest score is 82.58 (third most deprived nationally). Although the whole range of national deprivation is covered, the average score is 19.45 (median 16.67, sd 12.64), which means that in general the East of England is less deprived than the national average.
Occupational social class was categorised into six classes (based on latest occupation)-Professional, Managerial, Skilled non-manual, Skilled manual, Semi-skilled manual, and Unskilled manual or on state benefit. Employment status was defined as full time employed, part-time employed, retired, and not working. Ethnicity was based on Office of National Statistics (ONS) classifications of 18 different ethnic groups.
Statistical Analyses
The sample was divided into approximate quintiles of area deprivation score and characteristics of participants were compared. A non-parametric test for trend was used to calculate p-values for significant trend across quintiles for categorical variables, and a linear regression model for continuous variables. Multivariable linear regression analyses were performed to examine the association between BMI, height, weight, healthy lifestyle score and neighbourhood deprivation. Multivariable logistic regression analyses were performed to estimate the odds ratio for each healthy behaviour (outcome variable) comparing quintiles of neighbourhood deprivation (exposure variable), with the least deprived quintile as the reference category. In all regression analyses, robust standard errors were calculated to take account of the clustering of individuals within a PCT. The basic model adjusted for age (Model 1), and subsequent models additionally adjusted for gender, ethnicity (Model 2), employment category, and occupational social class (individual level socioeconomic factors-Model 3). We excluded participants with missing data for ethnicity (n=8), employment category (n=7) and occupational social class (n=537) from all models. In order to examine the independent association with individual level socioeconomic status, we fitted a multivariable logistic regression model to examine the risk of healthy behaviour across six occupational social class categories, using the ‘Professional’ category as the reference. All analyses were performed using STATA statistical software, version 10 (STATACORP, College Station, USA).
RESULTS
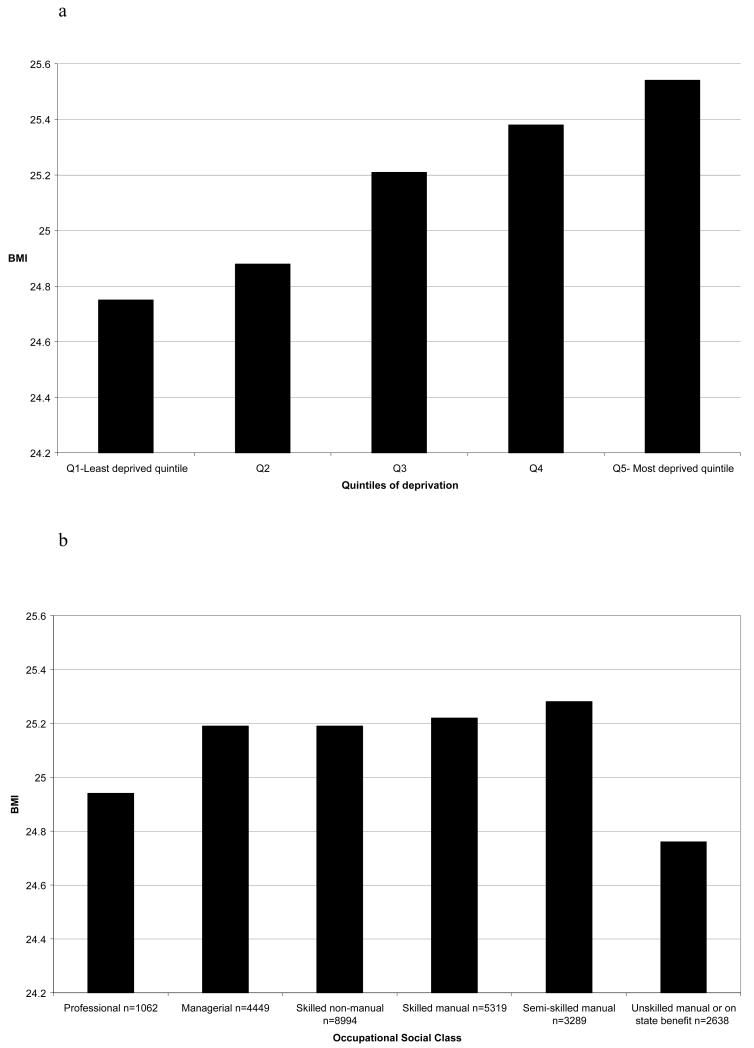
The response rate was 11% and a total of 26,290 interviews were conducted (women n=13,992). Across quintiles of increasing neighbourhood deprivation score, participants were more likely to report that their general health was bad or very bad (7.85% in most deprived quintile versus 3.05% in least deprived quintile) and have a long-term illness or disability that limited activity (20.51% versus 13.05%). Not surprisingly, they were more likely to be unemployed and in semi-skilled or un-skilled occupations (individual-level social economic factors) (Table 1). After adjusting for age, gender, ethnicity and occupational social class, across quintiles of neighbourhood deprivation, participants were shorter (regression coefficient β= −0.30, p<0.0001), heavier (β= 0.39, p<0.0001) and had a higher BMI (β= 0.21, p<0.0001). In contrast with the linear trend of BMI with neighbourhood deprivation, there was no linear trend with occupational social class categories (Figure 1).
Table 1.
