Abstract
Objective
We sought to determine the extent to which adoption of health information technology (HIT) by physician practices may differ from the extent of use by individual physicians, and to examine factors associated with adoption and use.
Materials and methods
Using cross-sectional survey data from the National Study of Small and Medium-Sized Physician Practices (July 2007–March 2009), we examined the extent to which organizational capabilities and external incentives were associated with the adoption of five key HIT functionalities by physician practices and with use of those functionalities by individual physicians.
Results
The rate of physician practices adopting any of the five HIT functionalities was 34.1%. When practices adopted HIT functionalities, on average, about one in seven physicians did not use those functionalities. One physician in five did not use prompts and reminders following adoption by their practice. After controlling for other factors, both adoption of HIT by practices and use of HIT by individual physicians were higher in primary care practices and larger practices. Practices reporting an emphasis on patient-centered management were not more likely than others to adopt, but their physicians were more likely to use HIT.
Discussion
Larger practices were most likely to have adopted HIT, but other factors, including specialty mix and self-reported patient-centered management, had a stronger influence on the use of HIT once adopted.
Conclusions
Adoption of HIT by practices does not mean that physicians will use the HIT.
Keywords: Physician practices, electronic health records, meaningful use
Introduction
Early evidence suggests that use of health information technology (HIT) by healthcare providers may help improve disease management, care coordination, and health outcomes, especially for patients with one or more chronic illnesses.1–6 However, to date, many physician practices have failed to adopt HIT.7–12 Several factors associated with practices’ ability and willingness to adopt HIT have been well documented, including availability of resources,8–10 incentives for use of HIT,9 better care outcomes,9 and training and technical support for providers.8 10 13 14 Barriers to adoption include concerns about lack of interoperability with hospitals, the cost of purchasing and maintaining HIT, loss of productivity during the transition to HIT, and concerns about future obsolescence of purchased technology.8 10 12 14 15 These findings provided the basis for the inclusion of ‘meaningful use’ incentives for the adoption and use of HIT into the American Recovery and Reinvestment Act of 2009, which began offering incentive payments during 2011 (with a maximum value of around $60 000 per eligible provider, paid over the course of 3 years).16 17
A few studies have demonstrated that individual physicians do not always use HIT functionalities once their practice has adopted them,12 18 but no study to date has systematically examined organizational factors associated with the use of HIT by individual physicians once it has been adopted by their practice. This subtle but important point differentiates between the capital resources required for physician practices to purchase and implement HIT and the cultural, managerial, and organizational conditions under which individual physicians will be more likely to use available technology. Rao et al12 reported that physicians in some practices, especially in the smallest practices, did not use adopted functionalities ‘most or all of the time,’ but their study did not examine the effect of factors other than practice size on the use of HIT.
Drawing from data collected through the National Survey of Small and Medium-sized Physician Practices, we studied a comprehensive set of factors related to organizational capabilities and external incentives9 19–21 in modeling the adoption of five basic HIT functionalities by physician organizations and use of HIT functionalities by individual physicians once adopted. We studied five key HIT functionalities: problem lists, progress notes, drug interactions, prompts and reminders, and alerts for abnormal tests. As suggested by previous studies, greater availability of resources and the ability to obtain economies of scale—achieved through increased practice size or ownership by a hospital, system, or health maintenance organization (HMO)8 9—may especially enable adoption. In contrast, individual physician use of HIT may be contingent on other factors, such as the motivation of providers.22 For example, physicians working in practices owned by an external entity—typically a hospital—may feel less control over HIT implementation and may be less likely to use it.23 Practices that incorporate patient feedback in a systematic manner may be more inclined to use available HIT in comparison to less patient-centered practices. The motivation to use data to improve the patient experience may, in some cases, provide the extra push for individuals to fully use the functionalities of their HIT system. Finally, practices containing physicians from different specialties—multispecialty practices—may be more likely than others to use HIT once it has been adopted, because of a greater need to use basic HIT functionalities for internal communication about patients within the practice, stemming from internal referrals.24 25
Methods
Data
This analysis draws on data from the National Study of Small and Medium-Sized Physician Practices.21 The National Study of Small and Medium-Sized Physician Practices was a 40 min cross-sectional telephone survey conducted between July 2007 and March 2009 with the lead physician or lead administrator of a national sample of physician practices that had 1–19 physicians. Respondents were paid $175 for their time.
Survey sample
There is no publicly available database of US physician practices. We used a comprehensive private database, the IMS Healthcare Organization Services database,26 to create the population from which we sampled practices. In 2007, this national database, updated daily, included 793 235 US physicians linked to the practices in which they work. IMS data are widely accepted and have been used in dozens of studies published in peer-reviewed journals.27–29
Practices were eligible for the survey if they had 1–19 physicians of whom at least 60% were some combination of adult primary care providers (family physicians, general internists, and general practitioners), cardiologists, endocrinologists, and pulmonologists. We included only practices with these specialties because the survey focused on care management processes for preventive care and for four major chronic illnesses: asthma, congestive heart failure, diabetes, and depression. We included hospital-owned practices but not academic faculty practices.
