Abstract
BACKGROUND
In the treatment of Graves’ ophthalmopathy, rectus muscle resections generally are avoided because of the concern of reaggravating inflammation and creating excessive extraocular muscle restriction. In patients with large-angle strabismus and in patients with residual strabismus after maximal recession surgery, however, rectus muscle resection may be considered. We report a series of 8 patients with Graves’ ophthalmopathy who underwent rectus muscle resections.
METHODS
The records of 270 patients with Graves’ ophthalmopathy who had undergone strabismus surgery were retrospectively reviewed. Data from subjects who had undergone rectus muscle resections were collected, including age at surgery, duration of disease, duration of diplopia, previous eye or strabismus surgeries, history of radioactive iodine or corticosteroid treatment, current thyroid medications, current use of corticosteroids, tobacco use, and signs and symptoms used to diagnose Graves’ ophthalmopathy.
RESULTS
Eight patients (5 females) were identified (mean age, 51.1 ± 17.6 years). Preoperatively, 4 patients had a horizontal deviation and 4 patients had both horizontal and vertical deviations in primary gaze. Mean preoperative horizontal deviation was 27.9Δ ± 15.2Δ and mean vertical deviation was 6.3Δ ± 5.4Δ. At final follow-up examination, 7 patients were orthotropic in primary gaze; 1 patient had a larger deviation from slippage as the result of a broken suture within the first postoperative week. None of the patients were overcorrected or developed atypical inflammation.
CONCLUSIONS
In this series, patients with Graves’ ophthalmology were successfully treated with the use of rectus muscle resections as part of the surgical plan. Careful ocular motility assessment and patient selection is critical if this option is contemplated.
Strabismus occurs in 17%–51% of patients with Graves’ ophthalmopathy1–4 and is most commonly secondary to extraocular muscle restriction from inflammatory and fibrotic changes. Surgical treatment of these patients typically involves recession rather than resection of the affected muscles5,6 because of concern for severe inflammation and increased restriction of already-tight extraocular muscles. However, in certain cases, resections must be considered: functionally monocular patients who refuse bilateral surgery, patients with residual under-corrections after maximal rectus muscle recessions, and patients with a residual deviation and no restriction to ocular rotations. The purpose of this study was to report a series of patients with Graves’ ophthalmopathy in whom resections of extraocular rectus muscles were performed.
Subjects and Methods
This study was approved by the University of California, Los Angeles Institutional Review Board and conformed to the requirements of the U.S. Health Insurance Portability and Accountability Act. The records of 270 patients with Graves’ ophthalmopathy who had undergone strabismus surgery seen in the ocular motility and oculoplastics clinics at Jules Stein Eye Institute between 1993 and 2012 were retrospectively reviewed.
Data from all patients who had undergone rectus muscle resections were collected. Four different eye muscle specialists performed the surgeries with adjustable sutures using the bow tie technique.7 Preoperative data were collected, including age at resection, duration of Graves’ disease, duration of diplopia, previous eye or strabismus surgeries, history of radioactive iodine or corticosteroid treatment, current thyroid medications, current use of corticosteroids, tobacco use, and signs and symptoms used to diagnose Graves’ ophthalmopathy.
All subjects underwent complete ophthalmologic examinations, including extensive ocular motility testing. Ocular alignment was assessed by the use of cover-uncover and alternate prism cover testing at distance (20 feet) in the cardinal gaze positions. Ocular alignment at near was assessed at 14 inches. In patients with poor visual acuity, corneal light reflex combined with prisms was used to assess ocular alignment.8,9 All motor evaluations were performed using spectacle correction. Ocular ductions were measured using a standard 4-point scale.10 Torsional deviations were assessed with double Maddox rods.11 Stereoacuity at near was tested using the standard Titmus test (Stereo Optical Co Inc, Chicago, IL).
External examinations consisted of a description of the upper and lower eyelid position, and all patients were examined for orbital and ocular signs of inflammation, including corneal staining, conjunctival injection, chemosis, and proptosis.
The following surgical data were collected: intraoperative passive forced duction testing using a qualitative scale12; amount of muscle resected, muscle(s) operated on; use of adjustable suture; and use of perioperative steroids, including route and dose.
