Abstract
We report a case of isolated pulmonary infectious endocarditis (IE) with Candida parapsilosis. A 66-year-old man presented with fever and cough. Echocardiography showed severe pulmonary regurgitation and vegetations on the pulmonary valves. Initially, antibiotics were prescribed against bacterial IE, and the vegetations disappeared; however, the pulmonary vegetations relapsed, and C. parapsilosis was grown from blood cultures. We performed a debridement without a pulmonary valve replacement. There was no recurrence of IE for 3 years, and then the patient developed right ventricular enlargement and severe tricuspid regurgitation due to severe pulmonary regurgitation. Pulmonary valve replacement was performed. Now the patient is free from infection.
Keywords: Endocarditis, Pulmonary valve, Fungi, Reoperation
INTRODUCTION
Infectious endocarditis (IE) is a major life-threatening disease. Although left-sided IE is common, right-sided IE is rare [1]. The incidence of isolated pulmonary valve IE is <2%. Generally, IE results from bacterial infection, and fungal infection is uncommon [2]. We report a case of isolated pulmonary valve IE due to Candida parapsilosis treated by a separating two-stage operation.
CASE REPORT
A 66-year-old man was admitted to our hospital with fever and cough. He had no past history of cardiac disease, diabetes mellitus, hypertension, immunodeficiency or drug abuse. Physical examination revealed systolic murmur on the anterior chest. The results of laboratory studies showed that C-reactive protein was elevated to 17.64 mg/dl, with a white blood cell count of 17 200 cells/mm3. Thoracic computed tomography showed multifocal pulmonary embolism, and echocardiography showed severe pulmonary regurgitation and valve vegetations (Fig. 1). Initially, meropenem was prescribed. Staphylococcus aureus was detected in the blood cultures, and the antibiotic therapy was de-escalated to cefazolin sodium hydrate (3 g/day). After cefazolin sodium hydrate was discontinued, the fever and pulmonary valve vegetation recurred. Candida parapsilosis was grown from blood culture, and amphoterici B was administered for 4 weeks.
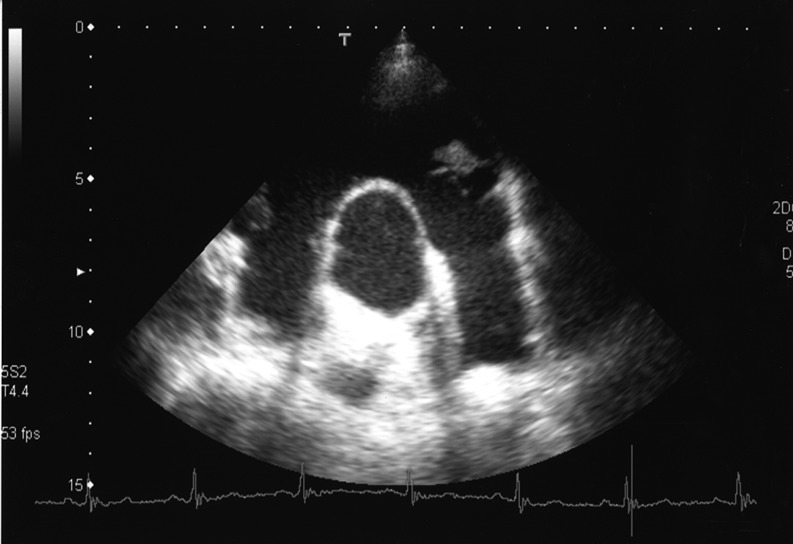
Figure 1:
The echocardiography shows vegetation on the pulmonary valve.
At the initial operation, no cardiac anomaly was observed. Although there were no vegetations on the tricuspid valve, there were several vegetations adherent to each of the pulmonary leaflets. All pulmonary leaflets with vegetations were resected, but the valve was not replaced. The excised specimen showed fungi (Fig. 2). Although severe pulmonary regurgitation remained, the infectious endocarditis was controlled and the pulmonary embolism was improved after the operation. Antimycotic therapy was discontinued 8 weeks after the first operation. In outpatient follow-up, the patient did not have recurrence of IE.
Figure 2:
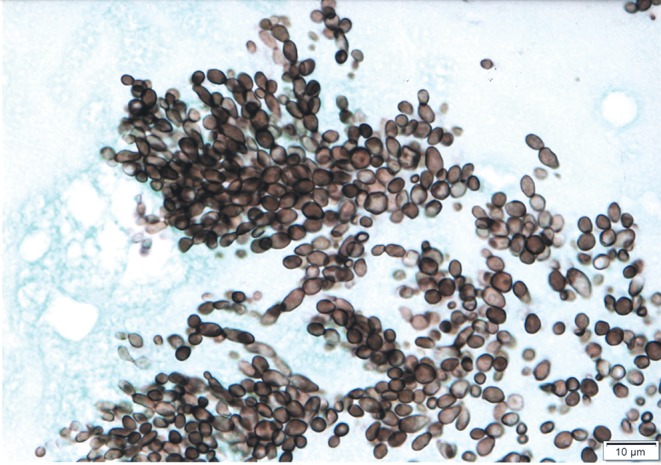
Candida parapsilosis was detected from pulmonary valve specimens by Grocott stain.