The National Study of Small and Medium-Sized Physician Practices was intended to provide data that would be as nationally representative as possible and that would also be useful for program evaluation purposes in 14 sites involved in the Aligning Forces for Quality initiative, sponsored by the Robert Wood Johnson Foundation.30 Sites consisted of a range of geographic areas, including states such as Maine, and metropolitan areas such as Cleveland.31
Using the IMS database and the eligibility criteria described above, we drew a random sample of practices, stratifying by practice size (1–2, 3–8, 9–12, and 13–19 physicians), each of the four specialty types listed above, and location (each of the 14 Aligning Forces for Quality sites and the remainder of the USA). We oversampled the strata that had relatively few practices, such as single-specialty pulmonology practices with 13–19 physicians. We also oversampled within each of the Aligning Forces for Quality sites, to ensure an adequate sample for evaluation.
The number of practices that responded to the survey was 1744 (1200 from the 14 Aligning Forces for Quality communities and 544 from the national sample). The overall adjusted response rate was 63.2% (64.3% for the Aligning Forces for Quality communities and 61.3% for the national sample).32
Measures
Outcome variables
This study examined the adoption and use of five basic functionalities of HIT: problem lists, progress notes, drug interactions, prompts and reminders, and alerts for abnormal tests. All responding practice leaders were asked whether their practice made available an electronic medical record including each of the five functionalities. We also examined whether practices adopted all HIT functionalities or any functionalities.
Each of these five questions was followed by a separate question asking what percentage of the physicians in their practice used that HIT functionality. In order to examine use of HIT for practices adopting each functionality, any functionality, and all functionalities, the mean percentage of physicians using each of the adopted functionalities was examined.
Explanatory variables
To model adoption and use of HIT, we included factors reflecting organizational capabilities and external incentives. Organizational capabilities may have enabled practices to adopt and use HIT more effectively and efficiently.33 For instance, the size of each practice, as indicated by the number of physicians, was an important component. Larger practices may have had more resources or may have experienced benefits due to economies of scale.9–12 Practices with more than one site may gain extra benefit from using HIT compared to paper records, which are only readily available at a single site. Practices owned by an external entity—a hospital, system, or HMO—may have more resources to implement HIT, but less buy-in from individual physicians.19 Independent practice associations (IPAs) and physician–hospital organizations (PHOs) may have influence over many physician practices, through their ability to provide access to new patients and assistance to practices with care management processes.19 34 We thus included a binary indicator capturing whether practices reported receiving ‘a significant amount of their patients’ from IPAs or PHOs. The specialty composition of each practice was captured according to whether they included only primary care physicians, physicians from multiple specialties, or physicians entirely from a single specialty (including all cardiology, endocrinology, or pulmonology).
Practice capabilities also included participation in quality improvement (QI) programs and a measure of the patient-centeredness of the practice. Practices participating in a QI program may have been more likely to be exposed to information about how HIT can help improve clinical coordination. Practices reporting a greater emphasis on patient-centered management may also have been more motivated to adopt and use HIT.35 To capture this, we constructed a ‘patient-centered management’ index, adapted from the National Malcolm Baldrige Quality Award criteria, using the following items: practice assesses patient needs; staff promptly resolve patient complaints; patients’ complaints are studied to identify patterns and prevent reoccurrence; practice uses data from patients to improve care; and practice uses data on patient satisfaction when developing new services.36–38 Practices answered each item on a scale of 1 (strongly disagree) to 5 (strongly agree). To capture the extent to which practices placed an especially strong emphasis on these items, we constructed the index such that one point was given for each item only when respondents answered ‘strongly agree’ to that item. The resulting ‘patient-centered management’ scale thus has a range from 0 to 5.21
We included a measure of payer mix—the proportion of practices’ revenue from Medicaid and uninsured patients21 39—because having more patients with poor or no insurance may have diminished the available capital for practices that might have been invested in HIT. We also included two measures of patient demographics: percentage of patients who are African-American and percentage of patients with limited English proficiency, because practices caring for large numbers of minority patients have reported lower payment levels and increased challenges delivering high-quality care.40 41
Finally, prior studies found that external incentives were associated with the adoption of HIT.8 9 Thus, we controlled for whether practices reported participating in programs awarding bonus income for the adoption or use of HIT in the last year.9 We also accounted for whether health plans publicly reported practice data on patient satisfaction and clinical quality, creating an index ranging from 0 to 2.21
Analysis
We first explored summary statistics for the adoption of each of the five key HIT functionalities by practice and their use by individual physicians, if adopted. We report mean values for each of the explanatory factors, stratified by whether practices had adopted any of the five HIT functionalities. We used t tests to compare the mean values between the two groups (adopted no functionalities and adopted any functionalities).
We examined factors associated with adoption and use of each functionality in separate regression analyses. Adoption of each functionality by practices, captured through binary indicators, was examined using logit models. From those logit models, we calculated the average marginal probability associated with adopting HIT functionalities for each factor.42 We report marginal probabilities because they allow for a more straight-forward interpretation of effect sizes.43 The average marginal probabilities were largely consistent with ORs produced from the same models. To examine use of HIT by individual physicians, linear regression was used, because use was captured as a percent of physicians within practices using each functionality. To account for the non-linear relationship between practice size and the outcomes, size was logged in regression analyses.