Postoperative measurements of horizontal, vertical, and torsional deviations were collected at day 1, postoperative weeks 6–10, and at the most recent available examination or the last examination before additional surgery was performed. Complications and additional eye and strabismus surgeries were noted.
The Fisher exact test was used to assess for an association between successful strabismus surgery (orthotropia in primary gaze) and history of treatment with corticosteroids, cigarette use, history of radioactive iodine treatment and use of postoperative corticosteroids, with a P value of <0.05 considered statistically significant.
Results
A total of 8 patients (5 females) were included in the study. Mean age at time of surgery was 51.1 ± 17.6 years. Graves’ disease data, preoperative clinical findings, and surgical and postoperative data for all of the patients are provided in Tables 1 and 2. Duration of Graves’ disease before resection ranged from 1 to 15 years (median, 3 years). Four patients had a history of treatment with radioactive iodine, and 4 patients had a history of treatment with corticosteroids. Four patients had a history of smoking.
Table 1A.
Clinical information regarding thyroid disease for patients undergoing rectus muscle resection in Graves’ ophthalmopathy: History and treatments
| Case | Duration Graves’ disease, years |
Graves’ ophthalmopathy signs and symptoms |
Duration diplopia, years |
Radioactive iodine |
Corticosteroid treatments | Current thyroid medications | Smoking |
|---|---|---|---|---|---|---|---|
| Patients with restrictive strabismus | |||||||
| 1 | 7 | Proptosis OU | 6 | 5 yrs before resection | Pred, methylprednisolone 5–6 yrs bef resect | Levo | 20 pack-yr; quit 7 yrs before resection |
| 2 | 15 | Proptosis OU, increased IOP in upgaze, exposure keratopathy, upper lid retraction OU | 5 | None | Levo | Quit 5 yrs before resection | |
| 3 | 4 | Proptosis, lagophthalmos OU | >2 | None | Pred 2 yrs before resection and 1 yr before resection (after orbital decompression) | None; MMZ until 1 yr before resection | Quit 1 yr before resection |
| 4 | 2 | Proptosis, lid edema OU | 1.5 | 1.5 yrs before resection | None | Levo, MTX | |
| 5 | 5 | Inflammation treated with steroids, intermittent edema, bilat congestion | 2 | None | Oral and injected steroids 4–5 yrs before resection | MMZ | |
| Patients with nonrestrictive strabismus | |||||||
| 6 | 2 | Proptosis, upper lid retraction OU None | None | 2 mos before resection | None | PTU | 20 pack-yr; currently smokes one-half pack per day |
| 7 | 1 | None | 12 | None | None | MMZ | |
| 8 | 2 | Proptosis OU, tearing, eye pain, upper lid retraction OU | 1 | 2 yrs before resection | DXS × 2 mos 1 yr before resection | Levo, liothyronine | |
| Table 1B. Clinical information regarding thyroid disease for patients undergoing rectus muscle resection in Graves’ ophthalmopathy: visual acuity and ocular motility | |||||
|---|---|---|---|---|---|
| Preoperative ductions in field of action |
|||||
| Case | Visual acuity | Right eye | Left eye | ||
| Patients with restrictive strabismus | |||||
| 1 | OD 20/25 + 2 | −3 | −3 | −3 | −3 |
| OS 20/20 −3 | −1.5 | −2 | −1.5 | −1 | |
| −1 | −2 | −1 | −1 | ||
| 2 | OU 20/25 −2 | −3 | 0 | 0 | −4 |
| 0 | −3 | −1 | −3 | ||
| 0 | 0 | 0 | 0 | ||
| 3 | OU 20/30 | −1 | −1 | −1 | −1 |
| −1 | −1 | −2 | 0 | ||
| 0 | 0 | 0 | 0 | ||
| 4 | OD 20/25 + 2 | −2 | −2 | −2 | −2 |
| OS 20/40 | −3.5 | −0.5 | −0.5 | −3 | |
| −1 | −1 | −1 | −1 | ||
| 5 | OD 20/30 | 0 | 0 | +1 | 0 |
| OS 20/20 | 0 | −1 | 0 | 0 | |
| 0 | 0 | +1 | 0 | ||
| Patients with nonrestrictive strabismus | |||||
| 6 | OD NLP (childhood traumatic optic nerve atrophy) | −2 | +2 | +2 | 0 |
| 0 | −1 | −1 | 0 | ||
| OS 20/20 | 0 | +2 | +2 | 0 | |
| 7 | OU 20/20 | 0 | 0 | 0 | 0 |
| 0 | 0 | 0 | 0 | ||
| 0 | 0 | 0 | 0 | ||
| 8 | OU 20/20 | 0 | 0 | 0 | 0 |
| −3 | 0 | 0 | 0 | ||
| 0 | 0 | 0 | 0 | ||
DXS, dexamethasone; IOP, intraocular pressure; Levo, levothyroxine; MMZ, methimazole; MTX, methotrexate; OU, both eyes; pred, prednisone; PTU, propylthiouracil.