Characteristics of 26,290 men and women who participated in the East of England Lifestyle survey (2008) by approximate quintiles of neighbourhood deprivation score (IMD 2007).
| Variablesa | Quintiles of neighbourhood deprivation scoreb | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Q1 (n=5281) IMD score 0.67-8.54 |
Q2 (n=5248) IMD score 8.55-13.52 |
Q3 (n=5248) IMD score 13.53-20.15 |
Q4 (n=5287) IMD score 20.18-29.54 |
Q5 (n=5226) IMD score 29.56-82.58 |
p-trendc | |
| Age in years-mean (sd) | 47.83 (18) | 47.79 (18) | 48.66 (18) | 47.79 (18) | 46.01 (19) | <0.0001 |
|
| ||||||
| Gender | <0.0001 | |||||
| Men n=12298 | 48.91 | 46.82 | 46.28 | 46.70 | 45.16 | |
| Women n=13992 | 51.09 | 53.18 | 53.72 | 53.30 | 54.84 | |
| Ethnicity | <0.0001 | |||||
| White British n=23279 | 91.86 | 91.44 | 90.28 | 87.82 | 81.29 | |
| White other n=1094 | 03.84 | 04.15 | 03.89 | 04.39 | 04.54 | |
| Black and minority ethnicity n=1909 |
04.28 | 04.36 | 05.83 | 07.75 | 14.12 | |
| Self perception of health | <0.0001 | |||||
| Very good/good n=20045 | 81.59 | 79.43 | 75.78 | 74.23 | 70.86 | |
| Fair n=4767 | 15.36 | 16.10 | 18.69 | 19.42 | 21.28 | |
| Bad/very bad n=1430 | 03.05 | 04.47 | 05.54 | 06.35 | 07.85 | |
|
Has long term limiting illness or
disability which limits activity n=4363 |
13.05 | 14.63 | 16.84 | 17.97 | 20.51 | <0.0001 |
| Work category | <0.0001 | |||||
| Full time employed n=13056 | 52.11 | 50.78 | 49.75 | 50.01 | 45.62 | |
| Part-time employed n=2961 | 11.19 | 12.00 | 11.17 | 10.93 | 11.02 | |
| Retired n=5962 | 22.44 | 22.73 | 24.09 | 23.04 | 21.09 | |
| Not working n=4304 | 14.24 | 14.42 | 14.98 | 16.02 | 22.23 | |
| Occupational social class | <0.0001 | |||||
| Managerial or Professional n= 5511 |
31.89 | 24.66 | 20.39 | 16.36 | 11.44 | |
| Skilled manual, clerical, junior | 54.19 | 55.39 | 56.29 | 55.34 | 50.98 | |
| managerial or professional n= 14313 |
||||||
| Semi- un-skilled or on state benefit n=5927 |
12.01 | 17.85 | 21.28 | 26.31 | 35.36 | |
| BMI unadjusted mean (se) | 24.79 (0.12) | 24.90 (0.12) | 25.26 (6.47) | 25.40 (0.09) | 25.40 (0.11) | <0.0001 |
| BMIdmean (se) | 24.75 (0.12) | 24.88 (0.11) | 25.21 (0.12) | 25.38 (0.09) | 25.53 (0.09) | <0.0001 |
| Heightdmean (se) | 169.8 (0.29) | 169.4 (0.13) | 169.2 (0.12) | 169.2 (0.18) | 168.4 (0.17) | <0.0001 |
| Weightd mean (se) | 72.28 (0.31) | 72.27 (0.31) | 73.11 (0.29) | 73.52 (0.25) | 73.58 (0.32) | <0.0001 |
Values are percentages for categorical variables and means (standard deviations or standard errors) for continuous variables.
Each participant was assigned a IMD 2007 score for post-code of residence.
Non-parametric test for trend for categorical variables and linear regression for continuous variables.
BMI, height and weight adjusted for age, sex, ethnicity (18 categories) and occupational social class (6 categories).
Figure 1.
a: Mean Body Mass Index (adjusted for age, sex, ethnicity and occupational social class) across quintiles of neighbourhood deprivation (p for trend 0.001).
b: Mean Body Mass Index (adjusted for age, sex, ethnicity and neighbourhood deprivation score) across occupational social class categories (p for trend =0.230).
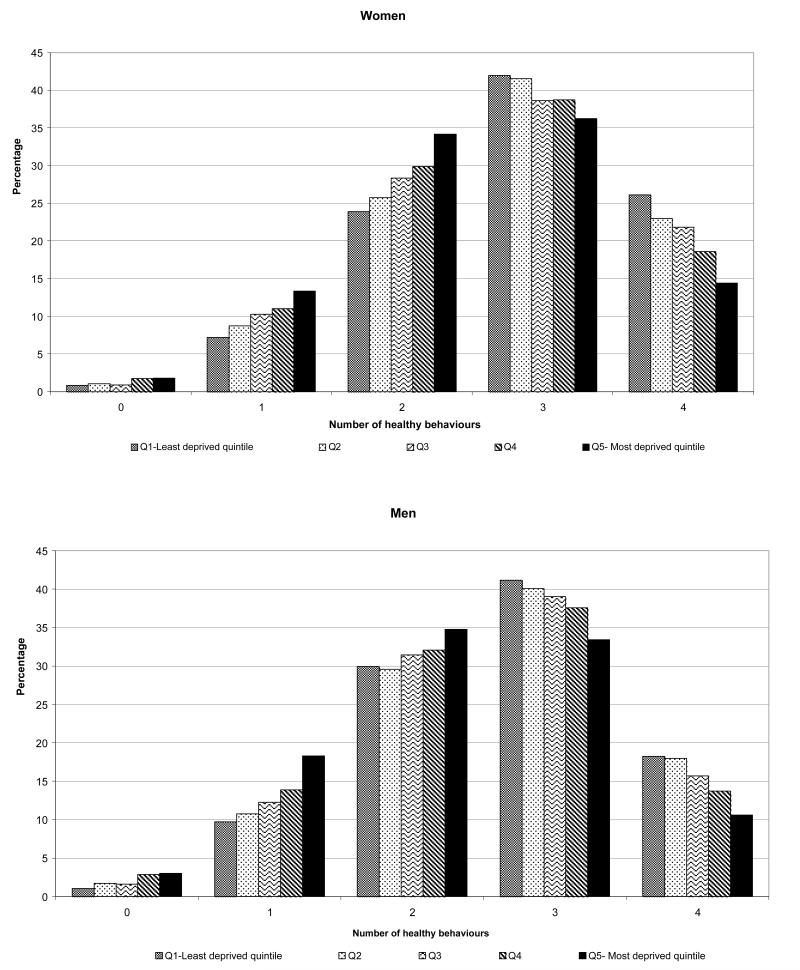
As shown in Table 2, there was a linear gradient across quintiles of deprivation for smoking, alcohol consumption and fruit and vegetable intake (all p for trend <0.0001). For example among more deprived communities, smoking prevalence was higher (27.82% in the most deprived versus 13.54% in the least deprived quintile) and smokers were also more likely to want to quit (68.02% versus 63.92%, although p for linear trend across quintiles did not reach statistical significance). Participants were less likely to consume any alcohol (21.28% versus 8.52% non-drinkers in the most deprived versus the most affluent quintile) and less likely to drink in excess (16.17% versus 23.06% hazardous or harmful drinkers). Consumption of fruits and vegetables was also lower (32.85% versus 45.39% achieving the five-a-day recommendations). Fewer participants in the most deprived quintile achieved all four healthy behaviours (12.69% versus 22.27%) and a greater proportion did not achieve any or achieved only a single healthy behaviour (17.91% versus 9.34%) (Figure 2).