All results were weighted to be nationally representative. Standard errors were adjusted to account for the complex survey design of the National Survey of Small and Medium-Sized Physicians.44
Results
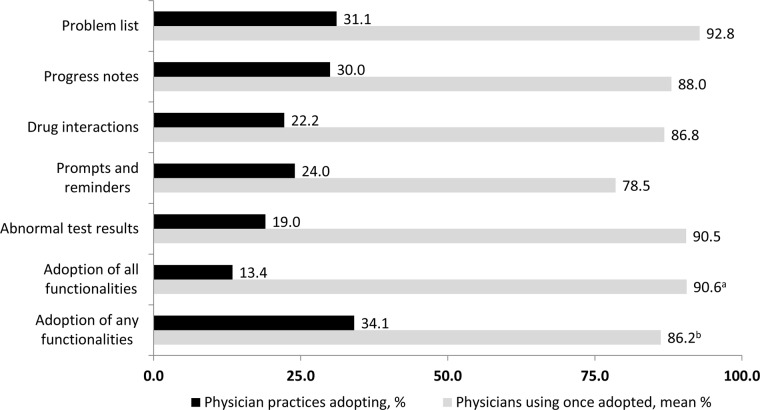
Thirty-four percent of small and medium-sized physician practices adopted at least one of the five HIT functionalities, but only 13.4% adopted all five (figure 1). Problem lists were adopted most frequently (31.1%), while functionalities for tracking abnormal test results were adopted the least (19.0%).
Figure 1.
Adoption and use of health information technology. N=1744 physician practices. Percentages are weighted to be nationally representative. HIT, health information technology. aThe mean percentage of physicians using each functionality within practices that adopted all functionalities, averaged across those practices. bThe mean percentage of physicians using each adopted functionality within practices that adopted any functionalities, averaged across those practices. Source: National Survey of Small and Medium-sized Physician Practices (July 2007–March 2009).
Among the 34% of practices adopting any functionality, an average of 86.2% of their physicians used the functionality. That is, on average, one physician in seven did not use a functionality, even though it had been adopted by the practice. Problem lists were the most likely to be used by individual physicians once adopted (92.8% of physicians), while, consistent with prior studies which suggest that they are disliked by many physicians,45 46 respondents reported that their physicians were least likely to use prompts and reminders (78.5%).
In bivariate analyses comparing practices that adopted any of the five focal HIT functionalities to those that did not, practices were more likely to have adopted HIT if they were larger, participated in one or more QI programs, and/or were in a program in which they could receive a bonus for use of HIT (table 1). Practices were less likely to have adopted HIT if they had a higher percentage of patients with limited English proficiency. Adopting practices did not differ significantly from non-adopting practices in ownership, specialty type, self-reported patient-centered management, or participation in an IPA or PHO.
Table 1.
Descriptive statistics for factors associated with adoption by practices of health information technology (HIT), stratified by whether practices had adopted any HIT functionalities
| Overall | No HIT | Any HIT | ||
|---|---|---|---|---|
| N=(1744) | n=(1118) | n=(626) | p Value | |
| Organizational capabilities | ||||
| Size (number of physicians), mean | 3.2 (1.0) | 2.7 (0.9) | 4.2 (1.0) | <0.001 |
| More than one practice site, mean | 0.2 (0.1) | 0.2 (0.1) | 0.2 (0.1) | 0.136 |
| Hospital, system, or HMO ownership (%) | 9.6 (3.8) | 7.8 (2.5) | 13.1 (5.5) | 0.107 |
| Significant proportion of patients from an IPA or PHO (%) | 29.2 (1.3) | 30.7 (2) | 26.3 (1.6) | 0.089 |
| Practice specialty mix (%) | ||||
| Primary care | 82.2 (11.4) | 84 (10.8) | 78.6 (13) | 0.391 |
| Multispecialty | 9.1 (7.4) | 6.9 (5.8) | 13.4 (10.3) | 0.221 |
| Single specialty | 8.7 (5.9) | 9.0 (6.6) | 8.0 (5.1) | 0.770 |
| Participated in QI program (%) | 10.4 (2.3) | 7.4 (2) | 16.2 (1.5) | <0.001 |
| Patient-centered management index (range 0–5) (mean) | 2.2 (0.2) | 2.3 (0.2) | 2.1 (0.1) | 0.065 |
| Revenue from Medicaid or uninsured, mean (%) | 11.7 (0.6) | 11.5 (0.7) | 12.1 (0.7) | 0.504 |
| African-American patients, mean (%) | 13.8 (0.4) | 14.1 (0.5) | 13.4 (0.5) | 0.347 |
| Patients with limited English proficiency, mean (%) | 7.6 (1.2) | 9.4 (1.5) | 4.3 (0.5) | 0.003 |
| External incentives | ||||
| Public reporting index (range 0–2) (mean) | 0.5 (0.0) | 0.5 (0.0) | 0.5 (0.0) | 0.564 |
| Bonus income for HIT (%) | 11.7 (1.9) | 9.3 (2.3) | 16.4 (0.6) | 0.004 |
Results are weighted to be nationally representative. Numbers in parentheses are SEs. p Values indicate whether practices adopting any HIT significantly differed from those not adopting HIT on each item.
Source: National Survey of Small and Medium-sized Physician Practices (July 2007–March 2009).
HIT, health information technology; HMO, health maintenance organization; IPA, independent practice association; PHO, physician–hospital organization; QI, quality improvement.