NLP, no light perception; OD, right eye; OS, left eye; OU, both eyes.
Table 2.
Surgical and postoperative data for patients undergoing rectus muscle resection in Graves’ ophthalmopathy
| Previous surgeries | Preoperative alignment primary gaze, PD |
Restriction on forced duction testing |
Rectus muscle resect surgery |
Postoperative steroids |
Postoperative alignment, primary gaze, PD |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Age at resect, years | Sex | Orbital decompression |
Strabismus | Within 1 week | Last follow-up | Complications | ||||
| Patients with restrictive strabismus | |||||||||||
| 1 | 70 | M | Bilat, 4.5 yrs before resection | (1) Bilat MR recess 7 mm + LIR recess 3 mm, 4 yrs before resection | D = ET 13 N = ET 3 |
Lateral ductions, upward/downward rotation OD: moderate | R LR resect 4.5 mma, excision of scar tissue OD | Day 1: ortho | No further follow-up available | ||
| (2) RMR recess 13.5 mm to 16 mm posterior to limbus + R IR recess 3.5 mm, 2 yrs before resection | |||||||||||
| 2 | 61 | F | Bilat, 1 yr before resection | (1) Bilat MR recess 5 mm + L IR recession 4 mm, 10 mos before resection | D = XT 15 LHoT 6 |
Bilateral LRs: none | R MR resect 4.5 mm + advance 5 mm and L IR recess 6 mma | Day 1: LHT 2; Day 5: XT 20, L HT 16 (broken suture noted) |
Month 3.5: XT 25, L HT 10 | Broken MR suture, persistent XT with dipl; underwent strabismus surgery at postoperative mo 3 (L LR recess 9 mma, R IR recess 13 mm from limbusa + R LR recess 9 mm) | |
| (2) R IR recess 4 mm, 9 mos before resection | |||||||||||
| 3 | 29 | F | Bilat, 1 yr before resection | Bilat MR recess 6 mm on semiadjustable, 4 mos before resection | D = ET 37 R HT 3 N = ET 40 |
Bilat LR resect 6 mma OD and 5.5 mm OS | Topical + antibiotic, oral steroid | Day 0: ortho | Month 8: flick ET | ||
| 4 | 53 | M | (1) OS, 1 yr before resection | Bilat MR recess 6.5 mm, LMRa, 5 mos before resection | D = ET 55 N = ET 40 |
Abduction OU: moderate; elevation OU: mild; adduction and depression: none | R LR resect 6 mma + L LR resection 6 mma, dissection of scar tissue OU | Topical + antibiotic, oral MP taper | Day 0: ET 8, no adjustment Day 2: ET 6 |
Month 2: ortho | |
| (2) OD, 6 mos before resection | |||||||||||
| 5 | 57 | F | (1) OS, 4 mos before resection | D = XT 25 RHT 14 N = XT 30 R HT 15 |
Data NA | L IR recess 4 mma, R LR recess 5 mma, R MR resection 4 mm | Day 0: XT 5, LHT 5 (adjusted to flick LHT); Week 1: ortho |
Month 2: ortho | |||
| (2) OD, 4 mos before resection, 2 wks after (1) | |||||||||||
| Patients with nonrestrictive strabismus | |||||||||||
| 6 | 51 | M | D = XT 42 N = XT 50 |
Adduction OD: mild to moderate | R MR resection 5 mm; R LR recession 9 mma (refused bilat) | Topical + antibiotic | Day 1: ortho | Year 1.5: ortho | |||
| 7 | 65 | F | D = ET 20 RHT 2 |
Data NA | R MR recess 3.5 mma; RLR resection 5 mm | Day 1: XT 4, flick LHT (adjusted to ortho); Week 1: ortho |
Month 2: ET 1 (no dipl primary pos, occasional dipl when lying on side); | ||||
| 8 | 25 | F | Bilat, 9 mos before resection | D = ET 16 | Lateral ductions: none | R MR recess 4 mma; R LR resect 5 mm | Week 1: ortho | Month 15: ortho (occasional dipl in right gaze) | |||
Bilat, bilateral; D, distance; dipl, diplopia; ET, esotropia; F, female; HT, hypertropia; IR, inferior rectus muscle; L, left; LR, lateral rectus muscle; LHoT, left hypotropia; M, male; MP, methylprednisolone; MR, medial rectus muscle; N, near; NA, not available; OD, right eye; ortho, orthotropic; OS, left eye; OU, both eyes; PD, prism diopters; R, right; XT, exotropia.