Table 2.
Distribution of four behavioural factors among 26,290 men and women who participated in the East of England Lifestyle survey (2008) by approximate quintiles of neighbourhood deprivation score (IMD 2007).
| Variables Percentagea |
Quintiles of neighbourhood deprivation score | |||||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | p-trend | |
| Smoking b | <0.0001 | |||||
| Yes n=5298 | 13.54 | 16.60 | 19.34 | 23.51 | 27.82 | |
| No n=20987 | 86.42 | 83.40 | 80.64 | 76.45 | 72.81 | |
| Want to quit smoking (among smokers n=5298)c |
0.136 | |||||
| Yes n=3485 | 63.92 | 66.02 | 64.73 | 64.92 | 68.02 | |
| No n=1573 | 31.47 | 29.28 | 31.82 | 30.17 | 20.29 | |
| Alcohol consumption d | <0.0001 | |||||
| Non-drinker n=3489 | 8.52 | 9.95 | 12.73 | 13.94 | 21.28 | |
| Moderate drinker n=16942 | 66.88 | 66.60 | 64.96 | 64.27 | 59.47 | |
| Hazardous drinker n=4022 | 18.10 | 16.63 | 15.63 | 14.34 | 11.77 | |
| Harmful drinker n=1247 | 04.96 | 04.86 | 04.84 | 04.65 | 04.40 | |
|
Consumption of at least five
portions of fruit and vegetables e |
<0.0001 | |||||
| Less than 1 day/week n=3952 | 12.63 | 13.99 | 13.87 | 15.87 | 18.83 | |
| 1-4 days per week n=11777 | 41.81 | 43.27 | 44.34 | 46.66 | 47.91 | |
| 5-7 days/week n=10473 | 45.39 | 42.44 | 41.37 | 37.09 | 32.85 | |
| Physical activity level f | 0.287 | |||||
| High n=11209 | 41.34 | 43.20 | 41.94 | 43.71 | 43.00 | |
| Moderate n=8896 | 35.81 | 34.05 | 34.26 | 32.48 | 32.59 | |
| Low n=5875 | 21.72 | 21.91 | 22.58 | 22.60 | 22.92 | |
|
| ||||||
| Healthy Lifestyle scoreg n=25739 | ||||||
| Healthy lifestyle score –mean (se) | 2.76 (0.01) |
2.70 (0.01) |
2.63 (0.03) |
2.54 (0.02) |
2.41 (0.04) |
<0.0001 |
| Healthy lifestyle score –mean (se) adjusted for age and sex |
2.76 (0.01) |
2.70 (0.01) |
2.63 (0.03) |
2.54 (0.02) |
2.40 (0.04) |
<0.0001 |
| Healthy lifestyle score –mean (se) adjusted for age, sex, ethnicity and occupational social class |
2.71 (0.01) |
2.67 (0.02) |
2.62 (0.02) |
2.56 (0.07) |
2.49 (0.01) |
<0.0001 |
| Mean healthy lifestyle score adjusted for age and sex across occupational social class categories |
||||||
| Professional n=1062 | 2.91 | 2.87 | 2.81 | 2.75 | 2.65 | |
| Managerial n=4449 | 2.89 | 2.84 | 2.79 | 2.72 | 2.62 | |
| Skilled Non-Manual n=8994 | 2.75 | 2.71 | 2.66 | 2.59 | 2.49 | |
| Skilled Manual n=5319 | 2.70 | 2.66 | 2.61 | 2.54 | 2.44 | |
| Semi-Skilled Manual n=3289 | 2.61 | 2.57 | 2.51 | 2.44 | 2.35 | |
| Unskilled manual/ on state benefit n=2638 |
2.41 | 2.37 | 2.31 | 2.25 | 2.15 | |
Percentages may not add up to 100% due to missing data.
Answer to question ‘Do you smoke cigarettes, roll-ups, cigars, or a pipe at all nowadays?’
Current smokers asked ‘would you like to give up smoking altogether?’
Non-drinker – O units/ week, Moderate drinker 1-21 units/week for men and 1-14 units/week for women, Hazardous drinker 22-50 units/week for men and 15-35 units/week for women, Harmful drinker >51 units/week for men and >36 units /week for women
Answer to the question ‘Can you tell me how often, on average, you eat five portions of fruit or vegetables a day?’
Physical activity measured using IPAQ.
Score calculated based on number of the 4 healthy behaviours achieved: Not current smoker, Moderate alcohol consumption, consuming five portions of fruit and vegetables on at least five days a week, and high or moderate levels of physical activity. All scores calculated using robust standard errors to account for clustering of individuals within a PCT. Participants with missing data on ethnicity and occupational social class were excluded.
Figure 2.
Percentages of women and men in each neighbourhood deprivation quintile achieving none, 1, 2, 3 or 4 healthy behaviours.