When we controlled for other factors through logit regression analysis, the results were similar to those found in bivariate analyses (table 2). Practice size had a large, positive, and significant association with adoption of all five functionalities (each one-unit increase in the logged number of physicians was associated with an increase in the probability of adoption ranging from 0.08 to 0.16, or 8 to 16 percentage points). Participation in a QI program was also associated with a substantial increase in the probability of adopting problem lists (average marginal probability: 0.15, 95% CI 0.04 to 0.26), progress notes (0.16, 95% CI 0.03 to 0.29), and prompts and reminders (0.10, 95% CI 0.04 to 0.15). Participating in programs awarding bonus income for the use or adoption of HIT was also associated with the adoption of prompts and reminders (0.10, 95% CI 0.04 to 0.17) and alerts for abnormal test results (0.10, 95% CI 0.06 to 0.14). The effects on the adoption of HIT associated with seeing patients with limited English proficiency were negative and statistically significant across all functionalities, ranging around one percentage point for each additional percentage point of patients with limited English proficiency. While this effect appears small, it could become quite large for practices where a substantial proportion of patients had limited English proficiency. Ownership by a hospital, system, or HMO had no significant effect on the adoption by practices of any HIT functionality.
Table 2.
Factors associated with the adoption of health information technology functionalities: results from logit regression models
| Problem list | Progress notes | Drug interactions | Prompts and reminders | Abnormal test results | Adoption of all functionalities | Adoption of any functionalities | |
|---|---|---|---|---|---|---|---|
| Log size | 0.16*** (0.13 to 0.18) | 0.14*** (0.12 to 0.17) | 0.13*** (0.09 to 0.17) | 0.08*** (0.06 to 0.11) | 0.10*** (0.07 to 0.13) | 0.08*** (0.04 to 0.11) | 0.16*** (0.13 to 0.18) |
| More than one practice site | −0.07* (−0.15 to 0.00) | −0.06 (−0.16 to 0.04) | −0.03 (−0.10 to 0.03) | −0.01 (−0.10 to 0.08) | 0.00 (−0.07 to 0.07) | −0.00 (−0.05 to 0.04) | −0.07 (−0.17 to 0.04) |
| Hospital, system, or HMO ownership | −0.04 (−0.23 to 0.15) | 0.01 (−0.15 to 0.18) | −0.01 (−0.09 to 0.08) | −0.06 (−0.17 to 0.06) | −0.04 (−0.13 to 0.06) | −0.05 (−0.13 to 0.03) | −0.02 (−0.22 to 0.18) |
| Significant proportion of patients from an IPA or PHO | −0.03 (−0.13 to 0.08) | −0.07 (−0.17 to 0.02) | −0.02 (−0.11 to 0.07) | 0.03 (−0.07 to 0.14) | 0.02 (−0.08 to 0.12) | −0.01 (−0.07 to 0.06) | −0.03 (−0.15 to 0.09) |
| Specialty mix (reference is primary care practices) | |||||||
| Multispecialty practice type | −0.00 (−0.15 to 0.15) | −0.05 (−0.12 to 0.02) | −0.04 (−0.22 to 0.14) | −0.02 (−0.17 to 0.13) | −0.11* (−0.23 to 0.01) | −0.09*** (−0.15 to −0.03) | 0.00 (−0.14 to 0.15) |
| Single specialty practice type | −0.04 (−0.11 to 0.02) | −0.05 (−0.11 to 0.01) | −0.04 (−0.10 to 0.02) | −0.13*** (−0.18 to −0.08) | −0.09*** (−0.15 to −0.04) | −0.11*** (−0.17 to −0.04) | −0.05 (−0.12 to 0.02) |
| Participated in QI program | 0.15*** (0.04 to 0.26) | 0.16* (0.03 to 0.29) | 0.05 (−0.02 to 0.12) | 0.10*** (0.04 to 0.15) | 0.12 (−0.04 to 0.28) | 0.04 (−0.02 to 0.11) | 0.14*** (0.05 to 0.24) |
| Patient-centered management index (range 0–5) | 0.01 (−0.01 to 0.03) | −0.00 (−0.03 to 0.02) | −0.01 (−0.04 to 0.02) | −0.00 (−0.03 to 0.03) | 0.01 (−0.01 to 0.02) | 0.00 (−0.01 to 0.02) | 0.00 (−0.02 to 0.03) |
| Revenue from Medicaid or uninsured | 0.00 (−0.00 to 0.00) | −0.00 (−0.00 to 0.00) | −0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.00) |
| African-American patients | −0.00 (−0.00 to 0.00) | −0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.00) | 0.00 (−0.00 to 0.00) | −0.00 (−0.00 to 0.00) |
| Patients with limited English proficiency | −0.01*** (−0.01 to −0.00) | −0.01*** (−0.01 to −0.00) | −0.01*** (−0.01 to −0.00) | −0.01*** (−0.01 to −0.00) | −0.01*** (−0.01 to −0.00) | −0.00** (−0.01 to −0.00) | −0.01*** (−0.02 to −0.00) |
| Public reporting index (range 0–2) | −0.03* (−0.06 to 0.00) | −0.02 (−0.05 to 0.01) | −0.00 (−0.04 to 0.03) | 0.02 (−0.01 to 0.04) | −0.02* (−0.05 to 0.00) | −0.01 (−0.03 to 0.01) | −0.02* (−0.04 to 0.00) |
| Bonus income for HIT | 0.07 (−0.01 to 0.16) | 0.04 (−0.03 to 0.11) | 0.03 (−0.10 to 0.16) | 0.10*** (0.04 to 0.17) | 0.10*** (0.06 to 0.14) | 0.03 (−0.07 to 0.13) | 0.11* (−0.00 to 0.22) |
| N | 1744 | 1744 | 1744 | 1744 | 1744 | 1744 | 1744 |
*p<0.10; **p<0.05; ***p<0.01.