For 2 years, brain natriuretic peptide remained at 10 pg/ml and right-sided heart failure did not develop, but echocardiography showed right ventricular enlargement, with a right ventricular diastolic diameter of 47 mm, and moderate to severe tricuspid regurgitation in addition to the previous severe pulmonary regurgitation. At the second operation, a pulmonary valve remnant was resected and a 23-mm Carpentier-Edwards PERIMOUNT Magna Ease aortic heart valve (Edwards Lifesciences, Irvine, CA, USA) was implanted in an intra-annular position. Simultaneously, tricuspid annuloplasty was performed with an Edwards MC3 tricuspid Annuloplasty Ring (Edwards Lifesciences). Postoperative echocardiography showed mild pulmonary regurgitation and mild tricuspid regurgitation, and the right ventricle had become smaller. One year later, 45 months after the first operation, IE had not recurred.
DISCUSSION
Although left-sided IE is common, right-sided IE comprises only 5–10% of the total number of cases [1]. Right-sided IE is generally seen in patients with predisposing conditions, such as drug abuse, indwelling catheters, pacemaker leads or structural heart diseases, such as congenital heart disease. Given that most of the right-sided IE cases involve the tricuspid valve, isolated pulmonary IE, without infection of other valves, is very rare. Furthermore, fungal endocarditis is extraordinary, accounting for only 1.3–6% of all cases of IE [3]. About two-thirds of all fungal endocarditis is accounted for by Candida species. The majority of these infections are caused by C. albicans, with 21% C. parapsilosis, 15% C. glabrata and 9% C. tropicalis [2]. In our patient, there were no predisposing factors, but it is possible that use of broad-spectrum antibiotics could result in microbial substitution by C. parapsilosis.
Pulmonary valve replacement has widely been adopted as the management strategy for patients with pulmonary insufficiency [4]. It has been shown to result in an improvement of symptoms, a decrease in right ventricular size, stabilization of the QRS complex and a reduction in the incidence of atrial and ventricular arrhythmias [5]. However, patients can tolerate considerable pulmonary regurgitation after pulmonary valvotomy or valve resection.
Candida parapsilosis is likely to produce biofilm structures that are morphologically different from those produced by C. albicans [3]. Therefore, IE induced by C. parapsilosis is recognized as difficult to treat completely. It has been reported that it can recur as late as 43 months after a positive blood culture [3]. In the present case, because the recurrence of endocarditis was a profound concern at the initial operation, only pulmonary valve resection, without implantation of an artificial valve, was done as a first stage. As a result, we administered amphotericin B for only 8 weeks at the first operation. The two-stage operation required no additional antimycotic therapy.
CONCLUSION
We experienced a rare case of isolated pulmonary valve infectious endocarditis due to C. parapsilosis. In order to avoid the recurrence of IE, the surgical treatment was designed as a two-stage procedure, with initial debridement, followed by valve replacement at a second operation. Postoperative follow-up was mandatory, and up to now the patient has been satisfactory, without any recurrence of IE.
Conflict of interest: none declared.
References
- 1.Musci M, Siniawski H, Pasic M, Grauhan O, Weng Y, Meyer R, et al. Surgical treatment of right-sided active endocarditis with or without involvement of the left heart: 20-year single center experience. Eur J Cardiothorac Surg. 2007;32:118–25. doi: 10.1016/j.ejcts.2007.02.034. doi:10.1016/j.ejcts.2007.02.034. [DOI] [PubMed] [Google Scholar]
- 2.Baddley JW, Benjamin DK, Jr, Patel M, Miro J, Athan E, Barsic B, et al. Candida infective endocarditis. Eur J Clin Microbiol Infect Dis. 2008;27:519–29. doi: 10.1007/s10096-008-0466-x. doi:10.1007/s10096-008-0466-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gullu AU, Akcar M, Arnaz A, Kizilay M. Candida parapsilosis tricuspid native valve endocarditis: 3-year follow-up after surgical treatment. Interact CardioVasc Thorac Surg. 2008;7:513–4. doi: 10.1510/icvts.2007.173435. doi:10.1510/icvts.2007.173435. [DOI] [PubMed] [Google Scholar]
- 4.Fiore AC, Rodefeld M, Turrentine M, Vijay P, Reynolds T, Standeven J, et al. Pulmonary valve replacement: a comparison of three biological valves. Ann Thorac Surg. 2008;85:1712–8. doi: 10.1016/j.athoracsur.2008.02.001. doi:10.1016/j.athoracsur.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 5.Shinkawa T, Anagnostopoulos PV, Johnson NC, Watanabe N, Sapru A, Azakie A. Performance of bovine pericardial valves in the pulmonary position. Ann Thorac Surg. 2010;90:1295–300. doi: 10.1016/j.athoracsur.2010.06.021. doi:10.1016/j.athoracsur.2010.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]