Across quintiles of increasing neighbourhood deprivation, participants were more likely to smoke and less likely to consume five portions of fruit and vegetables on five or more days of the week (least deprived versus most deprived quintile- odds ratios for not smoking 0.38 [0.33 to 0.42]; and fruit and vegetable consumption 0.60 [0.55 to 0.66]; adjusted for age, sex, and ethnicity; p for trend <0.0001). The association was attenuated but remained significant when additionally adjusted for individual socioeconomic factors (employment and occupational social class). This suggests that the effect of neighbourhood deprivation is present over and above the effect of occupational social class (Table 3).
Table 3a.
Adjusted odds ratios for behavioural factors among 25,739 men and women who participated in the East of England Lifestyle survey (2008) by approximate quintiles of neighbourhood deprivation score (IMD 2007).
| Quintiles of neighbourhood deprivation score | ||||||
|---|---|---|---|---|---|---|
| Odds Ratiosa | Q1 | Q2 | Q3 | Q4 | Q5 | p-trendb |
| Not Smoking | ||||||
| Model 1 | 1 | 0.79 [0.71-0.88]*** | 0.64 [0.56-0.73]*** | 0.51 [0.44-0.58]*** | 0.41 [0.34-0.50]*** | <0.0001 |
| Model 2 | 1 | 0.78 [0.71-0.87]*** | 0.63 [0.55-0.71]*** | 0.49 [0.43-0.55]*** | 0.38 [0.33-0.42]*** | <0.0001 |
| Model 3 | 1 | 0.83 [0.74-0.92]** | 0.69 [0.61-0.77]*** | 0.55 [0.49-0.62]*** | 0.45 [0.41-0.51]*** | <0.0001 |
|
Consuming five portions of fruits and vegetables on at
least 5 days/week |
||||||
| Model 1 | 1 | 0.88 [0.81-0.97]* | 0.84 [0.75-0.93]** | 0.71 [0.66-0.76]*** | 0.60 [0.54-0.66]*** | <0.0001 |
| Model 2 | 1 | 0.87 [0.79-0.96]** | 0.83 [0.74-0.92]** | 0.70 [0.65-0.75]*** | 0.60 [0.55-0.66]*** | <0.0001 |
| Model 3 | 1 | 0.91 [0.83-0.99]* | 0.89 [0.80-0.97]* | 0.77 [0.72-0.82]*** | 0.70 [0.64-0.76]*** | <0.0001 |
| High or moderate levels of physical activity | ||||||
| Model 1 | 1 | 1.00 [0.94-1.07] | 0.97 [0.87-1.08] | 0.96 [0.87-1.05] | 0.90 [0.80-1.01] | 0.487 |
| Model 2 | 1 | 1.01 [0.94-1.07] | 0.99 [0.89-1.10] | 0.98 [0.90-1.08] | 0.98 [0.91-1.04] | 0.949 |
| Model 3 | 1 | 1.02 [0.96-1.09] | 1.02 [0.92-1.13] | 1.03 [0.94-1.13] | 1.06 [0.99-1.12] | 0.254 |
| Moderate alcohol consumption c | ||||||
| Model 1 | 1 | 0.99 [0.91-1.09] | 0.92 [0.82-1.03] | 0.90 [0.83-0.98]* | 0.75 [0.60-0.79]* | 0.045 |
| Model 2 | 1 | 0.98 [0.89-1.08] | 0.94 [0.85-1.03] | 0.93 [0.87-1.00] | 0.86 [0.82-0.90]*** | <0.0001 |
| Model 3 | 1 | 0.99 [0.90-1.10] | 0.95 [0.86-1.06] | 0.96 [0.88-1.04] | 0.91 [0.86-0.96]*** | 0.0002 |
|
Not exceeding recommended limits for alcohol
consumption d |
||||||
| Model 1 | 1 | 1.09 [0.98-1.21] | 1.16 [1.03-1.31]* | 1.27 [1.16-1.38]*** | 1.57 [1.28-1.92]*** | <0.0001 |
| Model 2 | 1 | 1.07 [0.97-1.19] | 1.12 [0.99-1.26] | 1.20 [1.11-1.30]*** | 1.37 [1.28-1.48]*** | <0.0001 |
| Model 3 | 1 | 1.04 [0.94-1.16] | 1.07 [0.95-1.20] | 1.13 [1.05-1.21]* | 1.23 [1.15-1.32]*** | <0.0001 |
P <0.05
P<0.01
P <0.001 for significant odds ratios compared to the first quintile for IMD score (least deprived).
Model 1-adjusted for age. Model 2- adjusted for age, gender, ethnicity (18 categories). Model 3- Model 2+ adjusted for work category (four categories) and occupational social class (six categories).
Test for linear trend across quintiles of deprivation using regression model.
Moderate alcohol consumption – 1-21 units per week for men and 1-14 units per week for women.
Alcohol consumption less than 22 units per week for men and 15 units per week for women (includes non-drinkers).
Table 3b.
Odds ratios for behavioural risk factors by occupational social class adjusted for age, sex, ethnicity, work category, and neighbourhood deprivation score (IMD 2007).
| Odds ratios | Occupational social class | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Professional | Managerial | Skilled non-manual | Skilled manual | Semi-skilled manual | Un-skilled manual or on state benefit |
p-trend | |
| Not Smoking | 1 | 0.86 [0.63-1.18] | 0.62 [0.45-0.84]** | 0.50 [0.37-0.68]*** | 0.43 [0.33-0.56]*** | 0.33 [0.24-0.46]*** | <0.0001 |
|
Consuming five portions of
fruits and vegetables on at least 5 days/week |
1 | 0.83 [0.75-0.93]** | 0.63 [0.57-0.70]*** | 0.56 [0.50-0.62]*** | 0.46 [0.41-0.53]*** | 0.50 [0.44-0.57]*** | <0.0001 |
|
High or moderate levels of
physical activity |
1 | 0.90 [0.77-1.04] | 0.82 [0.70-0.96]* | 0.90 [0.79-1.03] | 0.85 [0.72-1.00] | 0.58 [0.48-0.69]*** | <0.0001 |
| Moderate alcohol consumption | 1 | 1.22 [1.06-1.42]** | 1.20 [1.06-1.37]** | 1.16 [1.00-1.33]* | 1.12 [0.97-1.30] | 0.81 [0.71-0.93]** | <0.0001 |
|
Not exceeding recommended
limits for alcohol consumption |
1 | 1.34 [1.14-1.56]*** | 1.45 [1.27-1.65]*** | 1.55 [1.36-1.76]*** | 1.77 [1.53-2.04]*** | 1.94 [1.53-2.48]*** | <0.0001 |
P <0.05
P<0.01
P <0.001 for significant odds ratios compared to Professional occupation.