Logit regression analysis was used for all models. Results are presented as marginal probability (95% CI), and are weighted to be nationally representative.
Source: National Survey of Small and Medium-sized Physician Practices (July 2007–March 2009).
HIT, health information technology; HMO, health maintenance organization; IPA, independent practice association; PHO, physician–hospital organization; QI, quality improvement.
In linear regression analyses of use of HIT by individual physicians in practices that had adopted HIT, multispecialty practices in particular were associated with reduced use of HIT functionalities by physicians, relative to primary care practices (table 3). Multispecialty practice type was associated with a 12.9 percentage point reduction in use of any adopted HIT (95% CI −17.05 to 8.69). Self-reported patient-centered management was positively associated with use of HIT (three of five HIT functionalities significantly associated; range across all five: 1.0–8.4 percentage points for each additional point on the patient-centered management index). For most functionalities, physicians in larger practices were more likely to use HIT once their practice adopted it. Other variables, including the availability of bonuses for the practice for HIT use, were not significantly associated with use of HIT by physicians.
Table 3.
Factors predicting use of health information technology functionalities, conditional on adoption of each functionality: results from linear regression models
| Problem list | Progress notes | Drug interactions | Prompts and reminders | Abnormal test results | Adopted all HIT† | Adopted any HIT† | ||
|---|---|---|---|---|---|---|---|---|
| Log size | −2.99*** (−5.23 to −0.76) | 3.24 (−0.74 to 7.21) | 3.66 (−0.91 to 8.23) | 11.39*** (5.66 to 17.13) | 13.16*** (5.91 to 20.41) | 6.06** (1.44 to 10.67) | 3.69** (0.43 to 6.96) | |
| More than one practice site | 3.08 (−5.97 to 12.13) | −4.10 (−16.66 to 8.47) | 0.94 (−4.81 to 6.70) | −7.80*** (−13.66 to −1.93) | −2.37 (−10.44 to 5.71) | −0.42 (−7.31 to 6.47) | 1.83 (−8.50 to 12.16) | |
| Hospital, system, or HMO ownership | 3.76** (0.23 to 7.28) | 2.10 (−4.01 to 8.21) | 11.42*** (5.21 to 17.62) | 12.41 (−17.61 to 42.43) | −1.31 (−12.80 to 10.18) | 7.86* (−1.40 to 17.13) | 2.80 (−1.08 to 6.68) | |
| Significant proportion of patients from an IPA or PHO | −5.32* (−11.24 to 0.60) | −4.79* (−10.06 to 0.47) | 114.15*** (−19.20 to −9.09) | −7.51* (−15.68 to 0.66) | 12.39* (−2.15 to 26.93) | −3.59*** (−5.81 to −1.37) | −1.79 (−8.71 to 5.12) | |
| Specialty mix (reference is primary care) | ||||||||
| Multispecialty practice type | −12.76** (−22.68 to −2.85) | −6.77 (−14.87 to 1.33) | −6.28 (−15.67 to 3.12) | −22.08*** (−30.61 to −13.56) | −13.56*** (−18.64 to −8.48) | −20.95*** (−36.65 to −5.24) | −12.87*** (−17.05 to −8.69) | |
| Single specialty practice type | −5.29* (−10.88 to 0.30) | 1.91 (−5.18 to 9.00) | −1.35 (−7.65 to 4.94) | −1.05 (−12.29 to 10.19) | −6.88 (−17.83 to 4.07) | −8.83*** (−15.47 to −2.19) | −3.51 (−8.67 to 1.65) | |
| Participated in QI program | 2.32 (−4.17 to 8.81) | 9.43 (−2.40 to 21.27) | −28.53** (−50.45 to −6.60) | 15.01* (−2.30 to 32.31) | 5.03 (−5.29 to 15.35) | 10.12 (−5.07 to 4.83) | 3.52 (−4.16 to 11.20) | |
| Patient-centered management index (range 0–5) | 1.01*** (0.33 to 1.69) | 1.42 (−4.01 to 6.85) | 3.61*** (2.27 to 4.94) | 8.35*** (3.92 to 12.78) | 2.74* (−0.05 to 5.52) | 3.75*** (1.86 to 5.63) | 3.24* (−0.46 to 6.93) | |
| Revenue from Medicaid or uninsured | 0.06 (−0.13 to 0.24) | 0.10 (−0.16 to 0.36) | −0.05 (−0.38 to 0.27) | 0.05 (−0.23 to 0.33) | 0.21 (−0.16 to 0.59) | 0.12 (−0.10 to 0.33) | 0.08 (−0.09 to 0.24) | |
| African-American patients | 0.07 (−0.07 to 0.22) | 0.23* (−0.01 to 0.47) | 0.04 (−0.36 to 0.43) | 0.28 (−0.13 to 0.68) | −0.09 (−0.31 to 0.12) | 0.05 (−0.19 to 0.29) | 0.14*** (0.04 to 0.25) | |
| Patients with limited English proficiency | −0.19 (−0.55 to 0.16) | −0.22 (−0.70 to 0.27) | 0.55* (−0.08 to 1.18) | −0.77*** (−1.34 to −0.20) | −0.32 (−1.01 to 0.37) | −0.36** (−0.70 to −0.02) | −0.08 (−0.34 to 0.17) | |
| Public reporting index (range 0–2) | −0.46 (−3.12 to 2.20) | 5.11** (0.25 to 9.96) | 6.06*** (4.36 to 7.75) | −0.77 (−8.79 to 7.25) | −7.82** (−14.45 to −1.18) | −0.50 (−2.78 to 1.79) | 0.14 (−3.22 to 3.50) | |
| Bonus income for HIT | 3.08 (−2.96 to 9.13) | −3.97 (−24.20 to 16.25) | 5.72** (0.40 to 11.04) | −2.22 (−15.03 to 10.60) | 8.43 (−3.63 to 20.49) | 3.96 (−2.25 to 10.17) | 0.75 (−9.59 to 11.09) | |
| Constant | 95.08*** (90.79 to 99.36) | 76.92*** (57.01 to 96.84) | 76.16*** (73.19 to 79.13) | 51.01*** (26.74 to 75.29) | 69.60*** (53.19 to 86.01) | 77.21*** (66.91 to 87.52) | 73.73*** (58.98 to 88.48) | |
| N | 576 | 551 | 451 | 387 | 379 | 240 | 626 | |
| R2 | 0.09 | 0.07 | 0.21 | 0.18 | 0.22 | 0.33 | 0.08 | |
*p<0.10; **p<0.05; ***p<0.01 .