On adjustable suture.
Of the 8 patients, 6 had a history of orbital decompressions performed before any strabismus surgery; all 6 had developed strabismus before orbital decompression. Of the 6 patients, 5 had a change in their strabismus measurements after decompression, and 1 patient’s strabismus did not change after orbital decompression. Four (50%) patients had a history of strabismus surgery, consisting of recessions, before rectus muscle resection was performed.
Preoperative alignment and intraoperative forced duction testing data are given in Table 2. Preoperative alignment before the rectus muscle resection demonstrated a horizontal deviation in 8 patients and a vertical deviation in 5 patients. Of those with a horizontal deviation, 5 (62.5%) had esotropia ranging from 13Δ to 55Δ (28.2Δ ± 17.6Δ) and 3 (37.5%) had exotropia ranging from 15Δ to 42Δ (27.3Δ ± 13.7Δ). Of those with exotropia, 1 (case 2) had a consecutive exotropia after medial rectus recession, 1 (case 5) was likely a decompensation of intermittent exotropia given a lack of limited ductions that would indicate a restrictive etiology, and 1 (case 6) was likely a sensory exotropia. Vertical deviations ranged from 2Δ to 14Δ (6.3Δ ± 5.4Δ). Intraoperative forced duction testing data was available for 6 patients, 3 of whom had positive forced ductions.
A total of 10 rectus muscles were resected, involving the lateral rectus muscle in 5 patients (62.5%) and the medial rectus muscle in 3 (37.5%). No more than one muscle was resected per eye. Bilateral resection of the lateral rectus muscles was performed in 2 patients (25%). At the time of resection, 4 patients (50%) had bilateral strabismus surgery. Two patients (25%) had had prior rectus muscle recessions in the muscles that underwent resection.
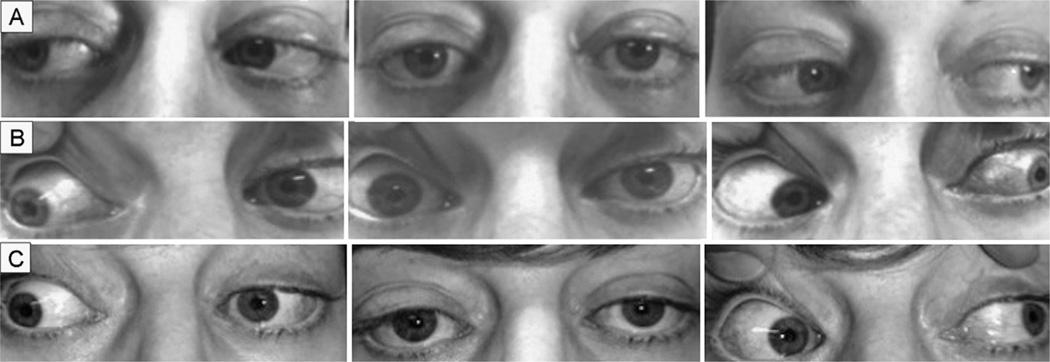
Postoperatively, 7 patients (87.5%) were orthotropic in primary position. Intraoperative forced duction testing in case 3 revealed restriction to abduction before the first strabismus surgery. The patient underwent bilateral medial rectus recession, which relieved the restriction in abduction. However, immediate and 2-month postoperative alignment revealed no improvement of the preoperative esotropia. Further strabismus surgery consisted of bilateral lateral rectus resections with negative intraoperative forced duction testing. Postoperative examinations showed orthotropia. One patient had persistent and worsened exotropia associated with slippage of the resected medial rectus muscle secondary to a broken suture on postoperative day 1. The medial rectus muscle was recovered and resutured to near orthotropia (flick of exotropia) on postoperative day 5. However, at subsequent postoperative visits, the exotropia recurred and worsened, requiring additional strabismus surgery at postoperative month three. None of the patients developed atypical inflammation beyond typical postoperative conjunctival injection. In addition, none of the resections resulted in overcorrection. Preoperative and postoperative clinical photographs of cases 6 (Figure 1) and 3 (Figure 2) demonstrate orthotropic postoperative alignment in primary gaze without unusual conjunctival scarring or orbital asymmetry. Case 6 had mild limitation to abduction in the right eye at postoperative year 1.5. Case 3 had mild limitation to adduction in both eyes at postoperative month 6.