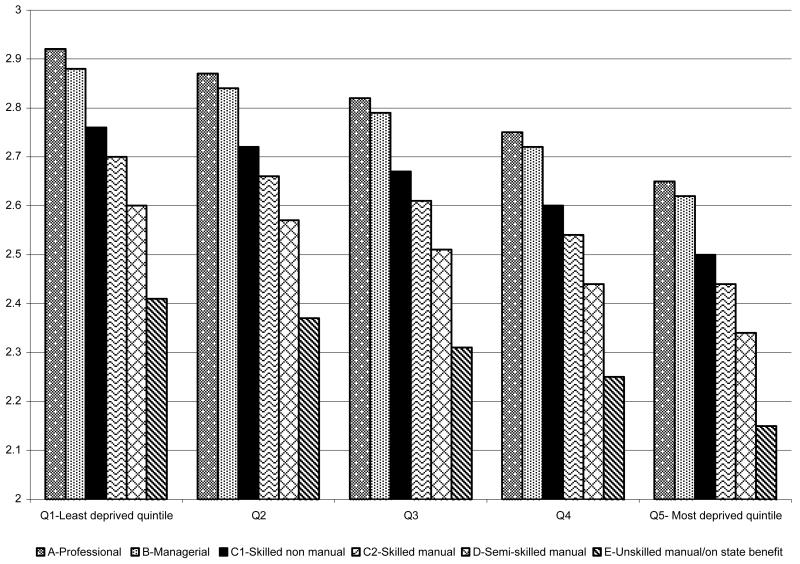
The average healthy lifestyle score was lower across increasing quintiles of neighbourhood deprivation even after adjusting for occupational social class (p for trend <0.0001). Age and sex adjusted mean healthy lifestyle scores were 2.65 for professionals in the most deprived neighbourhood quintile which was comparable to the mean score for semi-skilled manual workers in the least deprived quintile (score 2.61). As shown in Figure 3, there was a linear trend for the summary healthy lifestyle score across the neighbourhood deprivation quintiles and across the six occupational categories (both p for trend <0.0001) with no significant interaction.
Figure 3.
Mean Healthy lifestyle score across quintiles of neighbourhood deprivation and six categories of occupational social class (adjusted for age and sex; p for trend <0.0001).
DISCUSSION
Main Findings of this study
In this large population based study, increasing neighbourhood deprivation was associated with a higher BMI, shorter adult height (which may suggest long-term deprivation), poorer perception of health, and more long-term limiting illness or disability. Across quintiles of increasing neighbourhood deprivation, participants were more likely to smoke and less likely to consume five portions of fruits and vegetables on at least five day a week. With excess alcohol consumption, the pattern was reversed and across quintiles of increasing neighbourhood deprivation, participants were less likely to exceed the recommendations for alcohol intake (22 units per week for men and 15 units per week for women). Although there was a trend for physical activity with occupational social class, this trend was not present for neighbourhood deprivation. The inverse association between neighbourhood deprivation and the summary healthy lifestyle score was independent of occupational social class.
What is already known on this topic
There is overwhelming evidence that modifiable behavioural risk factors such as smoking, diet, alcohol and physical activity influence health. Khaw et al examined the relationship between four health behaviours: not smoking, not physically inactive, moderate alcohol intake (1-14 units a week), and Vitamin C levels > 50 mmol/l indicating at least five servings of fruit and vegetables every day4. Adjusted for age, sex, BMI and social class, relative risks for mortality were 1.77 for smoker versus non-smoker, 1.44 for Vitamin C levels < 50 mmol/l, 1.26 for alcohol intake <1 or > 14 units per week, and 1.24 for physically inactive versus not inactive. The mortality risk for those with four compared to zero health behaviours was equivalent to being 14 years younger4. A subsequent paper on the same cohort quantified the association of the four health behaviours with incidence of stroke. In fully adjusted models, the relative risks for incident stroke were 1.69 for smoker versus non-smoker, 1.39 for Vitamin C levels < 50 mmol/l, 1.28 for alcohol intake <1 or > 14 units per week, and 1.29 for physically inactive versus not inactive5. These data suggest that successfully promoting the four healthy behaviours can significantly reduce mortality and morbidity.
A recent review to map out the area effects on health identified 86 studies published between July 1998 and December 2005. Most studies found an area (contextual) effect independently of individual level socioeconomic (compositional) effects21. Most studies have examined associations between area deprivation and health outcomes such as cardiovascular disease22, diabetes23, cognitive impairment24, quality of life25, disability26, self rated health27 and mortality28-31 but few have studied the proximal determinants of health outcomes such as behavioural risk factors and obesity which could be mediating the association23,32. In particular very few studies have examined the interaction between area and individual socioeconomic effects33. In one study in Scotland the association between a ‘bad’ diet and area deprivation was present only among affluent households34 and in another study neighbourhood deprivation was associated with higher body mass index in women but not men, after controlling for individual factors28.