†Because these models aggregate all five of the focal HIT functionalities, the dependent variable represents the average of the percent of physicians using each adopted function within each practice.
Ordinary Least Squares (OLS) regression analysis was used for all models. Results are presented as β coefficient (95% CI) and are weighted to be nationally representative.
Source: National Survey of Small and Medium-sized Physician Practices (July 2007–March 2009).
HIT, health information technology; HMO, health maintenance organization; IPA, independent practice association; PHO, physician–hospital organization; QI, quality improvement.
Discussion
Using a unique set of national data on small and medium-sized physician practices, we found that only 13% of practices had adopted all five key HIT functionalities, while 34% had adopted any of the five. In practices that had adopted any HIT, nearly 14% of individual physicians—one in seven—did not use available HIT functionalities.
We found that larger practices, practices participating in QI programs, practices potentially eligible to receive bonus income for adoption of HIT, and primary care practices were most likely to adopt HIT functionalities. This suggests either that QI programs and incentives for adoption of HIT are effective and/or that practices that participated in these programs are more likely, for reasons which we could not observe, to adopt HIT. Ownership by a hospital, system, or HMO was not significantly associated with the adoption or use of HIT; however, this may not be surprising in light of the lagging adoption rates of HIT by hospitals. As DesRoches and collaborators47 have reported, fewer than 30% of hospitals had adopted any HIT by 2011. As hospital use of HIT increases, many late adopting, hospital-owned physician practices may follow. We also found that practices treating more patients with limited English proficiency were less likely than others to have adopted HIT functionalities, suggesting that those practices might benefit from stronger financial and technical support.
Among practices adopting HIT functionalities, individual physicians were more likely to use the functionalities in larger practices, primary care practices, and practices that scored higher on a self-reported measure of patient-centeredness. Physicians in multispecialty practices were much less likely to use HIT once it had been adopted than those in primary care practices. Many general purpose HIT systems are not well-suited for specialist care, and the multitude of specialty-specific electronic health record platforms may add to the complexity of implementing HIT faced by multispecialty practices.48 Developing flexible HIT systems that fit well with different specialists’ particular needs may improve the rates of use among non-primary care physicians.
Notably, although practices were more likely to adopt HIT if they participated in one or more QI programs and if they had the potential to receive bonuses for use of HIT, these two factors were not associated with an increased probability that physicians within practices would use HIT, once it was adopted. More targeted incentives around the use of specific functionalities, as reflected in the design of the federal ‘Meaningful Use’ incentives,17 may help motivate use of HIT along with adoption.
Our analyses have limitations. First, the cross-sectional design limits our ability to draw causal inferences. Second, our study includes only practices with fewer than 20 physicians. Third, our data come from a single knowledgeable person within each physician practice. It is possible that the results would differ if more physicians within the practice had been queried or if use of the processes were independently audited. Finally, it is possible that practices that did not respond to the survey differed from those that did; however, the Survey of Small and Medium-sized Physician Practices had a high response rate (63.2%) and minimal response bias by practice size and specialty type (see the online supplementary appendix).
Conclusion
Adoption of HIT by a physician practice does not necessarily mean that physicians within the practice will use key functionalities provided by the HIT. Furthermore, the factors associated with adoption of HIT may be different from the factors associated with use of the HIT by individual physicians once their practice has adopted HIT.
Different types of practices may need different kinds of support in achieving meaningful use of HIT. Smaller practices may need special assistance—such as can be provided by regional extension centers—to help promote both adoption of HIT and use of the HIT by physicians once the practice has adopted it. Physicians in multispecialty practices will be more likely use HIT if vendors can create HIT systems that are perceived as useful by physicians across many specialties.