FIG 1.
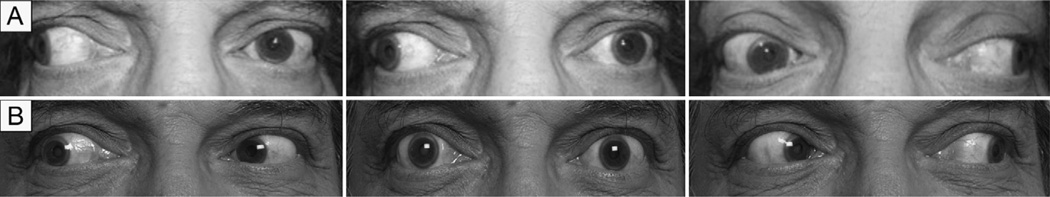
A, preoperative clinical photographs of case 6 showing large-angle exotropia caused by sensory deprivation in the right eye. B, postoperative year 1.5 photographs showing orthotropia in primary gaze and mild limitation of abduction in the right eye.
FIG 2.
A, clinical photographs of case 3 prior to any strabismus surgery and after bilateral orbital decompression. B, postoperative photographs at 2 months’ follow-up following bilateral medial rectus muscle recession 6.0mmin both eyes using adjustable sutures. C, postoperative photographs at 6 months’ follow-up after bilateral lateral rectus muscle resection.
There was no significant difference in successful strabismus surgery (orthotropia in primary gaze) between patients who had a history of treatment with corticosteroids (P = 0.62), cigarette use (P = 0.50), history of radioactive iodine treatment (P = 0.37), and use of postoperative corticosteroids (P = 0.62).
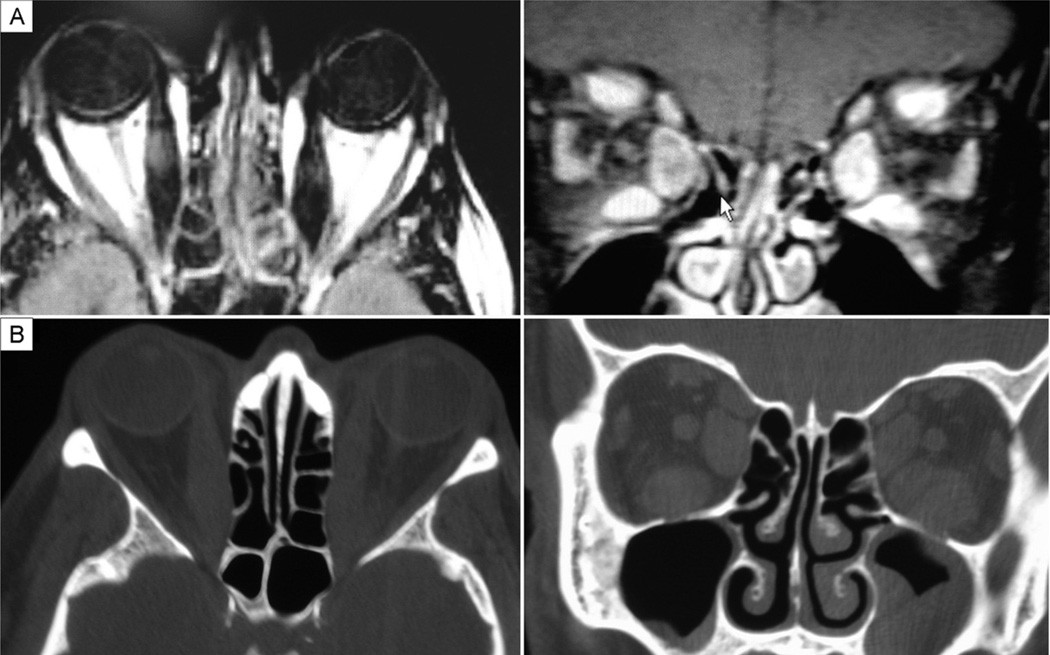
Computed tomography (CT) imaging of the orbits was available in 4 cases. Cases 8 and 3 (Figure 3A) had smaller lateral rectus muscles compared with the other rectus muscles. In case 1 (Figure 3B), the lateral rectus and superior rectus muscles were smaller than medial and inferior rectus muscles. In case 4, the lateral rectus muscle was smaller than the superior, medial, and inferior rectus muscles in the right eye. In the left eye, only the superior rectus appeared enlarged with a comparatively smaller lateral rectus.
FIG 3.
CT orbital imaging showing extraocular muscle enlargement that spares the lateral rectus muscles. A, case 3 shows no enlargement of the lateral rectus muscle. B, case 1 shows no enlargement of the lateral and superior rectus muscles.
Discussion
Although most clinicians believe that rectus muscle resections should not be performed in patients with Graves’ ophthalmopathy because of a risk of worsening restrictive strabismus,5,6 a search of the peer-reviewed literature yielded only 2 articles that included rectus muscle resections in patients with Graves’ ophthalmopathy; no reports of serious complications after rectus muscle resection in Graves’ ophthalmopathy were found.
Yan and colleagues13 reported 27 patients with Graves’ ophthalmopathy who had strabismus surgery involving recessions with a traction suture for large angle deviations (>25°). Of the 27 patients, 6 underwent simultaneous resection of the ipsilateral antagonist muscle. None of the patients who underwent rectus muscle resections were overcorrected. The authors suggested that a resection of the antagonist muscle could be considered in patients whose deviations