Three studies found that neighbourhood deprivation was associated with smoking35-37. Numerous studies have assessed the contribution of smoking to the socioeconomic differences in mortality and estimates vary from 24% to over 50%38-40. Neighbourhood deprivation has also been associated with lower plasma carotenoid and vitamin C levels (both markers of fruit and vegetable intake)41,42. Pollack et al found that although alcohol availability was concentrated in the most deprived neighbourhoods, adults in least deprived neighbourhoods were most likely to be heavy drinkers43. At an individual level, excess alcohol intake was associated with increasing education, wealth and subjective social status44.
The association between physical activity and area neighbourhood deprivation is less clear with one study showing that area deprivation was associated with increased sedentary behaviour (measured as TV viewing and screen-based recreation)45, and another study showing that area deprivation was associated with less moderate or vigorous physical activity among older women46. One study found that area deprivation was associated with smoking, less fruit and vegetable intake and exercise habits47.
What this study adds
This study showed that smoking and a poor diet are the most significant modifiable behavioural risk factors that should be targeted by public health interventions aimed at reducing health inequalities associated with neighbourhood deprivation. More research is needed to investigate the association between drinking behaviour (binge, moderate, hazardous, and harmful drinking) and deprivation so that public health messages regarding moderate drinking can be tailored appropriately. In addition to individual level socioeconomic factors, features in the neighbourhood (such as housing, shops, recreational facilities, the built environment, reputation of the area, peer pressure, isolation from people with healthy behaviours, access to health promotion messages and services) also contribute to unhealthy lifestyles that lead to poorer health. Since there is a neighbourhood effect beyond the individual effect, strategies to reduce inequalities could combine individual level and neighbourhood level approaches. These could include providing a wider range of healthy options to those living in more deprived neighbourhoods.
Individuals in deprived neighbourhoods achieved a shorter adult height and this may suggest that they suffer worse health from childhood; hence interventions could target early life and childhood and not focus solely on the health of adults, as suggested by other studies as well48.
Limitations of this study
We cannot rule out response bias due to the method of using random digit dialling since only 83% of UK households have a landline. However, this is unlikely to affect the association between behavioural risk factors and deprivation and the pattern of variation is likely to be a good reflection of the true pattern. We also tried to ensure the sample was representative of the population by setting quotas (in this case, on age, gender, employment status, ethnicity, and neighbourhood deprivation) within each PCT. Although the response rate was low (11%), the quotas on neighbourhood deprivation were set to boost the response from people living in the most deprived areas within each PCT, in order to better reflect the more deprived population (who traditionally are less likely to have a landline)49.
Self-reported measures may result in biased reporting to socially acceptable behaviours and this is a limitation of all surveys. If individuals in more deprived neighbourhood were more likely to report healthy behaviours, this would attenuate the association and vice versa. When self reported height and weight data collected in this survey were compared to objectively measured height and weight data from Health Survey for England, we found that height was over estimated and weight was under estimated, resulting in lower BMI values50. There is no reason to believe that there was a systematic bias in underreporting by neighbourhood deprivation levels, hence any errors would attenuate the association and the true association is likely to be stronger. We have used recommendations for weekly alcohol consumption although these have been replaced by daily recommendations to identify binge drinking patterns. We were not able to calculate daily alcohol consumption based on the data we gathered.
The strengths of this study also merit consideration. The main strength was that a combination of individual and neighbourhood socioeconomic factors was used. Previously validated questions were used to gather comprehensive data on the four important behaviours that are known to have a significant impact on morbidity and mortality. This was a large population based survey including participants from diverse socioeconomic backgrounds and ethnicity. Although the East of England is less deprived on average than England, because quotas were set to interview 40% of the participants from the most deprived quintile of each PCT, the complete ranges of area deprivation scores for the country were captured (minimum IMD 2007 score 0.67 and maximum 82.58) making the findings generalisable to the rest of the country.
Acknowledgements
We would like to thank all the participants and Ipsos MORI who carried out the survey. Special thanks also to Liam Cahill, Lee Whitehead and Clare Humphreys who contributed to the survey and to Stephen Sharp for expert statistics advice.
Funding
This work was supported by the East of England Strategic Health Authority and Primary Care Trusts within the region. RL is supported by a MRC Health Services and Health of the Public Research Fellowship and is in receipt of a Sackler fellowship.
Footnotes
Publisher's Disclaimer: This is a pre-copy-editing, author-produced PDF of an article accepted for publication in the Journal of Public Health following peer review. The definitive publisher-authenticated version J Public Health (2011) 33 (2): 234-245 is available online at: http://jpubhealth.oxfordjournals.org/content/33/2/234.long
Conflict of interest
None declared.