Better understanding of the differences between adoption of HIT by practices and use of HIT by individual physicians within adopting practices should aid planning for policy makers and leaders of provider organizations. Research is needed around the mechanisms driving these patterns, especially on factors such as organizational leadership, culture, and the specific role that HIT systems play in each healthcare setting.49
Acknowledgments
William Dow, in the Health Services and Policy Analysis Department, UC Berkeley School of Public Health, provided much appreciated feedback on an early draft of the manuscript. Additionally, the statements, findings, conclusions, views, and opinions contained and expressed in this article are based in part on data obtained under license from the following IMS Health Incorporated information service(s): Healthcare Organizational Services, Healthcare Relational Services (2011) IMS Health Incorporated. All Rights Reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IMS Health Incorporated or any of its affiliated or subsidiary entities.
Footnotes
Funding: The National Study of Small and Medium-Sized Physician Practices was funded by the Robert Wood Johnson Foundation (Award No. 35305).
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data from the National Study of Small and Medium-sized Physician Practices are not currently available publicly, but may be shared upon request.
References
- 1.Cebul RD, Love TE, Jain AK, et al. Electronic health records and quality of diabetes care. N Engl J Med 2011;365:825–33 [DOI] [PubMed] [Google Scholar]
- 2.Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood) 2011;30:464–71 [DOI] [PubMed] [Google Scholar]
- 3.Holroyd-Leduc JM, Lorenzetti D, Straus SE, et al. The impact of the electronic medical record on structure, process, and outcomes within primary care: a systematic review of the evidence. J Am Med Inform Assoc 2011;18:732–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herrin J, da Graca B, Nicewander D, et al. The effectiveness of implementing an electronic health record on diabetes care and outcomes. Health Serv Res 2012;47:1522–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Malley AS. Tapping the unmet potential of health information technology. N Engl J Med 2011;364:1090–1 [DOI] [PubMed] [Google Scholar]
- 6.Kern LM, Barrón Y, Dhopeshwarkar RV, et al. ,with the HITEC Investigators. Electronic health records and ambulatory quality of care. J Gen Intern Med 2012. (Epub ahead of print). doi:10.1007/s11606-012-2237-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hogan SO, Kissam SM. Measuring meaningful use. Health Aff (Millwood) 2010;29:601–6 [DOI] [PubMed] [Google Scholar]
- 8.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med 2008;359:50–60 [DOI] [PubMed] [Google Scholar]
- 9.Robinson JC, Casalino LP, Gillies RR, et al. Financial incentives, quality improvement programs, and the adoption of clinical information technology. Med Care 2009;47:411–17 [DOI] [PubMed] [Google Scholar]
- 10.Gans D, Kralewski J, Hammons T, et al. Medical groups’ adoption of electronic health records and information systems. Health Aff (Millwood) 2005;24:1323–33 [DOI] [PubMed] [Google Scholar]
- 11.Hsiao CJ, Decker SL, Hing E, et al. Most physicians were eligible for federal incentives in 2011, but few had EHR systems that met meaningful-use criteria. Health Aff (Millwood) 2012;31:1100–7 [DOI] [PubMed] [Google Scholar]
- 12.Rao SR, Desroches CM, Donelan K, et al. Electronic health records in small physician practices: availability, use, and perceived benefits. J Am Med Inform Assoc 2011;18:271–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nanji KC, Cina J, Patel N, et al. Overcoming barriers to the implementation of a pharmacy bar code scanning system for medication dispensing: a case study. J Am Med Inform Assoc 2009;16:645–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller RH, Sim I. Physicians’ use of electronic medical records: barriers and solutions. Health Aff (Millwood) 2004;23:116–26 [DOI] [PubMed] [Google Scholar]
- 15.Ash JS, Sittig DF, Wright A, et al. Clinical decision support in small community practice settings: a case study. J Am Med Inform Assoc 2011;18:879–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blumenthal D, Tavenner M. The ‘meaningful use’ regulation for electronic health records. N Engl J Med 2010;363:501–4 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare and Medicaid Services CMS EHR Meaningful Use Overview. Last modified: 10/12/2011. Cited 2012 Jul 2. https://www.cms.gov/ehrincentiveprograms/30_Meaningful_Use.asp (accessed 20 Nov 2011).