are too large to be treated by a maximal recession. Ph Mourits and colleagues14 reported 38 patients with Graves’ ophthalmopathy who underwent strabismus surgery, 3 of whom had “very tight muscles” and underwent resection of a lateral rectus muscle in combination with extraocular muscle recession. The authors did not indicate which extraocular muscles were tight or the rationale for resection in combination with recession. Postoperatively, 2 of their patients who underwent rectus muscle resection had single vision in primary and reading positions without prisms. None of the patients were overcorrected. The authors remarked that their surgical failures might be explained by the fact that mostly recessions were done, which can displace the center of rotation of the globe, affecting the surgical result. They suggested recession be paired with resection of the antagonist muscle to avoid displacement of the center of rotation of the globe.
In our case series, we also found that patients with Graves’ ophthalmopathy underwent rectus muscle resections without resulting in increased restriction or overcorrection. None of the 8 cases developed overcorrection, and most of the cases (87.5%) were orthotropic in primary gaze. Among our 8 patients, 3 (cases 3, 5, 6) had large angle deviations and were orthotropic postoperatively. Thus recession-resection procedure of antagonist muscles may be considered in patients with large-angle deviations that are unlikely to improve with a maximal recession or in patients who request surgery in one eye, which was the case in case 6.
Metz5 states that rectus extraocular muscle resections are not indicated in patients with Graves’ ophthalmopathy because they can increase “muscle stiffness”; however, he notes that he has had occasional successful cases of small resections of rectus muscles. Pre- and postresection ocular rotations were available for 7 patients in our series: 2 patients’ ocular rotations remained unchanged, and 1 patient’s ocular rotations improved. Three patients who underwent recession and resection of antagonist muscles in the same eye had mildly decreased rotations (0 to −1) in the opposite direction of the resected muscles. No previous recessions of the antagonist muscles had been performed in these patients until the time of the recession and resection procedure. One case that underwent resection and advancement of the right medial rectus muscle had no change in ocular rotations in the right eye before subsequent strabismus surgery for persistent exotropia associated with a broken suture. Thus, no increased restriction of the resected muscle or unanticipated decreased ocular rotations occurred.