Reference List
- (1).Shohaimi S, Welch A, Bingham S, et al. Residential area deprivation predicts fruit and vegetable consumption independently of individual educational level and occupational social class: a cross sectional population study in the Norfolk cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk) Journal of Epidemiology and Community Health. 2004;58:686–691. doi: 10.1136/jech.2003.008490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Deans KA, Bezlyak V, Ford I, et al. Differences in atherosclerosis according to area level socioeconomic deprivation: cross sectional, population based study. BMJ. 2009;339:b4170. doi: 10.1136/bmj.b4170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).Sundquist J, Malmstrom M, Johansson SE. Cardiovascular risk factors and the neighbourhood environment: a multilevel analysis. Int J Epidemiol. 1999;28:841–845. doi: 10.1093/ije/28.5.841. [DOI] [PubMed] [Google Scholar]
- (4).Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: The EPIC-Norfolk prospective population study. Plos Medicine. 2008;5:518. doi: 10.1371/journal.pmed.0050012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Myint PK, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Combined effect of health behaviours and risk of first ever stroke in 20 040 men and women over 11 years’ follow-up in Norfolk cohort of European Prospective Investigation of Cancer (EPIC Norfolk): prospective population study. British Medical Journal. 2009:338. doi: 10.1136/bmj.b349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (6).Cesaroni G, Agabiti N, Forastiere F, Perucci CA. Socioeconomic Differences in Stroke Incidence and Prognosis Under a Universal Healthcare System. Stroke. 2009;40:2812–2819. doi: 10.1161/STROKEAHA.108.542944. [DOI] [PubMed] [Google Scholar]
- (7).Brunner E, Shipley M, Spencer V, et al. Social Inequality in Walking Speed in Early Old Age in the Whitehall II Study. Journals of Gerontology Series A-Biological Sciences and Medical Sciences. 2009;64:1082–1089. doi: 10.1093/gerona/glp078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Christiansen T, Kooiker S. Inequalities in health: evidence from Denmark of the interaction of circumstances and health-related behaviour. Scandinavian Journal of Public Health. 1999;27:181–188. [PubMed] [Google Scholar]
- (9).Clarke R, Emberson J, Fletcher A, Breeze E, Marmot M, Shipley MJ. Life expectancy in relation to cardiovascular risk factors: 38 year follow-up of 19000 men in the Whitehall study. British Medical Journal. 2009:339. doi: 10.1136/bmj.b3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Drukker M, van Os J. Mediators of neighbourhood socioeconomic deprivation and quality of life. Social Psychiatry and Psychiatric Epidemiology. 2003;38:698–706. doi: 10.1007/s00127-003-0690-8. [DOI] [PubMed] [Google Scholar]
- (11).Jones S, Johansen A, Brennan J, Butler J, Lyons RA. The effect of socioeconomic deprivation on fracture incidence in the United Kingdom. Osteoporosis International. 2004;15:520–524. doi: 10.1007/s00198-003-1564-3. [DOI] [PubMed] [Google Scholar]
- (12).Kondo N, Kawachi I, Hirai H, et al. Relative deprivation and incident functional disability among older Japanese women and men: prospective cohort study. Journal of Epidemiology and Community Health. 2009;63:461–467. doi: 10.1136/jech.2008.078642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Larranaga I, Arteagoitia JM, Rodriguez JL, Gonzalez F, Esnaola S, Pinies JA. Socio-economic inequalities in the prevalence of Type 2 diabetes, cardiovascular risk factors and chronic diabetic complications in the Basque Country, Spain. Diabetic Medicine. 2005;22:1047–1053. doi: 10.1111/j.1464-5491.2005.01598.x. [DOI] [PubMed] [Google Scholar]
- (14).Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S, Commission Social DH. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- (15).Acheson D. Independent Inquiry into Inequalites in Health. Department of Health; 1998. [Google Scholar]
- (16).Department of Health . Tackling health inequalities: A Programme for Action. [accessed March 2010]. 2003. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4008268. [Google Scholar]
- (17).Marmot M. Strategic Review of Health Inequalities in England Post 2010. [accessed March 2010]. 2010. http://www.ucl.ac.uk/gheg/marmotreview/ [Google Scholar]
- (18).Kivimaki M, Shipley MJ, Ferrie JE, et al. Best-practice interventions to reduce socioeconomic inequalities of coronary heart disease mortality in UK: a prospective occupational cohort study. Lancet. 2008;372:1648–1654. doi: 10.1016/S0140-6736(08)61688-8. [DOI] [PubMed] [Google Scholar]
- (19).Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of Physical Activities: an update of activity codes and MET intensities. Medicine and Science in Sports and Exercise. 2000;32:S498–S516. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- (20).UK Local government, Communities and Neighbourhood . IMD 2007. [accessed March 2010]. 2007. http://www.communities.gov.uk/communities/neighbourhoodrenewal/deprivation/deprivation07/ [Google Scholar]
- (21).Riva Mn, Gauvin L, Barnett TA. Toward the next generation of research into small area effects on health: a synthesis of multilevel investigations published since July 1998. Journal of Epidemiology and Community Health. 2007;61:853–861. doi: 10.1136/jech.2006.050740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Roux AVD, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. New England Journal of Medicine. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- (23).Krishnan S, Cozier YC, Rosenberg L, Palmer JR. Socioeconomic Status and Incidence of Type 2 Diabetes: Results From the Black Women’s Health Study. Am J Epidemiol. 2010;171:564–570. doi: 10.1093/aje/kwp443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Basta NE, Matthews FE, Chatfield MD, Brayne C, MRC CFAS. Community-level socio-economic status and cognitive and functional impairment in the older population. Eur J Public Health. 2008;18:48–54. doi: 10.1093/eurpub/ckm076. [DOI] [PubMed] [Google Scholar]
- (25).Breeze E, Jones DA, Wilkinson P, et al. Area deprivation, social class, and quality of life among people aged 75 years and over in Britain. Int J Epidemiol. 2005;34:276–283. doi: 10.1093/ije/dyh328. [DOI] [PubMed] [Google Scholar]