- 18.Simon SR, McCarthy ML, Kaushal R, et al. Electronic health records: which practices have them, and how are clinicians using them? J Eval Clin Pract 2008;14:43–7 [DOI] [PubMed] [Google Scholar]
- 19.Casalino L, Gillies RR, Shortell SM, et al. External incentives information technology and organized processes to improve healthcare quality for patients with chronic diseases. JAMA 2003;289:434–41 [DOI] [PubMed] [Google Scholar]
- 20.Shortell SM, Gillies R, Siddique J, et al. Improving chronic illness care: a longitudinal cohort analysis of large physician organizations. Med Care 2009;47:932–9 [DOI] [PubMed] [Google Scholar]
- 21.Rittenhouse DR, Casalino LP, Shortell SM. Small and medium-size physician practices use few patient-centered medical home processes. Health Aff (Millwood) 2011;30:1575–84 [DOI] [PubMed] [Google Scholar]
- 22.Felt-Lisk S, Johnson L, Fleming C, et al. Toward understanding EHR use in small physician practices. Health Care Financ Rev 2010;31:11–22 [PMC free article] [PubMed] [Google Scholar]
- 23.Skolnik NS, Timko M, Myers C. A view from the trenches: primary care physicians on electronic health records. In: Skolnik NS, ed., Electronic medical records: a practical guide for primary care. New York: Humana Press, 2011;15–36 [Google Scholar]
- 24.The Commonwealth fund The development and testing of EHR-based care coordination performance measures in ambulatory care. 2011. Cited 2012 Jul 2. http://www.commonwealthfund.org/~/media/Files/Publications/Issue%20Brief/2011/Nov/1551_Chan_devel_testing_EHRbased_care_coord_tech_report.pdf
- 25.Thompson J. Organizations in action. Brunswick, NJ: McGraw, 1967 [Google Scholar]
- 26.IMS Health Incorporated. Healthcare Relational Services. 2012. http://www.imshealth.com/portal/site/ims/menuitem.edb2b81823f67dab41d84b903208c22a/?vgnextoid=9c08be83557d0310VgnVCM1000007f8c2ca2RCRD (accessed 31 Jan 2013). [Google Scholar]
- 27.Nyweide DJ, Weeks WB, Gottlieb DJ, et al. Relationship of primary care physicians’ patient caseload with measurement of quality and cost performance. JAMA 2009;302:2444–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.IMS Health Incorporated. Data and information resources. 2012. http://www.imshealth.com/portal/site/ims/menuitem.5ad1c081663fdf9b41d84b903208c22a/?vgnextoid=9bf947a738e80310VgnVCM1000007f8c2ca2RCRD (accessed 31 Jan 2013). [Google Scholar]
- 29.Casalino LP, Rittenhouse DR, Gillies RR, et al. Specialist physician practices as patient-centered medical homes. N Engl J Med 2010;362:1555–8 [DOI] [PubMed] [Google Scholar]
- 30.Painter MW, Lavizzo-Mourey R. Aligning Forces for Quality: a program to improve health and health care in communities across the United States. Health Aff (Millwood) 2008;27:1461–4 [DOI] [PubMed] [Google Scholar]
- 31.Aligning forces for quality, national program office Aligning forces for quality: improving health and healthcare in communities across America. Cited 2012 Jul 2. http://forces4quality.org/
- 32.American Association for Public Opinion Research Standard Definitions. Deerfield, IL: AAPOR, 2009. http://www.aapor.org/Standard_Definitions1.htm (accessed 31 Jan 2013). [Google Scholar]
- 33.Ulrich D, Smallwood N. Capitalizing on capabilities. Harv Bus Rev 2004;82:119–27 [PubMed] [Google Scholar]
- 34.Robinson JC, Casalino LP. Vertical integration and organizational networks in health care. Health Aff (Millwood) 1996;15:7–22 [DOI] [PubMed] [Google Scholar]
- 35.Institute of Medicine, Committee on Quality of Health Care in America Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press, 2001 [Google Scholar]
- 36.Rittenhouse DR, Shortell SM, Gillies RR. Improving chronic illness care: findings from a national study of care management processes in large physician practices. Med Care Res Rev 2010;67:301–20 [DOI] [PubMed] [Google Scholar]
- 37.Shortell SM, Marsteller JA, Lin M, et al. The role of perceived team effectiveness in improving chronic illness care. Med Care 2004;42:1040–8 [DOI] [PubMed] [Google Scholar]
- 38.Department of Commerce, National Institute of Standards and Technology, Baldrige National Quality Program Health care criteria for performance excellence. 2009. http://www.nist.gov/baldrige/publications/upload/2009_2010_HealthCare_Criteria.pdf (accessed 31 Jan 2013).
- 39.Martsolf GR, Alexander JA, Shi Y, et al. The patient-centered medical home and patient experience. Health Serv Res 2012;47:2273–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Varkey AB, Manwell LB, Williams ES, et al. Separate and unequal: clinics where minority and nonminority patients receive primary care. Arch Intern Med 2009;169:243–50 [DOI] [PubMed] [Google Scholar]
- 41.Friedberg MW, Coltin KL, Safran DG, et al. Medical home capabilities of primary care practices that serve sociodemographically vulnerable neighborhoods. Arch Intern Med 2010;170:938–44 [DOI] [PubMed] [Google Scholar]
- 42.StataCorp LP Margins. In: Stata Base Reference Manual: Release 12. College Station, TX: StataCorp LP, 2011:1027–98 [Google Scholar]
- 43.Wooldridge JM. Introductory Econometrics: a Modern Approach. Mason, OH: Thomson South-western, 2006 [Google Scholar]
- 44.StataCorp LP Svy. In: Stata Survey Data Reference Manual: Release 12. College Station, TX: StataCorp LP, 2011:66–73 [Google Scholar]
- 45.Downs SM, Anand V, Dugan TM, et al. You can lead a horse to water: physicians’ responses to clinical reminders. AMIA Annu Symp Proc 2010;2010:167–71 [PMC free article] [PubMed] [Google Scholar]
- 46.Shojania KG, Jennings A, Mayhew A, et al. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev 2009;(3):CD001096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.DesRoches CM, Worzala C, Joshi MS, et al. Small, nonteaching, and rural hospitals continue to be slow in adopting electronic health record systems. Health Aff (Millwood) 2012;31:1092–9 [DOI] [PubMed] [Google Scholar]
- 48.Mandl KD, Kohane IS. Escaping the EHR trap—the future of health IT. N Engl J Med 2012;366:2240–2 [DOI] [PubMed] [Google Scholar]
- 49.Nembhard IM, Singer SJ, Shortell SM. The cultural complexity of medical groups. Health Care Manage Rev 2012;37:200–13 [DOI] [PubMed] [Google Scholar]