Metz5 also recommended subconjunctival corticosteroids to minimize postoperative inflammation and scarring. Three patients in our series received either topical or topical and oral steroids after extraocular muscle resection was performed; however, none of the patients in the series developed significant signs of inflammation whether or not they received steroids postoperatively.
CT imaging may also be useful in deciding whether resection can be considered. Hudson and Feldon15 studied CT imaging in 12 patients who developed late overcorrection after inferior rectus muscle recession for restrictive hypotropia in patients with Graves’ disease. The authors reported that 5 of the patients developed late overcorrection and, in comparison with the stable patients, had greater proptosis and larger superior rectus muscles on imaging preoperatively. They suggested that in patients with these preoperative findings, combined superior and inferior rectus muscle recession should be considered. Among the patients in our series, the CT images for 4 of the subjects showed relative sparing of the lateral rectus muscles, which were the resected muscles in all 4 cases. The right lateral rectus muscles were resected in cases 8 and 1, whereas the bilateral lateral rectus muscles were resected in cases 3 and 4. This finding may suggest that extraocular muscle resection in patients with Graves’ ophthalmopathy may be performed without complications of increased restriction or inflammation if the muscle is not enlarged on imaging.
Three patients had a nonrestrictive strabismus with a diagnosis of Graves’ disease and a range of Graves’ ophthalmopathy findings. Two of the patients did not have a history of orbital decompression. Case 7 had been diagnosed with Graves’ disease 1 year before presentation. Her Graves’ ophthalmopathy was mild, with diplopia that started 11 years before she was diagnosed with Graves’ disease. Case 6 was diagnosed with Graves’ disease 2 years before presentation. He had a longstanding large-angle sensory exotropia attributable to no light perception vision after childhood trauma and had mild Graves’ ophthalmopathy findings of bilateral lid retraction. Case 8 developed an esotropia after orbital decompression, likely due to an abducens nerve palsy and not restriction. Although these strabismus cases were nonrestrictive, they still demonstrate the possibility of undergoing resections in patients with Graves’ ophthalmopathy, which is generally avoided no matter the etiology of the strabismus.
We found that rectus muscle resections can be performed in Graves’ patients with persistent diplopia or strabismus despite previous strabismus surgeries or in patients requesting surgery in one eye, with no increase in extraocular muscle restriction or significant inflammation. One unifying feature of all the patients in this series was an absence of signs indicating active orbital or ocular inflammation preoperatively. We would avoid resection of muscles with positive forced ductions or that appear enlarged on imaging. Oral steroids may be considered postoperatively, although the majority of our patients were not treated with perioperative steroids.
Binocular field of single vision data were not available in this series but would be an important outcome to report in future studies of rectus muscle resections in Graves’ ophthalmopathy because strabismus surgery in exotropia typically decreases peripheral binocular field of single vision and increases it in esotropia.16 Other limitations of this study include the small number of cases and its retrospective nature. Also, the 4 surgeons may have had differing approaches when considering when to resect an extraocular muscle in their Graves’ ophthalmopathy patients. In addition, 2 patients’ forced duction testing and 4 patients’ orbital imaging were unavailable. Despite these limitations, our findings indicate that rectus muscle resections can be safely and successfully performed in appropriately selected patients with Graves’ disease. In patients with poor vision in one eye or who have failed maximal recession surgery, surgeons can consider rectus extraocular muscle resections in patients whose strabismus is stable, who have no evidence of active inflammation, and whose strabismus is not associated with restriction on forced duction testing or enlargement on orbital imaging.
Literature Search
PubMed and the Cochrane Library databases were searched using the following terms: Grave’s ophthalmopathy, thyroid ophthalmopathy, and rectus muscle resection.
Acknowledgments
We thank Dr. Sherwin Isenberg for his advice during preparation of the manuscript. The authors also gratefully acknowledge the late Arthur Rosenbaum’s years of thoughtful discussion, which led to the conception of this study.
Footnotes
Study conducted at Jules Stein Eye Institute, UCLA, Los Angeles, California.