- (26).Schmitz N, Nitka D, Gariepy G, et al. Association between neighborhood-level deprivation and disability in a community sample of people with diabetes. Diabetes Care. 2009;32:1998–2004. doi: 10.2337/dc09-0838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (27).Cummins S, Stafford M, Macintyre S, Marmot M, Ellaway A. Neighbourhood environment and its association with self rated health: evidence from Scotland and England. J Epidemiol Community Health. 2005;59:207–213. doi: 10.1136/jech.2003.016147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Smith GD, Hart C, Watt G, Hole D, Hawthorne V. Individual social class, area-based deprivation, cardiovascular disease risk factors, and mortality: the Renfrew and Paisley Study. Journal of Epidemiology and Community Health. 1998;52:399–405. doi: 10.1136/jech.52.6.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Borrell LN, ez Roux AV, Rose K, Catellier D, Clark BL. Neighbourhood characteristics and mortality in the Atherosclerosis Risk in Communities Study. Int J Epidemiol. 2004;33:398–407. doi: 10.1093/ije/dyh063. [DOI] [PubMed] [Google Scholar]
- (30).Bosma H, ke van de Mheen H, Borsboom GJJM, Mackenbach JP. Neighborhood Socioeconomic Status and All-Cause Mortality. Am J Epidemiol. 2001;153:363–371. doi: 10.1093/aje/153.4.363. [DOI] [PubMed] [Google Scholar]
- (31).Turrell G, Kavanagh A, Draper G, Subramanian SV. Do places affect the probability of death in Australia? A multilevel study of area-level disadvantage, individual-level socioeconomic position and all-cause mortality, 1998- 2000. Journal of Epidemiology and Community Health. 2007;61:13–19. doi: 10.1136/jech.2006.046094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Stringhini S, Sabia S, Shipley M, et al. Association of Socioeconomic Position With Health Behaviors and Mortality. JAMA. 2010;303:1159–1166. doi: 10.1001/jama.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (33).Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Social Science & Medicine. 2002;55:125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- (34).Ecob R, Macintyre S. Small area variations in health related behaviours; do these depend on the behaviour itself, its measurement, or on personal characteristics? Health Place. 2000;6:261–274. doi: 10.1016/s1353-8292(00)00008-3. [DOI] [PubMed] [Google Scholar]
- (35).van Lenthe FJ, Mackenbach JP. Neighbourhood and individual socioeconomic inequalities in smoking: the role of physical neighbourhood stressors. Journal of Epidemiology and Community Health. 2006;60:699–705. doi: 10.1136/jech.2005.043851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Kleinschmidt I, Hills M, Elliott P. Smoking behaviour can be predicted by neighbourhood deprivation measures. Journal of Epidemiology and Community Health. 1995;49:S72–S77. doi: 10.1136/jech.49.suppl_2.s72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).Shohaimi S, Luben R, Wareham N, et al. Residential area deprivation predicts smoking habit independently of individual educational level and occupational social class. A cross sectional study in the Norfolk cohort of the European Investigation into Cancer (EPIC-Norfolk) Journal of Epidemiology and Community Health. 2003;57:270–276. doi: 10.1136/jech.57.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Jha P, Peto R, Zatonski W, Boreham J, Jarvis MJ, Lopez AD. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet. 2006;368:367–370. doi: 10.1016/S0140-6736(06)68975-7. [DOI] [PubMed] [Google Scholar]
- (39).van Rossum CTM, Shipley MJ, van de Mheen H, Grobbee DE, Marmot MG. Employment grade differences in cause specific mortality. A 25 year follow up of civil servants from the first Whitehall study. Journal of Epidemiology and Community Health. 2000;54:178–184. doi: 10.1136/jech.54.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (40).Marmot M. Smoking and inequalities. Lancet. 2006;368:341–342. doi: 10.1016/S0140-6736(06)68976-9. [DOI] [PubMed] [Google Scholar]
- (41).Shohaimi S, Bingham S, Welch A, et al. Occupational social class, educational level and area deprivation independently predict plasma ascorbic acid concentration: a cross-sectional population based study in the Norfolk cohort of the European Prospective Investigation into Cancer (EPIC-Norfolk) European Journal of Clinical Nutrition. 2004;58:1432–1435. doi: 10.1038/sj.ejcn.1601979. [DOI] [PubMed] [Google Scholar]
- (42).Stimpson JP, Nash AC, Ju H, Eschbach K. Neighborhood deprivation is associated with lower levels of serum carotenoids among adults participating in the third national health and nutrition examination survey. Journal of the American Dietetic Association. 2007;107:1895–1902. doi: 10.1016/j.jada.2007.08.016. [DOI] [PubMed] [Google Scholar]
- (43).Pollack CE, Cubbin C, Ahn D, Winkleby M. Neighbourhood deprivation and alcohol consumption: does the availability of alcohol play a role? Int J Epidemiol. 2005;34:772–780. doi: 10.1093/ije/dyi026. [DOI] [PubMed] [Google Scholar]
- (44).Shankar A, McMunn A, Steptoe A. Health-Related Behaviors in Older Adults: Relationships with Socioeconomic Status. American Journal of Preventive Medicine. 2010;38:39–46. doi: 10.1016/j.amepre.2009.08.026. [DOI] [PubMed] [Google Scholar]
- (45).Stamatakis E, Hillsdon M, Mishra G, Hamer M, Marmot M. Television viewing and other screen-based entertainment in relation to multiple socioeconomic status indicators and area deprivation: the Scottish Health Survey 2003. Journal of Epidemiology and Community Health. 2009;63:734–740. doi: 10.1136/jech.2008.085902. [DOI] [PubMed] [Google Scholar]
- (46).Hillsdon M, Lawlor DA, Ebrahim S, Morris JN. Physical activity in older women: associations with area deprivation and with socioeconomic position over the life course: observations in the British Women’s Heart and Health Study. Journal of Epidemiology and Community Health. 2008;62:344–350. doi: 10.1136/jech.2006.058610. [DOI] [PubMed] [Google Scholar]
- (47).Amuzu A, Carson C, Watt HC, Lawlor DA, Ebrahim S. Influence of area and individual lifecourse deprivation on health behaviours: findings from the British Women’s Heart and Health Study. European Journal of Cardiovascular Prevention & Rehabilitation. 2009;16:169–173. doi: 10.1097/HJR.0b013e328325d64d. [DOI] [PubMed] [Google Scholar]
- (48).Hertzman C, Siddiqi A, Hertzman E, et al. Bucking the inequality gradient through early child development. BMJ. 2010;340:c468. doi: 10.1136/bmj.c468. [DOI] [PubMed] [Google Scholar]
- (49).Blumberg SJ, Luke JV. Reevaluating the need for concern regarding noncoverage bias in landline surveys. Am J Public Health. 2009;99:1806–1810. doi: 10.2105/AJPH.2008.152835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (50).Humphreys C, Walford H, Flowers J. [accessed March 2010];East of England Lifestyle Survey- supporting document. 2008 2008 http://www.erpho.org.uk/Download/Public/18684/1/2008%20East%20of%20England%20Lifestyle%20Survey%20-%20supporting%20document%20v2.docx. Eastern Region Public Health Observatory. [Google Scholar]