Presented at the 2012 Association for Research in Vision and Ophthalmology Annual Meeting, May 6–10, Fort Lauderdale, Florida.
References
- 1.Bahn RS. Graves’ ophthalmopathy. N Engl J Med. 2010;362:726–738. doi: 10.1056/NEJMra0905750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartley GB, Fatourechi V, Kadrmas EF, et al. Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol. 1996;121:284–290. doi: 10.1016/s0002-9394(14)70276-4. [DOI] [PubMed] [Google Scholar]
- 3.Lee H, Roh HS, Yoon JS, Lee SY. Assessment of quality of life and depression in Korean patients with Graves’ ophthalmopathy. Korean J Ophthalmol. 2010;24:65–72. doi: 10.3341/kjo.2010.24.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terwee C, Wakelkamp I, Tan S, Dekker F, Prummel MF, Wiersinga W. Long-term effects of Graves’ ophthalmopathy on health-related quality of life. Eur J Ophthalmol. 2002;146:751–757. doi: 10.1530/eje.0.1460751. [DOI] [PubMed] [Google Scholar]
- 5.Metz HS. Strabismus related to Graves’ ophthalmopathy. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management: Principles and surgical techniques. Philadelphia, PA: W.B. Saunders Co.; 1999. pp. 285–295. [Google Scholar]
- 6.Raab EL, Aaby AA, Bloom JN, et al. Special forms of strabismus. In: Skuta GL, Cantor LB, Simon JW, editors. Basic and clinical science course: Pediatric ophthalmology and strabismus. San Francisco, CA: American Academy of Ophthalmology; 2010. pp. 127–143. [Google Scholar]
- 7.Siegel LM, Lozano MJ, Santiago AP, Rosenbaum AL. Adjustable and nonadjustable recession and resection techniques. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management: Principles and surgical techniques. Philadelphia, PA: W. B. Saunders Co.; 1999. pp. 435–448. [Google Scholar]
- 8.Kraft SP. Selected exotropia entities and principles of management. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management: Principles and surgical techniques. Philadelphia, PA: W. B. Saunders Co.; 1999. pp. 176–201. [Google Scholar]
- 9.Egbert JE, Fantin A. Factors influencing measurement and response to strabismus surgery. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management: Principles and surgical techniques. Philadelphia, PA: W. B. Saunders Co.; 1999. pp. 73–83. [Google Scholar]
- 10.Mehta A. Chief complaint, history and physical examination. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management: Principles and surgical techniques. Philadelphia, PA: W. B. Saunders Co.; 1999. pp. 3–21. [Google Scholar]
- 11.Phillips PH, Hunter DG. Evaluation of ocular torsion and principles of management. In: Rosenbaum AL, Santiago AP, editors. Clinical strabismus management: Principles and surgical techniques. Philadelphia, PA: W. B. Saunders Co; 1999. pp. 52–72. [Google Scholar]
- 12.Santiago AP, Rosenbaum AL. Tests of muscle function. In: Rosenbaum AL, Santiago AP, editors. clinical strabismus management: Principles and surgical techniques. Philadelphia, PA: W. B. Saunders Co.; 1999. pp. 37–51. [Google Scholar]
- 13.Yan J, Zhang H. The surgical management of strabismus with large angle in patients with Graves’ ophthalmopathy. Int Ophthalmol. 2008;28:75–82. doi: 10.1007/s10792-007-9114-1. [DOI] [PubMed] [Google Scholar]
- 14.Ph Mourits M, Koorneef L, van Mourik-Noordenbos AM, et al. Extraocular muscle surgery for Graves’ ophthalmopathy: does prior treatment influence surgical outcome? Br J Ophthalmol. 1990;74:481–483. doi: 10.1136/bjo.74.8.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hudson HL, Feldon SE. Late overcorrection of hypotropia in Graves’ ophthalmopathy: Predictive factors. Ophthalmology. 1992;99:356–360. doi: 10.1016/s0161-6420(92)31965-7. [DOI] [PubMed] [Google Scholar]
- 16.Keltner JL. Strabismus surgery in adults: Functional and psychosocial implications. Arch Ophthalmol. 1994;112:599–600. doi: 10.1001/archopht.1994.01090170043019. [DOI] [PubMed] [Google Scholar]